Published online Apr 28, 2017. doi: 10.3748/wjg.v23.i16.2964
Peer-review started: December 31, 2016
First decision: January 19, 2017
Revised: February 10, 2017
Accepted: March 30, 2017
Article in press: March 30, 2017
Published online: April 28, 2017
Processing time: 124 Days and 6.8 Hours
To report our one-year experience with computer assisted propofol sedation (CAPS) for colonoscopy as the first United States Medical Center to adopt CAPS technology for routine clinical use.
Between September 2014 and August 2015, 2677 patients underwent elective outpatient colonoscopy with CAPS at our center. All colonoscopies were performed by 1 of 17 gastroenterologists certified in the use of the CAPS system, with the assistance of a specially trained nurse. Procedural success rates, polyp detection rates, procedure times and recovery times were recorded and compared against corresponding historical measures from 2286 colonoscopies done with midazolam and fentanyl from September 2013 to August 2014. Adverse events in the CAPS group were recorded.
The mean age of the CAPS cohort was 59.9 years (48.7% male); 31.3% were ASA I, 67.3% ASA II and 1.4% ASA III. 45.1% of the colonoscopies were for screening, 31.5% for surveillance, and 23.4% for symptoms. The mean propofol dose administered was 250.7 mg (range 16-1470 mg), with a mean fentanyl dose of 34.1 mcg (0-100 mcg). The colonoscopy completion and polyp detection rates were similar to that of historical measures. Recovery times were markedly shorter (31 min vs 45.6 min, P < 0.001). In CAPS patients, there were 20 (0.7%) cases of mild desaturation (< 90%) treated with a chin lift and reduction or temporary discontinuation of the propofol infusion, 21 (0.8%) cases of asymptomatic hypotension (< 90 systolic blood pressure) treated with a reduction in the propofol rate, 4 (0.1%) cases of marked agitation or discomfort due to undersedation, and 2 cases of pronounced transient desaturation requiring brief (< 1 min) mask ventilation. There were no sedation-related serious adverse events such as emergent intubation, unanticipated hospitalization or permanent injury.
CAPS appears to be a safe, effective and efficient means of providing moderate sedation for colonoscopy in relatively healthy patients. Recovery times were much shorter than historical measures. There were few adverse events, and no serious adverse events, related to CAPS.
Core tip: As the first United States Medical Center to adopt computer assisted propofol sedation (CAPS) technology for routine clinical use, we report our one-year experience with CAPS for colonoscopy. Between September 2014 and August 2015, 2677 patients underwent colonoscopy with CAPS. The colonoscopy completion and polyp detection rates were similar to that of historical controls who received midazolam and fentanyl sedation. Procedure and recovery times were shorter. In CAPS patients, there were only 2 cases of desaturation requiring mask ventilation, and no sedation-related serious adverse events. In conclusion, CAPS is a safe, effective and efficient means of providing moderate sedation for colonoscopy.
- Citation: Lin OS, La Selva D, Kozarek RA, Tombs D, Weigel W, Beecher R, Koch J, McCormick S, Chiorean M, Drennan F, Gluck M, Venu N, Larsen M, Ross A. One year experience with computer-assisted propofol sedation for colonoscopy. World J Gastroenterol 2017; 23(16): 2964-2971
- URL: https://www.wjgnet.com/1007-9327/full/v23/i16/2964.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i16.2964
In the United States, the administration of propofol sedation for gastrointestinal endoscopy has been fraught with controversy, primarily around the issues of reimbursement and privileging. Although most endoscopic procedures can be done with moderate sedation using midazolam and fentanyl (MF), propofol sedation carries distinct advantages, including more effective sedation and faster patient recovery[1]. In the United States, propofol is almost always administered by anesthesia professionals, with a vast increase in the incidence of propofol use over the past decade for routine outpatient endoscopic procedures in low-risk patients[2,3]. The use of anesthesiologist-administered propofol for low-risk endoscopies is estimated to cost the United States Health Care System hundreds of millions of dollars per year[4]. As a response, there have been attempts to introduce nurse-administered propofol sedation (NAPS). NAPS has been shown to be feasible and safe[5-7], but there are significant barriers to its use in the United States, including the FDA labeling for propofol (which specifies that propofol must be administered by personnel trained in anesthesia), insurance regulations, hospital credentialing rules and medicolegal concerns[8].
Computer assisted propofol sedation (CAPS) was approved by the FDA in 2013 as a means to provide moderate sedation for American Society of Anesthesiology (ASA) class I and II patients undergoing routine upper endoscopy and colonoscopy. CAPS allows non-anesthesiologists to administer a continuous propofol infusion after a single premedication dose of fentanyl. As the only endoscopy unit in the United States to introduce CAPS for large-scale clinical use, we report our one-year experience with CAPS for colonoscopy on a large cohort of low-risk patients, compared against similar historical controls who underwent colonoscopy using traditional MF sedation in the 12 mo immediately preceding the start of our CAPS usage.
In September 2014, our unit introduced CAPS (SEDASYS, Ethicon Endosurgery, Cincinnati, OH, United States) into our Seattle facility for routine, non-emergent, outpatient colonoscopies in relatively healthy, low-risk patients. All procedures were performed by one of 17 board certified, ACLS-certified, highly experienced attending gastroenterologists who had undergone mandatory formal training in use of the CAPS system. A specially trained nurse maintained or changed the infusion rate by controlling the CAPS device, according to verbal orders issued by the endoscopist; a technician was also present in the room to provide procedural support, such as when polypectomy was performed. An anesthesia professional was immediately available in the same building for assistance as needed.
The CAPS system continuously monitors multiple parameters, including capnography, oxygen saturation, EKG and blood pressure. In addition, the CAPS system periodically assesses patient alertness by automated response monitoring (ARM). With ARM, patients grip a plastic device during the procedure, and are prompted by voice and vibration prompts from the CAPS system every 3-5 min to squeeze the device. In patients with cognitive or language difficulties, ARM can be replaced by clinician response mode (CRM), whereby the nurse is prompted every 3-5 min by the CAPS system to assess the level of patient responsiveness and inputs that data into the system.
At the discretion of the endoscopist, intravenous fentanyl (a single bolus of 25-100 mcg) can be given to patients 3 min prior to the initiation of the 1% propofol infusion. The initial infusion rate is set by the endoscopist and must be between 25-75 mcg/kg per minute. To achieve a suitable level of sedation, the endoscopist can titrate the maintenance infusion rate upwards or downwards during the procedure, and can give intermittent boluses as needed. The CAPS system has multiple built-in safety measures: Each rate increase cannot be more than 50 mcg/kg per minute, the absolute maximum infusion rate cannot be more than 200 mcg/kg per minute, and boluses cannot be more than 0.25 mg/kg. Hypoventilation, oxygen desaturation, apnea or lack of patient responsiveness, manifesting as long lag times before the patient squeezes the ARM hand grip device (or inability to squeeze the device), will prevent further infusion rate increases or administration of boluses, and, if severe enough, can lead the CAPS system to decrease or discontinue the propofol infusion (the CAPS system can never unilaterally increase the infusion rate). To prevent a stacking effect, there is a 180 s lockout period after each infusion rate increase (during which further rate increases cannot occur), and a 90 s lockout after each bolus. Finally, as an additional safety measure, if the CAPS system detects hypoventilation, apnea or hypoxia it will automatically increase supplemental oxygen delivery to the patient and trigger visual and auditory alarms to alert the provider team.
Between September 1, 2014, and August 31, 2015, all patients who underwent colonoscopy with CAPS in our endoscopy unit were included in the study cohort. All CAPS procedures were performed in our downtown Seattle Buck Endoscopy Unit, which focuses exclusively on low-risk (mostly ASA I or II) out-patients with no major comorbidities. Sicker out-patients, as well as in-patients and those undergoing complex procedures, were assigned to our Jones Endoscopy Unit and did not receive CAPS. None of the CAPS patients had chronic obstructive pulmonary disease or chronic heart failure, since we specifically excluded such patients from the CAPS experience. The few ASA III subjects in our study suffered from non-cardiopulmonary conditions (such as renal or liver disorders) that would not be expected to affect the safety of the procedure or sedation; CAPS was used off-label for these patients. There was a Body Mass Index cutoff of 40 for all CAPS and control patients.
For CAPS patients, all data (including adverse events) were prospectively collected as part of a quality control initiative. During the same period, we also performed approximately 900 upper endoscopies with CAPS, but the use of CAPS for upper endoscopic procedures poses unique challenges quite different from that of colonoscopy, and are discussed in a separate manuscript.
Since almost no outpatient procedures in our hospital were done with MF sedation after December 2014, we used a historical control group to determine if CAPS resulted in any improvements in procedural success rates, polyp detection rates, procedure times and recovery times. We abstracted data from similar low-risk controls who underwent colonoscopy using MF in our Buck Unit during the 12 mo immediately preceding the introduction of CAPS into our unit (September 1, 2013 to August 31, 2014). The same group of 17 endoscopists performed the colonoscopies in both groups. Since all endoscopic procedures at our center are documented using Provation software (Wolters Kluwer, Minneapolis, United States), retrospective automated extraction of endoscopic data on large numbers of patients was feasible. However, adverse events could not be retrospectively abstracted for the control group.
Institutional Review Board approval was obtained for this study (IRB 15060); individual informed consent was not required.
For each CAPS and control subject, the following information was extracted: (1) demographics (age and sex); (2) ASA class; (3) indication for colonoscopy (screening, surveillance or diagnostic); (4) propofol, midazolam and/or fentanyl dose; (5) polyp detection rates; (6) procedural success rates (colonoscopy completion rates) and the incidence of incomplete or aborted procedures due to sedation issues; (7) procedure times, defined as the time of endoscope insertion to the time of endoscope withdrawal from the patient; (8) recovery times, defined as the time of the patient’s arrival at the recovery room to the time of departure; and (9) level of consciousness upon arrival at the recovery unit. Level of consciousness was rated by nursing staff on a 6-point scale ranging from “Awake” to “Unresponsive”.
For CAPS subjects, sedation-related adverse events (defined as cardiopulmonary compromise during or immediately after the procedure) and serious adverse events (defined as any intra- or post-procedural perforation, bleeding requiring hospitalization or transfusion, or cardiopulmonary event resulting in mask ventilation, intubation, having to call anesthesia personnel for help emergently, permanent injury, hospitalization, or death) were also recorded.
The primary study endpoints included polyp detection rate, procedural success rate, procedure time, recovery time and level of consciousness upon arrival at the recovery unit, compared against historical controls. In addition, adverse events, sedation-related adverse events, and serious adverse events in CAPS subjects are also described, although comparative analysis could not be done because the adverse event rate in the historical control group was not available.
All comparative analysis was done using the Chi-squared test or Fisher’s exact test for proportions, and Student’s t-test or non-parametric Mann-Whitney U test for means. All statistical calculations were performed using SPSS 19.0 (SPSS Inc., Chicago, IL, United States). P values were 2 tailed. Because multiple comparisons were made for a total of 5 study endpoints, the statistical significance threshold was taken as P < 0.01 (0.05 divided by 5) in accordance with Bonferroni correction principles.
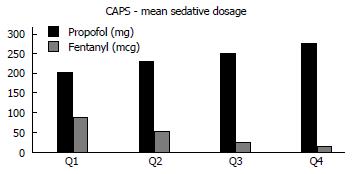
During the 12-mo study period, 2677 colonoscopies were performed with CAPS in our Seattle facility. The mean age of the CAPS cohort was 59.9 ± 11.7 years (48.7% male); 31.3% were ASA I, 67.3% ASA II and 1.4% ASA III. 45.1% of the colonoscopies were for screening, 31.5% for surveillance, and 23.4% for symptoms. The mean propofol dose administered was 250.7 ± 132 mg (range 16-1470 mg), with a mean fentanyl dose of 34.1 ± 14.6 mcg (0-100 mcg). In addition, there were 426 colonoscopies that were performed with CAPS as part of “double procedures” (upper endoscopies and colonoscopies done during the same session). For these CAPS “doubles”, the mean age was 57.6 ± 14.3 years (44.5% male); 25.9% were ASA I, 69.9% ASA II and 4.3% ASA III. As expected, sedative doses were significantly higher for double procedures as opposed to single colonoscopies (propofol 384.8 ± 180.2 mg vs 250.7 ± 132 mg and fentanyl 95.3 ± 11.5 mcg vs 34.1 ± 14.6 mcg; P < 0.001 for both). Temporal trend data showed that mean fentanyl doses decreased steadily with time as endoscopists found that fentanyl premedication was not needed to achieve adequate sedation, while propofol doses increased during the same time period to compensate for the absence of fentanyl (Figure 1).
In the 12 mo immediately preceding September 2014, there were 2286 historical controls who underwent colonoscopy alone with MF in our downtown facility. Their mean age was 60.3 ± 11.6 years (49.8% male); 46.4% were ASA I, 52.6% ASA II and 1.0% ASA III. 44.7% of these colonoscopies were for screening, 28.4% for surveillance, and 26.9% for symptoms. The mean midazolam dose administered was 4.8 ± 1.7 mg (range 1-16 mg) and mean fentanyl dose was 105.2 ± 32.9 mcg (25-425 mcg). There were also 417 colonoscopies performed with MF as part of “doubles”. For these patients, the mean age was 59.9 ± 14.0 years (41.7% male); 26.3% were ASA I, 68.4% ASA II and 5.3% ASA III. The mean midazolam dose was 6.8 ± 2.5 mg, with a mean fentanyl dose of 130.0 ± 41 mcg.
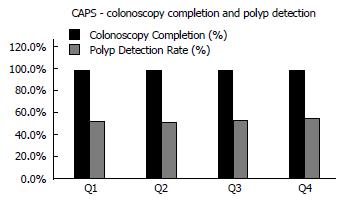
For CAPS patients who underwent colonoscopy as single procedures, the procedural completion rate was high (98.8%) and similar to that of historical controls (99.0%, P = 0.526) (Table 1). Polyp detection rates and large polyp detection rates were also similar to that of controls (53.4% vs 50.1% and 8.2% vs 8.2% respectively, P > 0.01 for both). There were no differences in colonoscopy completion rates and polyp detection rates between CAPS patients who underwent colonoscopy alone and CAPS patients who underwent colonoscopy as part of double procedures (data not shown). Temporal trend data showed that colonoscopy completion and polyp detection rates in the CAPS group were high right from the start of our experience with CAPS and remained high throughout the 12 mo study period (Figure 2).
| CAPS (n = 2677) | MF (n = 2286) | P value | |
| Mean age (yr) | 59.9 ± 11.7 | 60.3 ± 11.6 | 0.685 |
| Male sex | 48.7% | 49.8% | 0.427 |
| Colonoscopy completion rate | 98.8% | 99.0% | 0.526 |
| Polyp detection rate | 53.4% | 50.1% | 0.019 |
| Large (≥ 1 cm) polyp detection rate | 8.2% | 8.2% | 0.961 |
| Mean procedure time (min) | 22.2 ± 10.5 | 22.8 ± 9.3 | < 0.001 |
| Mean recovery time (min) | 31.0 ± 14.4 | 45.6 ± 17.9 | < 0.001 |
| Level of consciousness upon arrival at recovery unit - “Awake” | 83.3% | 49.2% | < 0.001 |
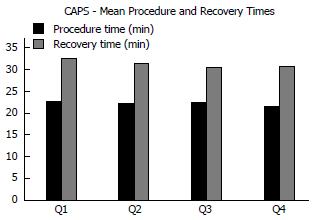
For patients who underwent colonoscopy alone, the mean procedure times were slightly shorter for the CAPS group than the historical controls (22.2 ± 10.5 vs 22.8 ± 9.3 min, P < 0.001). The maximum procedure time for the CAPS group was 125 min, vs 101 min for the controls. On the other hand, mean recovery times were markedly shorter (31.0 ± 14.4 min vs 45.6 ± 17.9 min, P < 0.001) (Table 1). In terms of level of consciousness on arrival at the recovery unit, 83.3% of CAPS subjects were recorded as “Awake” compared to 49.2% of the controls (P < 0.001) (Table 1). Despite the larger propofol doses given for doubles compared with colonoscopies done alone, there was no difference in recovery times between the two groups (31.7 ± 12.3 vs 31.0 ± 14.4, P = 0.368). On the other hand, the recovery time for CAPS colonoscopy done as part of “doubles” was much shorter than that of MF colonoscopy done as part of “doubles” (31.7 ± 12.3 vs 54.8 ± 23.3, P < 0.001). With regard to temporal trends, mean procedure and recovery times in CAPS patients were stable throughout the 12 mo study period (Figure 3).
In the CAPS group, there were 20 (0.7%) cases of mild oxygen desaturation (< 90%) treated with a chin lift and reduction or temporary discontinuation of the propofol infusion, 21 (0.8%) cases of asymptomatic hypotension (< 90 systolic blood pressure) treated with a reduction in the propofol rate, 4 (0.1%) cases of marked agitation or discomfort due to undersedation, and 2 cases of pronounced transient desaturation requiring brief (< 1 min) mask ventilation (including one that prompted the endoscopist to call for an anesthesiologist, although the latter did not perform any intervention because the patient recovered quickly). One patient who had presented with bloody diarrhea was diagnosed with ischemic colitis during the colonoscopy with CAPS, and died 14 d after the procedure despite surgical resection of the gangrenous colon. Aside from this delayed fatality, none of the subjects suffered any severe adverse event such as emergent intubation, unanticipated hospitalization, permanent injury or death. Sedation related complications were roughly evenly distributed throughout the 4 quartiles of our 12-mo study period (data not shown).
CAPS has the potential to allow for the safe, on-label availability of propofol sedation in the United States without the need for patients or their insurance plans to incur additional anesthesia-related costs. Despite considerable media attention, there still seems to be some misconceptions about this technology. The currently available CAPS system is not a “closed-loop” system. It can never increase drug delivery on its own; depending on patient physiology and responsiveness, the system may restrict, suspend, decrease or stop the propofol infusion, but any increase in drug delivery must be initiated by the clinician. In addition, CAPS is not a “target controlled” system. It does not control delivery based on the propofol concentration in the plasma or at the site of drug effect; instead, the infusion rate is determined by the clinician. Finally, CAPS is not a “patient-controlled sedation” system (analogous to patient-controlled analgesia pumps used in hospitalized patients), because the patient cannot directly change the infusion rate.
FDA approval for the currently available CAPS system was based on a large multi-center randomized controlled trial[9], in which 1000 (mostly ASA class I and II) adults undergoing routine colonoscopy or upper endoscopy were randomized to CAPS or MF. The investigators found that the area under the curve for oxygen desaturation (a composite measure of the frequency, severity and duration of hypoxic episodes) was significantly lower for the CAPS group. Furthermore, patient and endoscopist satisfaction were greater in the CAPS group, and CAPS subjects recovered much faster than the MF controls. The overall incidence of adverse events was 5.8% for CAPS versus 8.7% for MF; the CAPS group had only one subject with a desaturation complication compared with 27 in the control group. The only serious sedation-related adverse event occurred in a control patient who required transient mask ventilation.
As the first United States Medical Center to adopt CAPS for routine clinical use, we had a unique opportunity to assess the efficacy, safety and efficiency of CAPS for colonoscopy in a large number of patients over an extended period of time. We introduced two CAPS machines into our unit in September 2014, and once we confirmed that CAPS seemed to function well, we steadily increased our commitment to CAPS, such that by December 2014, almost all low-risk outpatient upper endoscopies and colonoscopies were being done by one of the seven CAPS systems deployed in our unit. We previously presented a non-randomized controlled study that represented the first three months of our experience with CAPS[10]. In this initial study involving 244 CAPS subjects and 328 MF controls who underwent upper endoscopy and/or colonoscopy, we found that procedural success rates and colonoscopic polyp detection rates were high and comparable between the CAPS and MF groups. The mean procedure times were also similar between the two groups. For CAPS, the mean recovery time was 26.4 min vs 39.1 min for MF (P < 0.001). For CAPS patients who underwent colonoscopy, 1 required transient mask ventilation for desaturation and 4 experienced asymptomatic hypotension or desaturation (that did not require any intervention other than reduction in the propofol rate). These adverse events rates were similar to that of the MF control group. For colonoscopy, CAPS was associated with higher patient satisfaction scores (according to validated satisfaction surveys) for sedation adequacy, the recovery process and global satisfaction, and much higher endoscopist satisfaction scores for ease of sedation administration, the recovery process and global satisfaction. As a follow-up to these encouraging initial results, we now present efficacy, efficiency and safety data on a much larger cohort of patients representing our first 12 mo of experience using CAPS for colonoscopy.
Similar to our previous study, we found that the procedural success rates in the CAPS group was high and comparable to that seen in the MF historical controls, demonstrating that CAPS delivered highly effective sedation for colonoscopy. Furthermore, the polyp detection rate and large polyp detection rate were also comparable to the controls, while procedure times were slightly faster. As expected, recovery times were much faster for CAPS patients than controls (31 min vs 45.6 min, P < 0.001), primarily due to the shorter half-life of propofol. It should be noted that the “recovery times” recorded in our study were heavily impacted by logistical issues, such as the time needed to educate patients about the colonoscopy results, get them dressed and confirm the arrival of their escorts. These factors tended to artificially prolong the “recovery time” for the CAPS group more than the MF group. In fact, CAPS patients were generally much more awake than control patients upon arrival in the recovery room, such that the difference in recovery times, although already highly significant, was less impressive than the difference in wakefulness upon arrival in the recovery room (Table 1). Even though the rapid recovery associated with propofol does not negate certain limitations, such as the prohibition against driving after the procedure, it has a major impact on patient convenience, satisfaction, post-procedural education and endoscopy unit flow[11]. Our previous study has already demonstrated that both patients and endoscopists were more satisfied with the recovery process for CAPS than that for MF[10]. In addition, we were able to reduce our recovery room staff overtime hours by 32%, resulting in over $14000 in savings per month despite increased procedure volumes[12].
Adverse events were relatively few, while serious adverse events were extremely rare. In the entire CAPS cohort of over 2500 patients, there were only two cases of desaturation requiring transient mask ventilation. The only death in the study, a CAPS patient who died from ischemic colitis, was felt to be caused by the underlying condition and not the colonoscopy or sedation. Aside from this delayed fatality, none of the subjects suffered any severe adverse event such as emergent intubation, unanticipated hospitalization, permanent injury or death. These findings echo those from our initial study, where there was only one CAPS patient who suffered desaturation requiring brief mask ventilation. The small number of adverse events was also consistent with the results of the randomized controlled trial, where no serious sedation-related complication occurred in the CAPS group[9].
Since CAPS has never been used in routine clinical practice before, our 12-mo cohort represents an ongoing learning experience from which we gleaned several practical principles for using CAPS: First, the learning curve for CAPS colonoscopy was relatively gentle compared to that for CAPS upper endoscopy; most endoscopists and nurses were very comfortable with CAPS colonoscopy by the end of the second month. Our temporal data show that colonoscopic completion and polyp detection rates were high right from the start (Figure 2). Complications were rare throughout the 12 mo experience. Once patients achieve a stable state of moderate sedation with CAPS, procedures usually go extremely smoothly without the intermittent awakening that can characterize MF sedation as drug levels wax and wane. CAPS is particularly well suited for lengthy colonoscopies, such as colonic endoscopic mucosal resection. CAPS for upper endoscopy is somewhat more challenging, and will be described in a separate paper. Second, we found that fentanyl premedication was not necessary in most patients, as demonstrated by the decreasing doses of fentanyl with time (Figure 1); towards the end of our 12 mo experience, most endoscopists preferred to use propofol alone, reserving fentanyl co-medication only for patients who were felt to be harder to sedate. Third, although our nursing staff initially exhibited varying degrees of anxiety associated with the introduction of CAPS into our unit, eventually our nurses, all of whom were already highly experienced with MF sedation, became the strongest proponents of CAPS.
There are several limitations to our study. First, we used historical controls, so there is the potential for discrepancies between the CAPS and control groups. Second, the study was unblinded for the providers and patients, which may have affected certain outcomes measures such as procedure time, recovery time, medication doses or even polyp detection rates. Third, the study was a retrospective analysis of prospectively collected quality control data, thus potentially subject to bias. This is particularly true for the historical control data. Finally, there are no complication data for the historical controls, thus no comparative analysis could be done for adverse events. However, the complication rate for the CAPS cohort was undeniably low and similar in magnitude to that seen in our previous controlled study as well as the randomized controlled trial[9].
In conclusion, CAPS is a safe and effective means of providing moderate sedation for low-risk patients undergoing routine colonoscopy in a high-volume endoscopy unit. The major advantage appears to be much faster recovery times. Because CAPS provides trained GI physicians with on-label access to propofol for low-risk procedures, this frees up anesthesia professionals to focus on more challenging cases, which may address the current shortage of anesthesia professionals in the United States while potentially reducing overall health care costs. Unfortunately, the manufacturer of the only FDA-approved CAPS system in the United States closed down its CAPS division at the end of 2016, presumably due to the company’s inability to project profitability from this technology. Currently, there are significant financial incentives for endoscopy practices to continue using anesthesia-administered propofol[13,14], thereby limiting the number of providers willing to invest in a CAPS system. However, with the anticipated advent of bundled payment for screening and surveillance colonoscopy[15-17], we believe that non-anesthesiologist-administered propofol sedation has considerable potential once the United States health care financial landscape changes. In our unit, the universal enthusiasm for non-anesthesiologist-administered propofol sedation on the part of nurses, doctors and patients motivated us to develop so-called nurse-administered propofol continuous infusion sedation (NAPCIS), which is a method of propofol delivery that replicates the capabilities of CAPS by using programmable intravenous fluid infusion pumps commonly available in the hospital (Alaris® pump module, Becton Dickinson, Franklin Lakes, NJ, United States). Unlike NAPS, which uses frequent, small, intermittent boluses of propofol administered by the nurse, NAPCIS delivers propofol as a continuous infusion controlled by the nurse and endoscopist, using a dosing and safety protocol identical to that in CAPS. Towards the end of 2016, we transitioned seamlessly from CAPS to NAPCIS, with over 200 NAPCIS cases performed at the time of this writing. So far, our experience with NAPCIS has been excellent, and we expect to report research data on this new mode of sedation administration in the near future.
The authors would like to thank Drs. Elisa Boden, Blaire Burman, Ian Gan, Shayan Irani, Geoffrey Jiranek, James Lord, Julia Pollock and Qing Zhang for their assistance and input.
Computer assisted propofol sedation (CAPS) was approved by the FDA in 2013 as a means to provide moderate sedation for American Society of Anesthesiology (ASA) class I and II patients undergoing routine upper endoscopy and colonoscopy. CAPS allows non-anesthesiologists to administer a continuous propofol infusion after a single premedication dose of fentanyl. As the only endoscopy unit in the United States to introduce CAPS for large-scale clinical use, we report our one-year experience with CAPS for colonoscopy on a large cohort of low-risk patients, compared against similar historical controls who underwent colonoscopy using traditional MF sedation in the 12 mo immediately preceding the start of our CAPS usage.
The use of anesthesiologist-administered propofol for low-risk endoscopies is estimated to cost the United States Health Care System hundreds of millions of dollars per year. As a response, there have been attempts to introduce nurse-administered propofol sedation (NAPS). NAPS has been shown to be feasible and safe, but there are significant barriers to its use in the United States, including the FDA labeling for propofol (which specifies that propofol must be administered by personnel trained in anesthesia), insurance regulations, hospital credentialing rules and medicolegal concerns. Thus, novel methods of delivering propofol safely and effectively without the prohibitive costs of anesthesia are needed.
CAPS appears to be a safe, effective and efficient means of providing moderate sedation for colonoscopy in relatively healthy patients. Recovery times were much shorter than historical measures. There were few adverse events, and no serious adverse events, related to CAPS.
CAPS can potentially make affordable non-anesthesia administered propofol sedation for gastrointestinal procedures widely available in the United States.
This is very interesting and important topic and nicely written manuscript. It will be nice if the authors can provide some more information (or explanation) about technical characteristics of CAPS system.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Kim JW, Stein J, Vujasinovic M S- Editor: Gong ZM L- Editor: A E- Editor: Zhang FF
| 1. | McQuaid KR, Laine L. A systematic review and meta-analysis of randomized, controlled trials of moderate sedation for routine endoscopic procedures. Gastrointest Endosc. 2008;67:910-923. [PubMed] |
| 2. | Inadomi JM, Gunnarsson CL, Rizzo JA, Fang H. Projected increased growth rate of anesthesia professional-delivered sedation for colonoscopy and EGD in the United States: 2009 to 2015. Gastrointest Endosc. 2010;72:580-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 92] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 3. | Liu H, Waxman DA, Main R, Mattke S. Utilization of anesthesia services during outpatient endoscopies and colonoscopies and associated spending in 2003-2009. JAMA. 2012;307:1178-1184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 134] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 4. | Hassan C, Rex DK, Cooper GS, Benamouzig R. Endoscopist-directed propofol administration versus anesthesiologist assistance for colorectal cancer screening: a cost-effectiveness analysis. Endoscopy. 2012;44:456-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 63] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Sieg A, Beck S, Scholl SG, Heil FJ, Gotthardt DN, Stremmel W, Rex DK, Friedrich K. Safety analysis of endoscopist-directed propofol sedation: a prospective, national multicenter study of 24 441 patients in German outpatient practices. J Gastroenterol Hepatol. 2014;29:517-523. [PubMed] |
| 6. | Rex DK, Deenadayalu VP, Eid E, Imperiale TF, Walker JA, Sandhu K, Clarke AC, Hillman LC, Horiuchi A, Cohen LB. Endoscopist-directed administration of propofol: a worldwide safety experience. Gastroenterology. 2009;137:1229-1237; quiz 1518-1519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 284] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 7. | Rex DK, Heuss LT, Walker JA, Qi R. Trained registered nurses/endoscopy teams can administer propofol safely for endoscopy. Gastroenterology. 2005;129:1384-1391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 192] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 8. | Rex DK. Effect of the Centers for Medicare & amp; Medicaid Services policy about deep sedation on use of propofol. Ann Intern Med. 2011;154:622-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Pambianco DJ, Vargo JJ, Pruitt RE, Hardi R, Martin JF. Computer-assisted personalized sedation for upper endoscopy and colonoscopy: a comparative, multicenter randomized study. Gastrointest Endosc. 2011;73:765-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 84] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | Lin OS, Kozarek RA, Tombs D, La Selva D, Weigel W, Beecher R, Jensen A, Gluck M, Ross A. The First U.S. Clinical Experience With Computer-Assisted Propofol Sedation: A Retrospective Observational Comparative Study on Efficacy, Safety, Efficiency and Endoscopist and Patient Satisfaction. Anesthesia and Analgesia. 2017;In press. |
| 11. | Horiuchi A, Graham DY. Special topics in procedural sedation: clinical challenges and psychomotor recovery. Gastrointest Endosc. 2014;80:404-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Koch J, Tombs D, Lin OS, Kozarek RA, Gluck M, Larsen M, Ross A. Economic impact of computer assisted propofol sedation. Gastroenterology. 2016;150:S101. |
| 13. | Rex DK, Vargo JJ. Anesthetist-Directed Sedation for Colonoscopy: A Safe Haven or Siren’s Song? Gastroenterology. 2016;150:801-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Dumonceau JM. Nonanesthesiologist administration of propofol: it’s all about money. Endoscopy. 2012;44:453-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Brill JV, Jain R, Margolis PS, Kosinski LR, Holt WS, Ketover SR, Kim LS, Clote LE, Allen JI. A bundled payment framework for colonoscopy performed for colorectal cancer screening or surveillance. Gastroenterology. 2014;146:849-853.e9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Patel K, Presser E, George M, McClellan M. Shifting Away From Fee-For-Service: Alternative Approaches to Payment in Gastroenterology. Clin Gastroenterol Hepatol. 2016;14:497-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Dorn SD. The Road Ahead 3.0: Changing Payments, Changing Practice. Clin Gastroenterol Hepatol. 2016;14:785-789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |