Published online Dec 21, 2016. doi: 10.3748/wjg.v22.i47.10461
Peer-review started: June 22, 2016
First decision: August 22, 2016
Revised: September 5, 2016
Accepted: September 28, 2016
Article in press: September 28, 2016
Published online: December 21, 2016
Processing time: 181 Days and 21.5 Hours
Focal nodular hyperplasia (FNH) of the liver is a benign lesion occurring in 0.6%-3% of the general population that probably reflects a local hyperplastic response of hepatocytes to a vascular abnormality. Most lesions are diagnosed incidentally and the natural history of the disease remains largely unknown. It has been shown that most FNH remain stable, or even regress, over a long follow-up period. We present a patient with FNH of the liver who was followed up for 7 years. A 26-year-old woman with a 5-year history of oral contraceptive use was referred to our hospital in February 2005 for further examination of a liver tumour. The diagnosis of FNH was made using magnetic resonance (MR) imaging with hepatospecific contrast media; this technique allows a correct diagnosis, in particular distinguishing FNH from hepatic adenoma, avoiding an invasive procedure such as the lesion biopsy. After 7-year from the diagnosis, we observed the complete spontaneous regression of the lesion by enhanced MR scanning. In this patient, discontinuation of oral contraceptive use and two childbirths may have influenced the natural history of FNH. To our knowledge, in the English literature there is no report illustrating a complete regression of giant FNH but only studies of decreasing in size. The present case suggests that a young patient with giant FNH should be managed conservatively rather than by resection, because FNH has the potential for spontaneous regression.
Core tip: We present a patient with focal nodular hyperplasia (FNH) of the liver who was followed up for 7 years. A 26-year-old woman with a 5-year history of oral contraceptive use was referred to our hospital in February 2005 for further examination of a liver tumour. The diagnosis of FNH was made using magnetic resonance (MR) imaging with hepatospecific contrast media. After 7-year from the diagnosis, we observed the complete spontaneous regression of the lesion by enhanced MR scanning. In this patient, discontinuation of oral contraceptive use and two childbirths may have influenced the natural history of FNH.
- Citation: Mamone G, Caruso S, Cortis K, Miraglia R. Complete spontaneous regression of giant focal nodular hyperplasia of the liver: Magnetic resonance imaging evaluation with hepatobiliary contrast media. World J Gastroenterol 2016; 22(47): 10461-10464
- URL: https://www.wjgnet.com/1007-9327/full/v22/i47/10461.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i47.10461
Focal nodular hyperplasia (FNH) is a benign hepatic lesion common in young women; a localized increase in arterial blood flow produced by a vascular abnormality may be involved in the pathogenesis of FNH[1].
The natural history of FNH is still unknown, because long-term follow-up studies of histologically proven FNH have been performed only in small series of patients, with conflicting results[2-6].
Surgery or interventional radiology treatment are not recommended, except in few cases when the tumour compresses neighbouring organs, liver vessels or bile ducts[7].
We report a patient with giant FNH of the liver, in whom the complete spontaneous regression of the lesion was observed on enhanced magnetic resonance with hepatobiliary phase, after a 7-year period of observation.
A 26-year-old woman was referred to our centre in February 2005 with an incidentally detected liver lesion on an abdominal ultrasound done as part of the imaging work-up for mild abdominal pain. No relevant past medical or surgical history was elicited. The patient was on the oral contraceptive pill for the past five years. Physical examination and a routine biochemical liver screen were unremarkable.
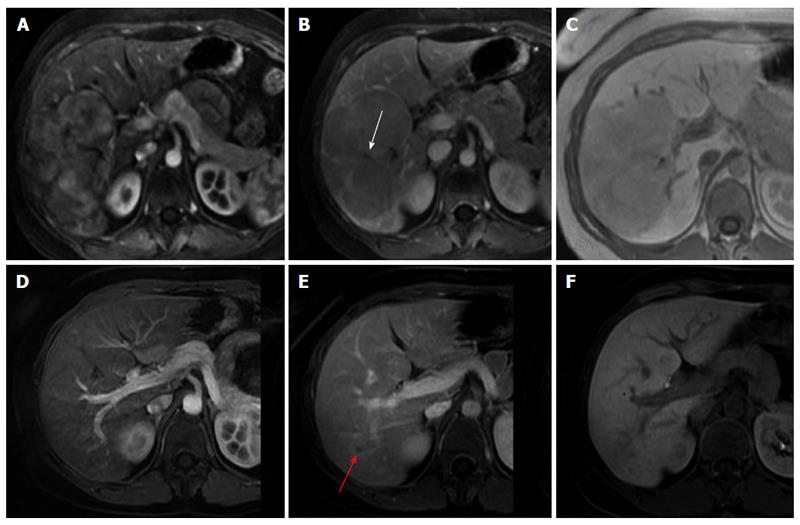
Further imaging was performed by magnetic resonance imaging (MRI), using a hepatospecific contrast agent (Gd-BOPTA, MultiHance, Bracco Imaging, Milan, Italy). This showed a 11.5 cm T1 and T2 isointense mass lesion in the right liver lobe, with small central scar, mosaic arterial enhancement, iso to hypoenhancement to liver on the delayed venous phases, and uptake of Gd-BOPTA on the hepatobiliary phase at two hours post contrast administration (Figure 1A-C). These findings were considered pathognomonic for FNH, and a biopsy was therefore deemed unnecessary[8-10].
The patient discontinued the oral contraceptive pill soon after diagnosis. She had two successful gestations (in 2006 and 2010). A follow-up Gd-BOPTA enhanced MRI performed in January 2012 showed complete involution of the known FNH (Figure 1D-F), except for a subcentimetre hypointense area that was attributed to residual scarring. At present, the patient remains asymptomatic and is doing well.
FNH of the liver is a benign condition occurring in 0.6%-3% of the general population. Most lesions are diagnosed incidentally and the natural history of the disease remains largely unknown. It has been postulated that a localized increase in arterial blood flow produced by a pre-existing vascular abnormality may be involved in the pathogenesis of FNH, through an exaggerated hyperplastic response[1]. FNH is the second commonest benign lesion of the liver following hemangioma[11] and FNH nodules are well-circumscribed unencapsulated nodules composed of hyperplastic hepatocytes surrounded by fibrous bands radiating from a central fibrotic scar containing thick-walled arteries[1,11].
The natural history of FNH is still unknown, because long-term follow-up studies of histologically proven FNH have been performed only in small cohort of patients, with conflicting results[2-6]. Surgical or interventional radiological treatment is usually not advocated, except in the rare exceptional cases where large FNH compress neighbouring organs, liver vessels or bile ducts[7].
The non-invasive diagnosis of FNH was quite challenging prior to the introduction of MRI performed using hepatospecific contrast agents. The typical MR imaging features of FNH include the presence of a central scar, arterial enhancement, and sustained enhancement in the venous phases. FNH usually shows iso to slightly hypointensity on T1 and iso to slightly hyperintensity on T2 weighted images. FNH nodules appear as bright, or brighter, than normal liver parenchyma on the hepatobiliary phase of MRI performed with such agents[8-10], avoiding the need for imaging-guided biopsy.
The pathogenesis and natural history of FNH remain largely unknown[1-6]. A possible aetiological link to endogenous oestrogens has been considered given the female predominance and peak incidence during childbearing years[1]. Exogenous oestrogens might also promote growth and marked vascular changes in FNH, and are usually discontinued in patients with FNH[12-14]. Regression has been reported following withdrawal of the oral contraceptive pill[13-15]. To our knowledge, in the English literature there is no report illustrating a complete regression of giant FNH but only studies of decreasing in size. The available data is limited and conflicting, with some studies reporting that neither the size nor the number of FNH lesions were influenced by oral contraceptive use[3,4] and that pregnancy was also not associated with FNH changes or complications[16].
Therefore, the relationship between low-dose oestrogen, pregnancy and FNH remains controversial. In our patient, discontinuation of oral contraceptive use and two childbirths may have influenced the natural history of FNH. The present case suggests that asymptomatic FNH could be managed conservatively with discontinuation of the oral contraceptive pill, since this might promote spontaneous regression.
The authors report a patient with giant focal nodular hyperplasia (FNH) of the liver, in whom the complete spontaneous regression of the lesion was observed on enhanced magnetic resonance with hepatobiliary phase, after a 7-year period of observation.
The patient remained asymptomatic and was doing well.
No differential diagnosis.
All labs were within normal limits.
A follow-up Gd-BOPTA enhanced magnetic resonance imaging (MRI) showed complete involution of the known FNH, except for a subcentimetre hypointense area that was attributed to residual scarring.
No pathological diagnosis.
Discontinuation of the oral contraceptive pill.
Regression of FNH has been reported following withdrawal of the oral contraceptive pill. To our knowledge, in the English literature there is no report illustrating a complete regression of giant FNH but only studies of decreasing in size. In our patient, discontinuation of oral contraceptive use and two childbirths may have influenced the natural history of FNH.
FNH of the liver is a benign lesion occurring in 0.6%-3% of the general population that probably reflects a local hyperplastic response of hepatocytes to a vascular abnormality.
The present case suggests that asymptomatic FNH could be managed conservatively with discontinuation of the oral contraceptive pill, since this might promote spontaneous regression.
This manuscript is well-written and easy for readers to follow. It highlights the possibility that discontinuation of oral contraceptive pill and two childbirths may influence the lesion’s regression. The hepatospecific contrast media used in MRI to clearly diagnose FNH is Gd-BOPTA. Overall, this paper can help improve readers’ clinical practice.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Liu GJ S- Editor: Yu J L- Editor: A E- Editor: Zhang FF
| 1. | Wanless IR, Mawdsley C, Adams R. On the pathogenesis of focal nodular hyperplasia of the liver. Hepatology. 1985;5:1194-1200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 475] [Cited by in RCA: 365] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 2. | Stocker JT, Ishak KG. Focal nodular hyperplasia of the liver: a study of 21 pediatric cases. Cancer. 1981;48:336-345. [PubMed] |
| 3. | Di Stasi M, Caturelli E, De Sio I, Salmi A, Buscarini E, Buscarini L. Natural history of focal nodular hyperplasia of the liver: an ultrasound study. J Clin Ultrasound. 1996;24:345-350. [PubMed] |
| 4. | Mathieu D, Kobeiter H, Maison P, Rahmouni A, Cherqui D, Zafrani ES, Dhumeaux D. Oral contraceptive use and focal nodular hyperplasia of the liver. Gastroenterology. 2000;118:560-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 120] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Leconte I, Van Beers BE, Lacrosse M, Sempoux C, Jamart J, Materne R, Baudrez V, Horsmans Y. Focal nodular hyperplasia: natural course observed with CT and MRI. J Comput Assist Tomogr. 2000;24:61-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 36] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Kuo YH, Wang JH, Lu SN, Hung CH, Wei YC, Hu TH, Chen CH, Yen YH, Lee CM, Eng HL. Natural course of hepatic focal nodular hyperplasia: a long-term follow-up study with sonography. J Clin Ultrasound. 2009;37:132-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Amesur N, Hammond JS, Zajko AB, Geller DA, Gamblin TC. Management of unresectable symptomatic focal nodular hyperplasia with arterial embolization. J Vasc Interv Radiol. 2009;20:543-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Grazioli L, Morana G, Kirchin MA, Schneider G. Accurate differentiation of focal nodular hyperplasia from hepatic adenoma at gadobenate dimeglumine-enhanced MR imaging: prospective study. Radiology. 2005;236:166-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 287] [Cited by in RCA: 243] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 9. | Grazioli L, Morana G, Federle MP, Brancatelli G, Testoni M, Kirchin MA, Menni K, Olivetti L, Nicoli N, Procacci C. Focal nodular hyperplasia: morphologic and functional information from MR imaging with gadobenate dimeglumine. Radiology. 2001;221:731-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 108] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Pirovano G, Vanzulli A, Marti-Bonmati L, Grazioli L, Manfredi R, Greco A, Holzknecht N, Daldrup-Link HE, Rummeny E, Hamm B. Evaluation of the accuracy of gadobenate dimeglumine-enhanced MR imaging in the detection and characterization of focal liver lesions. AJR Am J Roentgenol. 2000;175:1111-1120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 66] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Nguyen BN, Fléjou JF, Terris B, Belghiti J, Degott C. Focal nodular hyperplasia of the liver: a comprehensive pathologic study of 305 lesions and recognition of new histologic forms. Am J Surg Pathol. 1999;23:1441-1454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 271] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 12. | Pain JA, Gimson AE, Williams R, Howard ER. Focal nodular hyperplasia of the liver: results of treatment and options in management. Gut. 1991;32:524-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 81] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Aldinger K, Ben-Menachem Y, Whalen G. Focal nodular hyperplasia of the liver associated with high-dosage estrogens. Arch Intern Med. 1977;137:357-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Scott LD, Katz AR, Duke JH, Cowan DF, Maklad NF. Oral contraceptives, pregnancy, and focal nodular hyperplasia of the liver. JAMA. 1984;251:1461-1463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 36] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Ross D, Pina J, Mirza M, Galvan A, Ponce L. Letter: Regression of focal nodular hyperplasia after discontinuation of oral contraceptives. Ann Intern Med. 1976;85:203-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Weimann A, Mössinger M, Fronhoff K, Nadalin S, Raab R. Pregnancy in women with observed focal nodular hyperplasia of the liver. Lancet. 1998;351:1251-1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |