Published online Aug 28, 2017. doi: 10.3748/wjg.v23.i32.5849
Peer-review started: May 16, 2017
First decision: June 5, 2017
Revised: July 25, 2017
Accepted: August 1, 2017
Article in press: August 2, 2017
Published online: August 28, 2017
Processing time: 107 Days and 22 Hours
Acute appendicitis (AA) develops in a progressive and irreversible manner, even if the clinical course of AA can be temporarily modified by intentional medications. Reliable and real-time diagnosis of AA can be made based on findings of the white blood cell count and enhanced computed tomography. Emergent laparoscopic appendectomy (LA) is considered as the first therapeutic choice for AA. Interval/delayed appendectomy at 6-12 wk after disease onset is considered as unsafe with a high recurrent rate during the waiting time. However, this technique may have some advantages for avoiding unnecessary extended resection in patients with an appendiceal mass. Non-operative management of AA may be tolerated only in children. Postoperative complications increase according to the patient’s factors, and temporal avoidance of emergent general anesthesia may be beneficial for high-risk patients. The surgeon’s skill and cooperation of the hospital are important for successful LA. Delaying appendectomy for less than 24 h from diagnosis is safe. Additionally, a semi-elective manner (i.e., LA within 24 h after onset of symptoms) may be paradoxically acceptable, according to the factors of the patient, physician, and institution. Prompt LA is mandatory for AA. Fortunately, the Japanese government uses a universal health insurance system, which covers LA.
Core tip: Acute appendicitis develops in a progressive and irreversible manner, and emergent laparoscopic appendectomy (LA) is mandatory. The Japanese government uses a universal health insurance system. Any physician and institution can routinely perform expensive emergent LA in Japan, in accordance with medical ethics. Unsafe, but cost-effective, treatments such as interval/delayed appendectomy and conservative management only are unsuitable in Japan. Time-honored practices, (i.e., emergent LA) should be respected in Japan.
- Citation: Hori T, Machimoto T, Kadokawa Y, Hata T, Ito T, Kato S, Yasukawa D, Aisu Y, Kimura Y, Sasaki M, Takamatsu Y, Kitano T, Hisamori S, Yoshimura T. Laparoscopic appendectomy for acute appendicitis: How to discourage surgeons using inadequate therapy. World J Gastroenterol 2017; 23(32): 5849-5859
- URL: https://www.wjgnet.com/1007-9327/full/v23/i32/5849.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i32.5849
Acute appendicitis (AA) is a clinical diagnosis[1,2]. The first appendectomy was performed in New York in 1886[1], and thereafter, appendectomy was considered the most common emergency surgery[2-4]. Prompt appendectomy has long been the standard of care for AA because of the risk of progression to advanced pathophysiology[3].
Currently, laparoscopic appendectomy (LA) is available as the first therapeutic choice for AA[1,3]. However, surgeons on call when a patient is admitted is an important factor for determining whether a patient can receive an advantageous LA or conventional open surgery[5]. Additionally, a poor clinical course in a hospital with an unfavorable combination for emergent laparoscopic surgery is a critical matter[3,6]. In brief, factors of hospitals and physicians affect the severity of AA[3,5-7].
A 24-h surgical shift in a quadratic/tertiary care hospital is stressful for surgeons[8]. Emergent surgeries during overtime service and off-days result in higher rates of morbidity and mortality[9,10]. However, AA indicates a surgical emergency.
AA may be managed in an elective manner once antibiotic therapy is initiated[2,11-14]. Initial non-operative management followed by interval and/or delayed appendectomy for AA has been challenged, especially in pediatric patients[3]. However, the necessity and validity of an interval/delayed appendectomy is still controversial in adult patients[2,3,11-18], though some researchers believed that interval/delayed appendectomy has some advantages only for treatment of appendiceal mass[12,14].
We review major controversy in management of AA based on previous studies, and discuss what practice is the best option for patients with AA.
The exact mechanism of AA is still unclear, but is believed to be multifactorial. Inadequate dietary fiber, familial factors, and luminal obstruction from fecalith impaction or lymphoid hyperplasia, and other processes, such as parasitic infestation, may be involved[19-22]. Luminal obstruction by external (i.e., lymphoid hyperplasia) or internal (i.e., inspissated fecal material and appendicoliths) compression plays a major pathophysiological role[3]. This subsequently leads to increased mucus production, bacterial overgrowth, viral infection, and stasis, which increase appendiceal wall tension[3,19-24]. Consequently, blood and lymph flow is diminished, and necrosis and perforation follow[3]. Because these events occur over time, only an early surgical approach might prevent progression of disease[3,4]. The immunological orchestra around the ileocecal portion is well developed and complicated, and the appendix has its own immunological features[25-28]. Many major immunological and cellular function-associated gene sets involved in the protective effect of AA followed by appendectomy in experimental colitis have been identified[25].
Once disease is triggered, AA develops in a progressive and irreversible manner[3,4,29]. Even a histologically normal appendix clearly shows evidence of inflammatory responses against AA, as shown by cytokine production/expression[29].
An appendiceal mass (tumor formation after perforating AA) is the end result of a walled-off appendiceal perforation[2,16]. Pathologically, this mass may range from phlegmon to abscess[16]. A pus-containing mass is an inflammatory tumor consisting of an inflamed appendix, its adjacent viscera, and the greater omentum[16].
In AA, tumor necrosis factor-α is at the top of the pathway[29,30], and interferon-γ and interleukin-6 play an important role[30,31]. Fas-mediated induction of apoptosis is a major factor in selection of lymphocytes and downregulation of immunological processes, and endothelial Fas-ligand expression is elevated in AA[26]. AA develops in a progressive and irreversible pathway[2,16], even if the clinical course of AA can be temporarily modified by intentional medications[32].
Physical findings of AA are well established[33]. Many researchers, such as Charles McBurney, Niels Thorkild Rovsing, Jacob Moritz Blumberg, Otto Lanz, Frederic Treves, and others were involved in the initial study of AA[1,34]. Most patients present early in the disease process[2], although, in 2%-6% of patients, diagnosis is made when an appendiceal mass is discovered on preoperative imaging[16,35]. Young female patients have the highest risk of being falsely diagnosed with AA and thus have unnecessary surgery[36].
Computed tomography (CT) is more reliable for diagnosis than an ultrasound examination[37,38], and enhanced CT should be routinely performed for suspected appendicitis[39]. Enhanced CT scans have become the main diagnostic tool for patients with AA and have a high sensitivity and specificity[39]. Briefly, enhanced CT is a powerful tool for a strict diagnosis and assessment of the degree of inflammation[15,36,37,39-42], and enhanced CT is superior to a physician’s clinical examination[36,37,39,40]. A helical CT image study should be performed with contrast enhancement, even with lower doses[37,43]. Routine CT for suspected appendicitis improves patients’ care, shortens the duration to surgery, and reduces the use of hospital resources and overall admission costs[39].
Laboratory data show that serum levels of the white blood cell (WBC), C-reactive protein (CRP), and interleukin-6 are related to AA[44-46]. The most reliable marker is neither the neutrophil count nor CRP, but the WBC count[1,44].
The WBC count and CT findings equally provide surgeons with complementary information in discerning the necessity for an urgent operation[36,44,47]. With development of WBC measurement and enhanced CT imaging, the rate of negative appendectomy has decreased to as low as < 5%[1,36,40,48].
LA was reported in 1983[49]. Thereafter, some advantages of LA, such as less pain, fine cosmetics, shorter hospital stay, faster recovery, less wound infection, and lower cost, compared with conventional open surgery were shown from the 1990s[50-63]. Postoperative complications are also lower in LA than in conventional open surgery[56,64-66]. Therefore, LA has spread to become the standard surgery worldwide[1,15,50,62,65-67]. Although the operative time, including buried sutures, may be longer in LA[50-52,55], there are no significant differences in the rate of severe morbidity/mortality between open and laparoscopic appendectomies[68]. Currently, natural orifice transluminal endoscopic surgery is also considered as safe and feasible[69,70].
Many physicians have an interest in the duration from onset of symptoms to surgery. In adult patients with AA, the risk of developing advanced pathophysiology and postoperative complications increases with time[3,4]. However, there is the minority opinion that the duration from surgical admission to induction of anesthesia is not predictive in regression models for overall morbidity or serious morbidity/mortality[71].
Interval/delayed appendectomy is considered as unsafe[3], although the term of “interval appendectomy” can be used only in case of appendiceal mass and performed after 6-12 wk of the beginning of disease[1,12,14]. Any delays in seeking medical help results in difficulty in controlling AA, and prompt appendectomy is mandatory[3,4]. Interval/delayed appendectomy may not increase the risk of perforation and moderate/severe complications[1,71,72], but is significantly associated with an increased risk of surgical site infection (SSI) in patients with nonperforated appendicitis and prolongation of the hospital stay[71,73]. Prompt surgical intervention is warranted to avoid additional morbidity in this population[73].
Transferred patients are less likely to be ruptured, primarily because they present earlier[72]. Morbidity is not increased in patients who have appendectomy that is delayed for up to 24 h[1]. Delaying an appendectomy for longer than 6 hours, but less than 24 h, from diagnosis is safe and does not lead to worse outcomes[74]. This can help limit disruption to the schedules of the surgeon and the operating room[74]. Paradoxically, AA that is approached in a semi-elective manner (i.e., LA within 24 h after symptom onset) may be acceptable, according to the factors of physicians and hospitals[1,3,5-7,74].
A physician’s delay in avoiding negative appendectomy does not affect the stage of disease[7]. A surgeon’s decision to observe patients in hospital to clarify the diagnosis is justified[7], as it does not adversely affect the outcome[7].
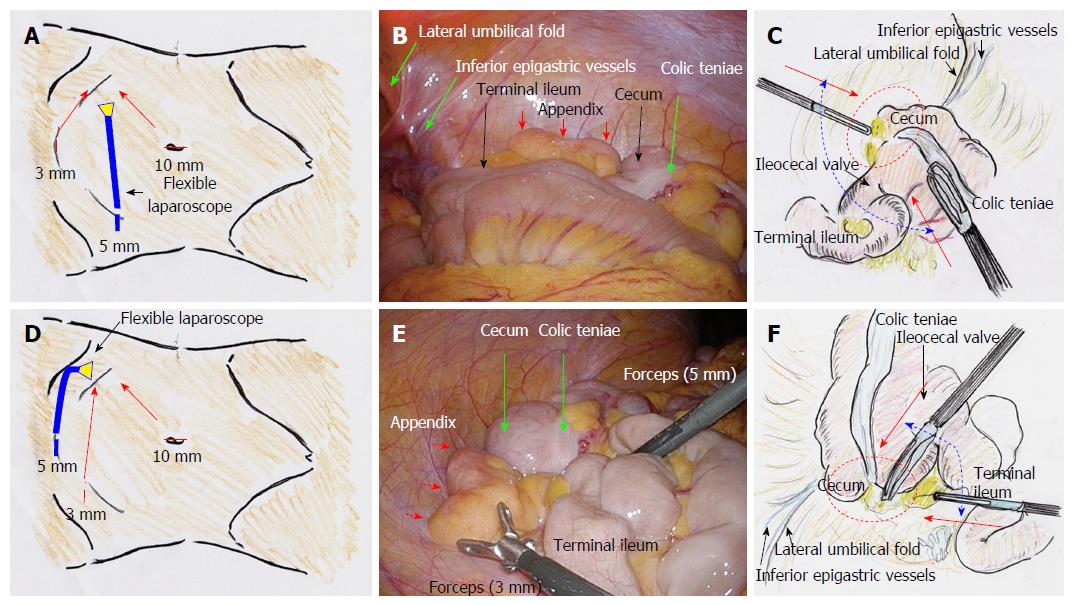
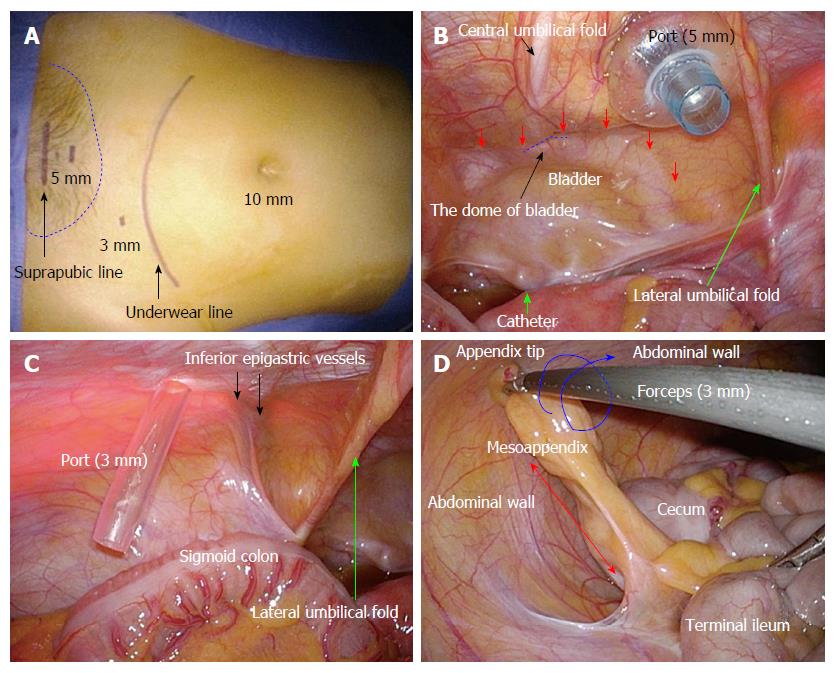
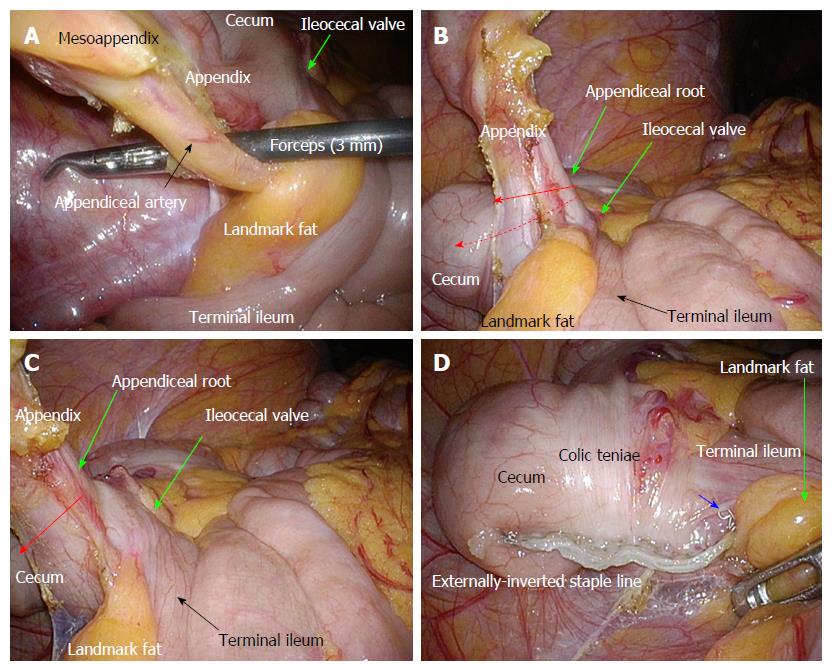
Actual procedures of LA are shown in detail in Figures 1-3. Gastric and bladder catheters are placed only during surgeries for decompression to avoid unexpected injuries[1].
Stump appendicitis is a critical result of an incomplete surgery[75], and management of the base of the appendix during LA is important. Surgeons need to decide the best management of the base of the appendix; choices include a clip, ligate, or staple. A flexible endostaple has some advantages in application of LA for day surgery and extended resection to the cecum[76-79]. However, an endostaple (Tri-staple camel 45 mm and iDrive; Medtronic, Minneapolis, MN, United States) may be excessive in quality and have a higher cost than a ligation tool (Endoloop; Ethicon, Cincinnati, OH, United States) or clip closure[80]. If there is any concern about the stump, a couple of interrupted seromuscular sutures can be added, although the suture technique is technically demanding[80].
Surgeons should be aware of a potentially higher incidence of intraabdominal abscess formation following LA[68,81,82]. Use of endobags (Rüsch MemoBag; Teleflex, Wayne, PA, United States), inversion of the appendiceal stump, and carefully conducted local irrigation of the abdomen in the supine position may reduce the incidence of abscess formation[81]. Peritoneal lavage during surgery is an effective, safe, and simple treatment for generalized peritonitis[83]. Irrigation of the abdominal cavity with more than 10 L of saline should be performed[84,85], and a cut-off level of saline volume to prevent intraabdominal abscess formation after surgery is 12 L[83]. Do not hesitate to place a drain. A drain pathway through the abdominal wall is adequately made at the right abdomen, to prevent a drain dislocation.
Primary closure is currently accepted, even in complicated appendicitis with a dirty abdominal wound[86-88]. However, delayed closure, which can occur several days after surgery, can lead to a decrease in SSI, a shorter hospital stay, and lower cost[89,90]. LA has an advantage of a lower rate of SSI, even in complicated appendicitis[82,91-93].
Video game playing, such as Nintendo Wii (Nintendo Co., Ltd., Kyoto, Japan) and Playstation 2 (Sony Interactive Entertainment Inc., Tokyo, Japan)[94-101], and laparoscopic performance skill are well associated. Therefore, the younger generation may be suitable for performing laparoscopic surgery[94-101]. LA performed by residents under the guidance of a staff surgeon is safe and feasible[102,103]. Operative time and postoperative complications can be reduced with increasing experience of a resident[104]. Incidental appendectomy during conventional open surgery is also important to educate young surgeons[105].
Some physicians consider that management of AA remains controversial[2,42]. An appendiceal mass is a misery form of perforated AA[2,16]. Initial conservative management of an appendiceal mass was first advocated in 1901 as a solution[106]. Interval/delayed appendectomy is performed electively after initial non-operative management[2,11-14], but has been questioned by a growing amount of evidence[2,11-18,107,108].
The recurrence rate of AA during the waiting time for interval/delayed appendectomy is 6%-37%[13-15,109-114], and the complication rate of surgery for recurrent AA is also not low (3%-23%)[11,107,109,115-117]. Advocates of interval/delayed appendectomy believe that the recurrence of AA is low, even though the actual rate is high, during the waiting period[3,13-15,109-114]. Interval/delayed appendectomy is routinely performed at 6-12 wk, mainly because of fear of recurrent appendicitis or because of concerns about the presence of malignancy[12,14,118,119].
Especially in a phlegmon or appendiceal mass, interval/delayed appendectomy may have some advantages. These advantages include providing a definite diagnosis, to rule out any underlying masquerading malignancy and to avoid an unnecessary extended resection[12,14,108,118-121].
This review shows that the severity of pathophysiology and the complication rate in adult patients with AA are time-dependent[3], and thus suggests that delaying appendectomy is unsafe[3,4].
Mortality due to AA is difficult to observe[3,76], and the mortality rate after appendectomy is nearly zero[76]. However, the rates of morbidity and mortality are clearly increased in older patients, male patients, and patients with steroid use, baseline disease, active pneumonitis, and a bleeding tendency[3,56,122]. Perioperative injection of antibiotics should be considered to reduce complications, including SSI[1,123,124]. Postoperative complications are also lower in LA than in conventional open surgery[56,64,65].
Notably, non-operative management has a cost advantage over routine interval/delayed appendectomy after initial successful conservative management[2]. Patients who recover from conservative treatment of an appendiceal mass should undergo colonoscopy or barium enema to detect any underlying diseases and to rule out coexistent colorectal cancer[12,14,108,118-121].
Laparoscopic surgery by experienced surgeons is a safe and feasible first-line treatment for appendiceal abscess[32,67]. Additionally, laparoscopic surgery is associated with fewer readmissions and fewer additional interventions than conservative treatment with a comparable hospital stay[67]. However, non-operative management is well tolerated and efficacious in select populations, especially in children[125-127]. Some patients who initially receive conservative treatments do not require surgical intervention[13,17,107,120,128], and AA should no longer be regarded as an indication for interval/delayed appendectomy[13,17,107,120,128,129]. Routine interval/delayed appendectomy benefits less than 20% of patients[14]. The majority of recurrence occurs in the first 6 mo[14,109-112], but the rate decreases to approximately 2% at 1 year[107,112,118]. Importantly, AA develops in a progressive and irreversible pathway[2,16], even if the clinical course of AA can be temporarily modified by intentional antibiotics[32]. The length of hospital stay and postoperative complications increase with advanced pathology during antibiotic treatment[3].
A gradual, adapted antibiotherapy in non-operative management of an appendiceal abscess and mass is effective[130]. There is no relevant predictive factor of failure of first-line antibiotics[130]. Monotherapy with a second-generation, broad-spectrum cephalosporin, such as cefotetan, administered twice a day, is an economical and effective adjunctive regimen[38]. A third-generation cephalosporin can be used[15], but is not recommended yet[131].
Some situations of patients are especially listed in surgical indications, such as older people, pregnancy, and negative appendectomy[1,48,129]. Although LA in pregnant women has been already reported, fetal loss and negative appendectomy should be avoided in this population[132,133]. The available low-grade evidence suggests that LA in pregnant women is associated with a greater risk of fetal loss[132,134]. Appendectomy and early appendicitis are associated with increased pregnancy rates[135]. Young women with early appendicitis have better pregnancy rates than those with advanced appendicitis. Early referral for laparoscopy and appendectomy is advocated[135]. Appendiceal tumors may be incidentally detected[136,137].
The cost effectiveness of LA has been reported[57]. Non-operative management without LA is the least costly[138]. Non-operative management has a cost advantage over routine interval appendectomy after initial successful conservative management[2].
Despite liberal use of disposable equipment, LA can still be performed within the confines of the national tariffs[139]. There is considerable variation in the cost of this procedure, and it may be possible to reduce costs by more stringent use of disposable equipment and standardizing recovery protocols[139].
Clinically, many surgeons believe that LA is an appropriate treatment[76]. However, LA requires general anesthesia, although LA under combined spinal-epidural or local anesthesia is currently being attempted[140,141]. LA in a semi-elective manner (within 24 h after onset of symptoms) may be beneficial for avoiding uncomfortable situations for anesthetic induction, such as a full stomach and dehydration[142,143]. However, even in a high-volume center, unfavorable combinations, such as low activity of the operation room during night time, affects the clinical course of AA[6]. Overall, LA in a semi-elective manner may be acceptable.
Each country has its own health insurance system. The Japanese government uses a universal health insurance system. Therefore, expensive imaging studies and emergent surgery can easily be performed in Japan. However, expensive studies and therapeutic options may be uncertain in the United States and Europe[144,145]. Novel procedures in Japan are not authorized until they are included in the health insurance system’s listing by the governmental council[146]. Paradoxically, if a surgery is once listed in Japanese health insurance system, any physician and institution can routinely perform it, even an expensive emergent surgery, in accordance with medical ethics. We have to consider how to dismantle interval/delayed appendectomy and antibiotics alone, in Japan.
Diagnostic methodology and subsequent management pathway have been already established[147]. The LA under the hands or directions of experienced surgeons is safe and has a lot of beneficial advantages[148,149]. High-volume centers should routinely perform emergent laparoscopic surgery including LA[148]. Physicians and surgeons have a large interesting frontier.
AA is pathophysiologically progressive. As time passes, AA is difficult to control. Prompt LA in a quadratic/tertiary care hospital is mandatory for AA, and this time-honored practice should be respected. Interval/delayed appendectomy and conservative management are unsuitable in Japan. The question can be asked: “Where should emergency physicians or general surgeons head in the next decade?”. We consider that it is important to focus on stabilizing prompt LA for AA around the world.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Biondi A, Demetrashvili Z, Dinc B, Lee SC S- Editor: Gong ZM L- Editor: A E- Editor: Zhang FF
| 1. | Stewart D. The management of acute appendicitis. In: Cameron JL, Cameron AM, editors. Current surgical therapy. Philadelphia: Elsevier Saunders; 2014: 252-255. . |
| 2. | Quartey B. Interval appendectomy in adults: A necessary evil? J Emerg Trauma Shock. 2012;5:213-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Ditillo MF, Dziura JD, Rabinovici R. Is it safe to delay appendectomy in adults with acute appendicitis? Ann Surg. 2006;244:656-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 190] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 4. | Udgiri N, Curras E, Kella VK, Nagpal K, Cosgrove J. Appendicitis, is it an emergency? Am Surg. 2011;77:898-901. [PubMed] |
| 5. | Cervini P, Smith LC, Urbach DR. The surgeon on call is a strong factor determining the use of a laparoscopic approach for appendectomy. Surg Endosc. 2002;16:1774-1777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Sicard N, Tousignant P, Pineault R, Dubé S. Non-patient factors related to rates of ruptured appendicitis. Br J Surg. 2007;94:214-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Eldar S, Nash E, Sabo E, Matter I, Kunin J, Mogilner JG, Abrahamson J. Delay of surgery in acute appendicitis. Am J Surg. 1997;173:194-198. [PubMed] |
| 8. | Langelotz C, Scharfenberg M, Haase O, Schwenk W. Stress and heart rate variability in surgeons during a 24-hour shift. Arch Surg. 2008;143:751-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Kelz RR, Freeman KM, Hosokawa PW, Asch DA, Spitz FR, Moskowitz M, Henderson WG, Mitchell ME, Itani KM. Time of day is associated with postoperative morbidity: an analysis of the national surgical quality improvement program data. Ann Surg. 2008;247:544-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 141] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 10. | Zare MM, Itani KM, Schifftner TL, Henderson WG, Khuri SF. Mortality after nonemergent major surgery performed on Friday versus Monday through Wednesday. Ann Surg. 2007;246:866-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 89] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 11. | Skoubo-Kristensen E, Hvid I. The appendiceal mass: results of conservative management. Ann Surg. 1982;196:584-587. [PubMed] |
| 12. | Hoffmann J, Lindhard A, Jensen HE. Appendix mass: conservative management without interval appendectomy. Am J Surg. 1984;148:379-382. [PubMed] |
| 13. | Adalla SA. Appendiceal mass: interval appendicectomy should not be the rule. Br J Clin Pract. 1996;50:168-169. [PubMed] |
| 14. | Lai HW, Loong CC, Chiu JH, Chau GY, Wu CW, Lui WY. Interval appendectomy after conservative treatment of an appendiceal mass. World J Surg. 2006;30:352-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Vons C, Barry C, Maitre S, Pautrat K, Leconte M, Costaglioli B, Karoui M, Alves A, Dousset B, Valleur P. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet. 2011;377:1573-1579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 408] [Cited by in RCA: 441] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 16. | Nitecki S, Assalia A, Schein M. Contemporary management of the appendiceal mass. Br J Surg. 1993;80:18-20. [PubMed] |
| 17. | Andersson RE, Petzold MG. Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg. 2007;246:741-748. [PubMed] |
| 18. | Mason RJ. Appendicitis: is surgery the best option? Lancet. 2011;377:1545-1546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Andersson N, Griffiths H, Murphy J, Roll J, Serenyi A, Swann I, Cockcroft A, Myers J, St Leger A. Is appendicitis familial? Br Med J. 1979;2:697-698. [PubMed] |
| 21. | Jones BA, Demetriades D, Segal I, Burkitt DP. The prevalence of appendiceal fecaliths in patients with and without appendicitis. A comparative study from Canada and South Africa. Ann Surg. 1985;202:80-82. [PubMed] |
| 22. | Larner AJ. The aetiology of appendicitis. Br J Hosp Med. 1988;39:540-542. [PubMed] |
| 23. | Canterino JE, McCormack M, Gurung A, Passarelli J, Landry ML, Golden M. Cytomegalovirus appendicitis in an immunocompetent host. J Clin Virol. 2016;78:9-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 24. | Plataras C, Tsangouri S, Bourikas D, Christianakis E. Acute appendicitis in a child with swine influenza (H1N1). BMJ Case Rep. 2015;2015:pii: bcr2014208219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Cheluvappa R, Luo AS, Palmer C, Grimm MC. Protective pathways against colitis mediated by appendicitis and appendectomy. Clin Exp Immunol. 2011;165:393-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 26. | Kokkonen TS, Karttunen TJ. Endothelial Fas-Ligand in Inflammatory Bowel Diseases and in Acute Appendicitis. J Histochem Cytochem. 2015;63:931-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Bockman DE. Functional histology of appendix. Arch Histol Jpn. 1983;46:271-292. [PubMed] |
| 28. | Di Sebastiano P, Fink T, di Mola FF, Weihe E, Innocenti P, Friess H, Büchler MW. Neuroimmune appendicitis. Lancet. 1999;354:461-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 77] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 29. | Wang Y, Reen DJ, Puri P. Is a histologically normal appendix following emergency appendicectomy alway normal? Lancet. 1996;347:1076-1079. [PubMed] |
| 30. | de Oliveira Machado SL, Bagatini MD, da Costa P, Baldissarelli J, Reichert KP, de Oliveira LS, Lemos JG, Duarte T, Chitolina Schetinger MR, Morsch VM. Evaluation of mediators of oxidative stress and inflammation in patients with acute appendicitis. Biomarkers. 2016;21:530-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 31. | Rivera-Chavez FA, Peters-Hybki DL, Barber RC, Lindberg GM, Jialal I, Munford RS, O’Keefe GE. Innate immunity genes influence the severity of acute appendicitis. Ann Surg. 2004;240:269-277. [PubMed] |
| 32. | Khalil M, Rhee P, Jokar TO, Kulvatunyou N, O’Keeffe T, Tang A, Hassan A, Gries L, Latifi R, Joseph B. Antibiotics for appendicitis! Not so fast. J Trauma Acute Care Surg. 2016;80:923-932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 33. | Wagner JM, McKinney WP, Carpenter JL. Does this patient have appendicitis? JAMA. 1996;276:1589-1594. [PubMed] |
| 34. | Lukáš K. [The story of Appendix]. Cas Lek Cesk. 2015;154:189-193. [PubMed] |
| 36. | Chen KC, Arad A, Chen KC, Storrar J, Christy AG. The clinical value of pathology tests and imaging study in the diagnosis of acute appendicitis. Postgrad Med J. 2016;92:611-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 37. | Kim HC, Yang DM, Kim SW, Park SJ. Reassessment of CT images to improve diagnostic accuracy in patients with suspected acute appendicitis and an equivocal preoperative CT interpretation. Eur Radiol. 2012;22:1178-1185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 38. | Hopkins JA, Wilson SE, Bobey DG. Adjunctive antimicrobial therapy for complicated appendicitis: bacterial overkill by combination therapy. World J Surg. 1994;18:933-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 39. | Rao PM, Rhea JT, Novelline RA, Mostafavi AA, McCabe CJ. Effect of computed tomography of the appendix on treatment of patients and use of hospital resources. N Engl J Med. 1998;338:141-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 508] [Cited by in RCA: 444] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 40. | Wagner PL, Eachempati SR, Soe K, Pieracci FM, Shou J, Barie PS. Defining the current negative appendectomy rate: for whom is preoperative computed tomography making an impact? Surgery. 2008;144:276-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 73] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 41. | Pritchett CV, Levinsky NC, Ha YP, Dembe AE, Steinberg SM. Management of acute appendicitis: the impact of CT scanning on the bottom line. J Am Coll Surg. 2010;210:699-705, 705-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 42. | Livingston EH, Woodward WA, Sarosi GA, Haley RW. Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg. 2007;245:886-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 320] [Cited by in RCA: 307] [Article Influence: 17.1] [Reference Citation Analysis (1)] |
| 43. | Aly NE, McAteer D, Aly EH. Low vs. standard dose computed tomography in suspected acute appendicitis: Is it time for a change? Int J Surg. 2016;31:71-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 44. | Zviedre A, Engelis A, Tretjakovs P, Jurka A, Zile I, Petersons A. Role of serum cytokines in acute appendicitis and acute mesenteric lymphadenitis among children. Medicina (Kaunas). 2016;52:291-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 45. | Sack U, Biereder B, Elouahidi T, Bauer K, Keller T, Tröbs RB. Diagnostic value of blood inflammatory markers for detection of acute appendicitis in children. BMC Surg. 2006;6:15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 85] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 46. | Sülberg D, Chromik AM, Kersting S, Meurer K, Tannapfel A, Uhl W, Mittelkötter U. [Appendicitis in the elderly. CRP value as decision support for diagnostic laparoscopy]. Chirurg. 2009;80:608-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 47. | Jeon BG. Predictive factors and outcomes of negative appendectomy. Am J Surg. 2017;213:731-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 48. | Kabir SA, Kabir SI, Sun R, Jafferbhoy S, Karim A. How to diagnose an acutely inflamed appendix; a systematic review of the latest evidence. Int J Surg. 2017;40:155-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 49. | Semm K. Endoscopic appendectomy. Endoscopy. 1983;15:59-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 807] [Cited by in RCA: 716] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 50. | Heinzelmann M, Simmen HP, Cummins AS, Largiadèr F. Is laparoscopic appendectomy the new ‘gold standard’? Arch Surg. 1995;130:782-785. [PubMed] |
| 51. | Chung RS, Rowland DY, Li P, Diaz J. A meta-analysis of randomized controlled trials of laparoscopic versus conventional appendectomy. Am J Surg. 1999;177:250-256. [PubMed] |
| 52. | Garbutt JM, Soper NJ, Shannon WD, Botero A, Littenberg B. Meta-analysis of randomized controlled trials comparing laparoscopic and open appendectomy. Surg Laparosc Endosc. 1999;9:17-26. [PubMed] |
| 53. | Golub R, Siddiqui F, Pohl D. Laparoscopic versus open appendectomy: a metaanalysis. J Am Coll Surg. 1998;186:545-553. [PubMed] |
| 54. | Sauerland S, Lefering R, Holthausen U, Neugebauer EA. Laparoscopic vs conventional appendectomy--a meta-analysis of randomised controlled trials. Langenbecks Arch Surg. 1998;383:289-295. [PubMed] |
| 55. | Temple LK, Litwin DE, McLeod RS. A meta-analysis of laparoscopic versus open appendectomy in patients suspected of having acute appendicitis. Can J Surg. 1999;42:377-383. [PubMed] |
| 56. | Faiz O, Clark J, Brown T, Bottle A, Antoniou A, Farrands P, Darzi A, Aylin P. Traditional and laparoscopic appendectomy in adults: outcomes in English NHS hospitals between 1996 and 2006. Ann Surg. 2008;248:800-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 59] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 57. | Fullum TM, Ladapo JA, Borah BJ, Gunnarsson CL. Comparison of the clinical and economic outcomes between open and minimally invasive appendectomy and colectomy: evidence from a large commercial payer database. Surg Endosc. 2010;24:845-853. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (1)] |
| 58. | Guller U, Hervey S, Purves H, Muhlbaier LH, Peterson ED, Eubanks S, Pietrobon R. Laparoscopic versus open appendectomy: outcomes comparison based on a large administrative database. Ann Surg. 2004;239:43-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 349] [Article Influence: 16.6] [Reference Citation Analysis (1)] |
| 59. | Moberg AC, Berndsen F, Palmquist I, Petersson U, Resch T, Montgomery A. Randomized clinical trial of laparoscopic versus open appendicectomy for confirmed appendicitis. Br J Surg. 2005;92:298-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 75] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 60. | Pedersen AG, Petersen OB, Wara P, Rønning H, Qvist N, Laurberg S. Randomized clinical trial of laparoscopic versus open appendicectomy. Br J Surg. 2001;88:200-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 151] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 61. | Kouhia ST, Heiskanen JT, Huttunen R, Ahtola HI, Kiviniemi VV, Hakala T. Long-term follow-up of a randomized clinical trial of open versus laparoscopic appendicectomy. Br J Surg. 2010;97:1395-1400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 62. | Tiwari MM, Reynoso JF, Tsang AW, Oleynikov D. Comparison of outcomes of laparoscopic and open appendectomy in management of uncomplicated and complicated appendicitis. Ann Surg. 2011;254:927-932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 106] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 63. | Brügger L, Rosella L, Candinas D, Güller U. Improving outcomes after laparoscopic appendectomy: a population-based, 12-year trend analysis of 7446 patients. Ann Surg. 2011;253:309-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 64. | Ball CG, Kortbeek JB, Kirkpatrick AW, Mitchell P. Laparoscopic appendectomy for complicated appendicitis: an evaluation of postoperative factors. Surg Endosc. 2004;18:969-973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 80] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 65. | Towfigh S, Chen F, Mason R, Katkhouda N, Chan L, Berne T. Laparoscopic appendectomy significantly reduces length of stay for perforated appendicitis. Surg Endosc. 2006;20:495-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 68] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 66. | Sahm M, Pross M, Otto R, Koch A, Gastinger I, Lippert H. Clinical Health Service Research on the Surgical Therapy of Acute Appendicitis: Comparison of Outcomes Based on 3 German Multicenter Quality Assurance Studies Over 21 Years. Ann Surg. 2015;262:338-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 67. | Mentula P, Sammalkorpi H, Leppäniemi A. Laparoscopic Surgery or Conservative Treatment for Appendiceal Abscess in Adults? A Randomized Controlled Trial. Ann Surg. 2015;262:237-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 82] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 68. | Ingraham AM, Cohen ME, Bilimoria KY, Pritts TA, Ko CY, Esposito TJ. Comparison of outcomes after laparoscopic versus open appendectomy for acute appendicitis at 222 ACS NSQIP hospitals. Surgery. 2010;148:625-635; discussion 635-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 146] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 69. | Bulian DR, Kaehler G, Magdeburg R, Butters M, Burghardt J, Albrecht R, Bernhardt J, Heiss MM, Buhr HJ, Lehmann KS. Analysis of the First 217 Appendectomies of the German NOTES Registry. Ann Surg. 2017;265:534-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 70. | Wood SG, Panait L, Duffy AJ, Bell RL, Roberts KE. Complications of transvaginal natural orifice transluminal endoscopic surgery: a series of 102 patients. Ann Surg. 2014;259:744-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 71. | Ingraham AM, Cohen ME, Bilimoria KY, Ko CY, Hall BL, Russell TR, Nathens AB. Effect of delay to operation on outcomes in adults with acute appendicitis. Arch Surg. 2010;145:886-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 110] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 72. | Norton VC, Schriger DL. Effect of transfer on outcome in patients with appendicitis. Ann Emerg Med. 1997;29:467-473. [PubMed] |
| 73. | Teixeira PG, Sivrikoz E, Inaba K, Talving P, Lam L, Demetriades D. Appendectomy timing: waiting until the next morning increases the risk of surgical site infections. Ann Surg. 2012;256:538-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 116] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 74. | Nagpal K, Udgiri N, Sharma N, Curras E, Cosgrove JM, Farkas DT. Delaying an appendectomy: is it safe? Am Surg. 2012;78:897-900. [PubMed] |
| 75. | Kanona H, Al Samaraee A, Nice C, Bhattacharya V. Stump appendicitis: a review. Int J Surg. 2012;10:425-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 76. | Perri S, Amendolara M, Gallo G, Valenti G, Meneghini G, Gelmi GF. [Laparoscopic appendectomy in clinical practice. Aesthetic and functional advantages]. G Chir. 1993;14:313-319. [PubMed] |
| 77. | Beldi G, Vorburger SA, Bruegger LE, Kocher T, Inderbitzin D, Candinas D. Analysis of stapling versus endoloops in appendiceal stump closure. Br J Surg. 2006;93:1390-1393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 82] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 78. | Sohn M, Hoffmann M, Pohlen U, Lauscher JC, Zurbuchen U, Holmer C, Buhr HJ, Lehmann KS. [Stump closure in laparoscopic appendectomy. Influence of endoloop or linear stapler on patient outcome]. Chirurg. 2014;85:46-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 79. | Guzman MJ, Gitelis ME, Linn JG, Ujiki MB, Waskerwitz M, Umanskiy K, Muldoon JP. A Model of Cost Reduction and Standardization: Improved Cost Savings While Maintaining the Quality of Care. Dis Colon Rectum. 2015;58:1104-1107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 80. | Matyja M, Strzałka M, Rembiasz K. Laparosocopic Appendectomy, Cost-Effectiveness of Three Different Techniques Used to Close the Appendix Stump. Pol Przegl Chir. 2015;87:634-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 81. | Horvath P, Lange J, Bachmann R, Struller F, Königsrainer A, Zdichavsky M. Comparison of clinical outcome of laparoscopic versus open appendectomy for complicated appendicitis. Surg Endosc. 2017;31:199-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 82. | Fleming FJ, Kim MJ, Messing S, Gunzler D, Salloum R, Monson JR. Balancing the risk of postoperative surgical infections: a multivariate analysis of factors associated with laparoscopic appendectomy from the NSQIP database. Ann Surg. 2010;252:895-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 83. | Lygidakis NJ. Surgical approaches to peritonitis. The value of intra- and postoperative peritoneal lavage. Acta Chir Belg. 1983;83:345-352. [PubMed] |
| 84. | Uematsu D, Akiyama G, Magishi A, Sano T, Niitsu H, Narita M, Komatsu H. Laparoscopic Hartmann’s procedure for fecal peritonitis resulting from perforation of the left-sided colon in elderly and severely ill patients. Tech Coloproctol. 2012;16:243-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 85. | Faranda C, Barrat C, Catheline JM, Champault GG. Two-stage laparoscopic management of generalized peritonitis due to perforated sigmoid diverticula: eighteen cases. Surg Laparosc Endosc Percutan Tech. 2000;10:135-138; discussion 139-141. [PubMed] |
| 86. | Bhangu A, Singh P, Lundy J, Bowley DM. Systemic review and meta-analysis of randomized clinical trials comparing primary vs delayed primary skin closure in contaminated and dirty abdominal incisions. JAMA Surg. 2013;148:779-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 87. | Siribumrungwong B, Srikuea K, Thakkinstian A. Comparison of superficial surgical site infection between delayed primary and primary wound closures in ruptured appendicitis. Asian J Surg. 2014;37:120-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 88. | Rucinski J, Fabian T, Panagopoulos G, Schein M, Wise L. Gangrenous and perforated appendicitis: a meta-analytic study of 2532 patients indicates that the incision should be closed primarily. Surgery. 2000;127:136-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 89. | Cohn SM, Giannotti G, Ong AW, Varela JE, Shatz DV, McKenney MG, Sleeman D, Ginzburg E, Augenstein JS, Byers PM. Prospective randomized trial of two wound management strategies for dirty abdominal wounds. Ann Surg. 2001;233:409-413. [PubMed] |
| 90. | Siribumrungwong B, Noorit P, Wilasrusmee C, Thakkinstian A. A systematic review and meta-analysis of randomised controlled trials of delayed primary wound closure in contaminated abdominal wounds. World J Emerg Surg. 2014;9:49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 91. | Markides G, Subar D, Riyad K. Laparoscopic versus open appendectomy in adults with complicated appendicitis: systematic review and meta-analysis. World J Surg. 2010;34:2026-2040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 110] [Article Influence: 7.3] [Reference Citation Analysis (1)] |
| 92. | Senekjian L, Nirula R. Tailoring the operative approach for appendicitis to the patient: a prediction model from national surgical quality improvement program data. J Am Coll Surg. 2013;216:34-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 93. | Romy S, Eisenring MC, Bettschart V, Petignat C, Francioli P, Troillet N. Laparoscope use and surgical site infections in digestive surgery. Ann Surg. 2008;247:627-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 94] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 94. | Rosser JC Jr, Lynch PJ, Cuddihy L, Gentile DA, Klonsky J, Merrell R. The impact of video games on training surgeons in the 21st century. Arch Surg. 2007;142:181-186; discusssion 186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 394] [Cited by in RCA: 295] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 95. | Badurdeen S, Abdul-Samad O, Story G, Wilson C, Down S, Harris A. Nintendo Wii video-gaming ability predicts laparoscopic skill. Surg Endosc. 2010;24:1824-1828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 65] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 96. | Glassman D, Yiasemidou M, Ishii H, Somani BK, Ahmed K, Biyani CS. Effect of Playing Video Games on Laparoscopic Skills Performance: A Systematic Review. J Endourol. 2016;30:146-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 97. | Middleton KK, Hamilton T, Tsai PC, Middleton DB, Falcone JL, Hamad G. Improved nondominant hand performance on a laparoscopic virtual reality simulator after playing the Nintendo Wii. Surg Endosc. 2013;27:4224-4231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 98. | Ju R, Chang PL, Buckley AP, Wang KC. Comparison of Nintendo Wii and PlayStation2 for enhancing laparoscopic skills. JSLS. 2012;16:612-618. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 99. | Overtoom EM, Jansen FW, van Santbrink EJ, Schraffordt Koops SE, Veersema S, Schreuder HW. Training in Basic Laparoscopic Surgical Skills: Residents Opinion of the New Nintendo Wii-U Laparoscopic Simulator. J Surg Educ. 2017;74:352-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 100. | Jalink MB, Goris J, Heineman E, Pierie JP, ten Cate Hoedemaker HO. Construct and concurrent validity of a Nintendo Wii video game made for training basic laparoscopic skills. Surg Endosc. 2014;28:537-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 101. | Bokhari R, Bollman-McGregor J, Kahoi K, Smith M, Feinstein A, Ferrara J. Design, development, and validation of a take-home simulator for fundamental laparoscopic skills: using Nintendo Wii for surgical training. Am Surg. 2010;76:583-586. [PubMed] |
| 102. | Wakasugi M, Tsujimura N, Nakahara Y, Matsumoto T, Takemoto H, Takachi K, Nishioka K, Oshima S. Single-incision laparoscopically assisted appendectomy performed by residents is safe and feasible: A single institution, retrospective case series. Ann Med Surg (Lond). 2017;15:43-46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 103. | Graat LJ, Bosma E, Roukema JA, Heisterkamp J. Appendectomy by residents is safe and not associated with a higher incidence of complications: a retrospective cohort study. Ann Surg. 2012;255:715-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 104. | Lin YY, Shabbir A, So JB. Laparoscopic appendectomy by residents: evaluating outcomes and learning curve. Surg Endosc. 2010;24:125-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 69] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 105. | Albright JB, Fakhre GP, Nields WW, Metzger PP. Incidental appendectomy: 18-year pathologic survey and cost effectiveness in the nonmanaged-care setting. J Am Coll Surg. 2007;205:298-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 106. | Ochsner A. The cause of diffuse peritonitis complicating appendicitis and its prevention. JAMA. 1901;26:1747-1754. |
| 107. | Willemsen PJ, Hoorntje LE, Eddes EH, Ploeg RJ. The need for interval appendectomy after resolution of an appendiceal mass questioned. Dig Surg. 2002;19:216-220; discussion 221. [PubMed] |
| 108. | Ahmed I, Deakin D, Parsons SL. Appendix mass: do we know how to treat it? Ann R Coll Surg Engl. 2005;87:191-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 109. | Mosegaard A, Nielsen OS. Interval appendectomy. A retrospective study. Acta Chir Scand. 1979;145:109-111. [PubMed] |
| 110. | Foran B, Berne TV, Rosoff L. Management of the appendiceal mass. Arch Surg. 1978;113:1144-1145. [PubMed] |
| 111. | Engkvist O. Appendectomy à froid a superfluous routine operation? Acta Chir Scand. 1971;137:797-800. [PubMed] |
| 112. | Tekin A, Kurtoğlu HC, Can I, Oztan S. Routine interval appendectomy is unnecessary after conservative treatment of appendiceal mass. Colorectal Dis. 2008;10:465-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 45] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 113. | Eriksson S, Granström L. Randomized controlled trial of appendicectomy versus antibiotic therapy for acute appendicitis. Br J Surg. 1995;82:166-169. [PubMed] |
| 114. | Styrud J, Eriksson S, Nilsson I, Ahlberg G, Haapaniemi S, Neovius G, Rex L, Badume I, Granström L. Appendectomy versus antibiotic treatment in acute appendicitis. a prospective multicenter randomized controlled trial. World J Surg. 2006;30:1033-1037. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 329] [Cited by in RCA: 352] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 116. | Eriksson S, Styrud J. Interval appendicectomy: a retrospective study. Eur J Surg. 1998;164:771-774; discussion 775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 30] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 118. | Corfield L. Interval appendicectomy after appendiceal mass or abscess in adults: what is “best practice”? Surg Today. 2007;37:1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 120. | Kaminski A, Liu IL, Applebaum H, Lee SL, Haigh PI. Routine interval appendectomy is not justified after initial nonoperative treatment of acute appendicitis. Arch Surg. 2005;140:897-901. [PubMed] |
| 121. | Yamini D, Vargas H, Bongard F, Klein S, Stamos MJ. Perforated appendicitis: is it truly a surgical urgency? Am Surg. 1998;64:970-975. [PubMed] |
| 122. | Margenthaler JA, Longo WE, Virgo KS, Johnson FE, Oprian CA, Henderson WG, Daley J, Khuri SF. Risk factors for adverse outcomes after the surgical treatment of appendicitis in adults. Ann Surg. 2003;238:59-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 90] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 123. | Andersen BR, Kallehave FL, Andersen HK. Antibiotics versus placebo for prevention of postoperative infection after appendicectomy. Cochrane Database Syst Rev. 2005;CD001439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 88] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 124. | Wong PF, Gilliam AD, Kumar S, Shenfine J, O’Dair GN, Leaper DJ. Antibiotic regimens for secondary peritonitis of gastrointestinal origin in adults. Cochrane Database Syst Rev. 2005;CD004539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 47] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 125. | López JJ, Deans KJ, Minneci PC. Nonoperative management of appendicitis in children. Curr Opin Pediatr. 2017;29:358-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 126. | Georgiou R, Eaton S, Stanton MP, Pierro A, Hall NJ. Efficacy and Safety of Nonoperative Treatment for Acute Appendicitis: A Meta-analysis. Pediatrics. 2017;139:pii: e20163003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 113] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 127. | Gonzalez DO, Deans KJ, Minneci PC. Role of non-operative management in pediatric appendicitis. Semin Pediatr Surg. 2016;25:204-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 128. | Kumar S, Jain S. Treatment of appendiceal mass: prospective, randomized clinical trial. Indian J Gastroenterol. 2004;23:165-167. [PubMed] |
| 129. | Park HC, Kim MJ, Lee BH. Antibiotic therapy for appendicitis in patients aged ≥80 years. Am J Med. 2014;127:562-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 130. | Parmentier B, Berrebi D, Peycelon M, Doit C, Ghoneimi AE, Bonnard A. Failure of First-Line Antibiotics in Nonoperative Management of Appendiceal Mass, toward a Second-Line Instead of Surgery? Eur J Pediatr Surg. 2016;26:267-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 131. | de Kraker ME, Wolkewitz M, Davey PG, Koller W, Berger J, Nagler J, Icket C, Kalenic S, Horvatic J, Seifert H. Burden of antimicrobial resistance in European hospitals: excess mortality and length of hospital stay associated with bloodstream infections due to Escherichia coli resistant to third-generation cephalosporins. J Antimicrob Chemother. 2011;66:398-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 170] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 132. | Sadot E, Telem DA, Arora M, Butala P, Nguyen SQ, Divino CM. Laparoscopy: a safe approach to appendicitis during pregnancy. Surg Endosc. 2010;24:383-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 66] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 133. | McGory ML, Zingmond DS, Tillou A, Hiatt JR, Ko CY, Cryer HM. Negative appendectomy in pregnant women is associated with a substantial risk of fetal loss. J Am Coll Surg. 2007;205:534-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 172] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 134. | Wilasrusmee C, Sukrat B, McEvoy M, Attia J, Thakkinstian A. Systematic review and meta-analysis of safety of laparoscopic versus open appendicectomy for suspected appendicitis in pregnancy. Br J Surg. 2012;99:1470-1478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 128] [Cited by in RCA: 110] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 135. | Wei L, Macdonald TM, Shimi SM. Appendicectomy is associated with increased pregnancy rate: a cohort study. Ann Surg. 2012;256:1039-1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 136. | Bucher P, Mathe Z, Demirag A, Morel P. Appendix tumors in the era of laparoscopic appendectomy. Surg Endosc. 2004;18:1063-1066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 60] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 137. | Wright GP, Mater ME, Carroll JT, Choy JS, Chung MH. Is there truly an oncologic indication for interval appendectomy? Am J Surg. 2015;209:442-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 66] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 138. | Wu JX, Dawes AJ, Sacks GD, Brunicardi FC, Keeler EB. Cost effectiveness of nonoperative management versus laparoscopic appendectomy for acute uncomplicated appendicitis. Surgery. 2015;158:712-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 139. | Needham PJ, Laughlan KA, Botterill ID, Ambrose NS. Laparoscopic appendicectomy: calculating the cost. Ann R Coll Surg Engl. 2009;91:606-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 140. | Uzman S, Donmez T, Erdem VM, Hut A, Yildirim D, Akinci M. Combined spinal-epidural anesthesia in laparoscopic appendectomy: a prospective feasibility study. Ann Surg Treat Res. 2017;92:208-213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 141. | Hamill JK, Liley A, Hill AG. Intraperitoneal Local Anesthetic for Laparoscopic Appendectomy in Children: A Randomized Controlled Trial. Ann Surg. 2017;266:189-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 142. | Sumiyoshi R. [Preoperative fasting and fluid management in pediatric patients]. Masui. 2013;62:1045-1052. [PubMed] |
| 143. | Chau-in W, Hintong T, Rodanant O, Lekprasert V, Punjasawadwong Y, Charuluxananan S, Tanudsintum S. Anesthesia-related complications of caesarean delivery in Thailand: 16,697 cases from the Thai Anaesthesia Incidents Study. J Med Assoc Thai. 2010;93:1274-1283. [PubMed] |
| 144. | Perez J, Barone JE, Wilbanks TO, Jorgensson D, Corvo PR. Liberal use of computed tomography scanning does not improve diagnostic accuracy in appendicitis. Am J Surg. 2003;185:194-197. [PubMed] |
| 145. | Nosé Y. Japanese government saves hemodialysis patients’ lives. Artif Organs. 1998;22:815. [PubMed] |
| 146. | Hori T, Kaido T, Iida T, Yagi S, Uemoto S. Comprehensive guide to laparoscope-assisted graft harvesting in live donors for living-donor liver transplantation: perspective of laparoscopic vision. Ann Gastroenterol. 2017;30:118-126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 147. | Di Saverio S, Birindelli A, Kelly MD, Catena F, Weber DG, Sartelli M, Sugrue M, De Moya M, Gomes CA, Bhangu A. WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis. World J Emerg Surg. 2016;11:34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 288] [Cited by in RCA: 251] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 148. | Agresta F, De Simone P, Leone L, Arezzo A, Biondi A, Bottero L, Catena F, Conzo G, Del Genio G, Fersini A, Guerrieri M, Illomei G, Tonelli P, Vitellaro M, Docimo G, Crucitti A; Italian Society Of Young Surgeons (SPIGC). Laparoscopic appendectomy in Italy: an appraisal of 26,863 cases. J Laparoendosc Adv Surg Tech A. 2004;14:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 149. | Biondi A, Di Stefano C, Ferrara F, Bellia A, Vacante M, Piazza L. Laparoscopic versus open appendectomy: a retrospective cohort study assessing outcomes and cost-effectiveness. World J Emerg Surg. 2016;11:44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |