Published online Aug 28, 2017. doi: 10.3748/wjg.v23.i32.6003
Peer-review started: March 28, 2017
First decision: April 10, 2017
Revised: July 2, 2017
Accepted: July 22, 2017
Article in press: July 24, 2017
Published online: August 28, 2017
Processing time: 153 Days and 10.9 Hours
Portal vein thrombosis (PVT) is a rare but serious postoperative complication associated with irreversible electroporation (IRE). We report a case of postoperative PVT in a 54-year-old woman who underwent IRE for locally advanced pancreatic cancer. Drain removal and discharge of the patient from the hospital were scheduled on postoperative day (POD) 7; however, a magnetic resonance imaging scan revealed the presence of PVT. We suspected postoperative inflammation in the pancreas as the main cause of PVT. However, the patient did not undergo any medical treatment because she did not have any clinical symptoms, and she was discharged on POD 8.
Core tip: Irreversible electroporation (IRE) is a medical technique that utilizes high voltage pulses to create permanent nanopores in the cell membrane, which in turn induces apoptosis of the targeted cells. Portal vein thrombosis (PVT) is a rare but serious postoperative complication associated with IRE. This review focuses on the mechanism of PVT after IRE for locally advanced pancreatic cancer.
- Citation: Su JJ, Su M, Xu K, Wang PF, Yan L, Lu SC, Gu WQ, Chen YL. Postoperative inflammation as a possible cause of portal vein thrombosis after irreversible electroporation for locally advanced pancreatic cancer. World J Gastroenterol 2017; 23(32): 6003-6006
- URL: https://www.wjgnet.com/1007-9327/full/v23/i32/6003.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i32.6003
Irreversible electroporation (IRE) is a medical technique that utilizes high voltage pulses to create permanent nanopores in the cell membrane, which in turn induces apoptosis of the targeted cells[1-4]. The main advantage of IRE over other approaches is the avoidance of thermal injury to the surrounding structures, thereby sparing essential structures such as the nerves, vessels, and bile ducts[5-8]. Although there are benefits of IRE, many adverse events should be taken into consideration before its use, including mild hypertension and hemodynamically relevant arrhythmia. Initial long-term survival data in animals have confirmed the safety of IRE as it does not show vascular thrombosis as a related complication[9,10]. We report a case of successful IRE in a patient with locally advanced pancreatic cancer who developed PVT shortly after IRE.
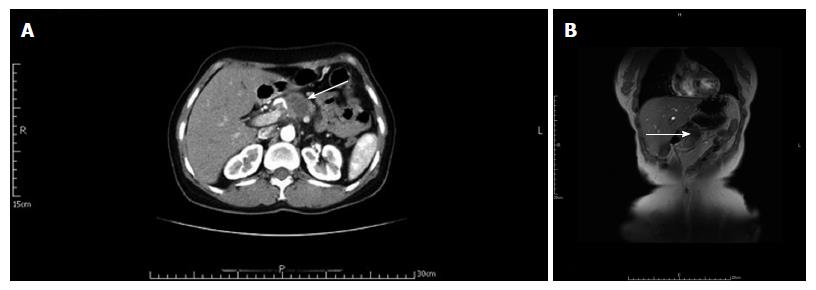
We report the case of a 54-year-old woman who was diagnosed with tumor in the body of the pancreas, using computed tomography (CT). Magnetic resonance imaging (MRI) of the abdomen also revealed a tumor mass located at the pancreatic body; hence, pancreatic cancer was suspected. Artery invasion was seen near the celiac axis (Figure 1).
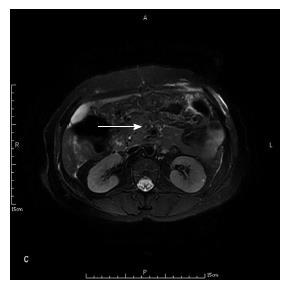
The patient underwent abdominal vascular ultrasonographic scanning of the hepatic vein, inferior vena cava, superior mesenteric vein, splenic vein, and portal vein, which showed that the blood flow was unobstructed prior to the surgery. The blood flow volume of the splenic vein was 14.5 cm/s and that of the superior mesenteric vein was 18.8 cm/s. The diameter of the portal vein was 1.1 cm and its blood flow volume was 28.8 cm/s. The patient underwent IRE ablation under balanced general anesthesia for pancreatic cancer because the tumor mass was considered unresectable because of tumor infiltration of the celiac axis root and major abdominal blood vessels. Furthermore, multiple metastases were established in the lymph nodes of different regions. Before the IRE ablation, we performed tumor mass biopsies. The patient was admitted to the hospital after routine blood tests, which showed normal levels of leukocytes, neutrophils, erythrocytes, leukocytes, platelets, and amylase. These levels increased on postoperative day (POD) 2. The levels of C-reactive protein (CRP), interleukin-6 (IL-6), interleukin-8 (IL-8), and tumor necrosis factor (TNF) were also increased on POD 2. The amylase level of the drain from the IRE was 922.8 U/L on POD 3, which was 6 times higher than the upper limit of the normal serum amylase level, indicating the presence of postoperative pancreatic fistula according to the International Study Group on Pancreatic Fistula classification[11]. The drain amylase level reached the normal serum range on POD 5 and after the drain removal. The levels of cancer antigen 199 in the serum were decreased after the surgery. The re-evaluation MRI scan following the IRE ablation demonstrated thrombosis of the portal vein trunk on POD 7 and revealed that the tumor size had decreased (Figure 2).
Non-occlusive PVT did not affect the patient’s general condition, and the patient was discharged from the hospital on POD 8 because she showed no other complications. The patient currently has good quality of life.
There is no effective treatment available for patients with pancreatic cancer. Therefore, we put forward a novel method of minimally invasive IRE for the treatment of pancreatic tumors, which was reported recently in 2008. Although IRE is now regarded as an attractive treatment option for locally advanced pancreatic cancer, there are some complications associated with the use of this method. PVT is a rare but serious postoperative complication of IRE[12]. Although the mechanism is still unclear[13], medical literature on the occurrence of PVT reports that it is associated with three factors: endothelial cell injury, slow blood flow, and hypercoagulable state of the blood. In pancreatitis, various inflammatory mediators are released with concomitant thrombosis, resulting in high levels of IL-6, IL-8, and TNF. These factors stimulate the hepatic cells, which in turn produce large quantities of CRP. CRP is a sensitive indicator of the severity of inflammation. The initial clinical signs of PVT are often subtle and similar to those observed in postoperative pancreatitis. PVT can be detected using CT, MRI, and Doppler ultrasonography. Doppler ultrasonography is a non-invasive, easily available bedside examination with an 89% sensitivity and 92% specificity in detecting PVT[14]. Early diagnosis of PVT might provide clinicians an opportunity for intervention before severe damage occurs. Once the thrombus is formed, thrombolysis and anticoagulation must be performed as soon as possible, including surgical treatment if necessary. In this case, the patient developed PVT, which did not completely block the portal vein. No clinical symptoms such as abdominal pain and portal hypertension were observed; hence, anticoagulant was not administered. However, the case was closely followed. The patient was administered no special medical treatment during the follow-up period because she recovered from acute pancreatitis and showed no signs of thrombus. In this case, the levels of prothrombin time, activated partial thromboplastin time, fibrinogen, and thrombin time were normal before the operation. But after surgery, the patient developed abnormal blood coagulation and significantly increased white blood cells, CRP, IL-6, IL-8, and TNF, which explains that PTV occurred due to abdominal surgery.
A 54-year-old woman was referred to our hospital because of a tumor in the body of the pancreas found by physical examination.
The abdomen was soft, lax, and nondistended without evidence of a palpable mass.
Abdominal sarcoma, abdominal neurogenic tumor, and cholangiocarcinoma.
Before surgery, laboratory results were normal.
Computed tomography scan showed a locally advanced malignant pancreatic mass of 34 mm in diameter that surrounded and narrowed the coeliac trunk. MRI demonstrated the mass located in the pancreatic body.
The tumor was diagnosed as a low differentiated adenocarcinoma in the pancreas.
The patient underwent irreversible electroporation (IRE) for locally advanced pancreatic cancer.
Portal vein thrombosis (PVT) is a rare but serious postoperative complication associated with IRE. To date, only a few cases have been reported in the English literature, including our case presented in this report.
PVT is a rare but serious postoperative complication associated with IRE. A patient with locally advanced pancreatic cancer who developed PVT shortly after IRE makes us suspect postoperative inflammation in the pancreas as the main cause of PVT.
This study highlights the mechanism of PVT after IRE in locally advanced pancreatic cancer and the authors also conducted a literature review so as to deepen the understanding of the subject. The information of this paper is valuable to the readers.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Dokus MK, Thiele M S- Editor: Qi Y L- Editor: Wang TQ E- Editor: Zhang FF
| 1. | Al-Sakere B, André F, Bernat C, Connault E, Opolon P, Davalos RV, Rubinsky B, Mir LM. Tumor ablation with irreversible electroporation. PLoS One. 2007;2:e1135. [PubMed] [DOI] [Full Text] |
| 2. | Edd JF, Horowitz L, Davalos RV, Mir LM, Rubinsky B. In vivo results of a new focal tissue ablation technique: irreversible electroporation. IEEE Trans Biomed Eng. 2006;53:1409-1415. [PubMed] [DOI] [Full Text] |
| 3. | Davalos RV, Mir IL, Rubinsky B. Tissue ablation with irreversible electroporation. Ann Biomed Eng. 2005;33:223-231. [PubMed] |
| 4. | Davalos RV, Otten DM, Mir LM, Rubinsky B. Electrical impedance tomography for imaging tissue electroporation. IEEE Trans Biomed Eng. 2004;51:761-767. [PubMed] [DOI] [Full Text] |
| 5. | Jiang C, Davalos RV, Bischof JC. A review of basic to clinical studies of irreversible electroporation therapy. IEEE Trans Biomed Eng. 2015;62:4-20. [PubMed] [DOI] [Full Text] |
| 6. | Dollinger M, Zeman F, Niessen C, Lang SA, Beyer LP, Müller M, Stroszczynski C, Wiggermann P. Bile Duct Injury after Irreversible Electroporation of Hepatic Malignancies: Evaluation of MR Imaging Findings and Laboratory Values. J Vasc Interv Radiol. 2016;27:96-103. [PubMed] [DOI] [Full Text] |
| 7. | Choi JW, Lu DS, Osuagwu F, Raman S, Lassman C. Assessment of chronological effects of irreversible electroporation on hilar bile ducts in a porcine model. Cardiovasc Intervent Radiol. 2014;37:224-230. [PubMed] [DOI] [Full Text] |
| 8. | Cannon R, Ellis S, Hayes D, Narayanan G, Martin RC 2nd. Safety and early efficacy of irreversible electroporation for hepatic tumors in proximity to vital structures. J Surg Oncol. 2013;107:544-549. [PubMed] [DOI] [Full Text] |
| 9. | Bower M, Sherwood L, Li Y, Martin R. Irreversible electroporation of the pancreas: definitive local therapy without systemic effects. J Surg Oncol. 2011;104:22-28. [PubMed] [DOI] [Full Text] |
| 10. | Charpentier KP, Wolf F, Noble L, Winn B, Resnick M, Dupuy DE. Irreversible electroporation of the pancreas in swine: a pilot study. HPB (Oxford). 2010;12:348-351. [PubMed] [DOI] [Full Text] |
| 11. | Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M; International Study Group on Pancreatic Fistula Definition. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8-13. [PubMed] [DOI] [Full Text] |
| 12. | Yan L, Chen YL, Su M, Liu T, Xu K, Liang F, Gu WQ, Lu SC. A Single-institution Experience with Open Irreversible Electroporation for Locally Advanced Pancreatic Carcinoma. Chin Med J (Engl). 2016;129:2920-2925. [PubMed] [DOI] [Full Text] |
| 13. | Paiella S, Butturini G, Frigerio I, Salvia R, Armatura G, Bacchion M, Fontana M, D’Onofrio M, Martone E, Bassi C. Safety and feasibility of Irreversible Electroporation (IRE) in patients with locally advanced pancreatic cancer: results of a prospective study. Dig Surg. 2015;32:90-97. [PubMed] [DOI] [Full Text] |
| 14. | Tessler FN, Gehring BJ, Gomes AS, Perrella RR, Ragavendra N, Busuttil RW, Grant EG. Diagnosis of portal vein thrombosis: value of color Doppler imaging. AJR Am J Roentgenol. 1991;157:293-296. [PubMed] [DOI] [Full Text] |