Published online Apr 7, 2017. doi: 10.3748/wjg.v23.i13.2365
Peer-review started: November 25, 2016
First decision: December 19, 2016
Revised: January 18, 2017
Accepted: March 15, 2017
Article in press: March 15, 2017
Published online: April 7, 2017
Processing time: 134 Days and 20.2 Hours
To develop a locally adapted, patient-focused transition-program, we evaluated the perceptions of adult and adolescent patients and parents regarding transition-programs and transfer.
We evaluated these perceptions by analyzing the responses of pre-transfer adolescents (n = 57), their parents (n = 57) and post-transfer adults (n = 138) from a cohort of pediatric-liver-transplant-patients using a self-designed questionnaire. Furthermore, we compared a responder group with a non-responder group as well as the provided answers with baseline characteristics and clinical outcomes to exclude selection bias, characterize high-risk patients for non-adherence and test for gender differences. Included in our study were all pre-transfer liver transplant and combined liver-kidney transplant recipients aged 11-19 currently under our care and their parents, as well as all post-transfer liver transplant and combined liver-kidney transplant recipients aged ≥ 17 years who had received a liver transplant and were treated at our center during childhood.
Fifty-seven (24 female) pre-transfer patients who received a transplant in the previous 8-186 mo (mean 93.9 mo, median 92 mo, SD 53.8 mo) and 138 (57 female) post-transfer patients who received a transplant in the preceding 2-29 years (mean 15.6 years, median 17, SD 6.90) met the inclusion criteria. A total of 67% of pre-transfer patients (71% of female; 64% of male; P = 0.78) and their parents replied. Additionally, 54% of post-transfer patients (26% of female; 48% of male; P = 0.01) replied. No differences in clinical outcomes were observed between the responder and non-responder groups, and responses did not differ significantly based on clinical complication rates, although they did differ based on gender and the location of medical follow-up after transfer. Adolescents were generally ambivalent toward transition programs. However, adults strongly supported transition programs.
Transition programs need to be developed in close collaboration with adolescents. The best clinical practices regarding transition should respect local circumstances, gender and the location of post-transfer medical follow-up.
Core tip: This was a retrospective study that evaluated the perceptions of adult and adolescent patients and their parents for transition programs as well as for the completed transition and transfer process. Furthermore, we compared a responder group with a non-responder group as well as the provided answers with baseline characteristics and clinical outcomes to exclude selection bias, characterize high-risk patients for non-adherence and test for gender differences. No differences in clinical outcomes were observed between the responder and non-responder groups. Responses differed significantly based on gender and the location of medical follow-up post-transfer. Adolescents were ambivalent toward transition programs. Adults strongly support them.
- Citation: Junge N, Migal K, Goldschmidt I, Baumann U. Transition after pediatric liver transplantation - Perceptions of adults, adolescents and parents. World J Gastroenterol 2017; 23(13): 2365-2375
- URL: https://www.wjgnet.com/1007-9327/full/v23/i13/2365.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i13.2365
In recent years, substantial medical and surgical improvements have led to the enormous success of pediatric liver transplantation with 10-year survival rates greater than 90%. Therefore, more children experience transfer from pediatric to adult health services. Due to this achievement, long-term problems, the psychological and social aspects of care, the quality of the patient’s life, and non-adherence to treatment have become more important. Non-adherence can lead to increased rates of hospitalization, graft loss and death and is well documented following pediatric liver transplant[1-3]. Since adolescence is a potentially risky period[4], this developmental period is challenging for all concerned - young people, parents and health professionals - and lends itself to a high risk for non-adherence in chronic diseases. Internal and external factors can influence adolescents during this developmental period and can create behaviors that lead to adherence or non-adherence. Furthermore, a change in healthcare provider that results from a transfer has a direct and strong influence on adherence. Therefore, a broad professional consensus exists regarding the need to prepare young people with chronic health conditions (including those patients with solid organ transplants) to enter adulthood with comprehensive self-management skills[5-8] that will theoretically improve psychological and social attributes as well as the quality of life for these patients. The process of transitioning from childhood to adulthood, which includes developmental aspects, self-reliance and understanding one’s own disease and medications, is known as transition and should not be confused with the term transfer, since transfer only describes the change in health care provider (from a pediatric clinic to an adult clinic). The American Academy of Pediatrics recommends a necessary process that includes a transition plan that should be implemented as early as 12 years of age[9]. In 2015, Suris et al[10] described the international consensus regarding the key points for a successful transition. Few pediatric liver transplant centers have adopted this approach and developed formal transition programs[6,11]. To facilitate the rapid and smooth introduction of a local transition program, we adopted and introduced a successfully pre-established transition program from a United Kingdom transplant center that was developed for adolescent liver transplant recipients ≥ 12 years of age, which fulfilled most of the previously identified key factors for successful transition (Table 1). This model was intended to be used as a template for the reproduction of successful elements while avoiding the de novo development of a specific local liver transplant transition plan for our center.
| Organization/structure of outpatient appointments, support peer group formation | Dedicated liaison with a transfer-accompanying youth worker and clinical nurse specialist, working in both pediatric and adult services, for continuity and for the provision of specific information to the adolescent during transfer |
| Joint outpatient clinics between adult and adolescent clinics | |
| “Parent-free portions” of outpatient appointments | |
| Adolescent-focused consultation sessions to provide information | |
| Support peer group formation | Encouragement of networking among adolescents by offering additional non-medical programs during transition clinics |
| Dedicated days in the ambulatory outpatient clinic for adolescents | |
| Education | Seminars for education and networking outside the clinic |
| Transfer | Staggered transfer into adult medical care |
We hypothesized that key elements from an existing transition program could be implemented in order to save time and resources. We intended to adapt and implement a local, highly effective patient- and resilience-oriented transition program for young people who received a liver transplant. Therefore, the aim of this study was to evaluate this adapted approach and test our hypothesis using a questionnaire that evaluated the perceptions of both patients and parents regarding elements of the established transition program that was adapted from the United Kingdom Liver Unit. We aimed to support this evaluation with an analysis of clinical outcome variables and a comparison of the incidence of adverse events, such as acute cellular rejection between responders and non-responders, to avoid bias resulting from patients in the non-responder group who may be at a higher risk for non-adherence. Furthermore, we attempted to identify patients at a high risk for non-adherence by correlating their clinical outcome to the answers provided on their questionnaire.
To test our hypothesis, we designed a pilot study to evaluate a purpose-built single-center survey in the format of a 9-item questionnaire that was built around statements regarding the newly proposed transition program. These statements were derived from key elements of the established transition pathway and addressed factors such as the introduction of a designated outpatient clinic for adolescents, time for one-on-one medical consultation, opportunities for networking between adolescents, and additional counseling time for psychosocial screening, which included health-risk behaviors, sexual and reproductive health issues and professional development (Table 2). The questionnaire was sent to young people with liver grafts before transfer (patients), their parents, and adults with liver grafts post-transfer to assess opinions on the transition program and seek their individual interest in and acceptance of the proposed statements. The questionnaire was modified for each specific group of recipients (Table 2) and was distributed in our clinic or sent by letter with a free-return envelope. Participants replied to the questionnaire in written form on the questionnaire sheet. Non-responders received two telephone reminders from a doctor known to the patient and family. With the exception of patients with significantly impaired cognitive function, the inclusion criteria for the two groups of patients were defined as follows: except for patients with significantly impaired cognitive function, all pre-transfer liver transplant and combined liver-kidney transplant recipients aged 11-19 years (cohort 1a, adolescents) currently under our care and their parents (cohort 1b). Our aim was to face the challenges in discrepancies that existed between parent and patient self-reporting. For the second group, all post-transfer liver transplant and combined liver-kidney transplant recipients aged ≥ 17 years who had received a liver transplant and were treated at our center during childhood were included (cohort 2, adults). Post-transfer (adult) patients were asked to evaluate some of the statements in the questionnaire twice, first from their current perspective [cohort 2b (cp)] and second from the perspective of their previous adolescent pre-transfer [cohort 2a (pp)]. In the first analysis, we searched for potential sources of bias and compared the baseline characteristics and outcome variables of responders to those of non-responders. Baseline characteristics and medical data were gathered by retrospective case review for all patients who met the inclusion criteria.
| Patients under the age of 18 yr (cohort 1a) | Parents (cohort 1b) | Adults (Patients > 18 yr) anticipated retrospective pre-transfer opinion (cohort 2a) | Adults (Patients > 18 yr) current opinion (cohort 2b) | |
| Q1 | I would appreciate more intense support during transfer1 | I would appreciate more intense support during transfer1 | I would have appreciated more intense support during transfer1 | I would appreciate more intense support for liver-transplanted adolescents during transfer1 |
| Q2 | I appreciate the transition program, but I prefer to choose a day for an outpatient appointment instead of having special “adolescent outpatient clinic days”1 | I appreciate the transition program, but I prefer to choose a day for an outpatient appointment instead of having special “adolescent outpatient clinic days”1 | I would have appreciated the transition program, but I would have preferred to choose a day for an outpatient appointment instead of having special “adolescent outpatient clinic days”1 | ND |
| Q3 | I appreciate the transition program, but I do not want to talk to the doctor on my own1 | I appreciate the transition program, but I do not want my child to talk to the doctor on his/her own1 | I would have appreciated the transition program, but I would have not wanted to talk to the doctor on my own1 | I do not think that it is beneficial or important for adolescents to have time to talk to the doctor alone or without their parents1 |
| Q4 | I appreciate the transition program, but I do not want to stay after my outpatient clinic appointment for collaborative activities1 | I appreciate the transition program, but I do not want my child to stay after his/her outpatient clinic appointment for collaborative activities1 | ND | ND |
| Q5 | I have no interest in education or transition programs1 | I have no interest in education or transition programs1 | I would have had no interest in education or transition programs1 | I do not think that education or transition programs are important for adolescents after liver transplantation1 |
| Q6 | At what age should a transition program should start?2 | At what age should a transition program start?2 | At what age should a transition program start?2 | At what age should a transition program start?2 |
| Q7 | I would prefer to have seminars and educational programs outside the clinic1 | I would prefer to have seminars and educational programs outside the clinic1 | ND | ND |
| Q8 | I appreciate the transition program, but….3 | I appreciate the transition program, but….3 | I appreciate the transition program, but….3 | I appreciate the transition program, but…3 |
| Q9 | I have further suggestions for a transition program…3 | I have further suggestions for a transition program…3 | I have further suggestions for a transition program…3 | I have further suggestions for a transition program…3 |
| Q10 | ND | ND | ND | How important is a multi-disciplinary team in the adult outpatient clinic?4 |
| Q11 | ND | ND | ND | A transition program can impair the development of autonomy1 |
| Q12 | ND | ND | ND | I was well informed about my disease and my health at transfer1 |
| Q13 | ND | ND | ND | I would have liked to have had more information about my disease and my health at transfer1 |
| Q14 | ND | ND | ND | How helpful would a social worker be to assist in the transfer process?4 |
| Q15 | ND | ND | ND | How would you rate your completed transfer?5 |
| Q16 | ND | ND | ND | How helpful would it have been if there was a joint outpatient clinic with pediatric and adult medicine?4 |
| Q17 | ND | ND | ND | A transition program would have influenced my professional career1 |
| Q18 | ND | ND | How anxious did you feel due to the transfer process?4 | |
| Q19 | ND | ND | ND | I would have liked to decide the transfer age on my own1 |
| Q20 | ND | ND | ND | Which person(s) were the most important for you during your transfer? |
| Q21 | ND | ND | ND | Which topics were the most important for you during transfer? |
Statistical analysis was performed using IBM SPSS (versions 22 and 23). Baseline characteristics and medical data were compared between groups using Mann-Whitney U tests, and further statistical analyses were conducted using Kruskal-Wallis and Fisher’s exact tests.
In the pre-transfer group (adolescents and parents), 57 patients (24 female) met the inclusion criteria and were offered participation in the survey. The median age at the time of the survey was 14 years (12-19 years; SD 2.092), and the median age at liver transplantation was 6.9 years (4.8 mo-17.9 years; SD 58.28 mo). Patients received follow-up over a period of 8-186 mo (mean 93.9 mo, median 92 mo, SD 53.8 mo) after liver transplantation. Four patients underwent re-transplantation and one patient received 3 liver transplants before completing the survey. Patients had the following diagnoses: biliary atresia (BA) n = 26 (45.6%), acute liver failure (ALF) n = 7 (12.3%), other conditions n = 6 (10.5%), Cystic Fibrosis-associated liver disease (CFLD) n = 5 (8.8%), progressive familial intrahepatic cholestasis (PFIC) n = 4 (7%), autosomal recessive polycystic kidney disease (ARPKD) n = 4 (7%), autoimmune hepatitis (AIH) n = 2 (3.5%), α-1-antitrypsin deficiency (A1ATD) n = 2 (3.5%) and Alagille Syndrome n = 1 (1.8%). Retrospective case note review identified 38 liver biopsy-proven acute rejection (BPAR) observed in 28 patients in this group.
The parents (n = 57) of all patients in this group were contacted and asked to participate in the questionnaire adapted for parents as shown in Table 2.
Of the pre-transfer group, 38 families (67%) had one patient and one parent each who responded to the survey. All responses that were received were paired, and no single patient or parent response was received.
For the post-transfer group (adults), all surviving patients who had received a liver transplant during childhood at our institution and who had a current postal address were identified irrespective of their current age. The questionnaire was sent to 138 patients (57 female). The median age of survey respondents was 23.5 years (17-41 years; SD 5.44). The median age at liver transplantation was 9 years (0-17 years; SD 5.36). Patients received follow-up over a period of 2-29 years (mean 15.6 years, median 17, SD 6.90) after liver transplantation. Underlying diagnoses that led to the indication for liver transplantation included BA n = 36 (26.8%), other conditions n = 24 (17.4%), PFIC n = 16 (11.6%), Alagille Syndrome n = 12 (8,7%), suspected malignant liver tumor n = 11 (8%), A1ATD n = 8 (5.8%), CFLD n = 7 (5.1%), AIH n = 5 (3.6%), Crigler Najjar Syndrome n = 4 (2.9%), primary sclerosing cholangitis n = 4 (2.9%), Wilson’s Disease n = 4 (2.9%), primary hyperoxaluria n = 3 (2.2%), ARPKD n = 2 (1.5%), and chronic hepatitis B/C n = 2 (1.5%).
Of the post-transfer group, 54 patients (39.1%) replied to the questionnaire.
The responder rate in the pre-transfer group (67%, n = 38) was higher than that in the post-transfer group (39%, n = 54). The only difference between the responder and non-responder cohorts was detected in the post-transfer group. In this group, significantly fewer women replied. Of the 57 women included, 15 (26.3%) replied, and 39 out of 81 males replied (48.1%); P = 0.01. With respect to clinical complication rate, age, diagnosis and time of diagnosis, the responder and non-responder groups were identical (Table 3). This analysis confirmed that the responses were representative of both patient cohorts. Furthermore, we tested for differences between responders and non-responders (adolescents and adults) based on gender, age at liver transplant, time between liver transplantation and questionnaire, BPARs, the number of re-transplantations and the diagnosis of acute liver failure as a reason for transplantation, but there were no significant differences.
| Adults (post-transfer), [n = 138 (F/M = 57/81), median age: 24.6 yr] | Adolescents (pre-transfer), [n = 57 (F/M = 24/33), median age: 14.7 yr] | |||||
| Responder | Non-responder | P value | Responder | Non-responder | P value | |
| n | 54 (39) | 84 (61) | 38 (67) | 19 (33) | ||
| Female | 15 (26) | 42 (74) | 0.012 | 17 (71) | 7 (29) | 0.782 |
| Male | 39 (48) | 42 (52) | 21 (64) | 12 (36) | ||
| Survey-age (yr), mean ± SD | 25.6 ± 5.70 | 24.1 ± 5.22 | 0.121 | 14.7 ± 2.14 | 14.8 ± 2.04 | 0.881 |
| OLT-age (yr), mean ± SD | 8.3 ± 5.60 | 8.6 ± 5.22 | 0.801 | 7.5 ± 5.25 | 6.0 ± 3.90 | 0.301 |
| OLT-survey (yr), mean ± SD | 16.8 ± 6.88 | 14.9 ± 6.82 | 0.111 | 7.2 ± 4.88 | 8.9 ± 3.44 | 0.211 |
| BPAR, mean ± SD | 1.02 ± 0.83 | 1.04 ± 1.20 | 0.481 | 0.84 ± 0.82 | 0.42 ± 0.61 | 0.061 |
| BPAR outpatient, mean ± SD | 0.51 ± 0.68 | 0.64 ± 1.11 | 0.751 | 0.55 ± 0.72 | 0.37 ± 0.60 | 0.341 |
| #OLT, mean ± SD | 1.37 ± 0.57 | 1.29 ± 0.51 | 0.271 | 1.16 ± 0.50 | 1.21 ± 0.54 | 0.811 |
| Re-OLT outpatient, mean ± SD | ND | ND | ND | 0.11 ± 0.31 | 0.16 ± 0.50 | 0.951 |
| LDLT | 0 | 0 | ND | 6 (16) | 1 (5) | 0.412 |
| ALV | 7 (13) | 10 (7) | > 0.92 | 5 (13) | 2 (11) | > 0.92 |
| “In-Center-Transfer” | 30 (61) | 32 (44) | 0.042 | ND | ND | ND |
| Chronic rejection | 6 (5) | 10 (8) | 0.822 | 0 | 0 | ND |
In Table 4, the mean answers provided by each cohort for questions [Q]1-7 are displayed. Q1, 3, 5 and 6 were posed to all cohorts, and Q2 was posed to all cohorts except for cohort 2b (the current perspective of post-transfer patients).
| cohort 1a mean answer (SD), n = 38 | cohort 1b (parents) mean answer (SD),n = 38 | P value cohort 1a vs 1b | cohort 2a (pp) mean answer (SD),n = 54 | P value cohort 2a (pp) vs 1a | P value cohort 2a (pp) vs 1b (parents) | cohort 2b (cp) mean answer (SD),n = 54 | P value cohort 2b (cp) vs 1a | P value cohort 2b (cp) vs 1b (parents) | P value cohort 2b (cp) vs 2a | |
| Q 1 “appreciate more intense support during transfer” | 2.111 (1.37) | 1.421 (0.98) | 0.01 | 2.151 (0.91) | NS | < 0.001 | 1.541 (1.19) | 0.040 | NS | 0.001 |
| Q2 “no special adolescent outpatient clinic days” | 2.471 (1.56) | 2.421 (1.64) | NS | 3.411 (1.66) | 0.002 | 0.010 | - | -- | - | -- |
| Q3 “no patient-doctor alone (parent-free) time” | 2.161 (1.42) | 2.681 (1.66) | NS | 2.911 (1.62) | 0.030 | NS | 3.631 (1.25) | 0.001 | 0.010 | 0.006 |
| Q4 “no collaborative activities after the outpatient appointment” | 2.031 (1.40) | 2.291 (1.45) | NS | - | - | - | - | - | - | - |
| Q5 “no interest in education or transition programs” | 3.551 (1.54) | 4.131 (1.23) | NS | 2.721 (1.34) | 0.005 | < 0.001 | 4.191 (0.91) | NS | NS | 0.001 |
| Q6 “transition program starting age” | 14.082 (2.22) | 13.872 (2.22) | NS | 15.442 (2.01) | 0.003 | 0.010 | 15.092 (1.95) | 0.040 | 0.012 | 0.010 |
| Q7 “prefer seminars outside the e clinic” | 3.031 (1.40) | 2.951 (1.53) | NS | - | - | - | - | - | - | - |
Except for question one [Q1], adolescents and parents did not differ significantly in their general views and stated that they would appreciate the support provided by a transition program. However, the parents appreciated the support during transfer significantly more than did the adolescents. In summary, adolescents tended to be more ambivalent or negative toward specific elements, such as special adolescent outpatient days, collaborative activities in the afternoon after outpatient visits or seeing the physician on their own.
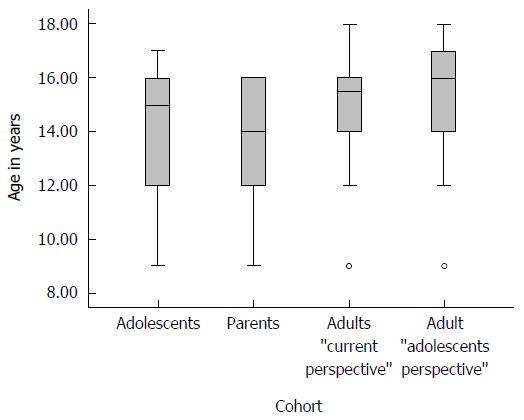
The support of the key components of transition programs differed significantly over the three patient groups, with the least support in the adolescent group (cohort 1a) and the strongest support in the post-transfer, current perspective adult group (cohort 2b), which was significantly more than in the parent group. The previous-perspective adult group (cohort 2a) differed significantly from cohort 2b (cp) on all points and showed a mixed representation when compared to cohorts 1a and 1b. Disinterest in the transition program or additional education was highest in cohort 2a. Medical providers that saw patients for a portion of the visit without their parents were the most accepted by cohort 2b (cp) and least accepted by adolescents (1a). All results are shown in Table 4. Regarding the best age for starting a transition program, the opinions ranged widely and every group differed significantly (Figure 1).
Some additional questions that evaluated previous transfer experiences and proposals for new transition programs were only posed to the post-transfer patients (adults, cohort 2b) (Table 5). Their answers showed that adult liver-transplant patients considered a multidisciplinary team, an accompanying social worker and a joint (pediatrician and adult-care specialist) outpatient clinic as important and helpful factors in the transfer process. They did not believe that a transition program would prevent the development of patient autonomy. Even though these patients had transferred to an adult clinic without a transition program, they mostly felt generally well-informed (Q12). On the other hand, they would have preferred to receive more information about their disease and overall health during their transfer period (Q13). They did not believe that a transition program would have influenced their professional career; they rated their transfer (without a transition program) as satisfactory (grade “C”) and felt somewhat unsettled due to the transfer. When asked for the most important person during the transfer, 28% of respondents mentioned the pediatrician, 26% said “others,” and 15% stated that it was the nurses. When asked for the most important topics during transfer, 25% of respondents cited medication, 17% cited education and employment, 13% said disease knowledge and 10% stated pregnancy.
| Question | mean answer (SD) | mean answer in words |
| How important is a multi-disciplinary team in the adult outpatient clinic? | 1.8 (1.05) | Important |
| A transition program can impair the development of autonomy | 3.9 (1.13) | Mostly not |
| I was well informed about my disease and my health at transfer | 2.1 (1.22) | Mostly yes |
| I would have liked to have had more information about my disease and my health at transfer | 2.3 (1.36) | Mostly yes |
| How helpful would a social worker be to assist in the transfer process? | 1.8 (0.93) | Mostly helpful |
| How would you rate your previous transfer? | 2.8 (1.36) | Satisfactory, “C” |
| How helpful would it have been if there was a joint outpatient clinic with pediatric and adult medicine? | 2.0 (0.90) | Mostly helpful |
| A transition program would have influenced my professional career | 3.5 (1.21) | Mostly not |
| How anxious did you feel due to the transfer process? | 2.7 (1.27) | Unsettled but not very much |
| I would have liked to decide the transfer age by my own | 2.6 (1.50) | Mostly agree |
| Which person(s) were the most important for you during your transfer? | 28% pediatrician, 26% others, 15% nurses, 9% doctor’s adult clinic, 8% siblings, 8% partner, 5% social worker 1% friends | |
| Which topics were the most important for you during transfer? | 25% medications, 17% school and profession, 13% disease knowledge, 10% pregnancy, 8% drugs and alcohol, 5% body image, 5% relationships, 4% sport, 4% adherence, 3% sexuality, 3% role in the family, 3% others | |
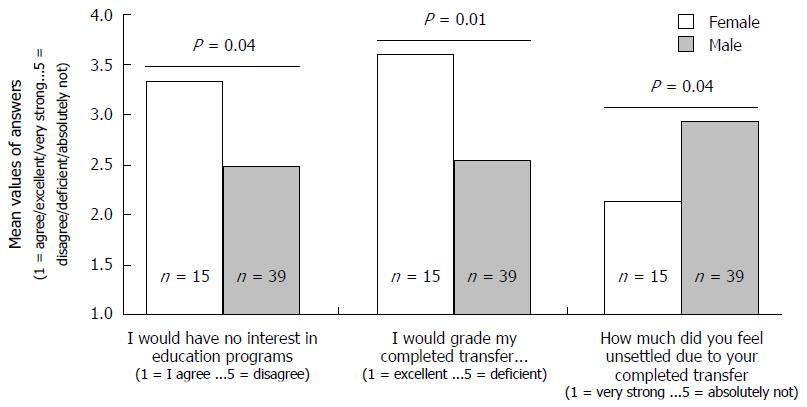
Different perceptions in and between groups were independent of clinical characteristics, clinical complication rates and time between the OLT and receipt of the questionnaire. For detailed results, please see Supplemental Tables 1-4. In cohorts 2a and 2b, we found gender-dependent differences regarding the interest in education and perceptions of the transfer experience. Females had a significantly higher interest in education and rated their transfer experience worse than did males (Figure 2).
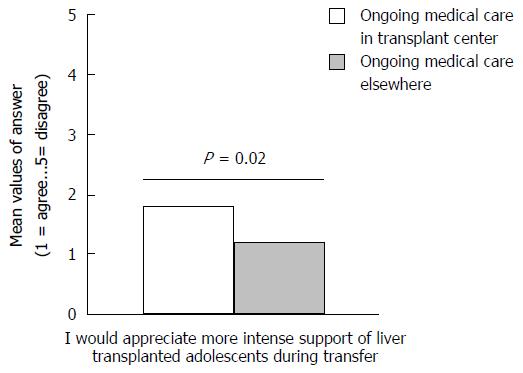
Furthermore, our results showed that adults who were transferred to medical care outside of our transplant center had a stronger desire for support during transfer (Figure 3).
The aim of this study was to evaluate the perceptions of patients, parents and adults regarding the elements of an established transition program from a UK Liver Unit, to facilitate a rapid and smooth introduction of a transition program in our local unit. Our results showed that this was not a straightforward process and underlined the need to consider local needs and circumstances, such as a centralization of the medical system, religion, type of education, school system and social status.
A strong point in our study was that we also surveyed adult patients who had received a liver-transplant as children and collected their opinions on transfer and transition. Therefore, we benefitted from their experience and mental maturity without parental bias, even though there was a wide age range in these adult patients, with a recall bias and different life circumstances. Irrespective of this, mentoring by an adult patient was also recommended by the international Delphi study[10]. The results of our study strongly support the inclusion of this element and show how much adults appreciate transition programs (cohort 2b) and how much they can understand the perspectives of adolescents (cohort 2a). This was demonstrated by significantly different answers from both perspectives in this group (Table 4).
More clearly than previous studies, our results demonstrated that patients appeared ambivalent to transition opportunities. This emphasizes that it is very important and difficult to balance between motivating adolescent patients to participate and slightly pushing them without forcing them too much. Perhaps, it is best not to identify the program as a “transition” but simply as one more step in the evolution of people with liver-transplants. Forcing them could result in an even greater negative response and could possibly result in non-adherence. The lack of motivation of younger patients to take part in a transition program concurred with the findings of Anthony et al[12], who showed a disinterest in adolescents regarding transition. Possible explanations for this include youth-unfriendly interventions, parental over-protection and/or the development of abstract thought and forward planning during adolescent brain development[13,14]. This means that to involve adolescents, we must first arouse interest. The advantage of peer-group effects can and should be used, and although this can be complicated by geography, e-health and m-health, internet-based social networking can currently provide potential solutions for this.
Our study also showed that over the years, the perceptions and attitudes of patients changed to those supporting transition programs. This may mean that adolescents are not able to anticipate (perhaps due to poorly explained benefits) the benefit of transition programs, while adult patients who were once adolescents and previously experienced a transfer from pediatrics to adult care can see the value, even if only retrospectively. This confirms that transition programs are beneficial and important tools, even if adolescents primarily regard these programs with ambivalence. Our adult cohort delivered important information from both a patient and adult perspective regarding transition and transfer after they had themselves completed a transfer as adolescents. Furthermore, adult patients stated a strong need for combined pediatric-adult outpatient clinics. This is an already well-known instrument for improving transfer and has a benefit that the transition program continues after transfer, which is very important, as shown by Fredericks et al[15]. However, when discussing perceptions of our adult cohort, it should be noted that we aimed to develop a transition program not for adults, but for adolescents, especially given the wide age range of the adult group in our study.
The available literature is unclear on the differences in the awareness of risk between parents and adolescents. Even though replies from parents and patients only differed significantly in one question - the important question number 1 (need for support during transfer) - the tendencies in other replies led to the assumption that parents were more aware of the risks during transition and were also more interested in transition, disease and medication education than were their children. These results were in-line with the findings of Anthony et al[12] and Boyle et al[16] but differed from Fredericks et al[17], who reported that parents and patients were aware of the problems and risks of the transition process. These results were also interesting regarding the possibility that an adolescent’s replies to the questionnaire could have been influenced by their parents. Our results made it unlikely that a significant influence occurred because they showed different replies for most questions and a significantly different reply in one question.
Notable also were the responses to question 3: “Should medical caregivers see the patient for a portion of the visit without the parents?” This was least accepted by adolescents and, surprisingly, not significantly more accepted by the parents, but it was mostly accepted by the adults in cohort 2b (cp). We believe that this fact demonstrates an over-protection by parents and anxiety on the part of the adolescents. Therefore, this is a very important aspect for a transition program and shows again why an adult patient’s viewpoint on transition is important for developing transition programs.
Surprisingly, all of our cohorts preferred to start the transition program later and between the ages of 13.9-15.4 years. In the literature, opinions on the optimal age for starting a transition program vary greatly and can depend on the definition and perception of the transition process. Many studies[18] have shown that an early start is favorable and that transition programs, especially education programs, are most effective when they started between the ages of 11-14 years[19]. In this early stage of the transition process, the most important points are educating parents regarding the gradual shift in responsibility for health management tasks from the parent to the adolescent[15] and educating the young person on their own development and outlook towards shared management. These points may not have been considered as part of the transition by our patients and parents and could be the reason why they preferred to start later, but they could also mean that our patients and parents were not aware of the importance of these aspects and that, in this situation, more education is especially important. How such educational interventions for parents can be realized and how effective they are were recently shown by Akre et al[20].
To the best of our knowledge, our study is the first to evaluate baseline characteristics and clinical outcomes of non-responders in order to exclude any selection bias. Although, apart from a gender difference, significantly more male than female adults answered the survey, we did not see any differences between responders and non-responders regarding age, the number of liver transplants, BPAR, or the time between OLT and survey. This aspect has not been clearly described in the literature and emphasizes the difficulty in predicting transition outcome in patients. A selection of “high risk” patients, which should receive more intense support, seems to be impossible so far. But we could find following tendencies, which could help to identify these patients. In the pre-transfer group, the non-responders tended to have longer times between transplantation and the questionnaire when compared to the responder group. This could mean that patients with liver transplants that occurred further in the past had less of a desire for a transition process; this could be due to lower compliance, as reported by Berquist[2], or because the patients assumed their medication duties more naturally.
However, testing for correlation between clinical outcomes or the baseline characteristics of the patients to the type of answers revealed a significant gender difference in adults (Figure 2) with women who were more anxious about the transfer process and reported worse transfer experiences than men. Consistently, women were also significantly more interested in education. Even though these results must be interpreted with caution since the female cohort was significantly smaller in those groups, they show an important aspect regarding gender-specific transitional care. Except for these gender differences, perceptions in and between groups appeared to be independent from the clinical course and the rates of certain complications, such as acute or chronic rejection, re-transplantation and acute or chronic liver failure. Interestingly, adults who were transferred to medical care outside our adult liver transplant outpatient clinic retrospectively expressed a stronger desire for support and educational programs during the transition. This may indicate that ongoing medical care in the same transplant center is an important part of the transfer and can improve the whole transition process[18]. However, this may imply that patients transferred to a hepatologist outside of the transplant center needed more intensive support, and thus, cooperation with these hepatologists must be improved. Therefore, gender and differences in the location of follow-up after transfer, depending on local circumstances, should be carefully examined when transition programs are developed.
Limitations in our study are mainly based on the lack of feasibility in validating our questionnaire, the heterogeneous cohort and the potential recall bias for adults who remembered past adolescent pre-transfer perspectives, especially since the time between transfer and receipt of the questionnaire differed from 0 to 23 years. Although unlikely, we cannot exclude that adolescents’ replies to questionnaire were influenced by their parents, even though this is unlikely, as discussed above. The responder group may have been biased due to the reminder calls, since we cannot differ between patients who responded to the survey with or without reminder calls. However, a significant bias is unlikely since there was an insignificant difference between the responder and non-responder groups and the numbers of patients who responded after reminder calls was minor.
Even though our results emphasize existing ideas about transition, this is the first time these strategies are analyzed from the point of view of patients, parents and adults. We feel that the evaluation of their perceptions is essential prior to working with theoretically developed transition strategies, especially since the long-term evaluation of the effectiveness of “transition-tools/concepts” is difficult.
In conclusion, we identified a gender difference, with significantly more adult males than females replying to the questionnaire. This contrasted with a stronger desire for education programs by female adults. Furthermore, we found indicators that patients who were followed up with outside of the adult outpatient clinic at our center expressed a stronger need/desire for transition programs. We were not able to identify any other high-risk group with an impaired outcome during the transition process since responses appeared to be independent of clinical complication rates and neither group significantly differed with respect to clinical complications, age, date of transplant or type of liver failure.
In our study, adolescents appreciated the transition program but were ambivalent toward proposals from preexisting transition programs. Conversely, liver-transplanted adults agreed with the suggestions for such programs and indicated that adolescent patients may not be aware of future unmet problems and risks. Adolescents, like teenagers everywhere, oppose external guidance when it is presented as such. Taken together, this underlines the need and potential importance of such programs and the usefulness of adult patient mentoring. From this, we can conclude that transition programs need to be developed in close collaboration with adolescents but should perhaps be presented in such a way that allows adolescents to design their individual transition vs partaking in a pre-assigned journey.
We would like to thank Janet McDonagh very much for her very constructive feedback on this manuscript.
Currently, liver transplantation has a very good outcome. In children, the 10-year survival rates are above 90%. Therefore, more children experience the transfer from pediatric to adult health services. Due to this achievement, long-term problems, psychological and social aspects, as well as quality of life and non-adherence, have become more important. Non-adherence at the time of transition and transfer can lead to increased rates of hospitalization, graft loss and death and is well documented following pediatric liver transplantation. Therefore, to improve psychological and social aspects as well as quality of life, a broad professional consensus exists regarding the need to prepare young people with chronic health conditions, including patients with solid organ transplants, to enter adulthood with comprehensive self-management skills. However, data on the effectiveness of such programs are rare, and even less data are available concerning the perceptions of patients pre- and post-transfer, as well as those of their parents, with respect to such programs and transfer. Furthermore, it is unclear if existing programs can be used universally. To verify this and to evaluate the perceptions of patients and their parents, we conducted this study using a questionnaire.
The published literature is unclear regarding the differences in the awareness of risk for parents and adolescents. The lack of motivation of younger patients to take part in a transition program has been described by different authors. Previous studies lack baseline characteristics and outcomes of the non-responder.
This study showed that adolescents appreciated transition programs but were ambivalent towards proposals from preexisting transition programs and that they may oppose external guidance when it is presented as such. Conversely, liver-transplanted adults agreed with suggestions for such programs, and indicated that adolescent patients may not be aware of future unmet problems and risks. This study could not detect differences in clinical outcomes or baseline characteristics between responders and non-responders. An association of baseline characteristics or outcomes could only be provided for gender and location of medical follow-up.
The study underlines the need and potential importance of transition programs as well as the usefulness of adult patient mentoring. It also shows that transition programs need to be developed in close collaboration with adolescents but perhaps presented in such a way that adolescents design their individual transition rather than partake in a pre-assigned journey. Furthermore, gender differences and the location of medical follow-up should also to be considered.
Transfer describes the changeover from pediatric medical care to adult medical care. Transition describes much more. The transition process starts years before transfer and continues for years after transfer. Both pediatric and adult medicine doctors should be mindful of the transition process. The transition process includes not only medical aspects but also aspects of adolescence, such as becoming responsible, separation from parents, first partnership, choosing a line of employment or education, and much more.
This retrospective study provides important guidance for the design and understanding of transition programs for pediatric liver transplant centers.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Germany
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Qin JM, Wang GY S- Editor: Gong ZM L- Editor: A E- Editor: Wang CH
| 1. | Berquist RK, Berquist WE, Esquivel CO, Cox KL, Wayman KI, Litt IF. Adolescent non-adherence: prevalence and consequences in liver transplant recipients. Pediatr Transplant. 2006;10:304-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 67] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Berquist RK, Berquist WE, Esquivel CO, Cox KL, Wayman KI, Litt IF. Non-adherence to post-transplant care: prevalence, risk factors and outcomes in adolescent liver transplant recipients. Pediatr Transplant. 2008;12:194-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 64] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 3. | Sudan DL, Shaw BW, Langnas AN. Causes of late mortality in pediatric liver transplant recipients. Ann Surg. 1998;227:289-295. [PubMed] |
| 4. | Park MJ, Paul Mulye T, Adams SH, Brindis CD, Irwin CE. The health status of young adults in the United States. J Adolesc Health. 2006;39:305-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 277] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 5. | Fredericks EM, Magee JC, Opipari-Arrigan L, Shieck V, Well A, Lopez MJ. Adherence and health-related quality of life in adolescent liver transplant recipients. Pediatr Transplant. 2008;12:289-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 110] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 6. | Wright J, Elwell L, McDonagh JE, Kelly DA, Wray J. ‚It‘s hard but you‘ve just gotta get on with it‘--The experiences of growing-up with a liver transplant. Psychol Health. 2015;30:1129-1145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Kelly D, Wray J. The adolescent liver transplant patient. Clin Liver Dis. 2014;18:613-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Bell LE, Bartosh SM, Davis CL, Dobbels F, Al-Uzri A, Lotstein D, Reiss J, Dharnidharka VR. Adolescent Transition to Adult Care in Solid Organ Transplantation: a consensus conference report. Am J Transplant. 2008;8:2230-2242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 168] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 9. | American Academy of Pediatrics; American Academy of Family Physicians; American College of Physicians; Transitions Clinical Report Authoring Group, Cooley WC, Sagerman PJ. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128:182-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 747] [Cited by in RCA: 768] [Article Influence: 54.9] [Reference Citation Analysis (0)] |
| 10. | Suris JC, Akre C. Key elements for, and indicators of, a successful transition: an international Delphi study. J Adolesc Health. 2015;56:612-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 190] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 11. | Shemesh E. Non-adherence to medications following pediatric liver transplantation. Pediatr Transplant. 2004;8:600-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 42] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Anthony SJ, Martin K, Drabble A, Seifert-Hansen M, Dipchand AI, Kaufman M. Perceptions of transitional care needs and experiences in pediatric heart transplant recipients. Am J Transplant. 2009;9:614-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 55] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 13. | Casey BJ, Giedd JN, Thomas KM. Structural and functional brain development and its relation to cognitive development. Biol Psychol. 2000;54:241-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 959] [Cited by in RCA: 898] [Article Influence: 35.9] [Reference Citation Analysis (0)] |
| 14. | Sowell ER, Thompson PM, Holmes CJ, Jernigan TL, Toga AW. In vivo evidence for post-adolescent brain maturation in frontal and striatal regions. Nat Neurosci. 1999;2:859-861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1008] [Cited by in RCA: 926] [Article Influence: 35.6] [Reference Citation Analysis (0)] |
| 15. | Fredericks EM, Magee JC, Eder SJ, Sevecke JR, Dore-Stites D, Shieck V, Lopez MJ. Quality Improvement Targeting Adherence During the Transition from a Pediatric to Adult Liver Transplant Clinic. J Clin Psychol Med Settings. 2015;22:150-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 16. | Boyle MP, Farukhi Z, Nosky ML. Strategies for improving transition to adult cystic fibrosis care, based on patient and parent views. Pediatr Pulmonol. 2001;32:428-436. [PubMed] |
| 17. | Fredericks EM, Dore-Stites D, Lopez MJ, Well A, Shieck V, Freed GL, Eder SJ, Magee JC. Transition of pediatric liver transplant recipients to adult care: patient and parent perspectives. Pediatr Transplant. 2011;15:414-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 18. | Reid GJ, Irvine MJ, McCrindle BW, Sananes R, Ritvo PG, Siu SC, Webb GD. Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics. 2004;113:e197-e205. [PubMed] |
| 19. | McDonagh JE, Southwood TR, Shaw KL; British Society of Paediatric and Adolescent Rheumatology. The impact of a coordinated transitional care programme on adolescents with juvenile idiopathic arthritis. Rheumatology (Oxford). 2007;46:161-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 167] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 20. | Akre C, Ramelet AS, Berchtold A, Suris JC. Educational intervention for parents of adolescents with chronic illness: a pre-post test pilot study. Int J Adolesc Med Health. 2015;27:261-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |