Published online Jun 14, 2017. doi: 10.3748/wjg.v23.i22.4054
Peer-review started: January 15, 2017
First decision: March 16, 2017
Revised: March 28, 2017
Accepted: May 9, 2017
Article in press: May 9, 2017
Published online: June 14, 2017
Processing time: 149 Days and 12.6 Hours
To compare the Barcelona Clinic Liver Cancer (BCLC) and Hong Kong Liver Cancer (HKLC) classification systems when applied to HCC patients from the largest tertiary-level centre in Singapore.
One thousand two hundred and seventy hepatocellular carcinoma (HCC) patients prospectively enrolled in a tertiary-level centre registry in Singapore since 1988 were studied. Patients were grouped into their respective BCLC and HKLC stages. Data such as demography, aetiology of HCC and type of treatment were collected. Survival data was based on census with the National Registry of Births and Deaths on 31st October 2015. Statistical analyses were done using SPSS version 21 (Chicago, IL, United States). Survival analyses were done by the Kaplan-Meier method. Differences in survival rates were compared using the log-rank test.
The median age at presentation was 63 years (range 13-94); male 82.4%; Chinese 89.4%, Malay 7.1%, Indian, 2.8%. Hepatitis B was the predominant aetiology (75.0%; Hepatitis C 7.2%, Hepatitis B and C co-infection 3.8%, non-viral 14.0%). Both BCLC and HKLC staging systems showed good separation with overall log rank test confirming significant survival differences between stages in our cohort (P < 0.001). 206 out of the 240 patients (85.8%) assigned for curative treatment by the BCLC treatment algorithm received curative therapy for HCC [Stage 0 93.2% (68/73); Stage A 82.6% (138/167)]. In contrast, only 341/558 (61.1%) patients received curative treatment despite being assigned for curative treatment by the HKLC treatment algorithm [Stage I 72.7% (264/363); Stage II 40.2% (66/164); Stage Va 35.5% (11/31)]. Patients who were assigned to curative treatment by HKLC but did not receive curative treatment had significantly poorer ECOG (P < 0.001), higher Child-Pugh status (P < 0.001) and were older (median age 66 vs 61, P < 0.001) than those who received curative therapy. Median overall survival in patients assigned to curative treatment groups by BCLC and HKLC were 6.1 and 2.6 years respectively (P < 0.001). When only patients receiving curative treatment were analyzed, BCLC still predicted overall median survival better than HKLC (7.1 years vs 5.5 years, P = 0.037).
BCLC performs better than HKLC in our multiethnic Asian population in allocating patients to curative treatment in a real-life situation as well as in predicting survival.
Core tip: This is a retrospective study of Barcelona Clinic Liver Cancer (BCLC) and Hong Kong Liver Cancer (HKLC) staging systems when applied to a multiethnic Asian cohort, where Chinese ethnicity and hepatitis B aetiology are predominant. BCLC was more accurate in directing therapy, with a significantly higher proportion of patients assigned to curative therapy receiving the recommended curative treatment (85.8% vs 61.1%, P < 0.001). Median overall survival in patients assigned to curative therapy by the BCLC and HKLC staging systems was 6.1 and 2.6 years respectively (P < 0.001). Thus, overall, BCLC performed better than HKLC for staging our cohort of patients.
- Citation: Li JW, Goh BBG, Chang PE, Tan CK. Barcelona Clinic Liver Cancer outperforms Hong Kong Liver Cancer staging of hepatocellular carcinoma in multiethnic Asians: Real-world perspective. World J Gastroenterol 2017; 23(22): 4054-4063
- URL: https://www.wjgnet.com/1007-9327/full/v23/i22/4054.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i22.4054
Hepatocellular carcinoma (HCC) is the second leading cause of cancer-related death in men and the sixth leading cause of cancer death in women worldwide[1]. HCC in the context of a cirrhotic patient is unique as many factors have an impact on the type of treatment modality suitable for the individual patient, which in turn influence patient survival. These include tumor-related factors such as tumor size and extent (number and size of lesions) as well as patient-related factors such as underlying liver function and performance status (PS). The Barcelona Clinic Liver Cancer (BCLC) staging system has been widely used since its inception for this purpose[2], and is the preferred approach by many clinicians for more than a decade due to its treatment recommendations based on stage and its ability to offer predictions on patient survival[3,4]. More recently, the Hong Kong Liver Cancer (HKLC) staging system[5] was developed. Like the BCLC staging system, it also incorporates PS, underlying liver function and tumor stage in its treatment recommendations.
Two main criticisms of the BCLC staging system are that it was derived from a relatively small cohort of patients and that it was derived from a predominantly Western population. This has resulted in a limited applicability in some settings[6,7]. In comparison, the HKLC staging system was developed from a larger cohort of patients with predominantly viral etiology, in particular hepatitis B. The HKLC staging system is arguably more aggressive in its treatment recommendations, assigning intermediate stage tumors (for example HKLC stage IIb) to curative treatment, whereas these patients would have been assigned to palliative treatment under the BCLC staging system. Intuitively, more aggressive treatment of HCC will lead to better survival rates for patients stratified by the HKLC staging system. However, this hypothesis requires external validation, and there are limited large scale studies comparing the two staging systems in terms of prognostication and treatment recommendations[8].
Singapore is a multiethnic Asian country where HCC is the fourth most common cancer in males and the second most fatal cancer[9]. Most clinicians have adopted the BCLC staging system as it is more well-established[10], although the predominant etiology of HCC in Singapore is hepatitis B. The aim of our study was to compare the abilities of the BCLC and HKLC staging systems to correctly assign patients to curative treatment groups in real life and to prognosticate survival when applied to patients with HCC in Singapore.
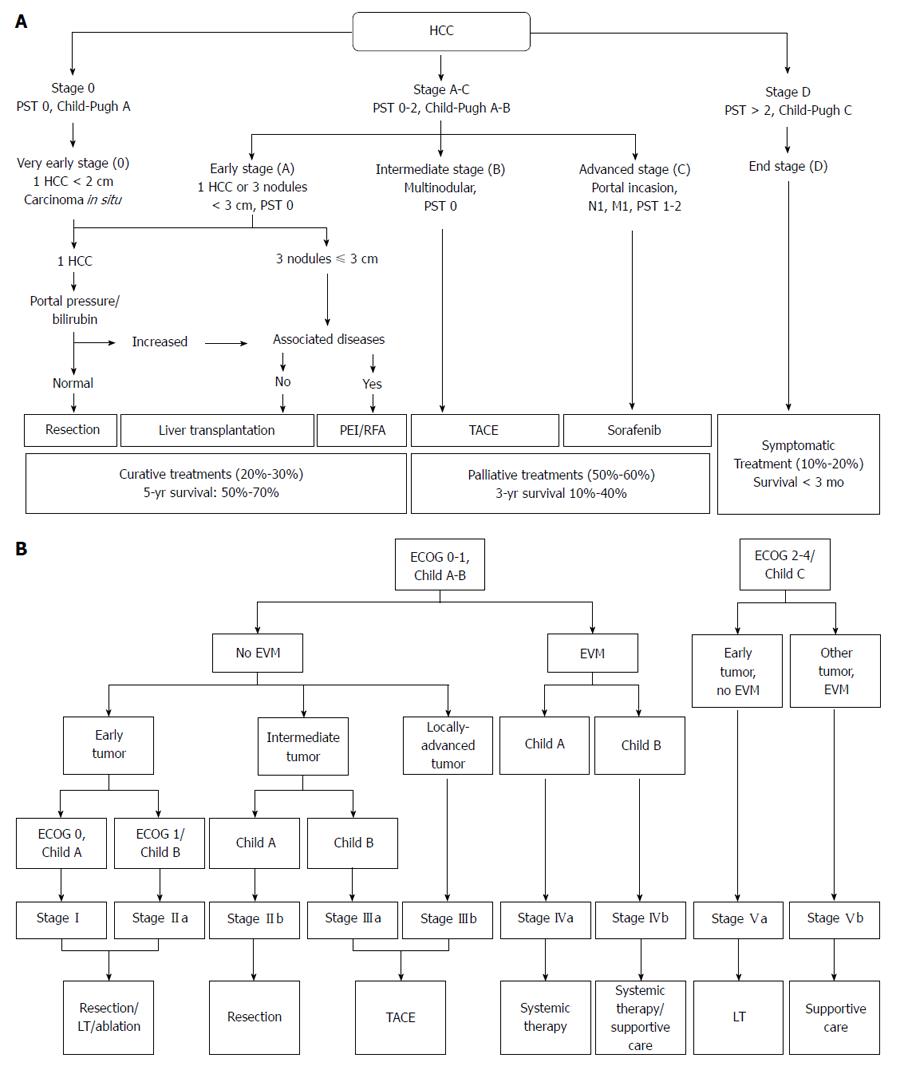
One thousand two hundred and seventy patients with HCC seen in the Department of Gastroenterology and Hepatology in the Singapore General Hospital, a tertiary-level medical center in Singapore, were studied. These patients were prospectively enrolled into a HCC registry since January 1988. The patients were enrolled upon diagnosis of HCC and were treatment-naïve at the time of enrollment. These patients were classified according to the BCLC and HKLC staging systems (Figure 1A and B). Patients assigned to the various tumor stages according to the BCLC and HKLC algorithms were divided into those who received treatment as recommended by the respective staging systems and those who did not.
The study protocol was approved by the Institutional Review Board and was conducted in accordance with the Declaration of Helsinki.
Data of patients enrolled in the HCC registry were prospectively collected. Patient characteristics include age at diagnosis, gender, etiology, PS by Eastern Cooperative Oncology Group (ECOG) stage, and Child Pugh status. Tumor characteristics such as number of lesions, size of individual lesions, presence of vascular invasion and extra-hepatic spread were collected. In addition, treatment modalities received by the patient such as surgical resection, radiofrequency ablation, liver transplantation, transarterial chemoembolization (TACE), and TACE with drug-eluding beads were also captured in the HCC registry. Survival census with the Singapore National Registry of Births and Deaths was performed on 31st October 2015.
Statistical analyses were done using SPSS version 21 (Chicago, IL, United States). Patients were grouped into the different stages according to the BCLC and HKLC staging systems. Survival rates for patients assigned to curative treatment by the respective staging systems were compared. Survival analyses were done by the Kaplan-Meier method. Differences in survival rates were compared using the log-rank test.
The median age at presentation of HCC was 63 years (range 13 to 94 years). 82.4% of the patients were male, and the majority were of Chinese ethnicity (89.4%), followed by Malays (7.1%), Indians (2.8%), and other ethnic groups (0.7%). Hepatitis B was the predominant etiology, accounting for 75% of cases. 7.2% of HCC cases had hepatitis C as the etiology, while hepatitis B and C co-infection comprised 3.8% of patients. Non-viral etiologies accounted for 14% of the patients. These findings, together with the Child Pugh class, are summarized in Table 1.
| Variable | All Patients (n = 1270) |
| Age, yr, median (range) | 63 (13-94) |
| Male | 1046 (82.4) |
| Ethnicity | |
| Chinese | 1135 (89.4) |
| Malay | 90 (7.1) |
| Indian | 36 (2.8) |
| Others | 9 (0.7) |
| Aetiology | |
| Hepatitis B | 953 (75.0) |
| Hepatitis C | 91 (7.2) |
| Hepatitis B and C co-infection | 48 (3.8) |
| Others | 178 (14.0) |
| Child-Pugh class | |
| A:B:C | 641 (50.5): 452 (35.6): 177 (13.9) |
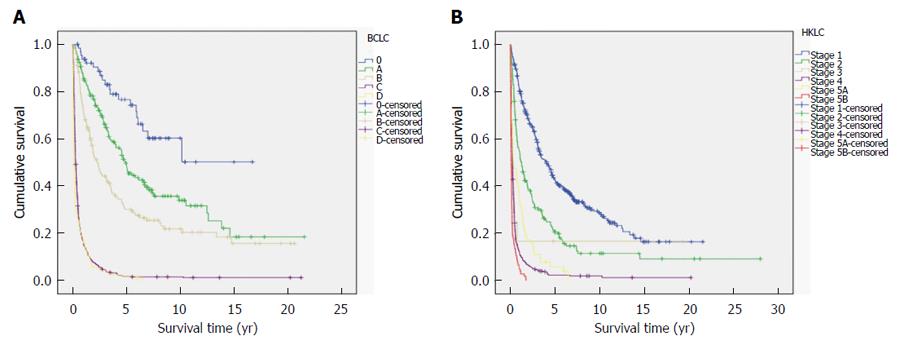
Both the BCLC and HKLC staging systems showed good differentiation in survival between the various stages, with the overall log-rank test showing significant survival differences between the stages (Figure 2A and B, respectively).
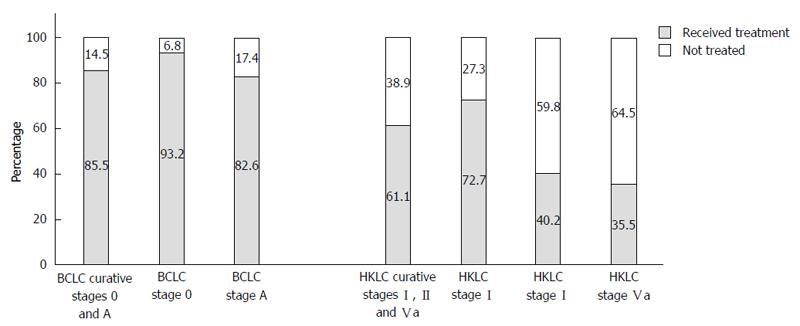
240 out of 1270 patients (18.9%) were assigned to curative treatment by the BCLC algorithm (Stage 0 5.7%, n = 73; Stage A 13.2%, n = 167). Within this group of patients, 206 out of the 240 patients (85.8%) received curative treatment, while the remaining patients (14.2%, n = 34) did not receive curative treatment despite being assigned as such. Between the BCLC stages recommending curative treatment, a higher proportion of patients in Stage 0 [93.2% (68/73)] received curative treatment compared to those assigned to Stage A [82.6% (138/167)], P < 0.05 (Figure 3).
Patients who received the recommended curative treatment according to their respective assignments had a better median survival than those who did not (7.1 years vs 1.1 years, n < 0.001). This observation was consistent when the survival analysis was applied to individual BCLC stage 0 and stage A.
In contrast to the BCLC staging system, more patients (43.9%, n = 558) in our study were assigned to curative treatment by the HKLC algorithm (Stage I 28.6%, n = 363; Stage II 12.9%, n = 164; Stage Va 2.4%, n = 31). Of these 558 patients, 341 (61.1%) received curative treatment as recommended by HKLC algorithm, while the remaining patients did not receive curative treatment. Within these HKLC stages, 264 out of 363 patients (72.7%) in HKLC Stage I received curative treatment, compared to 66 out of 164 patients (40.2%) in HKLC Stage II and 11 out of 31 patients (35.5%) in HKLC Stage Va (Figure 3).
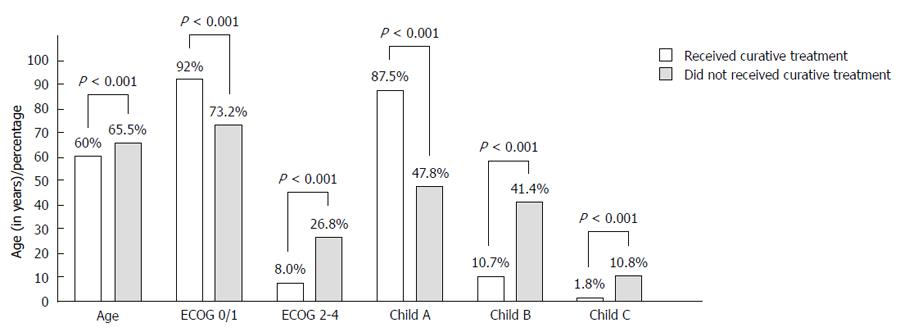
Patients assigned to curative treatment by the HKLC staging system but who did not receive the recommended treatment were significantly older (median age 66 years vs 60 years, P < 0.001), had significantly poorer ECOG status (P < 0.001), and were also of poorer Child-Pugh status (P < 0.001) at the time of diagnosis of HCC, compared to patients within the same group who received the recommended curative treatment (Figure 4).
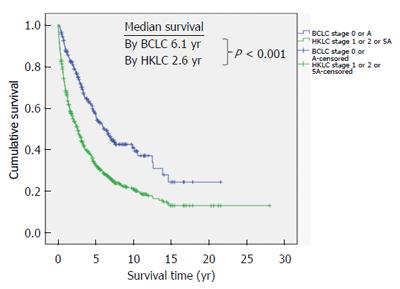
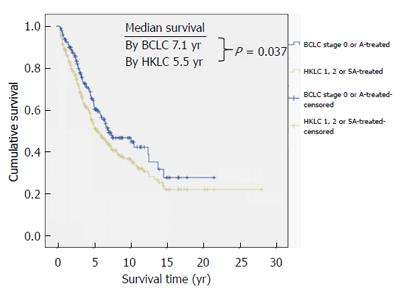
Median overall survival in patients assigned to curative treatment by the BCLC and HKLC staging systems were 6.1 and 2.6 years respectively (P < 0.001) (Figure 5). Among patients who received the recommended curative treatment by the respective staging systems, the BCLC system also predicted better overall survival than the HKLC system (7.1 vs 5.5 years respectively, P = 0.037) (Figure 6).
HCC treatment in the setting of liver cirrhosis is not always straightforward, given the need to consider the underlying liver function and ECOG status of the patient in addition to tumor extent to determine the most appropriate treatment modality. Both the BCLC and HKLC staging systems were developed in different cohorts with the intention of taking all these factors into account when recommending the most appropriate therapy for HCC. Besides the different ethnicities and HCC etiologies of the populations upon which the BCLC and HKLC staging systems were derived, the BCLC staging system has often been criticized for being too heterogeneous in its definition of stage B as well as being overly conservative[11,12]. This study adds further validation to both staging systems, as evidenced by the good separation of the survival curves when applied to our cohort of patients. In particular, it validates the BCLC system for prognostication of a multiethnic Asian HCC population with hepatitis B as the predominant etiology, a finding seen in few other studies to date[13].
Our study addressed the limitation of patients not receiving the treatment recommended. We examined the survival separately in patients who received and in those who did not receive the recommended curative treatment. We found significantly better survival in patients receiving the recommended curative treatment compared to those who did not despite assignment to the same stage in both staging systems. This demonstrated the validity of the curative treatment recommendations by both BCLC and HKLC staging systems in our population.
Of note, a significantly higher proportion of patients in our study were assigned to curative treatment by the HKLC staging system compared to BCLC (43.9% vs 18.9% respectively, P < 0.01). This is explained by the more aggressive approach by the HKLC staging system in the assignment of patients to curative therapy. For instance, the BCLC staging system utilizes PS as a veto factor to determine if a patient with HCC should be assigned to undergo curative treatment, and this has been criticized as one of its weaknesses. In contrast, the HKLC staging system collapses ECOG 0 and 1 patients into a single entity. In patients with early tumor, Child-Pugh B liver cirrhosis is also not a barrier to curative treatment. This effectively increases the pool of HCC patients being considered for curative treatment under HKLC staging, who would otherwise not receive such an assignment by the BCLC algorithm. These findings are similar to a recent study conducted in a separate Singapore center, where 57.3% (439/766) of patients were classified by HKLC into stages I, II and Va, while only 38.5% (295/766) were classified by BCLC into stages 0 and A[14].
However, despite the assignment, a significantly lower proportion of patients in our cohort classified by the HKLC staging system to receive curative therapy actually received the recommended curative treatment compared to BCLC (61.1% vs 85.8%, P < 0.001). This highlights important practical limitations in the application of the HKLC system in a real world setting. Certain forms of curative therapy, such as surgical resection, carry significant risk and morbidity, especially in patients with poorer ECOG status and more advanced cirrhosis. We postulate that this influenced both the managing physician’s ultimate recommended treatment option and the patient’s reluctance to accept treatment risks, resulting in a discrepancy between patients being assigned to curative treatment and those who actually received the recommended treatment. This is supported by the finding that patients who did not receive the recommended treatment were of older age, poorer ECOG status and worse Child-Pugh status within the patients assigned to curative treatment by the HKLC staging system. In addition, HKLC stage Va is curative liver transplantation therapy. Our liver transplantation program was set up only in 2014 and it was a small program in terms of numbers of transplantation done. Thus this also accounted for the less than expected patients receiving the assigned curative therapy. Nevertheless, even if we excluded the 31 patients who were assigned to HKLC stage Va (liver transplantation), there is still a significantly lower proportion of patients receiving curative treatment as recommended by HKLC staging compared to those similarly staged by BCLC (330/527 (62.6%) vs 206/240 (85.8%), P < 0.001).
At first glance, this difference in the proportion of patients receiving the curative treatment recommended by the respective staging systems could explain the significant differences in median overall survival between patients in the BCLC and HKLC curative stages (6.1 years and 2.6 years, P < 0.001). However, even when we looked only at patients who received curative treatment, patients assigned by BCLC still had significantly better median survival than HKLC (7.1 years vs 5.5 years, P = 0.037). This calls for further studies comparing the BCLC and HKLC staging systems to determine not just the prognostic predictability of the stages in each system, but the accuracy of the assignments as well.
In a review article by Maida et al[7], studies investigating the performance of different HCC staging systems then available in the literature were compared. The general trend was that staging systems developed in Western centers performed better when applied to Western populations. In particular, the BCLC staging system was the best prognostic model in studies conducted in Italy[15-18], Spain[19] and the United States[20]. These studies compared the BCLC against other staging systems, including those from Asia such as the Okuda staging system. Indeed, the converse was also true, as staging systems derived from Asian populations tended to be the best prognostic model when tested in cohorts from Asian countries[21-23]. The HKLC staging system represents a staging system developed from a large Asian population. Since its development, there have been studies evaluating its validity. Similar to the trends illustrated HKLC tends to perform better in Asian populations[24,25]. This was partly attributed to the predominance of hepatitis B in these Asian cohorts, as reflected in the study by Liu et al[25] that showed HKLC had better prognostic accuracy and therapeutic efficacy in hepatitis B-related HCC but not to hepatitis C-related HCC. Similarly, a study conducted by Adhoute et al[26] across two French centers, where hepatitis C and alcohol were the predominant etiologies, failed to show a better predictive value of HKLC compared to BCLC staging. In contrast, our study shows that the BCLC system is a better prognostic model than the HKLC system even though our population was of Asian ethnicity with predominantly hepatitis B-related HCC (Table 1).
A more recent study by Kim et al[8] looked individually at the BCLC and HKLC staging systems in a treatment-naïve Korean cohort, with the aim of investigating if survival is better if patients followed the recommended treatment by the respective staging systems. The findings in this study concurred with our study on 2 aspects: (1) the HKLC staging system could not direct therapy for a large proportion of patients; and (2) survival was better in general when patients in the early stages of either staging system received the recommended treatment, that is, curative therapy for HCC. However, our findings differ in that the BCLC staging system was able to direct curative treatment accurately for the vast majority (85.8%) of patients assigned to curative therapy groups, leading to drastically improved median survival times as demonstrated in Figure 5. This is in contrast to the findings by Kim et al[8], where only 49.5% and 55.6% of the population studied received the recommended therapy by BCLC and HKLC respectively. Moreover, our study compared the median survival of patients between the 2 staging systems when they were assigned to curative therapy, and further analyzed this trend when only patients who actually received the recommended curative treatment by either staging system were studied (Figure 6). In both instances, the BCLC staging system proved to be superior in predicting survival.
Our study has several limitations. Firstly, given the retrospective nature of this study, it was not possible to determine the exact reason why patients did not adhere to the treatments recommended by the BCLC and HKLC staging systems. We attempted to elucidate possible causes by examining differences in age, ECOG and Child-Pugh status between patients receiving and not receiving recommended curative treatment as assigned by the HKLC staging system. However, this cannot accurately pinpoint if the discrepancy was due to hesitancy on the part of the physicians to follow the treatment recommendations due to the clinical condition of the patient or patients declining curative treatment for other reasons, such as an unwillingness to accept the risks, financial constraints or social considerations. Moreover, it was also not possible to tell if other co-morbidities precluded certain curative treatment options, for example a patient with significant pulmonary hypertension or valvular heart disease would be a high risk candidate for surgery but still have a good ECOG and Child-Pugh status at the time of diagnosis of HCC. This was also the conclusion in the study by Selby et al[14], where nearly half of the patients did not follow treatment recommendations by either staging system due to patients’ personal and physicians’ professional decision. Secondly, therapies have evolved and so have the techniques and experience of physicians, surgeons and interventional radiologists over the three decades of our HCC registry. This could mean that the morbidity and mortality from the same treatment diminishes with time, given improvement in techniques and experience of the managing multidisciplinary team over the years, making accurate comparisons in survival difficult.
The strengths of this study are a large population of HCC patients that are well-characterized and studied over a long follow-up period. In addition, the survival data was robust as it is based on census by a national registry of deaths.
In summary, our study showed that the BCLC staging system performed better in predicting overall survival compared to the HKLC staging system in our cohort. This difference could be explained by the limitations in applying the more aggressive HKLC treatment recommendations in real life, as a lower proportion of patients than otherwise predicted by HKLC staging eventually received curative treatment. Moreover, the differences in survival when the survival analysis was performed according to patients receiving the recommended curative treatment highlight the need for continued refinement of these staging systems to ensure patients are appropriately directed to curative therapy, especially as new treatment modalities evolve and our collective experience in treating HCC increases.
We thank our colleagues from the Department of Gastroenterology and Hepatology, Singapore General Hospital, for allowing their patients to be enrolled and studied and staff from National Registry of Diseases Office, Ministry of Health, Singapore for assistance in providing data on survival census. We thank Mr Clement Lin for maintaining the HCC registry and for his help with the statistical analyses.
Hepatocellular carcinoma (HCC) is one of the leading causes of cancer-related mortality worldwide. It is important to accurately stage tumours according to patient characteristics, liver function and tumour extent, to determine the appropriate therapy. Both the Barcelona Clinic Liver Cancer (BCLC) and and newer Hong Kong Liver Cancer (HKLC) staging systems were developed for this purpose, although there are significant differences in the cohorts from which they were derived and the variations in treatment recommendations for different stages, in particular intermediate tumours. There have been limited large scale studies comparing the two staging systems in terms of their abilities to assign treatment recommendations accurately and for prognosis of survival.
The BCLC staging system has been criticised for being too heterogeneous in its definition of Stage B, as well as being overly conservative in its treatment recommendations. In contrast, the newer HKLC staging system offers a finer stratification into 5 main stages with Stages II to V having 2 sub-stages each, the treatment recommendations being tied closely to the 9 eventual stages from this algorithm. It is also arguably more aggressive in its curative treatment recommendations. With a more detailed algorithm derived from a larger cohort of patients and more aggressive treatment recommendations which have taken into account advances made in HCC research since the introduction of the BCLC staging system, it is intuitive to expect that the HKLC staging system will lead to better survival rates. However, this hypothesis still requires external validation. This study aimed to compare the abilities of the BCLC and HKLC staging systems to correctly assign patients to curative treatment groups in real life and to prognosticate survival when applied to patients with HCC from a multi-ethnic population with hepatitis B as the predominant etiology in the largest tertiary-level centre in Singapore.
The general trend from published studies investigating prognostic models in HCC shows that staging systems developed in Western centres tend to perform better when applied to Western study populations. The converse is also true, with more recent studies showing that HKLC tends to perform better in Asian populations but not necessarily in Western populations. This was partly attributed to the predominance of hepatitis B as the underlying etiology in Asian populations, which corresponds to the study population from which the HKLC staging system was derived. This study investigated a large cohort from an Asian population which was well-characterised and studied over a long follow-up period, with robust survival data based on an updated census by the national registry of deaths. It showed that the median overall survival in patients assigned to curative treatment by the BCLC staging system was significantly higher than those assigned to curative treatment by HKLC (6.1 and 2.6 years respectively, P < 0.001). Although a significantly higher proportion of patients in our study were assigned to curative treatment by HKLC compared to BCLC (43.9% vs 18.9% respectively, P < 0.01), BCLC was more accurate in directing therapy, with a significantly higher proportion of patients assigned to curative therapy receiving the recommended curative treatment compared to HKLC ( 85.8% vs 61.1%, P < 0.001). Thus, BCLC performed better than HKLC in terms of accuracy in assigning curative treatment and for prognosticating survival in a real-world setting. This could be due to the limitations in applying the more aggressive HKLC recommendations in real life, as reflected by the lower proportion of patients who eventually received curative treatment after being assigned to receive curative therapy by this staging system. Moreover, when only patients who received the recommended curative treatment were compared, BCLC still predicted better overall survival than HKLC (median survival 7.1 and 5.5 years respectively, P = 0.037).
This study highlights the need for continued refinement of the different staging systems for HCC to ensure that patients most likely to benefit from curative therapy are appropriately as such. This is especially true as new treatment modalities evolve and our collective understanding of HCC increases.
The topic is one of great interest today. They would insist more about the fact that the criteria raised in the HKLC system remain to be further adjusted and verified. The BCLC system, although widely used was created based on several small Western cohorts of patients with predominant alcoholic liver disease and hepatitis C related HCC. The system which links stage stratification with corresponding therapeutic recommendations was criticized for being too restrictive, having in mind for example, that liver resection is recommended only to the patients with early stage tumors, or the fact that patients with cancer- related symptoms should be classified as advanced HCC. More, recent papers argue that this system is indeed able to provide accurate outcome prediction and treatment recommendations for HCC patients with hepatitis B virus as the predominant etiology. The HKLC staging system recently proposed has been show to achieve better prognostic ability and to identify subsets of patients for more aggressive treatment (intermediate and advanced stage patients) in Eastern population, with hepatitis B as main etiology. The improved stratification of the patients with intermediate-to-advanced stage using the triad of tumor size, number of nodules and tumor thrombus seems to offer to this patients with multiple tumors the possibility to achieve a better outcome if they receive hepatic resection following HKLC criteria. It worth mentioning that this is still a controversial point, if they keep in mind regarding the patients with multiple tumors the problem of cancer genetic heterogeneity.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Singapore
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Preda CM S- Editor: Qi Y L- Editor: A E- Editor: Wang CH
| 1. | Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23762] [Cited by in RCA: 25504] [Article Influence: 1821.7] [Reference Citation Analysis (7)] |
| 2. | Bruix J, Llovet JM. Prognostic prediction and treatment strategy in hepatocellular carcinoma. Hepatology. 2002;35:519-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 837] [Cited by in RCA: 848] [Article Influence: 36.9] [Reference Citation Analysis (0)] |
| 3. | Santambrogio R, Salceda J, Costa M, Kluger MD, Barabino M, Laurent A, Opocher E, Azoulay D, Cherqui D. External validation of a simplified BCLC staging system for early hepatocellular carcinoma. Eur J Surg Oncol. 2013;39:850-857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Vitale A, Saracino E, Boccagni P, Brolese A, D’Amico F, Gringeri E, Neri D, Srsen N, Valmasoni M, Zanus G. Validation of the BCLC prognostic system in surgical hepatocellular cancer patients. Transplant Proc. 2009;41:1260-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Yau T, Tang VY, Yao TJ, Fan ST, Lo CM, Poon RT. Development of Hong Kong Liver Cancer staging system with treatment stratification for patients with hepatocellular carcinoma. Gastroenterology. 2014;146:1691-700.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 440] [Cited by in RCA: 540] [Article Influence: 49.1] [Reference Citation Analysis (0)] |
| 6. | Chen CH, Hu FC, Huang GT, Lee PH, Tsang YM, Cheng AL, Chen DS, Wang JD, Sheu JC. Applicability of staging systems for patients with hepatocellular carcinoma is dependent on treatment method--analysis of 2010 Taiwanese patients. Eur J Cancer. 2009;45:1630-1639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 64] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Maida M, Orlando E, Cammà C, Cabibbo G. Staging systems of hepatocellular carcinoma: a review of literature. World J Gastroenterol. 2014;20:4141-4150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 95] [Cited by in RCA: 89] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 8. | Kim KM, Sinn DH, Jung SH, Gwak GY, Paik YH, Choi MS, Lee JH, Koh KC, Paik SW. The recommended treatment algorithms of the BCLC and HKLC staging systems: does following these always improve survival rates for HCC patients? Liver Int. 2016;36:1490-1497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 9. | Singapore Cancer Registry Report No. 8. Trends in cancer incidence in Singapore 2010-2014. : National Registry of Diseases Office 2015; . |
| 10. | Li WJ, Goh BG, Lin YC, Tan CK. Changing epidemiology of hepatocellular carcinoma in Singapore – a study of 1,401 cases over 3 decades. : AASLD 2016; . |
| 11. | Bolondi L, Burroughs A, Dufour JF, Galle PR, Mazzaferro V, Piscaglia F, Raoul JL, Sangro B. Heterogeneity of patients with intermediate (BCLC B) Hepatocellular Carcinoma: proposal for a subclassification to facilitate treatment decisions. Semin Liver Dis. 2012;32:348-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 301] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 12. | Pecorelli A, Lenzi B, Gramenzi A, Garuti F, Farinati F, Giannini EG, Ciccarese F, Piscaglia F, Rapaccini GL, Di Marco M. Curative therapies are superior to standard of care (transarterial chemoembolization) for intermediate stage hepatocellular carcinoma. Liver Int. 2017;37:423-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 13. | Kim BK, Kim SU, Park JY, Kim DY, Ahn SH, Park MS, Kim EH, Seong J, Lee DY, Han KH. Applicability of BCLC stage for prognostic stratification in comparison with other staging systems: single centre experience from long-term clinical outcomes of 1717 treatment-naïve patients with hepatocellular carcinoma. Liver Int. 2012;32:1120-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Selby LK, Tay RX, Woon WW, Low JK, Bei W, Shelat VG, Pang TC, Junnarkar SP. Validity of the Barcelona Clinic Liver Cancer and Hong Kong Liver Cancer staging systems for hepatocellular carcinoma in Singapore. J Hepatobiliary Pancreat Sci. 2017;24:143-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Grieco A, Pompili M, Caminiti G, Miele L, Covino M, Alfei B, Rapaccini GL, Gasbarrini G. Prognostic factors for survival in patients with early-intermediate hepatocellular carcinoma undergoing non-surgical therapy: comparison of Okuda, CLIP, and BCLC staging systems in a single Italian centre. Gut. 2005;54:411-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 185] [Article Influence: 9.3] [Reference Citation Analysis (1)] |
| 16. | Cillo U, Bassanello M, Vitale A, Grigoletto FA, Burra P, Fagiuoli S, D’Amico F, Ciarleglio FA, Boccagni P, Brolese A. The critical issue of hepatocellular carcinoma prognostic classification: which is the best tool available? J Hepatol. 2004;40:124-131. [PubMed] |
| 17. | Cillo U, Vitale A, Grigoletto F, Farinati F, Brolese A, Zanus G, Neri D, Boccagni P, Srsen N, D’Amico F. Prospective validation of the Barcelona Clinic Liver Cancer staging system. J Hepatol. 2006;44:723-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 307] [Cited by in RCA: 329] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 18. | Guglielmi A, Ruzzenente A, Pachera S, Valdegamberi A, Sandri M, D’Onofrio M, Iacono C. Comparison of seven staging systems in cirrhotic patients with hepatocellular carcinoma in a cohort of patients who underwent radiofrequency ablation with complete response. Am J Gastroenterol. 2008;103:597-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | Pascual S, Zapater P, Such J, García-Herola A, Sempere L, Irurzun J, Palazón JM, Carnicer F, Pérez-Mateo M. Comparison of staging systems to predict survival in hepatocellular carcinoma. Liver Int. 2006;26:673-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 20. | Marrero JA, Fontana RJ, Barrat A, Askari F, Conjeevaram HS, Su GL, Lok AS. Prognosis of hepatocellular carcinoma: comparison of 7 staging systems in an American cohort. Hepatology. 2005;41:707-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 478] [Cited by in RCA: 474] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 21. | Toyoda H, Kumada T, Kiriyama S, Sone Y, Tanikawa M, Hisanaga Y, Yamaguchi A, Isogai M, Kaneoka Y, Washizu J. Comparison of the usefulness of three staging systems for hepatocellular carcinoma (CLIP, BCLC, and JIS) in Japan. Am J Gastroenterol. 2005;100:1764-1771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Nanashima A, Sumida Y, Abo T, Shindou H, Fukuoka H, Takeshita H, Hidaka S, Tanaka K, Sawai T, Yasutake T. Modified Japan Integrated Staging is currently the best available staging system for hepatocellular carcinoma patients who have undergone hepatectomy. J Gastroenterol. 2006;41:250-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 23. | Kondo K, Chijiiwa K, Nagano M, Hiyoshi M, Kai M, Maehara N, Ohuchida J, Nakao H, Ohkuwa Y. Comparison of seven prognostic staging systems in patients who undergo hepatectomy for hepatocellular carcinoma. Hepatogastroenterology. 2007;54:1534-1538. [PubMed] |
| 24. | Yan X, Fu X, Cai C, Zi X, Yao H, Qiu Y. Validation of models in patients with hepatocellular carcinoma: comparison of Hong Kong Liver Cancer with Barcelona Clinic Liver Cancer staging system in a Chinese cohort. Eur J Gastroenterol Hepatol. 2015;27:1180-1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 25. | Liu PH, Hsu CY, Lee YH, Su CW, Hsia CY, Huang YH, Chiou YY, Lin HC, Huo TI. Hong Kong Liver Cancer Staging System Is Associated With Better Performance for Hepatocellular Carcinoma: Special Emphasis on Viral Etiology. Medicine (Baltimore). 2015;94:e1772. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 26. | Adhoute X, Penaranda G, Bronowicki JP, Raoul JL. Usefulness of the HKLC vs. the BCLC staging system in a European HCC cohort. J Hepatol. 2015;62:492-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |