Published online May 14, 2017. doi: 10.3748/wjg.v23.i18.3309
Peer-review started: January 5, 2017
First decision: January 19, 2017
Revised: February 1, 2017
Accepted: March 30, 2017
Article in press: March 30, 2017
Published online: May 14, 2017
Processing time: 131 Days and 5.3 Hours
To verify the hypothesis that the Ling classification describes the endoscopic progressive process of achalasia and determine the ability of successful peroral endoscopic myotomy (POEM) to prevent endoscopic progression of achalasia.
We retrospectively reviewed the endoscopic findings, symptom duration, and manometric data in patients with achalasia. A total of 359 patients (197 women, 162 men) with a mean age of 42.1 years (range, 12-75 years) were evaluated. Symptom duration ranged from 2 to 360 mo, with a median of 36 mo. Patients were classified with Ling type I (n = 119), IIa (n = 106), IIb (n = 60), IIc (n = 60), or III (n = 14), according to the Ling classification. Of the 359 patients, 349 underwent POEM, among whom 21 had an endoscopic follow-up for more than 2 years. Pre-treatment and post-treatment Ling classifications of these 21 patients were compared.
Symptom duration increased significantly with increasing Ling classification (from I to III) (P < 0.05), whereas lower esophageal sphincter pressure decreased with increasing Ling type (from I to III) (P < 0.05). There was no difference in sex ratio or onset age among the Ling types, although the age at time of diagnosis was higher in Ling types IIc and III than in Ling types I, IIa, and IIb. Of the 21 patients, 19 underwent high-resolution manometry both before and after treatment. The mean preoperative and postoperative lower esophageal sphincter pressure were 34.6 mmHg (range, 15.3-59.4 mmHg) and 15.0 mmHg (range, 2.1-21.6 mmHg), respectively, indicating a statistically significant decrease after POEM. All of the 21 patients were treated successfully by POEM (postoperative Eckardt score ≤ 3) and still had the same Ling type during a mean follow-up period of 37.8 mo (range, 24-51 mo).
The Ling classification represents the endoscopic progressive process of achalasia and may be able to serve as an endoscopic assessment criterion for achalasia. Successful POEM (Eckardt score ≤ 3) seems to have the ability to prevent endoscopic evolvement of achalasia. However, studies with larger populations are warranted to confirm our findings.
Core tip: Achalasia is a progressive disease, as verified by manometric and radiographic findings. Thus, we speculated that this progressive process could be visualized by endoscopy. We have proposed the Ling classification for achalasia on the basis of the endoscopic morphological severity of the esophagus. This study supports the hypothesis that the Ling classification portrays the progressive process of achalasia. Preliminary evidence suggests that successful peroral endoscopic myotomy (POEM) has the ability to prevent endoscopic progression of achalasia. Moreover, this study suggests that the Ling classification may serve as a criterion for endoscopic assessment of achalasia and will be useful for long-term endoscopic follow-up of post-POEM achalasia.
- Citation: Zhang WG, Linghu EQ, Chai NL, Li HK. Ling classification describes endoscopic progressive process of achalasia and successful peroral endoscopy myotomy prevents endoscopic progression of achalasia. World J Gastroenterol 2017; 23(18): 3309-3314
- URL: https://www.wjgnet.com/1007-9327/full/v23/i18/3309.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i18.3309
Achalasia is a rare esophageal motility disorder characterized by symptoms of dysphagia, regurgitation, weight loss, and chest pain[1,2]. Achalasia is a progressive disease, as demonstrated by manometric and radiographic findings[3]. Thus, it can be inferred that there is also a progressive process of achalasia as revealed by endoscopy. Dr. En-Qiang Linghu has proposed the Ling classification for achalasia based on the endoscopic morphological severity of the esophagus. We hypothesized that the Ling classification could be used to describe the endoscopic progressive process of achalasia.
Peroral endoscopic myotomy (POEM) has been shown to be an effective and safe procedure for achalasia and is quickly becoming one of the first-line therapies for achalasia[4-6]. However, it remains unclear whether this procedure can prevent endoscopic progression of achalasia. Criteria to assess long-term endoscopic follow-up of post-POEM achalasia are still lacking. The present study aimed to verify the hypothesis that the Ling classification depicts the endoscopic progressive process of achalasia and to determine the ability of successful POEM to prevent the endoscopic evolvement of achalasia.
A total of 359 patients (197 women and 162 men) with a mean age of 42.1 years (range, 12-75 years) were evaluated. High-resolution manometry (HRM), endoscopy, and barium swallow were performed to confirm the diagnosis of achalasia. The duration of symptoms ranged from 2 to 360 mo, with a median of 36 mo. Patients were classified with Ling type I, IIa, IIb, IIc, or III, according to the Ling classification[7]. Duration of symptoms and lower esophageal sphincter pressure (LESP) were compared among the five Ling types. Of the 359 patients, 349 underwent POEM, among whom 21 had an endoscopic follow-up for more than 2 years. Pre-treatment and post-treatment Ling types of the 21 patients with long-term follow-up were compared.
Dr. Linghu proposed the Ling classification in 2011 and published it in 2013[7]. The Ling classification includes three types: type I, no multi-ring, crescent-like structure or diverticulum structure; type II, the presence of multi-ring or crescent-like structure but without diverticulum structure; and type III, the presence of diverticulum structure. Type II was further classified into three subtypes: IIa, IIb and IIc. The criteria for classifying Ling type II subtypes were as follows: Ling IIa, the presence of multi-ring structure; Ling IIb, the presence of crescent-like structure and the midpoint of its inner edge not larger than 1/3 of the esophageal lumen; Ling IIc, the presence of crescent-like structure and the midpoint of its inner edge over 1/3 of the esophageal lumen (Figure 1). The endoscopy reports of all 359 patients were collected and classified according to the diagnostic information by two endoscopists (Li HK and Linghu EQ), according to the criteria mentioned above. Of note, both endoscopists were blinded to the other data collected from each patient.
The duration of symptoms for each of the 359 patients was collected from medical records. The definition used for the appearance of symptoms was dysphagia or chest pain for ≥ 4 d of the week. All patients had been inquired about case history based on the definition mentioned above.
HRM was performed using the following protocol: a 36-channel, solid-state catheter system with high-fidelity circumferential sensors at 1-cm intervals (Manosacn; Sierra Scientific Instruments Inc, LosAngeles, CA, United States) was advanced through the nasal canal. Studies were performed with patients in a supine position after at least a 6-h fast. Pressure data of 10 wet swallows were recorded and analyzed using a dedicated computerized analysis system.
During the procedure, patients were kept in the supine position with the right shoulder elevated. General anesthesia was administered while the patient’s respirations, blood pressure, oxygen saturation, and electrocardiogram were monitored. An additional cap attached at the top of the endoscope was required. Then, POEM was performed as follows. First, a submucosal injection of methylene blue saline solution (1:10000) was administered, and a mucosal incision was made at the right posterior esophageal wall, approximately 6-10 cm from the gastroesophageal junction (GEJ). Then, a submucosal tunnel was established, passing over the GEJ and about 2-3 cm into the proximal stomach. Myotomy started at 2 cm distal to the incision and extended 2-3 cm into the stomach. After complete hemostasis and ensuring that an endoscope could easily pass the cardia of the stomach, the mucosal incision was sutured with approximately 5 hemostatic clips.
Patients were scheduled for a follow-up visit at 3 mo, 6 mo, and 1 year postoperatively, and yearly afterwards. Endoscopy, HRM, and 24-h esophageal pH monitoring were required at each follow-up.
All statistical analyses were performed using SPSS software version 17.0. Variables are expressed as mean or median. The Kruskal-Wallis test or single factor analysis of variance was used to compare the onset age, age at time of diagnosis, duration of symptoms, and LESP among the five Ling types. χ2 test was used to compare the sex ratio among the five Ling types. All reported P-values are two-tailed, with P-values < 0.05 considered statistically significant.
As shown in Table 1, a total of 359 patients (197 women and 162 men) with a mean age of 42.1 years (range, 12-75 years) were evaluated. The duration of symptoms ranged from 2 to 360 mo, with a median of 36 mo. Of the 359 patients, 119 were classified with Ling I, 106 with Ling IIa, 60 with Ling IIb, 60 with Ling IIc, and 14 with Ling III.
| Characteristic | Value |
| Sex, female/male (n) | 197/162 |
| Age (yr), mean (range) | 42.1 (12-75) |
| Duration of symptoms (mo), median (range) | 36 (2-360) |
| Lower esophageal sphincter pressure (mmHg), mean (range) | 33.0 (0.7-72.4) |
| Ling classification | |
| I | 119 (33.1) |
| IIa | 106 (29.5) |
| IIb | 60 (16.7) |
| IIc | 60 (16.7) |
| III | 14 (3.9) |
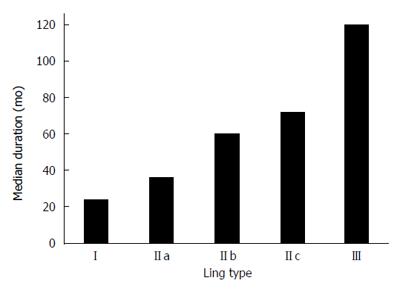
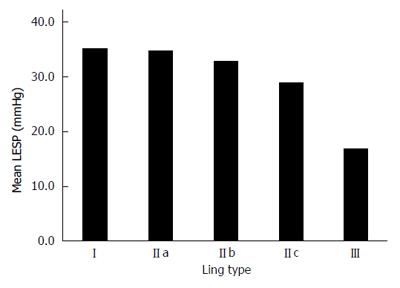
The duration of symptoms increased significantly when the Ling classification increased (from I to III) (P < 0.05), as shown in Figure 2. LESP decreased with increasing Ling classification (from I to III) (P < 0.05) as shown in Figure 3. There was no difference in sex ratio or onset age among the Ling types, although the age at time of diagnosis was higher in Ling types IIc and III than in Ling types I, IIa, and IIb (Table 2).
| Ling type | I | IIa | IIb | IIc | III | P value |
| n | 119 | 106 | 60 | 60 | 14 | |
| Onset age (yr), mean | 35.3 | 38.9 | 36.1 | 36.4 | 32.9 | > 0.05 |
| Age at time of diagnosis (yr), mean | 38.5 | 42.8 | 43.8 | 46.4 | 45.4 | < 0.05 |
| Sex (female/male) | 65/54 | 60/46 | 32/28 | 35/25 | 5/9 | > 0.05 |
| Duration (mo), median | 24 | 36 | 60 | 72 | 120 | < 0.05 |
| LESP (mmHg), mean | 35 | 34.7 | 32.8 | 28.9 | 16.9 | < 0.05 |
Of the 359 patients, 349 underwent POEM, among whom 21 had an endoscopic follow-up longer than 2 years. The demographics and treatment outcomes of the 21 patients (9 women, 12 men) with a post-POEM follow-up more than 2 years are shown in Table 3. Of the 21 patients, 8 were classified with Ling type I preoperatively, 7 with Ling type IIa, 5 with Ling type IIb, and 1 with Ling type III. Of the 21 patients, 19 had HRM both before and after treatment. The mean preoperative and postoperative LESP were 34.6 mmHg (range, 15.3-59.4 mmHg) and 15.0 mmHg (range, 2.1-21.6 mmHg), respectively, indicating a statistically significant decrease after POEM. All of the 21 patients were treated successfully by POEM (postoperative Eckardt score ≤ 3) and still had the same Ling type during a mean follow-up period of 37.8 mo (range, 24-51 mo).
| Characteristic | Value |
| Sex, female/male (n) | 9/12 |
| Age (yr), mean (range) | 43.8 (16-62) |
| Duration of symptoms (mo), median (range) | 36 (6-120) |
| Endoscopic follow-up (mo), mean (range) | 37.8 (24-51) |
| Manometry follow-up rate | 19 (90.5) |
| Lower esophageal sphincter pressure (mmHg), mean (range) | |
| Pre-treatment | 34.6 (15.3-59.4) |
| Post-treatment | 15.0 (2.1-21.6) |
| Ling classification | |
| I | 8 (38.1) |
| IIa | 7 (33.3) |
| IIb | 5 (23.8) |
| IIc | 0 (0) |
| III | 1 (4.8) |
| Treatment success rate (Eckardt score ≤ 3) | 21 (100) |
Achalasia is a progressive disorder as measured by manometric and radiographic findings[3]. Thus, there should exist a progressive process of achalasia as visualized by endoscopy. We have previously proposed the Ling classification for achalasia based on the endoscopic morphological severity of the esophagus[7]. Therefore, we hypothesized that the Ling classification can be used to assess the endoscopic progressive process of achalasia. The present study provided evidence supporting this hypothesis by comparing the duration of symptoms and LESP among the different Ling types.
Shiino et al[3] published a study in which patients with achalasia were divided into four groups according to the duration of symptoms: less than 5 years; 5 to 10 years; 10 to 15 years, and 15 years or longer. This study found that the tortuosity of the esophagus, as measured by the maximal angle of the esophageal axis on radiography, was significantly greater in patients with a longer duration of symptoms (P < 0.02). Henderson[8] classified achalasia into three stages according to the degree of esophageal dilatation on X-ray. Stage 1 has a diameter less than 4 cm, stage 2 has a diameter of 4-6 cm, and stage 3 has a diameter greater than 6 cm. A greater degree of esophageal dilation was shown to be related to the duration of symptoms. The present study found that duration of symptoms increased significantly for every type using the Ling classification (from I to III) (P < 0.05). Given that morphological severity of the esophagus increases from Ling type I to Ling type III, the results of the present study are compatible with both Yutaka’s and Henderson’s studies. However, while these previous studies were based on radiography, the present study was able to evaluate the endoscopic progressive process of achalasia by direct visualization.
LESP decreased with increasing Ling classification (from I to III) (P < 0.05). Shiino et al[3] reported that LESP decreased as the duration of symptoms increased, although the results were not significant. Given that the present study confirmed the association between longer duration of symptoms and increasing Ling classification (from I to III) (P < 0.05), the results of the present study and Yutaka’s support each other. However, the association between decreasing LESP with increasing symptom duration still requires to be confirmed by a further prospective study.
POEM was first reported as a treatment for achalasia in 2010[9] and has developed rapidly since then. Despite the evidence that POEM is effective and safe, it remains unclear whether the esophageal morphology in achalasia patients changes postoperatively. In the present study, a total of 21 patients had an endoscopic follow-up period more than 2 years after POEM. All 21 patients had their achalasia successfully treated (Eckardt score ≤ 3) and still had the same Ling type throughout a mean follow-up period of 37.8 mo (range, 24-51 mo), suggesting that POEM may prevent the endoscopic progression of achalasia. However, the sample size (21 patients) of our analysis was relatively small because most of the 349 patients who underwent POEM at our hospital did not undergo endoscopic follow-up beyond two years postoperatively. Thus, a prospective study with a larger sample is required to further confirm the conclusions based on the results above. Another limitation is that there is a lack of criteria to assess endoscopic follow-up of post-POEM achalasia. Furthermore, given that POEM has been utilized for only 6 years, the long-term (≥ 7 years) efficacy, especially with regard to esophageal morphology changes, remains uncertain. The Ling classification may be a good choice of criteria to endoscopically assess post-POEM achalasia.
Performing POEM for advanced achalasia, such as Ling types IIc-III or sigmoid-type achalasia, is more challenging. Thus, patients with achalasia should undergo POEM soon after diagnosis because of the progressive nature of the disease, which has been confirmed in previous studies and the present study[3].
One limitation to our study was the retrospective nature of our methods; however, the Ling classification, duration of symptoms, and LESP were recorded prospectively. Another limitation was that only 21 patients had an endoscopic follow-up for more than 2 years. To the best of our knowledge, this is the first study reporting the long-term postoperative esophageal morphological changes as visualized by endoscopy in patients with achalasia.
In conclusion, the Ling classification captures the endoscopic progressive process of achalasia and might be able to serve as criteria to assess achalasia endoscopically. Successful POEM may prevent the endoscopic evolvement of achalasia. However, future longitudinal studies with larger samples are warranted.
It has been proved that achalasia is a progressive disease, as verified by manometric and radiographic findings. Based on this knowledge, it could be speculated that there is also an endoscopic progressive process of achalasia.
The authors have proposed the Ling classification for achalasia in 2011, based on the endoscopic morphological severity of the esophagus. Therefore, they speculated that Ling classification represents the endoscopic progressive process of achalasia.
The authors confirmed that the Ling classification describes the endoscopic progressive process of achalasia. Moreover, to the best of this knowledge, this was the first study reporting the long-term postoperative esophageal morphological changes as revealed by endoscopy in patients with achalasia.
After being confirmed to have the ability to represent the endoscopic progressive process of achalasia, Ling classification might be able to serve as criteria to assess achalasia endoscopically.
Ling classification, an endoscopic classification for achalasia based on the morphological severity of the esophagus, was proposed by Professor Linghu in 2011. Peroral endoscopic myotomy, a recently developed endoscopic therapeutic technique, is performed for achalasia.
The present manuscript is related to Ling classification and the endoscopic progressive process of achalasia. Besides, successful POEM seems to have the ability to prevent the endoscopic evolvement of achalasia. The study demonstrated that the Ling classification does work.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Chow WK, Lee CL S- Editor: Gong ZM L- Editor: Wang TQ E- Editor: Wang CH
| 1. | Richter JE. Oesophageal motility disorders. Lancet. 2001;358:823-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 180] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 2. | Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet. 2014;383:83-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 390] [Cited by in RCA: 428] [Article Influence: 38.9] [Reference Citation Analysis (0)] |
| 3. | Shiino Y, Houghton SG, Filipi CJ, Awad ZT, Tomonaga T, Marsh RE. Manometric and radiographic verification of esophageal body decompensation for patients with achalasia. J Am Coll Surg. 1999;189:158-163. [PubMed] |
| 4. | Familiari P, Gigante G, Marchese M, Boskoski I, Tringali A, Perri V, Costamagna G. Peroral Endoscopic Myotomy for Esophageal Achalasia: Outcomes of the First 100 Patients With Short-term Follow-up. Ann Surg. 2016;263:82-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 113] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 5. | Shiwaku H, Inoue H, Yamashita K, Ohmiya T, Beppu R, Nakashima R, Takeno S, Sasaki T, Nimura S, Yamashita Y. Peroral endoscopic myotomy for esophageal achalasia: outcomes of the first over 100 patients with short-term follow-up. Surg Endosc. 2016;30:4817-4826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 6. | Von Renteln D, Fuchs KH, Fockens P, Bauerfeind P, Vassiliou MC, Werner YB, Fried G, Breithaupt W, Heinrich H, Bredenoord AJ. Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology. 2013;145:309-311.e1-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 265] [Cited by in RCA: 246] [Article Influence: 20.5] [Reference Citation Analysis (1)] |
| 7. | Li HK, Linghu EQ. New endoscopic classification of achalasia for selection of candidates for peroral endoscopic myotomy. World J Gastroenterol. 2013;19:556-560. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Henderson RD. Esophageal motor disorders. Surg Clin North Am. 1987;67:455-474. [PubMed] |
| 9. | Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1168] [Cited by in RCA: 1233] [Article Influence: 82.2] [Reference Citation Analysis (1)] |