Published online Jan 28, 2017. doi: 10.3748/wjg.v23.i4.661
Peer-review started: October 7, 2016
First decision: November 9, 2016
Revised: November 15, 2016
Accepted: December 2, 2016
Article in press: December 2, 2016
Published online: January 28, 2017
Processing time: 106 Days and 0.4 Hours
To assess the long-term outcomes of this procedure after removal of self-expandable metal stent (SEMS). The efficacy and safety of endoscopic ultrasound-guided gallbladder drainage (EUS-GBD) with SEMS were also assessed.
Between January 2010 and April 2015, 12 patients with acute calculous cholecystitis, who were deemed unsuitable for cholecystectomy, underwent EUS-GBD with a SEMS. EUS-GBD was performed under the guidance of EUS and fluoroscopy, by puncturing the gallbladder with a needle, inserting a guidewire, dilating the puncture hole, and placing a SEMS. The SEMS was removed and/or replaced with a 7-Fr plastic pigtail stent after cholecystitis improved. The technical and clinical success rates, adverse event rate, and recurrence rate were all measured.
The rates of technical success, clinical success, and adverse events were 100%, 100%, and 0%, respectively. After cholecystitis improved, the SEMS was removed without replacement in eight patients, whereas it was replaced with a 7-Fr pigtail stent in four patients. Recurrence was seen in one patient (8.3%) who did not receive a replacement pigtail stent. The median follow-up period after EUS-GBD was 304 d (78-1492).
EUS-GBD with a SEMS is a possible alternative treatment for acute cholecystitis. Long-term outcomes after removal of the SEMS were excellent. Removal of the SEMS at 4-wk after SEMS placement and improvement of symptoms might avoid migration of the stent and recurrence of cholecystitis due to food impaction.
Core tip: Endoscopic ultrasound-guided gallbladder drainage (EUS-GBD) was recently used to treat acute cholecystitis. The aim of this study was to assess the utility of removal of self-expandable metal stent (SEMS) at 4-wk after EUS-GBD. Twelve patients with acute calculous cholecystitis underwent EUS-GBD with a SEMS. The rates of technical success, clinical success, and adverse events were 100%, 100%, and 0%, respectively. Recurrence was seen in one patient (8.3%). The median follow-up period after EUS-GBD was 304 d. Removal of the SEMS at 4-wk after SEMS placement might avoid migration of the stent and recurrence of cholecystitis due to food impaction.
- Citation: Kamata K, Takenaka M, Kitano M, Omoto S, Miyata T, Minaga K, Yamao K, Imai H, Sakurai T, Watanabe T, Nishida N, Kudo M. Endoscopic ultrasound-guided gallbladder drainage for acute cholecystitis: Long-term outcomes after removal of a self-expandable metal stent. World J Gastroenterol 2017; 23(4): 661-667
- URL: https://www.wjgnet.com/1007-9327/full/v23/i4/661.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i4.661
Laparoscopic cholecystectomy is the standard treatment for acute cholecystitis caused by cholecystolithiasis[1,2]. For patients at high surgical risk, percutaneous transhepatic gallbladder aspiration (PTGBA) or percutaneous transhepatic gallbladder drainage (PTGBD) can be selected for treatment of cholecystitis. However, the efficacy rate of PTGBA is insufficient (61%-77%), and PTGBD involves an external drainage tube, which decreases the ability of the patient to carry out their normal daily activities[3,4]. Recently, endoscopic ultrasound-guided gallbladder drainage (EUS-GBD) was developed for acute cholecystitis[5-17]. Jang et al[14] showed that EUS-GBD was comparable with PTGBD in terms of its technical feasibility, efficacy, and procedural safety.
The aim of this study was to evaluate the outcomes of EUS-GBD in patients with acute calculous cholecystitis deemed unsuitable for cholecystectomy. The examined procedure used a self-expandable metal stent (SEMS), and we also assessed the long-term outcomes of the procedure following removal of the SEMS.
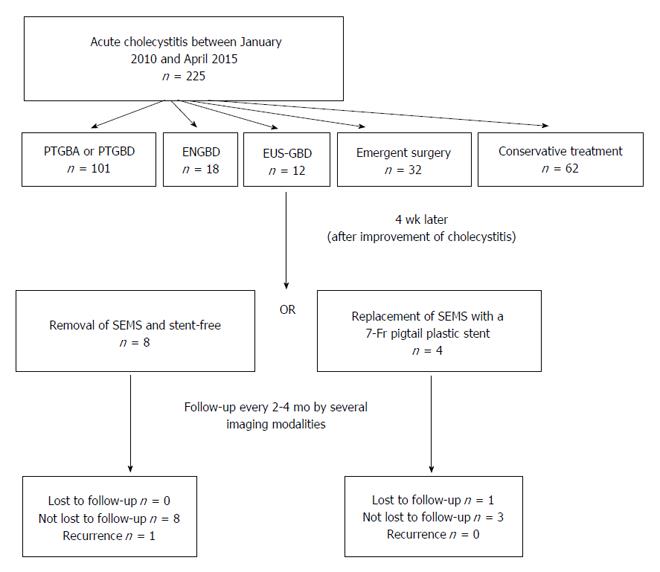
Between January 2006 and October 2014, 225 patients with acute cholecystitis due to gallstones visited our hospital. Among these, 101, 18, 32, and 62 patients underwent PTGBA and/or PTGBD, endoscopic naso-gallbladder drainage, emergent surgery and conservative treatment, respectively. The remaining 12 patients with acute calculous cholecystitis, who were deemed unsuitable for cholecystectomy because of poor surgical performance indications and had a risk of self-removal of drainage tube, underwent EUS-GBD. Cases of cholecystitis due to deployment of the metal stent and the cases that cystic duct was obstructed due to advanced cancer were excluded from this study.
The surgical performance indications for all patients were poor (class III or IV on the American Society of Anesthesiologists (ASA) Physical Status classification system). These patients were identified by retrospective review of the medical database of our hospital. Acute calculous cholecystitis was diagnosed in all patients on the basis of the characteristic clinical features (abdominal pain and fever), laboratory data (high level of serum C-reactive protein; CRP), and imaging studies. The study was approved by the institutional review board of the Kinki University Faculty of Medicine, and informed consent was obtained from the patients after explaining to them that we could perform PTGBA, PTGBD, or EUS-GBD.
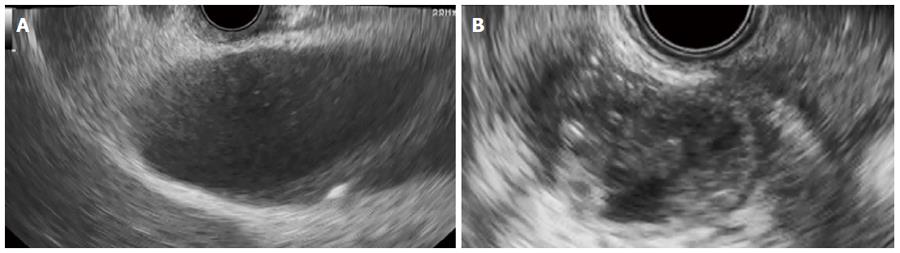
An echoendoscope (GF-UCT240-AL5, Olympus, Tokyo, Japan) was introduced into the stomach or duodenum. The echoendoscope images were used to ensure that gallstones were present in the swollen gallbladder before EUS-GBD was performed. After visualization of the swollen gallbladder adjacent to the antrum or duodenal bulb, the echoendoscope was manipulated until an appropriate puncture route, free from interposing vessels, was identified. The puncture site was selected as the region where the distance between the gastrointestinal tract and the gallbladder was smallest (1 cm or less). When both the stomach and duodenum provided equally good access, the duodenum was selected as the puncture site because it was easier to maintain the scope position at the duodenum than at the stomach.
The neck or body of the gallbladder was generally chosen as the ideal target, and was then punctured with a 19G needle (EchoTip Ultra, Cook Medical, Limerick, Ireland) under endosonographic guidance. The gallbladder was then irrigated with a saline solution through the 19G needle, using a 20 mL syringe. Irrigation was performed at least ten times, and was continued until the color of the bile became weak. This was performed to prevent peritonitis due to bile leakage immediately after the gallbladder was punctured. Thereafter, a sufficient length of 0.035 inch guidewire (Revowave, Piolax, Kanagawa, Japan) was inserted into the gallbladder lumen until there were more than two coils present. The puncture tract was then serially dilated using either biliary dilation catheters (6F-7F-9F, Soehendra Biliary Dilation Catheter, Cook, Bloomington, IN, United States) or a balloon dilator (Max Pass 4 mm, Olympus, Tokyo, Japan) over the guidewire. If passing dilators or balloons proved difficult, electrocautery was planned to be used. A SEMS (10 mm in diameter, 6 cm in length, Wallflex partially covered stent, Boston Scientific, Natick, MA, United States) was deployed between the gallbladder and the stomach or duodenum. If functional success was obtained, the SEMS was removed and/or replaced with a 7-Fr plastic pigtail stent (4 or 6 cm in length) 4 wk after the original EUS-GBD (Figure 1). Where possible, the stent was replaced after removal of the SEMS in order to keep the fistula considering the possibility of the recurrence. This technique was approved by the institutional review board of the Kinki University Faculty of Medicine.
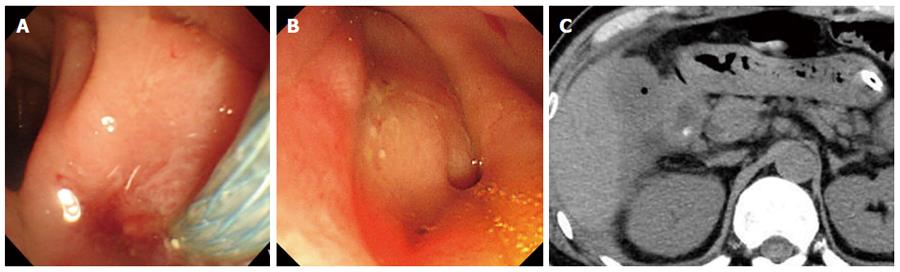
Several imaging modalities including ultrasonography, computed tomography (CT), fistulography, and/or EUS were performed to determine if gallstones remained in the gallbladder before removal of the SEMS. CT (looking for air images in the gallbladder) and/or fistulography were performed to determine if the fistula remained open 1 wk after removal of the SEMS. After removal of the SEMS, patients were continually followed up by blood tests and imaging modalities every 2-4 mo. It was determined whether the cystic duct was patent before and after removal of the SEMS by performing fistulography and/or EUS.
The long-term outcomes of EUS-GBD after removal of SEMS was the primary outcomes in this study. The outcomes assessed were technical and clinical success rates, adverse events rate, and recurrence rate. Technical success was defined as successful stent deployment between the gallbladder lumen and the stomach or duodenum. Clinical success was defined as improvement of typical clinical symptoms within 3 d, with confirmatory laboratory tests, with or without improved radiologic findings[14]. The incidence of the following adverse events was assessed: peritonitis, bile leakage, bleeding, stent migration, and stent occlusion. Recurrence of acute cholecystitis after EUS-GBD was defined on the basis of the characteristic clinical features, laboratory data, and imaging studies.
Continuous variables are expressed as median or mean values with standard deviation or range. All statistical analyses were performed using SAS software version 9.1 (SAS Institute, Cary, NC, United States).
Table 1 shows the patients’ characteristics. In total, 12 patients (mean age 76 years, 9 men and 3 women) underwent EUS-GBD. Eight patients were ASA class III, and the others were ASA class IV. One patient had advanced ovarian cancer which expected long-term survival and there was no influence of the tumor on the cystic duct. Blood examination revealed a mean white blood cell (WBC) count of 14525 cells per μL and a mean CRP level of 15.7 mg/dL. All cases were moderate cholecystitis. The diameter of gallstones was less than 10 mm in all patients. The EUS-GBD procedure was performed via the stomach or duodenum in three and nine cases, respectively. The distance between the gastrointestinal tract and the gallbladder was 1 cm or less in all cases. Dilation of the puncture site was performed by biliary dilation and/or balloon catheters without using electrocautery. Table 2 shows the outcomes of EUS-GBD. The technical success and clinical success rates were both 100% (12/12), with no adverse events recorded. At day 3 post-EUS-GBD, the mean WBC count and mean CRP were 7075 cells per μL and 2.37 mg/dL, respectively. The SEMS was removed from eight patients 4 wk after the EUS-GBD. In these eight patients, the plastic pigtail stent was not deployed after removal of the SEMS because the guidewire could not be sufficiently inserted due to shrinkage of the gallbladder by the EUS-GBD treatment. In the remaining four patients, the SEMS was replaced with a 7-Fr plastic double pigtail stent 4 wk after EUS-GBD. The median post-EUS-GBD follow-up period for these 12 patients was 304 d. During the follow-up period, one of the patients (8.3%) died due to advanced cancer. At the time the records were subjected to retrospective evaluation (April 1, 2016), recurrence was present in one of the patients (8.3%) who did not receive a replacement pigtail stent (Figure 2). In four patients received replacement of SEMS with a 7-Fr plastic double pigtail stent, the stent was kept permanently in all of those patients.
| Characteristics | |
| Age, mean ± SD, yr | 76.3 ± 12.1 |
| Sex, male/female | 9/3 |
| Underlying condition | |
| III | 66.7% (8/12) |
| IV | 33.3% (4/12) |
| Advanced malignancy | 8.3% (1/12) |
| White blood cell count (mean, range) | 14525 (9100-21300) per μL |
| C-reactive protein (mean, range) | 15.7 (2.0-32.7) mg/dL |
| Technical success rate | 100% (12/12) |
| Functional success rate | 100% (12/12) |
| Rate of removal | 67% (8/12) |
| Rate of replacement | 33% (4/12) |
| Adverse events | 0% (0/12) |
| Recurrence of cholecystitis | 8.3% (1/12) |
| Follow-up period, days [median, range] | 304 (78-1492) |
| Patient status on follow-up | |
| Alive | 91.7% (11/12) |
| Dead | 8.3% (1/12) |
Before removal of the SEMS, gallstones did not remain in the gallbladder in all cases. One week after removal of the SEMS, air in the gallbladder was imaged by CT in nine cases (Figure 3). The other three cases that did not show air images in the gallbladder were cases in which the double pigtail plastic stents were not deployed. Fistulography was performed in eight cases that did not undergo replacement of the stent. Among these, fistulography images of the gallbladder were obtained in three cases. In total, the fistula was confirmed by CT and/or fistulography in 9 of 12 cases. Cystic duct patency was confirmed by fistulography and/or EUS before as well as 1 week after removal of the SEMS in all cases.
The aim of the current study was to evaluate the feasibility of EUS-GBD for patients with acute calculous cholecystitis, who were deemed unsuitable for cholecystectomy. In this study, both technical and clinical success was achieved in the treatment of acute cholecystitis in all 12 patients. One of the risks of EUS-GBD is bile leakage into the peritoneal space, which can cause bile peritonitis. The bile leakage is caused by migration of the stent exposing the gap between the puncture tract and the stent[5,6,8]. In the present study, several techniques were used to avoid such bile leakage. Firstly, the guidewire was inserted until at least two full coils were in the lumen. The gallbladder lumen has more space for coiling than the bile duct, and yields better stability. Secondly, we irrigated the gallbladder lumen with saline solution after puncturing the gallbladder and before proceeding to the next step. This irrigation procedure may reduce the chance of peritonitis due to bile leakage during dilation. We also used SEMSs in our study, and, compared with plastic stents, SEMSs are better at sealing the gap between the stent and the needle tracts in the gallbladder wall, thus preventing bile leakage[8]. As a result, no adverse events occurred in this study. In a systematic review of EUS-guided biliary drainage by Wang et al[18] in 2016, the rate of adverse events was 38.46% in the group in which cystotomes were used during dilation of the puncture site, which was higher than that in the group in which dilators or balloons were used. Dilation of the puncture site was performed by biliary dilation and/or balloon catheters without using electrocautery in this study. This might be another reason why there were no adverse events in this study.
During a long-term follow-up with a median period of 275 d, Choi et al[19] reported that stent distal migration was noted in two patients (3.6%), one at 170 d and the other at 303 d post-EUS-GBD. They also reported recurrence of acute cholecystitis due to food impaction. To avoid stent migration and food impaction into the gallbladder, we either removed the SEMS, or replaced it with a pigtail plastic stent, 4 wk after EUS-GBD. In our study, there was neither stent migration nor food impaction. Performance of these additional procedures after EUS-GBD may prevent such complications.
Recently, the use of lumen-apposing metal stents (LAMS) with anchor flanges and flares for EUS-GBD resulted in excellent outcomes[13,15,20]. With a LAMS, the distance between the gastrointestinal tract and the gallbladder needs to be 1 cm or less[19]. In terms of this, a conventional biliary SEMS may have allowed us more freedom in selecting the puncture site, although this is not certain because the distance was 1 cm or less in all cases in this study.
In a study examining the use of LAMS for high-risk surgical patients with acutecholecystitis[20], Walter et al[20] reported that technical success was 90%, and clinical success was 96%, and that no migration was seen in any patients. In 15 of the 27 patients with technical success, LAMS were removed approximately 3 mo after EUS-GBD, whereas they were left in place in the other 12 patients. Removal of the LAMS was not achieved due to tissue overgrowth in two patients. Two patients also developed a LAMS obstruction. Thus, long-term deployment of metal stents in EUS-GBD could cause adverse events, including food impaction. Therefore, early removal of the metal stent after EUS-GBD, at a time of around 4 wk (as in the present study), may be considered desirable. However, we did observe a recurrence of acute cholecystitis in one patient (8.3%), where the SEMS was not replaced with a pigtail stent. There is a possibility that this patient recurred cholecystitis due to uncertain small gallstones or sludge remaining after EUS-GBD. Therefore, replacement with a pigtail plastic stent may be helpful for avoiding recurrence. Another reason for the low recurrence rate in this study might be that no gallstones remained in the gallbladder before removal of the SEMS in all cases.
Moon et al[21] reported that gross pathology showed adherence of the gallbladder to the stomach wall around the site of cholecystogastrostomy 4 wk after LAMS removal in an animal study. We also performed a preliminary examination of EUS-guided biliary drainage using a conventional biliary SEMS in an animal study using five pigs. We found that at autopsy 1 wk after the procedure, fistulas were created between the bile duct and duodenum in all pigs[22]. Thus, a strong fistula might develop between the gallbladder and the gastrointestinal tract within 4 wk using a conventional biliary SEMS as well as a LAMS. This study has a few limitations. Firstly, the number of EUS-GBD cases was low, and all cases were from a single institute. Secondly, the indications for EUS-GBD were limited to those patients deemed unsuitable for cholecystectomy. A larger study comparing the efficacy and safety of EUS-GBD with and without early SEMS removal is warranted. However, a large number of institutions are needed to obtain the required number of patients, otherwise the criteria used for patient selection should be less strict.
In a systematic review of EUS-GBD, LAMS seemed to have a high potential in terms of efficacy and safety; however, the technical success of LAMS (91.5%) was lower than that of conventional biliary SEMS (98.6%)[23]. Further studies including long-term results are required to investigate whether SEMS or LAMS are better for EUS-GBD.EUS-GBD with SEMS is a possible alternative treatment for acute cholecystitis. Long-term outcomes after removal of SEMS were promising. Removal of the SEMS after SEMS placement and improvement of symptoms might avoid migration of the stent and recurrence of cholecystitis due to food impaction.
Laparoscopic cholecystectomy is the standard treatment for acute cholecystitis caused by cholecystolithiasis. For patients at high surgical risk, percutaneous transhepatic gallbladder aspiration (PTGBA) or percutaneous transhepatic gallbladder drainage (PTGBD) can be selected for treatment of cholecystitis. However, the efficacy rate of PTGBA is insufficient (61%-77%), and PTGBD involves an external drainage tube, which decreases the ability of the patient to carry out their normal daily activities. Recently, endoscopic ultrasound-guided gallbladder drainage (EUS-GBD) was developed for acute cholecystitis.
There were few reports on long term outcomes of EUS-GBD. This study, the Long-term outcomes after removal of self-expandable metal stent (SEMS), was first report and the results of this study contribute to clarifying the potential of this procedure for acute cholecystitis.
In this study, EUS-GBD using SEMS was a useful for removal of gallstones in the gallbladder. Gallstones disappeared after EUS-GBD in all cases. During long-term follow-up period after the removal of the SEMS, the recurrence of the cholecystitis was seen in only one patient (8.3%) and there were no complications.
This study suggests that EUS-GBD using SEMS and removal of the SEMS 4 wk after the procedure are useful for patients with cholecystitis who were deemed unsuitable for cholecystectomy.
This study described the use of EUS-GBD for the treatment of acute cholecystitis in patients deemed unsuitable for surgical procedures. Long-term outcomes after removal of SEMS were promising. Removal of the SEMS after SEMS placement and improvement of symptoms might avoid migration of the stent and recurrence of cholecystitis due to food impaction. A larger study comparing the efficacy and safety of EUS-GBD with and without early SEMS removal is warranted.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Cariati A, Tsuyuguchi T, Tuncyurek O S- Editor: Qi Y L- Editor: A E- Editor: Wang CH
| 1. | Reddick EJ, Olsen DO. Laparoscopic laser cholecystectomy. A comparison with mini-lap cholecystectomy. Surg Endosc. 1989;3:131-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 604] [Cited by in RCA: 541] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 2. | Dubois F, Icard P, Berthelot G, Levard H. Coelioscopic cholecystectomy. Preliminary report of 36 cases. Ann Surg. 1990;211:60-62. [PubMed] |
| 3. | Chopra S, Dodd GD, Mumbower AL, Chintapalli KN, Schwesinger WH, Sirinek KR, Dorman JP, Rhim H. Treatment of acute cholecystitis in non-critically ill patients at high surgical risk: comparison of clinical outcomes after gallbladder aspiration and after percutaneous cholecystostomy. AJR Am J Roentgenol. 2001;176:1025-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 89] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 4. | Ito K, Fujita N, Noda Y, Kobayashi G, Kimura K, Sugawara T, Horaguchi J. Percutaneous cholecystostomy versus gallbladder aspiration for acute cholecystitis: a prospective randomized controlled trial. AJR Am J Roentgenol. 2004;183:193-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 125] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 5. | Baron TH, Topazian MD. Endoscopic transduodenal drainage of the gallbladder: implications for endoluminal treatment of gallbladder disease. Gastrointest Endosc. 2007;65:735-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 120] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 6. | Súbtil JC, Betes M, Muñoz-Navas M. Gallbladder drainage guided by endoscopic ultrasound. World J Gastrointest Endosc. 2010;2:203-209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (1)] |
| 7. | Lee SS, Park DH, Hwang CY, Ahn CS, Lee TY, Seo DW, Lee SK, Kim MW. EUS-guided transmural cholecystostomy as rescue management for acute cholecystitis in elderly or high-risk patients: a prospective feasibility study. Gastrointest Endosc. 2007;66:1008-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 77] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Takasawa O, Fujita N, Noda Y, Kobayashi G, Ito K, Horaguchi J, Obana T. Endosonography-guided gallbladder drainage for acute cholecystitis following covered metal stent deployment. Dig Endosc. 2009;21:43-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Itoi T, Itokawa F, Kurihara T. Endoscopic ultrasonography-guided gallbladder drainage: actual technical presentations and review of the literature (with videos). J Hepatobiliary Pancreat Sci. 2011;18:282-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Song TJ, Park DH, Eum JB, Moon SH, Lee SS, Seo DW, Lee SK, Kim MH. EUS-guided cholecystoenterostomy with single-step placement of a 7F double-pigtail plastic stent in patients who are unsuitable for cholecystectomy: a pilot study (with video). Gastrointest Endosc. 2010;71:634-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 62] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 11. | Jang JW, Lee SS, Park DH, Seo DW, Lee SK, Kim MH. Feasibility and safety of EUS-guided transgastric/transduodenal gallbladder drainage with single-step placement of a modified covered self-expandable metal stent in patients unsuitable for cholecystectomy. Gastrointest Endosc. 2011;74:176-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 106] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 12. | Kamata K, Kitano M, Komaki T, Sakamoto H, Kudo M. Transgastric endoscopic ultrasound (EUS)-guided gallbladder drainage for acute cholecystitis. Endoscopy. 2009;41 Suppl 2:E315-E316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Itoi T, Binmoeller KF, Shah J, Sofuni A, Itokawa F, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N. Clinical evaluation of a novel lumen-apposing metal stent for endosonography-guided pancreatic pseudocyst and gallbladder drainage (with videos). Gastrointest Endosc. 2012;75:870-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 311] [Article Influence: 23.9] [Reference Citation Analysis (0)] |
| 14. | Jang JW, Lee SS, Song TJ, Hyun YS, Park DY, Seo DW, Lee SK, Kim MH, Yun SC. Endoscopic ultrasound-guided transmural and percutaneous transhepatic gallbladder drainage are comparable for acute cholecystitis. Gastroenterology. 2012;142:805-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 180] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 15. | de la Serna-Higuera C, Pérez-Miranda M, Gil-Simón P, Ruiz-Zorrilla R, Diez-Redondo P, Alcaide N, Sancho-del Val L, Nuñez-Rodriguez H. EUS-guided transenteric gallbladder drainage with a new fistula-forming, lumen-apposing metal stent. Gastrointest Endosc. 2013;77:303-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 94] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 16. | Ogura T, Masuda D, Imoto A, Umegaki E, Higuchi K. EUS-guided gallbladder drainage and hepaticogastrostomy for acute cholecystitis and obstructive jaundice (with video). Endoscopy. 2014;46 Suppl 1 UCTN:E75-E76. [PubMed] |
| 17. | Teoh AY, Binmoeller KF, Lau JY. Single-step EUS-guided puncture and delivery of a lumen-apposing stent for gallbladder drainage using a novel cautery-tipped stent delivery system. Gastrointest Endosc. 2014;80:1171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 85] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 18. | Wang K, Zhu J, Xing L, Wang Y, Jin Z, Li Z. Assessment of efficacy and safety of EUS-guided biliary drainage: a systematic review. Gastrointest Endosc. 2016;83:1218-1227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 266] [Cited by in RCA: 233] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 19. | Choi JH, Lee SS, Choi JH, Park DH, Seo DW, Lee SK, Kim MH. Long-term outcomes after endoscopic ultrasonography-guided gallbladder drainage for acute cholecystitis. Endoscopy. 2014;46:656-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 117] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 20. | Walter D, Teoh AY, Itoi T, Pérez-Miranda M, Larghi A, Sanchez-Yague A, Siersema PD, Vleggaar FP. EUS-guided gall bladder drainage with a lumen-apposing metal stent: a prospective long-term evaluation. Gut. 2016;65:6-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 146] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 21. | Moon JH, Choi HJ, Kim DC, Lee YN, Kim HK, Jeong SA, Lee TH, Cha SW, Cho YD, Park SH. A newly designed fully covered metal stent for lumen apposition in EUS-guided drainage and access: a feasibility study (with videos). Gastrointest Endosc. 2014;79:990-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 70] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 22. | Minaga K, Kitano M, Gon C, Yamao K, Imai H, Miyata T, Kamata K, Omoto S, Takenaka M, Kudo M. Endoscopic ultrasonography-guided choledochoduodenostomy using a newly designed laser-cut metal stent: Feasibility study in a porcine model. Dig Endosc. 2016; Epub ahead of print. [PubMed] |
| 23. | Anderloni A, Buda A, Vieceli F, Khashab MA, Hassan C, Repici A. Endoscopic ultrasound-guided transmural stenting for gallbladder drainage in high-risk patients with acute cholecystitis: a systematic review and pooled analysis. Surg Endosc. 2016;30:5200-5208. [PubMed] |