Published online Dec 28, 2016. doi: 10.3748/wjg.v22.i48.10631
Peer-review started: April 14, 2016
First decision: June 20, 2016
Revised: July 13, 2016
Accepted: July 31, 2016
Article in press: August 1, 2016
Published online: December 28, 2016
Processing time: 256 Days and 22.1 Hours
To determine the effects of Lactobacillus acidophilus NCFM on irritable bowel syndrome (IBS) symptoms and quality of life (QoL).
In this randomized triple-blind trial, adult IBS volunteers who were recruited according to Rome III criteria received 109 or 1010 colony-forming units of NCFM or placebo daily for 12 wk. IBS Symptom Severity Score (IBS-SSS), which constituted the primary outcome, and secondary outcomes, including individual IBS symptoms, IBS-related QoL questionnaire, anxiety and depression, defecation frequency, and stool consistency, were assessed at baseline at the end of the 8-wk run-in period, after 4 and 12 wk of intervention, and after a 4-wk washout.
A total of 340 of 391 randomized volunteers completed the trial. IBS-SSS improved over 12 wk of treatment in all treatment groups, decreasing by a mean ± SD of 44.0 ± 80.2, 50.8 ± 82.4, and 48.3 ± 72.2 in the placebo, active low-dose, and active high-dose groups, respectively. Similarly, secondary outcomes did not differ between treatment groups. However, in a post hoc analysis of volunteers with moderate to severe abdominal pain at baseline (VAS > 35/100), the treatment significantly reduced the sensation of abdominal pain. Pain scores fell by 20.8 ± 22.8, 29.4 ± 17.9, and 31.2 ± 21.9 in the placebo, active low-dose, and active high-dose groups, respectively (P value for placebo vs combined active doses = 0.0460).
NCFM alleviates moderate to severe abdominal pain, consistent with earlier observations of this strain mitigating visceral pain through increased analgesic receptor expression.
Core tip: Symptoms of irritable bowel syndrome (IBS) might benefit from probiotic interventions, although mechanistic insights into probiotic function are seldom available. Lactobacillus acidophilus NCFM induces human colonic mucosal opioid receptor expression - the putative mechanism by which visceral pain is alleviated. In this study, 391 volunteers with IBS were treated with 109 or 1010 colony-forming units of NCFM or placebo and evaluated using symptom questionnaires. NCFM was not superior to placebo in improving the composite IBS symptom score, whereas abdominal pain - as an individual symptom - declined in IBS volunteers with moderate to severe pain at baseline.
- Citation: Lyra A, Hillilä M, Huttunen T, Männikkö S, Taalikka M, Tennilä J, Tarpila A, Lahtinen S, Ouwehand AC, Veijola L. Irritable bowel syndrome symptom severity improves equally with probiotic and placebo. World J Gastroenterol 2016; 22(48): 10631-10642
- URL: https://www.wjgnet.com/1007-9327/full/v22/i48/10631.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i48.10631
With a prevalence of 5% to 16% in northern Europe, irritable bowel syndrome (IBS) imposes considerable health care costs on society[1,2]. IBS affects adult age groups evenly but is more common in women[2]. According to the European Food Safety Authority, IBS volunteers can be recruited as an appropriate group for studying bowel discomfort symptoms that also affect the general population[3], allowing the results to be extrapolated to a wider potential market.
A host’s gastrointestinal (GI) microbiota can contribute to IBS etiology and symptomology through changes in bacterial abundance and fermentation products, lower diversity, and instability over time, which are associated with increased epithelial permeability, aberrations in immunity and brain-gut interactions, and altered GI neuromuscular function[4-7]. Thus, manipulation of the GI microbiota with probiotics is a putative therapeutic option for IBS [4,8].
Probiotics, defined as “live microorganisms that, when administered in adequate amounts, confer a health benefit on the host”[9], have shown efficacy in selected randomized clinical trials in relieving IBS symptoms and are generally well tolerated[10-12]. However, the quality of several probiotic intervention studies has been limited due to inadequate sample sizes and intervention periods, poor trial design, and undefined or unstable probiotic products[13]. Moreover, each strain or combination of strains and each dose requires a separate clinical trial to show efficacy [9,10].
Our aim was to perform a high-quality, randomized, triple-blind, and placebo-controlled dose-response clinical trial of 3 statistically adequately sized parallel groups. The supplement that we examined is a well-characterized and stable probiotic strain, mechanistic studies of which have reported putative efficacy in alleviating visceral pain. Lactobacillus acidophilus NCFM increases the visceral pain threshold in a rat model by 44% through the opioid pathway[14] and upregulates μ-opioid receptor (MOR) in humans[15].
Participant-reported severity of functional bowel symptoms, however, has merely been evaluated for a high-concentration combination of L. acidophilus NCFM and Bifidobacterium animalis subsp. lactis Bi-07[16], which is significantly less effective in increasing MOR expression than L. acidophilus NCFM alone[15]. Therefore, assessment of the clinical effects of L. acidophilus NCFM as a single-strain supplement for functional bowel symptoms, including visceral pain, was essential. Two doses, 109 and 1010 colony-forming units (CFU), were selected as clinically adequate and applicable for use in consumer products.
This trial was performed at 2 private clinics in Helsinki and Turku, Finland, from October 2012 to November 2014. Newspaper and radio advertisements, followed by prescreening phone calls, were used to invite potential eligible volunteers to screening visits that were held by gastroenterologists who were experienced in functional bowel disorders, including IBS. The recruited volunteers were adults (18-65 years) who were diagnosed with IBS according to Rome III criteria[17]. Volunteers who suffered from severe IBS symptoms were excluded due to the use of medications (strong pain medication, diarrhea medication, and laxatives) that might have confounded the primary outcome measure. Other inclusion criteria were sufficient general health and orientation for participation in the study, adequate Finnish language skills for being interviewed and completing questionnaires, high likelihood of compliance with and completion of the study, and a body mass index (BMI) between 19 and 35.
Volunteers were excluded if they had participated in a clinical trial with an investigational product (IP) or drug within 3 mo prior to the screening, were likely to be noncompliant with the protocol or judged to be unsuitable for study participation by the investigator for any reason, were planning major changes in lifestyle (e.g., diet, dieting, exercise level, travel), had a history of drug or alcohol abuse, were pregnant or breastfeeding, were diagnosed with or suspected of having organic GI disease (e.g., colitis, Crohn’s disease, celiac disease, bowel surgery, recurrent diverticulitis), or had severely impaired general health, including cancer and cancer therapy. Lactose-intolerant volunteers were allowed to enter the trial if they followed a non lactose diet. Any previous allergic reaction to any substance in the study product was also considered an exclusion criterion.
Medications that could affect the outcomes, including anticholinergic medications, antibiotics (including use during the 3 mo prior to the start of the study), pain medications that contained opiates or morphine, weight loss medication, misoprostol, 5-HT3 receptor antagonists, antacids with magnesium or aluminum, diarrhea medication, medication that accelerates the emptying of the stomach, sulfasalazine, laxatives, cholestyramine, cytostatics, biological medications, oral steroids (3 mo prior to and during the study), and probiotic products, excluded subjects from participation in the trial. Iron supplements, antidepressants, fiber supplements, statins, thyroxine, coxibs, acid medication, inhaled steroids, and other non excluding medications that did not affect outcome measures in the clinician’s opinion were allowed during the trial if they had been consumed for at least 30 d at the same dose.
During the screening visit, thorough demographic data were collected, including lifestyle habits, diet, medical history, and family history of GI disturbances. Screening safety blood tests included a basic blood count, C-reactive protein (CRP), celiac test, lactase gene test, and thyroid-stimulating hormone for constipated IBS volunteers. The test results complied with the inclusion and exclusion criteria and were clinically within normal-range values according to the recruiting gastroenterologists.
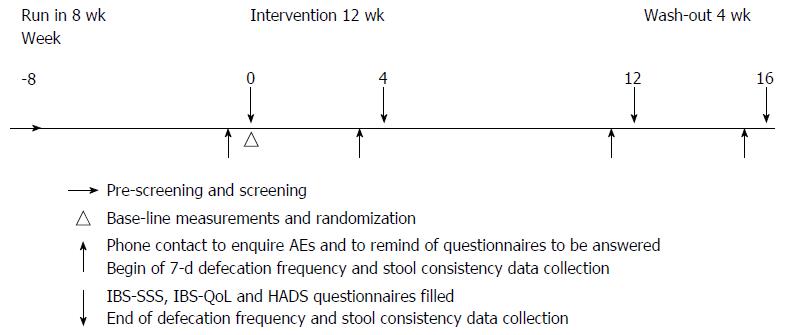
The trial was a randomized, triple-blind (volunteers, investigators, and statisticians blinded), placebo-controlled, dose-response intervention to determine the efficacy of a probiotic supplement in reducing IBS Symptom Severity Score (IBS-SSS)[18]. The trial comprised an 8-wk run-in period, a 12-wk intervention phase, and a 4-wk washout period (Figure 1). Outcome measures were assessed using questionnaires, and adverse events (AEs) were recorded through phone calls. Volunteers who withdrew were not replaced.
The primary outcome was the change in IBS-SSS from baseline at the end of the run-in period to after 12 wk of treatment[18]. IBS-SSS is a composite score of abdominal pain, number of days with abdominal pain, bloating/distension, satisfaction with bowel habits, and IBS-related quality of life (QoL). Each measure is rated from 0 to 100, with total scores ranging from 0 to 500. Based on previous trials[19,20], a 15% change in the IBS-SSS was determined to be clinically significant in measuring efficacy. QoL was evaluated with a thorough 34-item IBS-related QoL questionnaire (IBS-QoL), analyzed as a total score and as subscales on dysphoria, interference with activity, body image, health-related worries, food avoidance, social reactions, sexuality, and relationships[21]. Psychological comorbidities were evaluated with the Hospital Anxiety and Depression Scale (HADS) questionnaire[22].
IBS-SSS, IBS-QoL, and HADS data were collected at the end of the run-in, after 4 and 12 wk of treatment, and after the 4-wk washout. Weekly bowel movement frequency and consistency were recorded prior to each outcome assessment time point with an in-house questionnaire, based on the Bristol Stool Form Scale[23]. For analysis, stool consistencies were grouped into constipation (Bristol Scale 1 or 2), diarrhea (Bristol Scale 6 or 7), and normal (Bristol Scale 3, 4, or 5). Overall satisfaction with the treatment with regard to IBS symptoms was measured with a dichotomous adequate relief (AR) question[24]. The volunteers were instructed to compare AR from IBS symptoms during the past week to their symptom severity prior to consuming IPs. Volunteers who reported AR for at least half of the intervention weeks were considered to be responders. AR data were collected throughout the 12-wk intervention.
Prior to each visit (end of run-in, week 4, week 12, and end of washout), research nurses contacted the volunteers by phone to inquire about AEs and remind them of the sampling time point procedures.
The IPs were administered orally in 1 daily capsule that contained 109 (low dose) or 1010 (high dose) CFU of L. acidophilus NCFM (ATCC 700396), with microcrystalline cellulose as the excipient or microcrystalline cellulose as placebo. All treatments were supplied by Danisco USA (Madison, Wisconsin, United States). The formulations of all 3 treatments were similar in smell, taste, and appearance. The IPs were stored at -20 °C until they were distributed to the clinics, where they were refrigerated below 6 °C. Volunteers were allowed to store the IPs refrigerated or at room temperature. The CFU counts were checked in the active and placebo products during and after the trial.
Screening safety tests were performed by certified clinical laboratories of the private clinics Mehiläinen Töölö (Helsinki, Finland) and Mehiläinen Turku (Turku, Finland).
Volunteers received 84 capsules and were instructed to return the container after the 84-d treatment period. Leftover capsules were counted to estimate compliance.
This study was conducted according to the 2008 Sixth Revision of the Declaration of Helsinki, the EMA Note for Guidance on Good Clinical Practice (CPMP/ICH/135/95 - in operation 17.01.97), and laws and regulations for clinical research in Finland. Written informed consent was obtained from each volunteer before any study-specific procedures. The trial was registered at Clinicaltrials.gov under the identifier NCT01728610.
Case report forms were 100% monitored and double-entered independently into a database that was created with SAS®. Queries were raised in cases of illegible, missing, or inconsistent data. All discrepancies were resolved before the database was locked. Data management and statistics were performed by 4Pharma Ltd.
Determination of sample size: The primary analysis variable was the change in IBS-SSS from baseline to week 12. Baseline levels were estimated to be approximately 250 (halfway on the 0-500 scale). A difference of 15% - i.e., 37.5 points - was used in the sample size calculation[20]. Using 80% power and a 2-sided alpha level of 0.05, the sample size was calculated to be 104 for each group. Taking into account a discontinuation rate of 20%, approximately 390 patients were needed for randomization. The sample sizes were calculated using NQuery Advisor, version 7.0.
Analysis sets: The intent-to-treat dataset (ITT) included all randomized volunteers who received at least 1 dose of the IP and had at least 1 post baseline efficacy measurement available. The per protocol dataset (PP) was a subset of the ITT dataset, excluding volunteers and measurements for a given volunteer with major protocol violation(s) or concomitant medication use that was expected to alter the primary outcome. Volunteer classification into the ITT and PP populations was detailed after locking the database and completed before the study was unmasked. In addition, post hoc analyses of volunteers with IBS-SSS pain score VAS > 35/100 were performed.
Randomization: Volunteers were randomized at the end of the 8-wk run-in phase, because the long run-in period created risk of a high dropout rate. Randomization was performed with Research Randomizer[25], applying non repeating numbers in blocks of 6. Volunteers, investigators, statisticians, and monitors were blinded until the database was locked and the Statistical Analyses Plan was completed. The clinics were supplied with sealed, volunteer-specific envelopes for revealing the randomization code, if required by the investigators. None of the envelopes was opened during the trial.
Analysis of efficacy: Descriptive statistics for all variables were computed, and the disposition of volunteers was summarized by treatment. The primary efficacy variable (change in IBS-SSS from baseline) was analyzed using a repeated measures analysis of covariance (RM ANCOVA) model. The differences (low dose vs placebo and high dose vs placebo) in changes from baseline in IBS symptom score at 12 wk and their 95%CI were estimated with the RM ANCOVA model. Explorative comparisons were performed for high dose vs low dose and combined active group vs placebo and for within-group changes from baseline.
The individual domains of the IBS-SSS were analyzed with a similar RM ANCOVA model that was applied for IBS-SSSs. A logistic regression model was used to compare treatment groups against placebo for AR responder status. Changes in HADS and IBS-QOL scores from baseline were analyzed using an RM ANCOVA model. The stool consistencies (Bristol Stool Form) and defecation frequencies were summarized descriptively. Simple t-test was used in the post hoc analyses of subgroups (e.g., pain score VAS > 35/100).
All statistical analyses and volunteer data listings were performed at 4Pharma Ltd using SAS, version 9.3 (SAS Institute Inc., Cary, NC, United States).
Safety analyses: All randomized volunteers who received the study treatment were included in the safety analysis. AEs were counted by volunteer, event, type, treatment, severity, and causality. Each symptom of an AE or serious adverse event (SAE) case was recorded separately.
The statistical methods were reviewed by statistician Teppo Huttunen, 4Pharma Ltd.
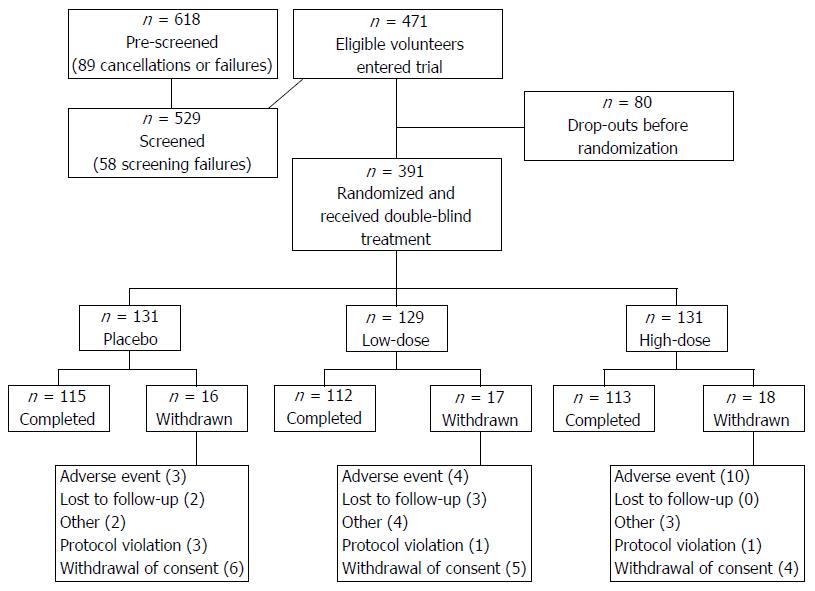
Altogether, 618 volunteers were prescreened by telephone interview for compliance with the inclusion and exclusion criteria, and thereafter, the eligibility of 529 potential volunteers was confirmed by gastroenterologists. A total of 471 volunteers entered the trial, of whom 391 were randomized after the 8-wk run-in phase, with 340 (87%) completing the trial (Figure 2). The results are presented for the ITT dataset; those for the PP dataset were comparable.
The volunteers from Helsinki (n = 276; 34 dropouts) and Turku (n = 115; 17 dropouts) were randomized evenly to the 3 treatments. The treatment groups were comparable with regards to age, sex, BMI, and lifestyle habits, including type of diet, exercise level, alcohol consumption, smoking (Table 1), and IBS symptom characteristics (Table 2). All groups were predominantly female (71.8% to 79.4% female), and men had a higher BMI (60.6% and 36.6% of male and female volunteers, respectively, had a BMI > 25). All findings on vital signs and the safety blood tests taken at screening were evaluated for their clinical significance in relation to the inclusion and exclusion criteria.
| Characteristics | Placebo (n = 131) | Low-dose (n = 129) | High-dose (n = 131) |
| Age (yr) | 49.4 ± 12.9 | 47.1 ± 13.3 | 47.2 ± 12.5 |
| Gender | |||
| Male | 37 (28.2) | 35 (27.1) | 27 (20.6) |
| Female | 94 (71.8) | 94 (72.9) | 104 (79.4) |
| BMI (kg/m2) | 24.9 ± 3.7 | 24.7 ± 3.7 | 24.5 ± 3.9 |
| Diet | |||
| Low-carbohydrate | 2 (1.5) | 0 (0.0) | 0 (0.0) |
| Vegetarian | 1 (0.8) | 2 (1.6) | 0 (0.0) |
| Non-lactose | 26 (19.8) | 32 (24.8) | 26 (19.8) |
| Regular | 77 (58.8) | 63 (48.8) | 67 (51.1) |
| Probiotics | |||
| Daily user | 24 (18.3) | 25 (19.4) | 18 (13.7) |
| Irregular user | 18 (13.7) | 17 (13.2) | 29 (22.1) |
| History of using | 65 (49.6) | 62 (48.1) | 66 (50.4) |
| No use | 23 (17.6) | 25 (19.4) | 18 (13.7) |
| N/A | 1 (0.8) | 0 (0.0) | 0 (0.0) |
| Exercise level | |||
| > 30 min 3 times a week | 62 (47.3) | 63 (48.8) | 59 (45.0) |
| ≤ 30 min 3 times a week | 57 (43.5) | 56 (43.4) | 63 (48.1) |
| No exercise | 12 (9.2) | 10 (7.8) | 9 (6.9) |
| Alcohol consumption | |||
| > 14 units/wk | 1 (0.8) | 0 (0.0) | 0 (0.0) |
| ≤ 14 units/wk | 96 (73.3) | 90 (69.8) | 90 (68.7) |
| Non-drinker | 34 (26.0) | 39 (30.2) | 41 (31.3) |
| Tobacco smoking | |||
| Current use | 11 (8.4) | 11 (8.5) | 14 (10.7) |
| Never used | 80 (61.1) | 86 (66.7) | 88 (67.2) |
| History of use | 40 (30.5) | 32 (24.8) | 29 (22.1) |
| Drug abuse | |||
| Never used | 131 (100) | 129 (100) | 131 (100) |
| Placebo (n = 131) | Low-dose (n = 129) | High-dose (n = 131) | |
| IBS subtype | |||
| IBS-C | 25 (19.1) | 20 (15.5) | 20 (15.3) |
| IBS-D | 49 (37.4) | 51 (39.5) | 52 (39.7) |
| IBS-M | 56 (42.7) | 58 (45.0) | 58 (44.3) |
| IBS-U | 1 (0.8) | 0 (0.0) | 1 (0.8) |
| Postinfectious IBS | 9 (6.9) | 4 (3.1) | 7 (5.3) |
| Psychological comorbidities | 9 (6.9) | 6 (4.7) | 13 (9.9) |
| Symptoms provoked by specific food | 103 (79.8)1 | 116 (89.9) | 120 (91.6) |
| Family history of intestinal disorders or diseases | 95 (72.5) | 97 (75.2) | 92 (70.8)2 |
Prior and concomitant medications for the alimentary tract, pain, and anxiety/depression were recorded, with gastroenterologists evaluating any putative bias of them on efficacy measures. The most common medications used before and during the study were drugs for gastric acid disorders, nonsteroidal anti-inflammatory drugs, and antidepressants/anxiolytics. Also, 36 volunteers were on thyroxine medication due to hypothyreosis.
The L. acidophilus NCFM CFU count was confirmed to be adequate for both active treatment doses (> 1.04 × 1010 and > 9.8 × 109 CFU/capsule for the high and low doses, respectively). For the placebo, the L. acidophilus NCFM count was below < 3.2 × 102 CFU/capsule. According to the number of returned capsules 95%, 95%, and 94% of IP capsules were consumed in the placebo and low-dose and high-dose treatment groups, respectively.
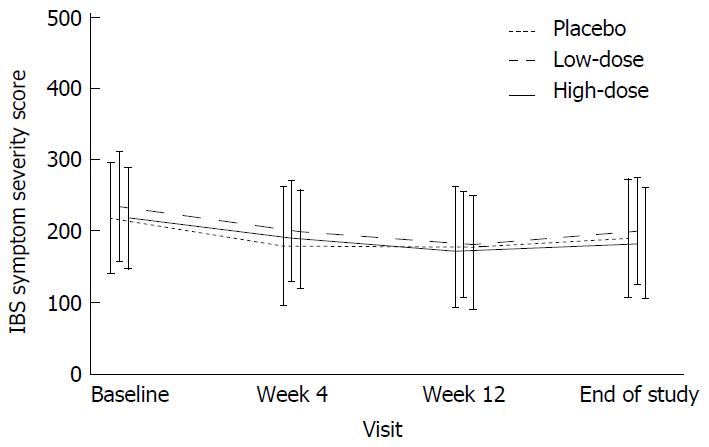
The IBS-SSS improved significantly from baseline to the end of the intervention by a mean ± SD of 44.0 ± 80.2, 50.8 ± 82.4, and 48.3 ± 72.2 in the placebo, low-dose, and high-dose groups, respectively (P < 0.001 for all groups), with no significance between the placebo and active groups (Figure 3). Results for individual IBS-SSS item scores were comparable between groups (Table 3). However, in a post hoc analysis of a subgroup of volunteers who suffered from moderate to severe pain (pain score VAS > 35/100 at baseline), L. acidophilus NCFM significantly reduced abdominal pain in the combined active groups compared with placebo (Table 4).
| Treatment | Baseline | Week 12 | Change from baseline | Within-group comparison | Comparison with placebo | Comparison with low- and high-dose | ||
| n | mean ± SD | n | mean ± SD | mean ± SD | P value | P value | P value | |
| Severity of pain | ||||||||
| Placebo | 121 | 20.2 ± 20.6 | 118 | 18.5 ± 20.7 | -2.2 ± 21.8 | 0.024 | NA | 0.303 |
| Low-dose | 124 | 24.1 ± 22.3 | 110 | 18.3 ± 18.6 | -5.2 ± 24.4 | 0.005 | 0.640 | NA |
| High-dose | 122 | 24.3 ± 21.5 | 113 | 16.4 ± 17.8 | -7.9 ± 21.8 | < 0.001 | 0.189 | NA |
| Number of days with pain over 10 d | ||||||||
| Placebo | 114 | 3.8 ± 2.8 | 111 | 2.8 ± 2.8 | -1.0 ± 2.7 | < 0.001 | NA | 0.234 |
| Low-dose | 115 | 4.4 ± 2.8 | 105 | 3.3 ± 2.6 | -1.1 ± 2.9 | < 0.001 | 0.470 | NA |
| High-dose | 121 | 4.1 ± 2.8 | 106 | 2.9 ± 2.4 | -1.2 ± 2.5 | < 0.001 | 0.634 | NA |
| Bloating/Distension | ||||||||
| Placebo | 121 | 39.0 ± 28.0 | 118 | 30.7 ± 25.6 | -8.3 ± 23.6 | < 0.001 | NA | 0.669 |
| Low-dose | 122 | 40.5 ± 29.9 | 110 | 31.0 ± 25.7 | -9.4 ± 29.6 | < 0.001 | 0.905 | NA |
| High-dose | 122 | 37.1 ± 26.6 | 113 | 31.0 ± 27.3 | -6.1 ± 25.8 | 0.002 | 0.535 | NA |
| Satisfaction with bowel habits | ||||||||
| Placebo | 121 | 57.4 ± 22.6 | 118 | 47.3 ± 24.2 | -10.3 ± 21.4 | < 0.001 | NA | 0.964 |
| Low-dose | 124 | 59.4 ± 22.7 | 110 | 46.3 ± 19.8 | -11.8 ± 22.4 | < 0.001 | 0.701 | NA |
| High-dose | 122 | 55.0 ± 19.7 | 113 | 46.4 ± 22.6 | -8.3 ± 23.3 | < 0.001 | 0.757 | NA |
| Interference of IBS with quality of life | ||||||||
| Placebo | 121 | 62.4 ± 17.0 | 118 | 48.6 ± 22.1 | -13.9 ± 20.3 | < 0.001 | NA | 0.210 |
| Low-dose | 124 | 60.8 ± 16.9 | 110 | 50.1 ± 19.4 | -9.8 ± 16.5 | < 0.001 | 0.133 | NA |
| High-dose | 122 | 59.8 ± 13.5 | 113 | 47.9 ± 16.5 | -11.7 ± 13.6 | < 0.001 | 0.509 | NA |
| Treatment | n | Baseline | Week 12 | Change from baseline | Mean difference for combined active doses | P value |
| mean ± SD | mean ± SD | mean ± SD | 95%CI | |||
| Placebo | 29 | 51.1 (9.3) | 30.3 (22.9) | -20.8 (22.8) | ||
| Low-dose | 36 | 53.6 (10.9) | 24.4 (19.4) | -29.4 (17.9) | -9.5 (-18.8; -0.17) | 0.046 |
| High-dose | 34 | 52.1 (10.7) | 21.9 (20.6) | -31.2 (21.9) |
During the intervention period, 28.4%, 25.0%, and 26.5% of volunteers considered their IBS symptoms to have been adequately relieved with the placebo, low-dose, and high-dose treatments, respectively (P = 0.8371 between groups by logistic regression). The IBS-QoL reflected a higher QoL at the end of the intervention in all treatment groups (Table 5), although neither active treatment dose was superior to placebo. The HADS total score declined significantly from baseline to the end of the intervention in both active treatment groups, HADS anxiety improved significantly in all treatment groups, but HADS depression improved significantly only in the high-dose group. However, none of the between-group comparisons reached statistical significance, although total HADS and HADS anxiety were slightly lower in the high-dose group compared with placebo (Table 5).
| Treatment | Baseline | Week 12 | Change from baseline | Within-group comparison | Comparison with placebo | Comparison with low- and high-dose | ||
| n | mean ± SD | n | mean ± SD | mean ± SD | P value | P value | P value | |
| IBS-QoL | ||||||||
| Placebo | 121 | 66.4 ± 17.5 | 118 | 73.2 ± 19.0 | 7.0 ± 12.3 | < 0.001 | NA | 0.412 |
| Low-dose | 124 | 63.9 ± 19.0 | 110 | 71.6 ± 19.3 | 7.4 ± 12.3 | < 0.001 | 0.812 | NA |
| High-dose | 122 | 68.2 ± 16.5 | 113 | 76.5 ± 15.8 | 8.5 ± 8.8 | < 0.001 | 0.238 | NA |
| HADS total score | ||||||||
| Placebo | 119 | 9.2 ± 5.6 | 110 | 8.6 ± 6.6 | -0.4 ± 4.3 | 0.302 | NA | 0.134 |
| Low-dose | 122 | 10.1 ± 5.7 | 109 | 9.2 ± 6.0 | -1.0 ± 4.4 | 0.034 | 0.435 | NA |
| High-dose | 118 | 9.7 ± 5.5 | 109 | 8.2 ± 5.8 | -1.5 ± 3.9 | < 0.001 | 0.071 | NA |
| HADS-Anxiety | ||||||||
| Placebo | 121 | 5.9 ± 3.5 | 114 | 5.3 ± 3.6 | -0.4 ± 2.6 | 0.036 | NA | 0.246 |
| Low-dose | 122 | 6.1 ± 3.3 | 109 | 5.5 ± 3.1 | -0.6 ± 2.7 | 0.011 | 0.726 | NA |
| High-dose | 119 | 6.2 ± 3.3 | 109 | 5.0 ± 3.1 | -1.0 ± 2.2 | < 0.001 | 0.099 | NA |
| HADS-Depression | ||||||||
| Placebo | 119 | 3.4 ± 2.9 | 111 | 3.4 ± 3.6 | 0.0 ± 2.3 | 0.906 | NA | 0.162 |
| Low-dose | 124 | 4.0 ± 3.0 | 109 | 3.7 ± 3.4 | -0.3 ± 2.2 | 0.258 | 0.376 | NA |
| High-dose | 119 | 3.5 ± 2.9 | 110 | 3.2 ± 3.1 | -0.4 ± 2.4 | 0.041 | 0.125 | NA |
None of the treatments had undesired effects on stool consistency (Table 6).
| n | Change to optimal from constipation or diarrhea | Change to constipation or diarrhea from optimal | |
| Placebo | 131 | ||
| Week 4 | 18 (13.7) | 15 (11.5) | |
| Week 12 | 21 (16.0) | 18 (13.7) | |
| Washout | 20 (15.3) | 17 (13.0) | |
| Low-dose | 129 | ||
| Week 4 | 26 (20.2) | 13 (10.1) | |
| Week 12 | 27 (20.9) | 14 (10.9) | |
| Washout | 14 (10.9) | 12 (9.3) | |
| High-dose | 131 | ||
| Week 4 | 14 (10.7) | 16 (12.2) | |
| Week 12 | 18 (13.7) | 20 (15.3) | |
| Washout | 14 (10.7) | 18 (13.7) | |
| Total | 391 | 172 (44.0) | 143 (36.6) |
AEs were evenly distributed in all groups, with 81, 57, and 61 AEs recorded during the treatment period in the placebo, low-dose, and high-dose treatment groups, respectively. The most common treatment-emergent AEs were GI disorders (abdominal discomfort, abdominal distension, abdominal pain, constipation, diarrhea, flatulence), gastroenteritis, and influenza. Potentially IP-related AEs - mild GI symptoms, which might also have been due to all volunteers having IBS that presented with similar symptoms - were recorded for 7, 7, and 9 volunteers in the placebo, low-dose, and high-dose treatment groups, respectively.
AEs led to discontinuation 10, 4, and 3 times in the high-dose, low-dose, and placebo groups, respectively, but these cases were not considered IP-related safety issues, based on the possibility of the IP-related cases being general IBS symptoms. Two SAE cases that presented with 3 symptoms were encountered: pneumonia with fever and cough and a case of syncope that resulted in a hospital visit; neither was associated with the IP or any trial procedure. The case of pneumonia, which involved hospitalization and antibiotic treatment, led to discontinuation.
This study is the first adequately powered clinical trial to determine the effects of L. acidophilus NCFM on IBS symptoms using patient-reported outcomes. The L. acidophilus NCFM strain is well characterized[26] and has been commercially available as a probiotic for several decades. It has been associated with the alleviation of the perception of visceral pain as a 2-strain blend with B. lactis Bi-07 in volunteers with bloating and among colonoscopy patients[14,15,27]. In a mechanistic study, however, L. acidophilus NCFM, as a single-strain supplement, was more effective than the combination in enhancing human colonic MOR expression and activity, although both treatments relieved bowel symptoms, albeit insignificantly[15,16].
L. acidophilus NCFM has been shown to elevate the visceral pain threshold in a rat model by 44% through the MOR-mediated pathway with an efficacy that is comparable with that of 1 mg/kg subcutaneous morphine[14]. Thus, there was tremendous interest in determining the efficacy of L. acidophilus NCFM as a single-strain supplement in mitigating functional bowel symptoms.
The volunteer recruitment was successful, and the trial completion rate and IP compliance were high. All 391 randomized volunteers fulfilled the Rome III criteria for IBS, with an even distribution of IBS subtypes and demographics between groups. Blood tests were performed at the screening visit (basic blood count and CRP) to rule out inflammatory causes of the bowel symptoms. Most volunteers (57%) had undergone a colonoscopy in the past due to chronic GI symptoms to rule out organic or inflammatory causes, but endoscopy was not performed during the screening.
Based on a crossover trial that raised concerns over the inadequate length of a 1-mo run-in period[28], all volunteers refrained from using any commercial or trial-related probiotics over an 8-wk run-in period to reduce any putative carryover effects. A total of 83% of randomized volunteers had a history of consuming commercial probiotics. The intervention period was designed to last for 12 wk to follow up on the efficacy and AEs for a sufficient period of time[10] and to limit the placebo effect toward the end of the trial. Altogether, we recruited an adequate number of reliably diagnosed, extensively examined volunteers who were not using any concomitant medications or supplements that could have affected outcomes. The treatment was a well-characterized probiotic strain that was supplemented in 2 common doses for an adequately long intervention period.
However, in this trial, based on a composite score of IBS symptom severity (IBS-SSS), L. acidophilus NCFM was not superior to placebo. No significant differences in the secondary outcomes were observed between groups, and none of the outcomes showed a dose-response effect. Nevertheless, in post hoc analyses of a subgroup that presented with moderate to severe abdominal pain at baseline (IBS-SSS pain score on VAS > 35/100 at baseline; active groups combined vs placebo), the level of abdominal pain declined in the active groups at week 12. These data are consistent with previous mechanistic findings of greater MOR expression and activity during L. acidophilus NCFM treatment in humans and rats[14,15] and earlier recovery from colonoscopy-associated pain[27].
IBS is associated with significant placebo effects, in part due to the subjective nature of the outcome measures (Shah and Pimentel, 2014). Our trial had an 8-wk run-in period during which volunteers did not consume any product (including placebo); thus, there was no pre-randomization selection for high placebo responders. The study products were administered daily, which should be beneficial for minimizing a placebo effect. However, the high frequency of contact by research nurses might have heightened the placebo response, although their attention and care were targeted originally toward evaluating safety adequately and ensuring high compliance with the protocol.
Our principal challenge was the significant placebo effect, which was comparable with the efficacy of the active treatments. A decrease of > 50 in IBS-SSS indicates clinical improvement of symptoms[18]. In the present trial, the IBS-SSS decreased from 44.0 to 50.8 in the 3 different treatment groups suggesting a borderline clinically significant effect. Similarly, IBS-QoL scores corresponded to moderate symptom severity at baseline vs mild symptom severity by the end of treatment in all groups[21]. Also, with the AR questionnaire, the placebo was as effective as the active treatment. Volunteers had had difficulty comprehending whether the weekly AR question should be referenced to the base-line period, as intended, or to the previous calendar week. Thus some participants compared consecutive intervention weeks rather than treatment to baseline in the AR questionnaire.
HADS was applied to subgroup participants by psychological comorbidity which has previously been associated with characteristics of intestinal microbiota[29]. Statistically significant reductions in HADS were observed in the active treatment groups. However, these changes were small and likely of no clinical relevance; further, the prevalence of anxiety and depression was low, and for all treatment groups HADS averages throughout the study were at normal levels[22]. No subgroup analyses were implemented. Nevertheless, the changes in HADS indicate a target for future study in a more appropriate population.
Changes in stool consistency are not unexpected for an IBS population[30], and none of the treatments appeared to cause undesirable alterations in stool form. Defecation frequencies were close to normal limits, suggesting that diarrhea and constipation in IBS volunteers are subjective phenomena that are related to defecation events, rather than a result of hard stool and slow transit or loose stool and accelerated transit. Thus recruitment of all IBS symptom subtypes is justifiable.
Selecting volunteers from only 1 IBS symptom subgroup or setting a threshold for baseline symptom severity as applied by Sisson and colleagues[31] can reduce variation in the response to treatment. However, our objective was to recruit IBS volunteers as a representation of the general population[3], which would have been distorted by selecting subgroups or IBS patients with more severe symptoms. In addition, because the etiology of IBS is multifactorial and, to a large extent, unknown and because symptom subgroups tend to vary over time in each volunteer[30], selecting between symptom subgroups is challenging. Moreover, excluding volunteers whom consume diarrhea medication, laxatives, and opiate- or morphine-containing pain medications was necessary, because these agents influence the outcome, but it also effectively excluded volunteers with severe IBS symptoms.
Another shortcoming in assessing the efficacy of bowel symptoms was the infrequent and retrospective evaluation of IBS symptoms[32]. The symptom questionnaires were administered 4 times in total and only twice during the 12-wk intervention period. More frequent assessments were initially considered to be a risk for noncompliance due to the laboriousness of answering so many questionnaires. Moreover, although the IBS-SSS questionnaire inquires about symptom severity over the past 10 d, the volunteers’ symptoms, everyday events, and mood when they complete the questionnaires are likely to bias the answers, resulting in potentially irrelevant variations in scores. Because volunteers were not severely symptomatic (mean IBS-SSS at baseline corresponded to moderate for all treatment groups), inquiring about symptom frequency instead of severity might have been more sensitive in measuring efficacy[33].
AEs were evenly distributed between groups. The slightly higher number of volunteer discontinuations due to AEs in the active high-dose group was not treatment-related. Digestive symptoms were the chief manifestation of the inclusion criteria of the study population; thus, GI discomfort, recorded as a possibly treatment-related AE, might have also been part of their normal symptomology.
L. acidophilus NCFM can be consumed safely by adult IBS volunteers over a 3-mo period but is ineffective against IBS symptoms in general compared to placebo. However, L. acidophilus NCFM treatment alleviated abdominal pain in IBS volunteers with at least moderately severe visceral pain. More frequent - preferably daily - assessment of bowel symptoms with a user-friendly application is recommended for future trials in this area. Moreover, enquiring individual symptoms rather than a composite score sum may be more applicable. Among the recruited IBS participants with moderate symptom severity at baseline bowel movement frequency appeared normal regardless of stool consistency and anxiety and depression levels were not clinically notable.
The IBS-SSS questionnaire (Francis et al[18], 1997) was back-translated into Finnish by the medical translation company Anita Paajanen-Mannila Oy and kindly provided for use in this study by Oy Verman Ab and Kajsa Kajander. We thank research nurses Päivi Kuusniemi for coordinating the clinics and Laura Lehtonen for her substantial efforts in archiving the trial according to GCP. We gratefully acknowledge Tad Stewart and Angela Paulsen for manufacturing the IP, Kaisa Olli for monitoring and Nicolas Yeung for providing the audio Core Tip. The authors would also like to thank gastroenterologists Tiina Kojo, Helena Kemppainen, and Janne Rajala for their efforts in screening participants and the volunteers for their commitment and participation.
Functional bowel symptoms are a common disturbance encountered transiently by most humans and in a chronic manner by many. Irritable bowel syndrome (IBS) is a functional bowel disorder with abdominal pain as its core symptom. In the present trial, Lactobacillus acidophilus NCFM, a probiotic bacterium that is known to enhance analgesic receptor expression in the gastrointestinal (GI) tract of rodents and humans, was evaluated for its ability to alleviate IBS symptoms.
In probiotic research there is a great demand for high quality clinical trials to show potential health efficacy for well-defined probiotic strains. This applies to an array of health areas, including GI wellbeing. On the other hand, also mechanistic insight into the modes of action of probiotics is required to enlighten their efficacy.
The present clinical trial was conducted with high quality applying an adequate population for statistical power and a well characterized probiotic strain with prior mechanistic efficacy data. A thorough set of participant-reported outcomes were evaluated on bowel symptoms, quality of life, psychological wellbeing and defecation habit and stool consistency. The participants complied well with the trial protocol allowing analysis of a comparatively large and complete dataset.
In the present trial the tested strain was not superior to placebo on IBS symptom alleviation in general. However, abdominal pain was relieved among participants with moderate to severe abdominal pain at baseline. The trial also gives insight into design and conduct of probiotic clinical trials on functional bowel disorders.
This article describes a very well designed clinical trial on the effect of the probiotic strain L. acidophilus NCFM in two doses on symptoms in IBS patients. The trial design is of high-quality including the use of a well-defined strain, as well as an adequate number of participants and a long enough intervention period.
Manuscript source: Unsolicited manuscript
Specialty Type: Gastroenterology and Hepatology
Country of Origin: Finland
Peer-Review Report Classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Ducrotte P, Konig J, Seow-Choen F, Lakatos PL S- Editor: Gong ZM L- Editor: A E- Editor: Zhang FF
| 1. | Hillilä MT, Färkkilä MA. Prevalence of irritable bowel syndrome according to different diagnostic criteria in a non-selected adult population. Aliment Pharmacol Ther. 2004;20:339-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 102] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 2. | Krogsgaard LR, Engsbro AL, Bytzer P. The epidemiology of irritable bowel syndrome in Denmark. A population-based survey in adults ≤50 years of age. Scand J Gastroenterol. 2013;48:523-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 3. | EFSA. Guidance on the scientific requirements for health claims related to gut and immune function. EFSA. 2011;9:1984. [RCA] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 4. | Hyland NP, Quigley EM, Brint E. Microbiota-host interactions in irritable bowel syndrome: epithelial barrier, immune regulation and brain-gut interactions. World J Gastroenterol. 2014;20:8859-8866. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 36] [Reference Citation Analysis (0)] |
| 5. | Kennedy PJ, Cryan JF, Dinan TG, Clarke G. Irritable bowel syndrome: a microbiome-gut-brain axis disorder? World J Gastroenterol. 2014;20:14105-14125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 215] [Cited by in RCA: 219] [Article Influence: 19.9] [Reference Citation Analysis (3)] |
| 6. | Rajilić-Stojanović M, Jonkers DM, Salonen A, Hanevik K, Raes J, Jalanka J, de Vos WM, Manichanh C, Golic N, Enck P. Intestinal microbiota and diet in IBS: causes, consequences, or epiphenomena? Am J Gastroenterol. 2015;110:278-287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 268] [Cited by in RCA: 267] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 7. | Moloney RD, Johnson AC, O’Mahony SM, Dinan TG, Greenwood-Van Meerveld B, Cryan JF. Stress and the Microbiota-Gut-Brain Axis in Visceral Pain: Relevance to Irritable Bowel Syndrome. CNS Neurosci Ther. 2016;22:102-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 259] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 8. | Bonfrate L, Tack J, Grattagliano I, Cuomo R, Portincasa P. Microbiota in health and irritable bowel syndrome: current knowledge, perspectives and therapeutic options. Scand J Gastroenterol. 2013;48:995-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (1)] |
| 9. | Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, Morelli L, Canani RB, Flint HJ, Salminen S. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;11:506-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4055] [Cited by in RCA: 5536] [Article Influence: 503.3] [Reference Citation Analysis (2)] |
| 10. | Ford AC, Quigley EM, Lacy BE, Lembo AJ, Saito YA, Schiller LR, Soffer EE, Spiegel BM, Moayyedi P. Efficacy of prebiotics, probiotics, and synbiotics in irritable bowel syndrome and chronic idiopathic constipation: systematic review and meta-analysis. Am J Gastroenterol. 2014;109:1547-1561; quiz 1546, 1562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 595] [Cited by in RCA: 489] [Article Influence: 44.5] [Reference Citation Analysis (0)] |
| 11. | Hungin AP, Mulligan C, Pot B, Whorwell P, Agréus L, Fracasso P, Lionis C, Mendive J, Philippart de Foy JM, Rubin G. Systematic review: probiotics in the management of lower gastrointestinal symptoms in clinical practice -- an evidence-based international guide. Aliment Pharmacol Ther. 2013;38:864-886. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 138] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 12. | Wall GC, Bryant GA, Bottenberg MM, Maki ED, Miesner AR. Irritable bowel syndrome: a concise review of current treatment concepts. World J Gastroenterol. 2014;20:8796-8806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Sanders ME, Guarner F, Guerrant R, Holt PR, Quigley EM, Sartor RB, Sherman PM, Mayer EA. An update on the use and investigation of probiotics in health and disease. Gut. 2013;62:787-796. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 345] [Cited by in RCA: 337] [Article Influence: 28.1] [Reference Citation Analysis (0)] |
| 14. | Rousseaux C, Thuru X, Gelot A, Barnich N, Neut C, Dubuquoy L, Dubuquoy C, Merour E, Geboes K, Chamaillard M. Lactobacillus acidophilus modulates intestinal pain and induces opioid and cannabinoid receptors. Nat Med. 2007;13:35-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 525] [Cited by in RCA: 541] [Article Influence: 28.5] [Reference Citation Analysis (0)] |
| 15. | Ringel-Kulka T, Goldsmith JR, Carroll IM, Barros SP, Palsson O, Jobin C, Ringel Y. Lactobacillus acidophilus NCFM affects colonic mucosal opioid receptor expression in patients with functional abdominal pain - a randomised clinical study. Aliment Pharmacol Ther. 2014;40:200-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 51] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 16. | Ringel-Kulka T, Palsson OS, Maier D, Carroll I, Galanko JA, Leyer G, Ringel Y. Probiotic bacteria Lactobacillus acidophilus NCFM and Bifidobacterium lactis Bi-07 versus placebo for the symptoms of bloating in patients with functional bowel disorders: a double-blind study. J Clin Gastroenterol. 2011;45:518-525. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 145] [Cited by in RCA: 130] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 17. | Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480-1491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3413] [Cited by in RCA: 3381] [Article Influence: 177.9] [Reference Citation Analysis (1)] |
| 18. | Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther. 1997;11:395-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 973] [Cited by in RCA: 1221] [Article Influence: 43.6] [Reference Citation Analysis (1)] |
| 19. | Simrén M, Ohman L, Olsson J, Svensson U, Ohlson K, Posserud I, Strid H. Clinical trial: the effects of a fermented milk containing three probiotic bacteria in patients with irritable bowel syndrome - a randomized, double-blind, controlled study. Aliment Pharmacol Ther. 2010;31:218-227. [PubMed] [DOI] [Full Text] |
| 20. | Williams EA, Stimpson J, Wang D, Plummer S, Garaiova I, Barker ME, Corfe BM. Clinical trial: a multistrain probiotic preparation significantly reduces symptoms of irritable bowel syndrome in a double-blind placebo-controlled study. Aliment Pharmacol Ther. 2009;29:97-103. [PubMed] [DOI] [Full Text] |
| 21. | Patrick DL, Drossman DA, Frederick IO, DiCesare J, Puder KL. Quality of life in persons with irritable bowel syndrome: development and validation of a new measure. Dig Dis Sci. 1998;43:400-411. [PubMed] |
| 22. | Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28548] [Cited by in RCA: 31781] [Article Influence: 756.7] [Reference Citation Analysis (0)] |
| 23. | Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997;32:920-924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1858] [Cited by in RCA: 2100] [Article Influence: 75.0] [Reference Citation Analysis (1)] |
| 24. | Passos MC, Lembo AJ, Conboy LA, Kaptchuk TJ, Kelly JM, Quilty MT, Kerr CE, Jacobson EE, Hu R, Friedlander E. Adequate relief in a treatment trial with IBS patients: a prospective assessment. Am J Gastroenterol. 2009;104:912-919. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 25. | Urbaniak G, Plous S. Research Randomizer. 4.0 ed, 2012: Computer software. Available from: https://www.randomizer.org/. |
| 26. | Altermann E, Russell WM, Azcarate-Peril MA, Barrangou R, Buck BL, McAuliffe O, Souther N, Dobson A, Duong T, Callanan M. Complete genome sequence of the probiotic lactic acid bacterium Lactobacillus acidophilus NCFM. Proc Natl Acad Sci USA. 2005;102:3906-3912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 454] [Cited by in RCA: 424] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 27. | D'Souza B, Slack T, Wong SW, Lam F, Muhlmann M, Koestenbauer J, Dark J, Newstead G. Randomized controlled trial of probiotics after colonoscopy. ANZ J Surg. 2015; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 28. | Childs CE, Röytiö H, Alhoniemi E, Fekete AA, Forssten SD, Hudjec N, Lim YN, Steger CJ, Yaqoob P, Tuohy KM. Xylo-oligosaccharides alone or in synbiotic combination with Bifidobacterium animalis subsp. lactis induce bifidogenesis and modulate markers of immune function in healthy adults: a double-blind, placebo-controlled, randomised, factorial cross-over study. Br J Nutr. 2014;111:1945-1956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 113] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 29. | Jeffery IB, O’Toole PW, Öhman L, Claesson MJ, Deane J, Quigley EM, Simrén M. An irritable bowel syndrome subtype defined by species-specific alterations in faecal microbiota. Gut. 2012;61:997-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 577] [Cited by in RCA: 635] [Article Influence: 48.8] [Reference Citation Analysis (0)] |
| 30. | Engsbro AL, Simren M, Bytzer P. Short-term stability of subtypes in the irritable bowel syndrome: prospective evaluation using the Rome III classification. Aliment Pharmacol Ther. 2012;35:350-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 31. | Sisson G, Ayis S, Sherwood RA, Bjarnason I. Randomised clinical trial: A liquid multi-strain probiotic vs. placebo in the irritable bowel syndrome--a 12 week double-blind study. Aliment Pharmacol Ther. 2014;40:51-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 107] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 32. | Lackner JM, Jaccard J, Keefer L, Firth R, Carosella AM, Sitrin M, Brenner D. The accuracy of patient-reported measures for GI symptoms: a comparison of real time and retrospective reports. Neurogastroenterol Motil. 2014;26:1802-1811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 33. | Azpiroz F, Guyonnet D, Donazzolo Y, Gendre D, Tanguy J, Guarner F. Digestive Symptoms in Healthy People and Subjects With Irritable Bowel Syndrome: Validation of Symptom Frequency Questionnaire. J Clin Gastroenterol. 2015;49:e64-e70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |