Published online Sep 7, 2017. doi: 10.3748/wjg.v23.i33.6187
Peer-review started: March 16, 2017
First decision: May 12, 2017
Revised: May 31, 2017
Accepted: July 12, 2017
Article in press: July 12, 2017
Published online: September 7, 2017
Processing time: 175 Days and 13.4 Hours
Arterioportal shunt (APS) is an organic communication between the hepatic arterial system and the portal venous system. The APS is one of the major causes of transient hepatic attenuation differences on dynamic computed tomography (CT) or magnetic resonance imaging (MRI). This condition is usually associated with trauma, liver cirrhosis, and malignancies of the liver. However, there has been no report about oxaliplatin-induced APS. A 41-year-old male was diagnosed with Stage IIIB gastric cancer. The patient initially underwent neoadjuvant chemotherapy with capecitabine and oxaliplatin After 3 cycles of therapy, the mass had markedly decreased, and a total gastrectomy with splenectomy was performed. Since the malignancy was locally invasive, the patient was continued on the same regimen of the adjuvant chemotherapy. After 3 more cycles, a computed tomography revealed a 1 cm sized arterial-enhancing nodule in the right lobe of the liver. An MRI revealed an arterial enhancing lesion, and a positron emission tomography CT scan showed a hypermetabolic lesion in the same portion of the liver. We tried to perform a liver biopsy; however, an ultrasonography could not detect any mass. A presumptive diagnosis of an APS due to a recurred cancer was made. We found a similar but slightly different case report of an oxaliplatin-induced liver injury, mimicking a metastatic tumor on an MRI. Based on a prior report, the patient was continued on treatment with adjuvant chemotherapy following discontinuation of oxaliplatin. After 2 cycles, the arterial enhancing liver mass resolved, supporting the final diagnosis of an APS, related to oxaliplatin-induced sinusoidal injury. The patient has not experienced any a relapse after two years of additional follow up recurrent gastric cancer upon interpretation of multiple imaging modalities.
Core tip: Although there have been several recent reports about oxaliplatin-induced sinusoidal injury, this is first case report of a non-tumorous incidental arterioportal shunt following oxaliplatin chemotherapy. We made a presumptive diagnosis of an AP shunt mimicking a recurred gastric cancer, due to an oxaliplatin-induced transsinusoidal injury. This case is the first report of an oxaliplatin-induced incidental arterioportal shunt mimicking recurred gastric cancer on various images.
- Citation: Kim HB, Park SG. Arterioportal shunt incidental to treatment with oxaliplatin that mimics recurrent gastric cancer. World J Gastroenterol 2017; 23(33): 6187-6193
- URL: https://www.wjgnet.com/1007-9327/full/v23/i33/6187.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i33.6187
Transient hepatic attenuation differences (THAD) lesions indicate areas of parenchymal enhancement, visible during the hepatic artery phase on a dynamic computed tomography (CT) or magnetic resonance imaging (MRI), and are thought to be a physiological phenomenon due to the dual hepatic blood supply. The arterioportal shunt (APS) is one of the most important THAD[1,2].
APS is an organic communication between the hepatic arterial system and the portal venous system, and is caused by the redistribution of arterial flow into a focal region of the portal venous flow. This condition is associated with hepatic tumors, trauma, intervention, liver cirrhosis and metastatic tumors[2-5].
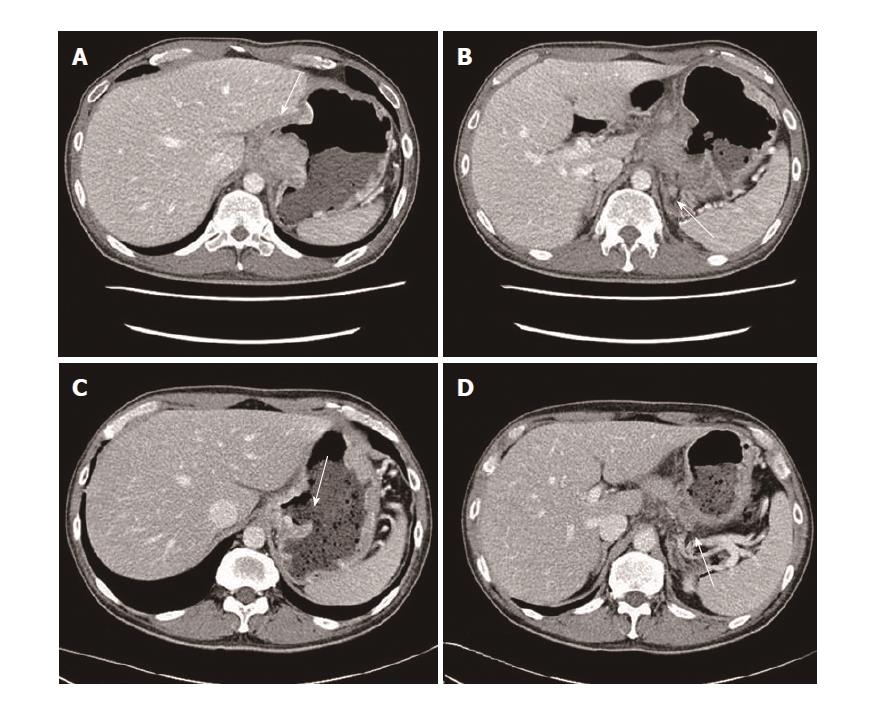
A 41-year-old Korean man was admitted with a chief complaint of epigastric pain. The patient initially underwent an endoscopy, which revealed a 4 cm sized ulcerofungating mass in the gastric cardia and CLO test (Campylobacter-like organism test; Rapid urease test) was negative. Pathologic findings revealed poorly differentiated adenocarcinoma without intestinal metaplasia and a CT scan showed a bulky ulcerative mass with direct invasion of the pancreas, and the left diaphragm. Furthermore, there were multiple perigastric and upper aortic lymph node enlargements. Based on these findings, the patient was diagnosed with Stage IIIB gastric cancer (T4N2M0) (Figure 1A and B). He had a far advanced stage of gastric cancer; therefore, the patient underwent firstly a neoadjuvant chemotherapy with capecitabine and oxaliplatin. After 3 cycles of this therapy (#1-#3), the mass had markedly decreased and a total gastrectomy with splenectomy was performed (Figure 1C and D). Since this was a stage IIIB gastric cancer [T4bN0 (0/48) M0], the patient was continued on the same regimen as adjuvant chemotherapy
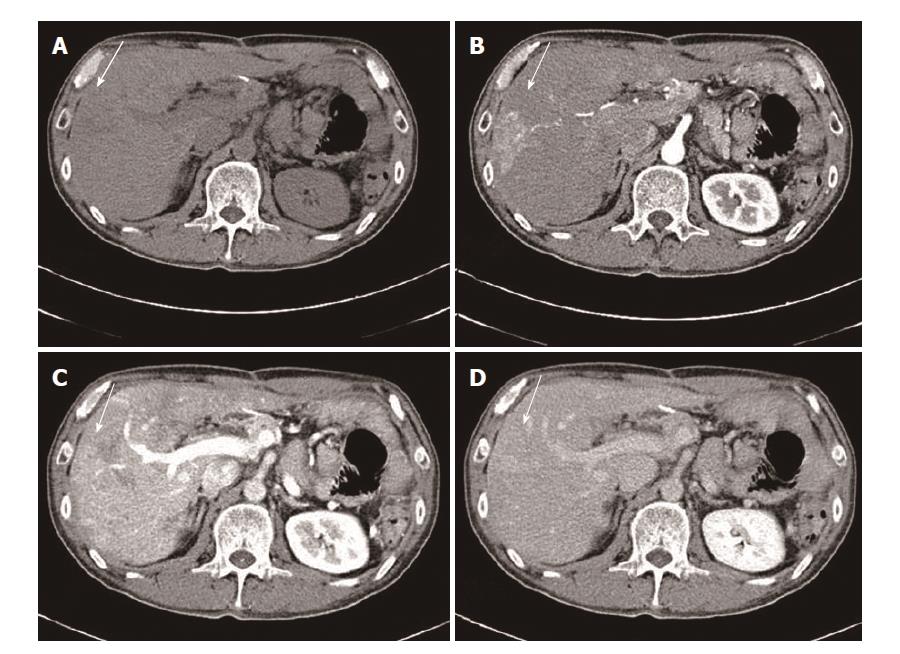
After another 3 cycles of therapy (#4-#6), a follow-up CT demonstrated an arterial enhancing mass like lesion in the peripheral portion of the right lobe of the liver (Figure 2).
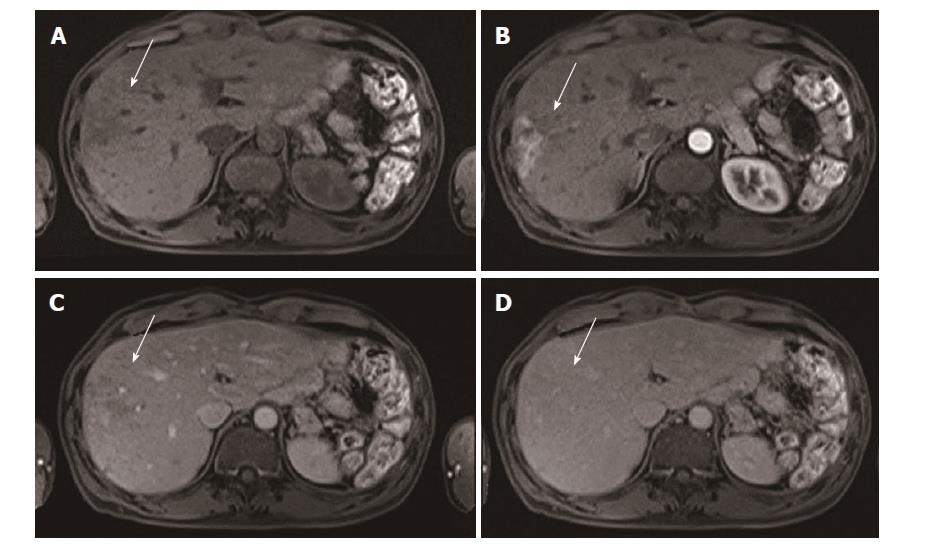
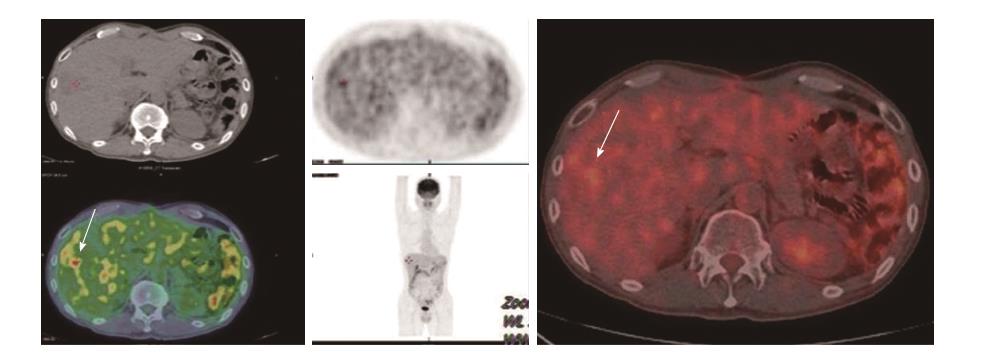
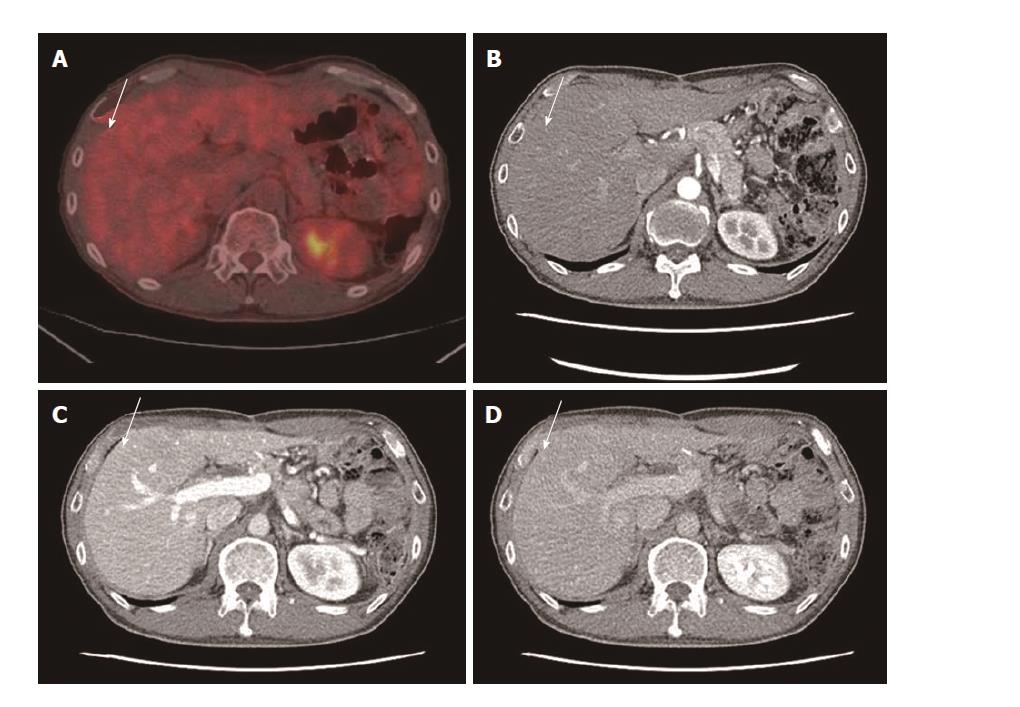
We presumed initially a new hepatocellular carcinoma or recurred gastric cancer, and we evaluated the arterial enhancing mass like lesion. He had a no history of hepatitis (hepatitis B and C) and he was social alcohol drinking. There was no proof of liver cirrhosis in CT, too. The test results showed HBsAg (-), HBsAb (+), and HCVAb (−) and tumor marker of hepatocellular carcinoma was under the normal range such as Alpha-fetoprotein (α-FP) of 2.2 ng/mL (normal; < 5 ng/mL) and protein induced by vitamin K absence-II of 23 mAU (0–39 mAU). CEA (Carcinoembryonic antigen) and CA 19-9 (carbohydrate antigen) were under the normal range, too. Various other image studies were done. An MRI showed the arterial enhancing lesion, and a PET CT scan showed a hypermetabolic lesion in that same portion of the liver (Figures 3 and 4). We tried to perform a pathological confirmation of the lesion through a liver biopsy. However, we could not obtain the tissue because no typical mass was detected on ultrasonography.
In summary, he had a no risk of hepatocellular carcinoma and normal range of tumor markers, and there was no mass in liver. He was initially far advanced stage of gastric cancer, and he was high risk subtype of recurrence. Base on the data, we assumed it might be an arterial-portal shunt in the liver. However, this phenomenon strongly indicated a recurred mass in the liver despite of no obvious proof of recurrence such as typical mass or elevated tumor marker (CEA, CA 19-9). After reviewing literature, we found a few case report of an oxaliplatin-induced liver injury, mimicking a metastatic tumor on an image, although it was a slightly different case (mainly colon cancer and different enhance pattern)[6-10].
Therefore, we continued with the adjuvant chemotherapy, this time, eliminating oxaliplatin. After 2 cycles of capecitabine monotherapy, the arterial enhancing mass in the liver disappeared (Figure 5). We were able to confirm the diagnosis of an AV shunt due to oxaliplatin-induced sinusoidal injury, the patient has not relapsed in 2 years.
A unique feature of the liver’s blood supply system is its dual blood supply, which comes from the hepatic artery (25%) and the portal vein (75%). A perfusion gradient between the artery and portal vein under various conditions such as diminished blood flow through the portal vein can result in an increased attenuation or signal intensity difference during the early phases of a contrast-enhanced dynamic imaging of the liver. In most cases, this finding reflects an increased arterial blood flow, related to an APS. APSs tend to show an amorphous or nodular appearance in the peripheral portion of the liver. There are various causes of APS: hepatic neoplasms, hepatic trauma including interventional procedure, liver cirrhosis, inflammatory diseases, obstruction of the portal or hepatic vein due to various causes, external compression such as hepatic tumor (hepatocellullar carcinoma and cholangiocarcinoma, metastatic tumor, hematoma), or an internal obstruction (tumor thrombus, invasion of cancer). There are various routes, depending on each cause. These routes are transtumoral (through the tumor itself), transversal (due to portal vein tumor thrombosis), transplexal (peribiliary vascular plexus) and transsinusoidal (between microscopic hepatic arterioles and portal venules, distal to portal vein compression or thrombosis), each of which can occur alone or in combination with each other[2-5].
However, our case was an incidental arterioportal shunt, mimicking a recurred gastric cancer, on various images (dynamic CT, MRI and PET). Actually, we are uncertain about why the arterial enhancing nodule (suspected APS) spontaneously disappeared. However, our patient had no history of liver cirrhosis, intervention of liver, or liver trauma (including trauma from surgery of the liver). Moreover, no typical mass was picked up by the sonography.
Oxaliplatin is platinum-based, and a third generation chemotherapeutic agent, administered to patients with gastric cancer, and colorectal cancer. It has comparably less toxic side effects than that of cisplatin. However, there are increasing numbers of reports indicating that oxaliplatin-based chemotherapy could cause damage to a non-tumor-bearing liver. Several reports have confirmed the association between hepatic sinusoidal injury and oxaliplatin. Oxaliplatin-induced hepatic sinusoidal injury can range from a mild sinusoidal dilatation to a hepatic sinusoidal obstruction syndrome. Clinical manifestations vary from asymptomatic to hepatomegaly, jaundice, and ascites. The oxaliplatin sinusoidal injury lesions appeared after the administration of oxaliplatin; however, most lesions disappeared after the cessation of oxaliplatin treatment[6-10].
The incidence of hepatic sinusoidal injury ranges between 19% and 54%. A retrospective study demonstrated that approximately half the patients who received preoperative chemotherapy with oxaliplatin developed some degree of hepatic sinusoidal dilation and microscopic hemorrhage related to damage to the hepatic sinusoidal endothelial cell barrier[11,12].
Oxaliplatin-induced liver damage is characterized histologically by sinusoidal dilatation and congestion outlined by atrophic hepatocyte and/or fibrosis and venular obstruction. An immunohistochemical study of cluster of differentiation 34 revealed a decrease in sinusoidal endothelial cells in this lesion. Such an injury often increases the porosity of the sinusoidal endothelium, and increases cellular fenestrations. This led to the obstruction of the sinusoids and interruption of the portal circulation, resulting in hepatic congestion and eventually elevated portal pressures. Finally, some advanced cases of oxaliplatin-induced sinusoidal injury, have induced veno-occlusive disease, sinusoidal obstruction and portal hypertension[13-15]. Among the pathogenesis of oxaliplatin-induced sinusoidal injury, hepatic congestion due to an obstruction of the sinusoids and an interruption of portal circulation is similar to APS, through a transsinusoidal route. It is thought that oxaliplatin-induced sinusoidal obliteration of peripheral hepatic venules could lead to a retrograde filling of small portal vein branches, by way of a trans-sinusoidal route[2-5].
Our patient underwent splenectomy, and there might be a question that it may affect to oxaliplatin induced sinusoidal injury. However, we couldn’t find the relationship between splenectomy and oxaliplatin-induced sinusoidal injury or APS, and splenectomy was rather as option of treatment of hypersplenism from oxaliplatin-induced sinusoidal injury[16].
In conclusion, although we had no established evidence of a relationship between oxaliplatin and incidental APS, we concluded on the diagnosis because of the following reasons: Firstly, there was no reason lead to be APS such as trauma, intervention and liver cirrhosis. Secondly, the arterial enhancing lesion appeared after the administration of oxaliplatin and disappeared after the cessation of oxaliplatin. Thirdly, although no definitive mechanism exists for our case, oxaliplatin-induced sinusoidal injury has been identified, and this is enough evidence from literature, to support our case. To the best of our knowledge, this is the first case report of arterioportal shunt incidental to treatment with oxaliplatin that mimics recurrent gastric cancer upon interpretation of multiple imaging modalities.
After adjuvant chemotherapy with capecitabine and oxaliplatin in stage IIIb gastric cancer, a computed tomography revealed a 1 cm sized arterial-enhancing nodule in the liver.
The authors presumed initially a new hepatocellular carcinoma or recurred gastric cancer.
Hepatocellular carcinoma, recurred gastric cancer, arterioportal shunt.
Various tumor marker were under the normal range.
Various imaging including dynamic computed tomography (CT), magnetic resonance imaging, and Positron emission tomography-CT showed an arterioportal shunt.
The authors could not obtain the tissue because no typical mass was detected on ultrasonography.
The patient was continued on treatment with adjuvant chemotherapy following discontinuation of oxaliplatin.
There was no report of non-tumorous incidental Arterioportal shunt (APS) related to treatment with oxaliplatin.
APS is an organic communication between the hepatic arterial system and the portal venous system.
The authors want to share this case as rare condition of arterioportal shunt due to oxaliplatin induced sinusoidal injury.
This is the first case report of arterioportal shunt incidental to treatment with oxaliplatin that mimics recurrent gastric cancer upon interpretation of multiple imaging modalities
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: South Korea
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Koch TR, Nakano H, Tziomalos K S- Editor: Qi Y L- Editor: A E- Editor: Huang Y
| 1. | Colagrande S, Centi N, Galdiero R, Ragozzino A. Transient hepatic intensity differences: part 1, Those associated with focal lesions. AJR Am J Roentgenol. 2007;188:154-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 42] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Choi BI, Lee KH, Han JK, Lee JM. Hepatic arterioportal shunts: dynamic CT and MR features. Korean J Radiol. 2002;3:1-15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 102] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 3. | Ahn JH, Yu JS, Hwang SH, Chung JJ, Kim JH, Kim KW. Nontumorous arterioportal shunts in the liver: CT and MRI findings considering mechanisms and fate. Eur Radiol. 2010;20:385-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 45] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Matsuo M, Kanematsu M, Kondo H, Maeda S, Goshima S, Suenaga I, Hoshi H. Arterioportal shunts mimicking hepatic tumors with hyperintensity on T2-weighted MR images. J Magn Reson Imaging. 2002;15:330-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Tian JL, Zhang JS. Hepatic perfusion disorders: etiopathogenesis and related diseases. World J Gastroenterol. 2006;12:3265-3270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in CrossRef: 15] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Uchino K, Fujisawa M, Watanabe T, Endo Y, Nobuhisa T, Matsumoto Y, Kai K, Sato S, Notohara K, Matsukawa A. Oxaliplatin-induced liver injury mimicking metastatic tumor on images: a case report. Jpn J Clin Oncol. 2013;43:1034-1038. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Choi JH, Won YW, Kim HS, Oh YH, Lim S, Kim HJ. Oxaliplatin-induced sinusoidal obstruction syndrome mimicking metastatic colon cancer in the liver. Oncol Lett. 2016;11:2861-2864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Arakawa Y, Shimada M, Utsunomya T, Imura S, Morine Y, Ikemoto T, Hanaoka J, Sugimoto K, Bando Y. Oxaliplatin-related sinusoidal obstruction syndrome mimicking metastatic liver tumors. Hepatol Res. 2013;43:685-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Lawal TO, Farris AB, El-Rayes BF, Subramanian RM, Kim HS. Oxaliplatin-induced hepatoportal sclerosis, portal hypertension, and variceal bleeding successfully treated with transjugular intrahepatic portosystemic shunt. Clin Colorectal Cancer. 2012;11:224-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Slade JH, Alattar ML, Fogelman DR, Overman MJ, Agarwal A, Maru DM, Coulson RL, Charnsangavej C, Vauthey JN, Wolff RA. Portal hypertension associated with oxaliplatin administration: clinical manifestations of hepatic sinusoidal injury. Clin Colorectal Cancer. 2009;8:225-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 83] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 11. | Vauthey JN, Pawlik TM, Ribero D, Wu TT, Zorzi D, Hoff PM, Xiong HQ, Eng C, Lauwers GY, Mino-Kenudson M. Chemotherapy regimen predicts steatohepatitis and an increase in 90-day mortality after surgery for hepatic colorectal metastases. J Clin Oncol. 2006;24:2065-2072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 970] [Cited by in RCA: 951] [Article Influence: 50.1] [Reference Citation Analysis (0)] |
| 12. | Rubbia-Brandt L, Lauwers GY, Wang H, Majno PE, Tanabe K, Zhu AX, Brezault C, Soubrane O, Abdalla EK, Vauthey JN. Sinusoidal obstruction syndrome and nodular regenerative hyperplasia are frequent oxaliplatin-associated liver lesions and partially prevented by bevacizumab in patients with hepatic colorectal metastasis. Histopathology. 2010;56:430-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 223] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 13. | Robinson SM, Mann J, Vasilaki A, Mathers J, Burt AD, Oakley F, White SA, Mann DA. Pathogenesis of FOLFOX induced sinusoidal obstruction syndrome in a murine chemotherapy model. J Hepatol. 2013;59:318-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 95] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 14. | Yeong ML, Wakefield SJ, Ford HC. Hepatocyte membrane injury and bleb formation following low dose comfrey toxicity in rats. Int J Exp Pathol. 1993;74:211-217. [PubMed] |
| 15. | Ryan P, Nanji S, Pollett A, Moore M, Moulton CA, Gallinger S, Guindi M. Chemotherapy-induced liver injury in metastatic colorectal cancer: semiquantitative histologic analysis of 334 resected liver specimens shows that vascular injury but not steatohepatitis is associated with preoperative chemotherapy. Am J Surg Pathol. 2010;34:784-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 74] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 16. | Litvak DA, Malad S, Wascher RA, Markman M, Niu J. Laparoscopic Splenectomy in Colorectal Cancer Patients with Chemotherapy-Associated Thrombocytopenia due to Hypersplenism. Case Rep Oncol. 2012;5:601-607. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |