Published online Dec 7, 2016. doi: 10.3748/wjg.v22.i45.10015
Peer-review started: August 24, 2016
First decision: October 20, 2016
Revised: November 1, 2016
Accepted: November 14, 2016
Article in press: November 16, 2016
Published online: December 7, 2016
Processing time: 106 Days and 1.8 Hours
To evaluate the efficacy of doubling time (DT) of gastrointestinal submucosal tumors (GIST).
From April 1987 through November 2012, a total of 323 patients were given a final histopathological diagnosis of GISTs on surgical resection or endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) in Kitasato University East Hospital or Kitasato University Hospital. We studied 53 of these patients (34 with resected tumors and 19 with unresected tumors) whose tumors could be measured on EUS on at least two successive occasions. The histopathological diagnosis was GIST in 34 patients, leiomyoma in 5, schwannoma in 3, ectopic pancreas in 1, hamartoma in 1, cyst in 1, Brunner’s adenoma in 1, and spindle-cell tumor in 7. We retrospectively calculated the DT of GISTs on the basis of the time course of EUS findings to estimate the growth rate of such tumors.
The DT was 17.2 mo for GIST, as compared with 231.2 mo for leiomyoma, 104.7 mo for schwannoma, 274.9 mo for ectopic pancreas, 61.2 mo for hamartoma, 49.0 mo for cyst, and 134.7 mo for Brunner’s adenoma. The GISTs were divided into risk classes on the basis of tumor diameters and mitotic figures (Fletcher’s classification). The classification was extremely low risk or low risk in 28 patients, intermediate risk in 3, and high risk in 3. DT of GIST according to risk was 24.0 mo for extremely low-risk plus low-risk GIST, 17.1 mo for intermediate-risk GIST, and 3.9 mo for high-risk GIST. DT of GIST was significantly shorter than that of leiomyoma plus schwannoma (P < 0.05), and DT of high-risk GIST was significantly shorter than that of extremely low-risk plus low-risk GIST (P < 0.05).
For GIST, a higher risk grade was associated with a significantly shorter DT. Small SMTs should initially be followed up within 6 mo after detection.
Core tip: The doubling time (DT) differed according to the type of submucosal tumors (SMTs), and gastrointestinal submucosal tumors (GISTs) were confirmed to have a significantly shorter doubling time than the other types of tumors. DT was 17.2 mo for GIST, as compared with 231.2 for leiomyoma, 104.7 for schwannoma. DT of GIST was significantly shorter than that of leiomyoma plus schwannoma (P < 0.05), and DT of high-risk GIST (3.9 mo) was significantly shorter than that of extremely low-risk plus low-risk GIST (24.0 mo) (P < 0.05). Even small SMTs less than 2 cm in diameter should initially be followed up within at least 6 mo after detection.
- Citation: Koizumi S, Kida M, Yamauchi H, Okuwaki K, Iwai T, Miyazawa S, Takezawa M, Imaizumi H, Koizumi W. Clinical implications of doubling time of gastrointestinal submucosal tumors. World J Gastroenterol 2016; 22(45): 10015-10023
- URL: https://www.wjgnet.com/1007-9327/full/v22/i45/10015.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i45.10015
In Japan, gastrointestinal submucosal tumors (SMTs) are often detected on radiographic and conventional endoscopic examinations during health checkups. SMTs are covered by mucosa, and the majority of lesions are nonepithelial tumors arising from the submucosa or muscularis propria. The presence of SMTs can be detected on radiography and conventional endoscopy, but qualitative diagnosis remains difficult on these imaging techniques. However, progress in endoscopic ultrasonography (EUS) and other diagnostic techniques has facilitated the qualitative evaluation of SMTs[1,2]. In the differential diagnosis of gastrointestinal stromal tumors (GISTs), considered clinically important lesions, endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) plays a major role in deciding the treatment policy and is now widely used clinically[3,4]. However, there remains room for improvement in the diagnostic performance of EUS-FNA for small lesions. Consequently, small SMTs yet to be definitively diagnosed are generally followed up once or twice per year[5]. To our knowledge, very few studies have evaluated the doubling time of SMTs, an index of the rate of tumor growth, according to diagnosis. We estimated the doubling time of different types of SMTs and report our findings.
From April 1987 through November 2012, a total of 323 patients were given a final histopathological diagnosis of gastrointestinal SMT on surgical resection or EUS-FNA in our hospital. We studied 53 of these patients (34 with resected tumors and 19 with unresected tumors) whose tumors could be measured on EUS on at least two successive occasions. Tumor-doubling time was estimated retrospectively. All examinations were carried out by endoscopists adequately experienced in EUS. Informed consent was obtained from each patient prior to the procedure. Regardless of the result, the good clinical practice was provided with consent of the patient. The longest and shortest tumor diameters were measured within the depicted range. The follow-up period was defined as the time between initial EUS and final EUS.
Radial scanning echoendoscopes (GF-UM20, GF-UM240, GF-UM2000, UM-DP20, and UM-DP12; Olympus Co., Tokyo, Japan) were used to perform EUS. EUS-FNA was performed with the use of convex array echoendoscopes (GF-UCT260, GF-UCT240, XGF-UCT160, GF-UC2000P; Olympus Co., Ltd.). The following puncture needles were used: 19-gauge needles (Wilson-Cook, Winston Salem, NC, United States), 22-gauge needles (NA-200H, Olympus Co., Ltd.), and 25-gauge needles (Echochip, Wilson-Cook). The aspiration pressure was 10 to 20 cc, and “in-and-out motion” was continued for 20 strokes (occasionally, 10 strokes). Puncture was performed 2 to 6 time (median, 3 times).
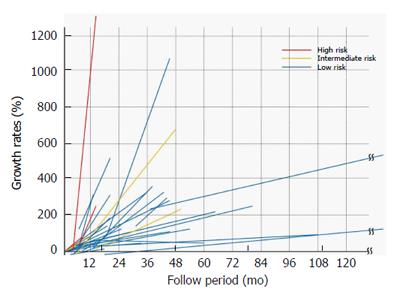
Three-dimensional EUS is more accurate than 2-dimensional EUS for the measurement of tumor volume. However, commercially available three-dimensional echoendoscopes are probe type, making it difficult to measure large lesions. In the present study, we therefore measured the longest and shortest diameters within the range depicted on two-dimensional EUS. Few SMTs show a completely spherical growth pattern, and many grow in an oval fashion. In this study, however, we assumed that the tumors were spherical and used the mean value of the longest and shortest diameters as the tumor diameter to calculate tumor volume. The following equation was used to calculate doubling time: tumor growth rate (%) = (V1-V0)/ V0 × 100, in which V0 is the tumor volume (mm3) at baseline EUS (πd03/6), V1 is the tumor volume (mm3) at the second or subsequent sessions of EUS (πd13/6), d0 is the tumor diameter (mm) at baseline EUS, and d1 is the tumor diameter (mm) at the second or subsequent sessions of EUS.
The time courses of tumor growth rates were plotted on scattergrams with trend lines. The point at which the tumor growth rate became 100% was defined as the doubling time.
On immunostaining of specimens obtained by surgical resection or FNA, tumors that stained positive for CD34 or KIT were diagnosed as GIST. Leiomyomas were diagnosed if immunostaining was positive for smooth-muscle antibodies (SMA) and negative for CD34 and KIT. Schwannomas were diagnosed if the tumor stained positive for S-100 and negative for CD34 and KIT. Spindle-cell tumors were diagnosed if spindle-shaped cells were confirmed on hematoxylin-eosin staining, but immunostaining was precluded by an inadequate sample size on FNA. GISTs were classified as extremely low risk, low risk, intermediate risk, and high risk on the basis of actual tumor diameters and mitotic figures in patients with resected tumors. In patients with unresected tumors, risk class was based on tumor diameter measured on EUS and mitotic figures.
For statistical analysis, the Mann-Whitney U test was used to compare doubling times. P values of less than 0.05 were considered to indicate statistical significance. SPSS statistical software, version 17.0 was used for statistical analysis.
The study group comprised 26 men and 27 women, with a median age of 63.0 years (range, 31 to 83). The tumor was located in the esophagus in 4 patients, the stomach in 47, and the duodenum in 2 (Table 1). The histopathological diagnosis was GIST in 34 patients, leiomyoma in 5, schwannoma in 3, ectopic pancreas in 1, hamartoma in 1, cyst in 1, Brunner’s adenoma in 1, and spindle-cell tumor in 7 (Table 2). The median follow-up in the study group as a whole was 31.7 mo (range, 6.6 to 210). The median number of EUS procedures performed during follow-up was 3 (range, 2 to 13). The median tumor diameter (mean of the longest and shortest diameters) was 19.1 mm (range, 10 to 44.8 mm) on initial EUS and 25.3 mm (range, 13 to 52.1 mm) on EUS before tumor resection or EUS-FNA for final diagnosis (Table 3).
| Characteristic | Value |
| Sex, No. | male/female: 26/27 |
| Age, median (range), yr | 63.0 (31-83) |
| Tumor location, No. | Esophagus/stomach/duodenum: 4/47/2 |
| Esophagus (n = 4) | Stomach (n = 47) | Duodenum (n = 2) | Total(n = 53) | |
| GIMT | 4 | 45 | 0 | 49 |
| GIST | 0 | 34 | 0 | 34 |
| Leiomyoma | 2 | 3 | 0 | 5 |
| Schwannoma | 1 | 2 | 0 | 3 |
| Spindle-cell tumor | 1 | 6 | 0 | 7 |
| Ectopic pancreas | 0 | 1 | 0 | 1 |
| Hamartoma | 0 | 0 | 1 | 1 |
| Intramural developmental cyst | 0 | 1 | 0 | 1 |
| Brunner’s adenoma | 0 | 0 | 1 | 1 |
| Resected tumors(n = 34) | Unresected tumors (n = 19) | Total (n = 53) | GIST (n = 34) | |
| Follow-up period, median (range), mo | 24.9 (6.6-210) | 36.5 (11.2-183.6) | 31.7 (6.6-210) | 27.3 (6.6-210) |
| EUS sessions, median (range) | 3 (2-8) | 4 (2-13) | 3 (2-13) | 3 (2-11) |
| Tumor diameter at initial EUS, median (range), mm | 19.5 (10-30) | 19.0 (11.5-44.8) | 19.1 (10-44.8) | 19.0 (10.9-44.8) |
| Tumor diameter before surgery or FNA, median (range), mm | 28.0 (20-43.1) | 22.8 (15.2-52.1) | 25.3 (13.7-52.1) | 26.7 (13.7-52.1) |
| Time from the final EUS to surgery, median (range) | 3.8 mo (22d-16.3 mo) | - | - | - |
Tumor resection was performed in 29 of the 34 patients with GIST. Among the 5 patients with unresectable tumors, surgery was precluded by poor general condition due to other diseases (neurologic diseases) in 2 patients, follow-up observation was requested by 1 patient, and 2 patients dropped out of the study. Of the 5 patients with leiomyoma, 1 underwent resection, and 4 were followed up. Of the 3 patients with schwannoma, 2 underwent resection, and 1 was followed up. The patient with ectopic pancreas and the patient with Brunner’s adenoma were followed up. Among the 7 patients with spindle-cell tumors, 5 were followed up, and 2 dropped out of the study.
In the patents with resected tumors and those with unresected tumors, the median follow-up was 24.9 mo and 36.5 mo, the median number of EUS sessions during follow-up was 3 and 4, the median tumor diameter at initial EUS was 19.5 and 19.0 mm, and the median tumor diameter on EUS before surgery or EUS-FNA was 28.0 and 22.8 mm, respectively. In patients with resected tumors, the median interval from final EUS to surgery was 3.8 mo (range, 22 d to 16.3 mo). The median longest tumor diameter of the resected specimens was 35 mm (range, 20 to 60 mm) (Table 3). None of the patients who underwent follow-up observation or who were observed after surgery died or had recurrence (excluding dropouts).
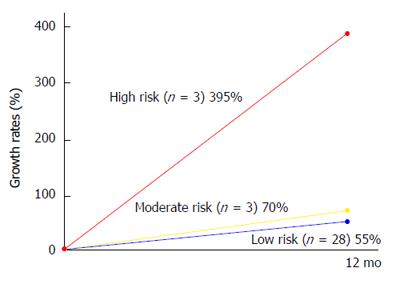
In the 34 patients with GIST, the median follow-up was 27.3 mo (range, 6.6 to 210), and the median tumor diameter at initial EUS was 19.0 mm (range, 10.9 to 44.8). The GISTs were divided into risk classes on the basis of tumor diameters and mitotic figures (Fletcher’s classification). The classification was extremely low risk or low risk in 28 patients, intermediate risk in 3, and high risk in 3. The median follow-up period was 31.0 mo in patients with extremely low-risk and low-risk GISTs, 47.3 mo in those with intermediate-risk GISTs, and 12.4 mo in those with high-risk GISTs. The doubling time according to risk was 24.0 mo for extremely low-risk plus low-risk GISTs, 17.1 mo for intermediate-risk GISTs, and 3.9 mo for high-risk GISTs (Table 4).
| Extremely low plus low risk (n = 28) | Intermediate risk(n = 3) | High risk (n = 3) | Total (n = 34) | |
| Follow-up period, median (range), mo | 31.0 (6.6-210) | 47.3 (11.2-49.9) | 12.4 (7.4-16.7) | 27.3 (6.6-210) |
| Initial tumor diameter, median (range), mm | 18.6 (10.9-30.0) | 28.5 (20.0-44.8) | 25.5 (14.0-27.3) | 19.0 (10.9-44.8) |
| Doubling time, median (range), mo | 24.0 (2.0-183.6) | 17.1 (6.1-19.4) | 3.9 (0.8-10.4) | 17.2 (0.8-183.6) |
The median doubling time for GISTs as a whole was 17.2 mo. In contrast, the doubling time was 231.2 mo for leiomyoma, 104.7 mo for schwannoma, 274.9 mo for ectopic pancreas, 61.2 mo for hamartoma, 49.0 mo for intramural developmental cyst, and 134.7 mo for Brunner’s adenoma (Table 5). The doubling time of GISTs was significantly shorter than the doubling times of leiomyoma plus schwannoma (P = 0.005). When the doubling times of GISTs were compared according to risk class, the doubling time of high-risk GISTs was significantly shorter than that of extremely low-risk plus low-risk GISTs (P = 0.033). Moreover, the doubling time of high-risk plus intermediate-risk GISTs was significantly shorter than that of extremely low-risk plus low-risk GISTs (P = 0.047). Doubling times did not differ significantly between high-risk and intermediate-risk GISTs or between extremely low-risk plus low-risk GISTs and intermediate-risk GISTs (Table 6). The growth rates of individual GISTs during follow-up and annual growth rates of GISTs according to risk class are shown in Figures 1 and 2, respectively.
| No. of patient | Follow-up period, median (range), mo | Doubling time, median (range), mo | |
| Leiomyoma | 5 | 47.1 (10.7-137.2) | 231.2 (21.3-1303.8) |
| Schwannoma | 3 | 50.1 (24.3-71.7) | 104.7 (3.9-305.4) |
| Ectopic pancreas | 1 | 66.5 | 274.9 |
| Hamartoma | 1 | 99.6 | 61.2 |
| Intramural developmental cyst | 1 | 29.5 | 49.0 |
| Brunner’s adenoma | 1 | 30.6 | 134.7 |
| Doubling time (mo), median | P value | |
| GIST vs Leiomyoma + schwannoma | 17.2 vs 204.2 | 0.005 |
| High risk vs Intermediate risk | 3.9 vs 17.1 | 0.127 |
| Intermediate risk vs Extremely low + low risk | 17.1 vs 24.0 | 0.423 |
| High risk vs Extremely low + low risk | 3.9 vs 24.0 | 0.033 |
| High + intermediate risk vs Extremely low + low risk | 8.2 vs 24.0 | 0.047 |
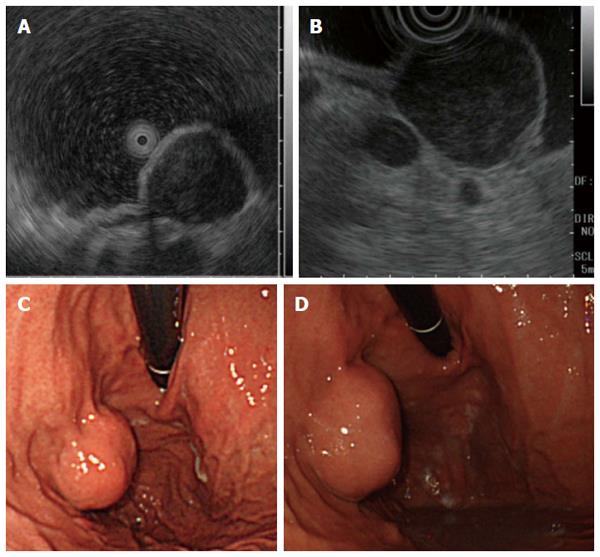
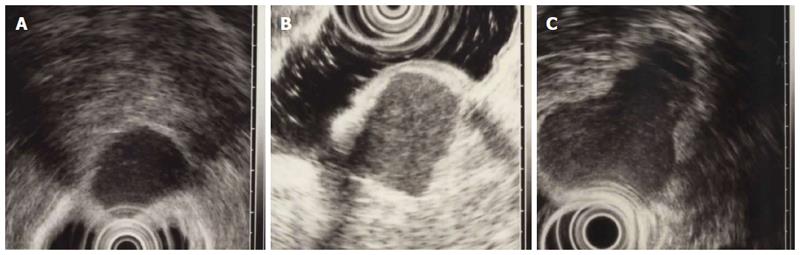
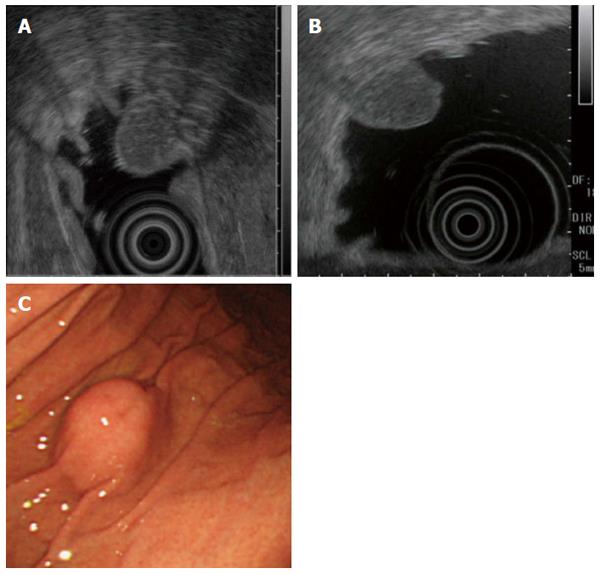
We show some endoscopic and EUS findings of low grade GIST (Figure 3A-D), high grade GIST (Figure 4A-C) and ectopic pancreas (Figure 5A-C).
Many gastrointestinal SMTs are asymptomatic and incidentally detected on radiographic examinations during health checkups or endoscopic or computed tomographic examinations performed to evaluate other diseases. Few studies have estimated the incidence of gastrointestinal SMTs, but most arise in the stomach, and the detection rate on endoscopy was reported to be 0.36%[3,6]. Tumorous lesions presenting with the characteristics of SMTs include mesenchymal tumors, lipomas, carcinoids, granular-cell tumors, glomus tumors, and metastatic deposits. Nontumorous lesions include cysts, ectopic pancreas, Brunner’s adenomas, and hamartomas[1]. Conventional endoscopy only provides information useful for the local diagnosis of SMTs, whereas EUS can depict the local structure and internal characteristics of the gastrointestinal wall, thereby facilitating qualitative diagnosis[7]. Although it is relatively easy to distinguish gastrointestinal mesenchymal tumors from tumors such as lipoma and cysts on EUS, it is difficult to differentially diagnose GISTs from leiomyomas and schwannomas, because all three of these lesions are depicted as hypoehoic tumors involving the fourth layer on EUS. The 2001 NIH GIST Consensus Meeting and the 2004 ESMO Consensus GIST Meeting proposed that GISTs are potentially malignant and recommended that surgical resection should be considered for all GISTs[8-10].
Miettinen et al[11] proposed a risk classification for GISTs, based on tumor diameter, mitotic figures, and location. They reported that tumors 2 cm or less in diameter have no risk of postoperative metastasis. However, metastasis has been associated with even small GISTs[12]. It is therefore difficult to conclude that small tumors are benign. A histopathological diagnosis has an important role in formulating the treatment policy for SMTs. However, SMTs are covered by mucosa similar to that of the surrounding region, which often makes diagnosis challenging on conventional endoscopy with mucosal biopsy. EUS-FNA thus plays an important clinical role in the diagnosis of SMTs. In lesions measuring less than 2 cm, however, the rate of obtaining adequate specimens is generally low[13]. There is also the risk of tumor seeding caused by lesion rupture on puncture with an aspiration needle. Moreover, it is difficult to obtain adequate tissue specimens for immunostaining or other examination techniques if adequate needle strokes cannot be taken. In general, EUS-FNA is indicated for lesions at least 2 cm in diameter. On the other hand, for lesions less than 2 cm in diameter with no findings suggesting malignancy, such as ulcer formation, irregular margins, or rapid growth[14], follow-up observation once or twice per year has been recommended[5]. However, with the exception of lesions showing distinct evidence of increasing size or an intragastric growth pattern, EUS is recommended for the follow-up of GISTs, particularly lesions showing an extragastric growth pattern precluding an accurate estimation of tumor size. EUS can be used to assess even small lesions and is simpler than computed tomography for the evaluation of small lesions.
Confirmation of differences in growth rate among specific types of SMTs during follow-up is expected to facilitate decision-making regarding the treatment policy. Similar to other types of tumors, a higher malignant potential of SMTs is generally assumed to be associated with a more rapid growth rate[15]. To date, however, few studies have investigated the growth rates of different types of SMTs. A previous study estimated the doubling time of SMTs on computed tomography[16]. To our knowledge, however, our study is the first to report the doubling time of SMTs on EUS. Because SMTs are generally oval tumors, EUS, which produces cross-sectional images, can be used to estimate the doubling time of most SMTs. However, some SMTs show a lobular growth pattern, making it difficult to accurately calculate the doubling time. In our study, we assumed that SMTs show a global growth pattern when we calculated the doubling time. The use of non-probe-type conventional three-dimensional EUS may allow tumor volumes to be more accurately estimated, but this issue must be addressed in future studies.
Our study confirmed that the growth rates of SMTs during follow-up differ according to the specific type of tumor. In particular, GIST had a shorter doubling time (17.2 mo) and a higher malignant potential than did the other types of SMTs. The difference in the doubling time between GISTs and mesenchymal tumors other than GIST (leiomyoma and schwannoma) may facilitate the differential diagnosis of GISTs from leiomyomas and schwannomas, all of which arise in the fourth layer of the gastrointestinal wall. Among GISTs, a higher risk class tended to have shorter doubling times. Because our study group was small, further studies of larger numbers of patients are needed. In our study, the doubling times of intermediate-risk and high-risk GISTs were less than 6 mo. Initial follow-up examinations should be therefore performed within at least the first 6 mo after diagnosis, even for small SMTs less than 2 cm in diameter.
GISTs, leiomyomas, schwannomas, and other SMTs arising in the fourth layer that have a prolonged doubling time are considered to have low malignant potential. Small SMTs can therefore undergo follow-up observation. Some extremely low-risk and low-risk GISTs have a longer doubling time than that of benign tumors, and we have encountered benign tumors with a shorter doubling time than that of GISTs. It is therefore important to obtain a histopathological diagnosis during follow-up, even for slowly growing tumors. Although considerable progress has been made in techniques and devices for EUS-FNA, the diagnostic accuracy is not 100%[4,17]. Patients in whom a histopathological diagnosis cannot be made should therefore be closely followed up. In our study, the median tumor diameter in patients who underwent EUS-FNA was 22.8 mm, which was adequate for EUS-FNA. For SMTs 20 mm or more in diameter that cannot be diagnosed, EUS-FNA should be repeated, and close follow-up is recommended.
In our study, the risk class of GIST was diagnosed on the basis of mitotic figures in specimens obtained by EUS-FNA in patients who did not undergo surgery. Histopathologically, GISTs are heterogeneous masses, making it difficult to classify GISTs solely on the basis of specimens obtained by EUS-FNA[18]. In our hospital, we aggressively perform EUS-FNA for lesions more than 2 cm in diameter as well as for lesions with heterogeneous contents suggestive of malignancy, even if the lesion diameter is less than 2 cm. If GIST is diagnosed, resection should be promptly performed, even if the tumor is small and shows few mitotic figures. For lesions that cannot be diagnosed and small lesions, the other techniques[19-21] can be considered to obtain sufficient specimen.
Many SMTs are detected incidentally on upper gastrointestinal endoscopy, and many patients with small SMTs 1 to 2 cm in diameter are most likely followed up. The management of small lesions measuring less than 2 cm is often perplexing. Our study showed that the doubling time differed according to the type of SMT, and GISTs were confirmed to have a significantly shorter doubling time than the other types of tumors. In addition, a higher risk class of GIST was found to be associated with a significantly shorter doubling time. Our findings suggest that even small SMTs less than 2 cm in diameter should initially be followed up within at least 6 mo after detection. In a limited number of patients, surgery or EUS-FNA is indicated. High-risk GISTs that are large and symptomatic are usually surgically resected at the time of detection. Three of high-risk GISTs those were followed up are included in this study. This is valuable information because we’re not able to follow up the high-risk GISTs after getting histopathological diagnosis recently. Our results demonstrated that SMTs showing evidence of rapid growth on follow-up EUS are likely to be high risk. The median doubling time for GISTs as a whole was 17.2 mo, but further studies of larger groups of patients are needed to confirm our findings.
Many gastrointestinal submucosal tumors (SMTs) are asymptomatic and incidentally detected. Among SMTs, gastrointestinal stromal tumors (GISTs) are potentially malignant and should be resected surgically. Endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) plays an important clinical role in the diagnosis of SMTs. However, the management of small lesions is often difficult. Confirmation of differences in growth rate among specific types of SMTs is expected to facilitate decision-making regarding the treatment policy.
EUS-FNA plays a major role in deciding the treatment policy. However, there remains room for improvement in the diagnostic performance of EUS-FNA for small lesions. Consequently, small SMTs yet to be definitively diagnosed are generally followed up once or twice per year.
To our knowledge, very few studies have evaluated the doubling time of SMTs, an index of the rate of tumor growth, according to diagnosis. The authors estimated the doubling time of different types of SMTs.
The doubling time of GIST was confirmed to be significantly shorter than that of other types of tumors. For GIST, a higher risk grade was associated with a significantly shorter doubling time. These findings suggest that small SMTs should initially be followed up within at least 6 mo after detection.
EUS: An endoscopic procedure to obtain images of the chest and abdominal organs through the wall of the gastrointestinal tract. EUS-FNA: A technique to obtain specimens of chest and abdominal lesions by puncturing the gastrointestinal tract under real-time EUS guidance.
This is a very meaningful research regarding the growth rate of the SMTs, which may be a very important character for the evaluation. Authors of this paper describe their strategy regarding observational duration for tumor in small size around 2 cm by analyzing the doubling times of each SMT. Initial follow-up examinations remain unclear in major guidelines. Therefore, this result provides an important information in the management of small SMT.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Kobara H, Sun SY S- Editor: Gong ZM L- Editor: A E- Editor: Wang CH
| 1. | Wiech T, Walch A, Werner M. Histopathological classification of nonneoplastic and neoplastic gastrointestinal submucosal lesions. Endoscopy. 2005;37:630-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 88] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 2. | Akahoshi K, Sumida Y, Matsui N, Oya M, Akinaga R, Kubokawa M, Motomura Y, Honda K, Watanabe M, Nagaie T. Preoperative diagnosis of gastrointestinal stromal tumor by endoscopic ultrasound-guided fine needle aspiration. World J Gastroenterol. 2007;13:2077-2082. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 159] [Cited by in RCA: 184] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 3. | Polkowski M. Endoscopic ultrasound and endoscopic ultrasound-guided fine-needle biopsy for the diagnosis of malignant submucosal tumors. Endoscopy. 2005;37:635-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 135] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 4. | Watson RR, Binmoeller KF, Hamerski CM, Shergill AK, Shaw RE, Jaffee IM, Stewart L, Shah JN. Yield and performance characteristics of endoscopic ultrasound-guided fine needle aspiration for diagnosing upper GI tract stromal tumors. Dig Dis Sci. 2011;56:1757-1762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 73] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 5. | Nishida T, Hirota S, Yanagisawa A, Sugino Y, Minami M, Yamamura Y, Otani Y, Shimada Y, Takahashi F, Kubota T; GIST Guideline Subcommittee. Clinical practice guidelines for gastrointestinal stromal tumor (GIST) in Japan: English version. Int J Clin Oncol. 2008;13:416-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 320] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 6. | Hedenbro JL, Ekelund M, Wetterberg P. Endoscopic diagnosis of submucosal gastric lesions. The results after routine endoscopy. Surg Endosc. 1991;5:20-23. [PubMed] |
| 7. | Akahoshi K, Oya M. Gastrointestinal stromal tumor of the stomach: How to manage? World J Gastrointest Endosc. 2010;2:271-277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 29] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, Miettinen M, O’Leary TJ, Remotti H, Rubin BP. Diagnosis of gastrointestinal stromal tumors: A consensus approach. Hum Pathol. 2002;33:459-465. [PubMed] |
| 9. | Blay JY, Bonvalot S, Casali P, Choi H, Debiec-Richter M, Dei Tos AP, Emile JF, Gronchi A, Hogendoorn PC, Joensuu H. Consensus meeting for the management of gastrointestinal stromal tumors. Report of the GIST Consensus Conference of 20-21 March 2004, under the auspices of ESMO. Ann Oncol. 2005;16:566-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 500] [Cited by in RCA: 486] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 10. | Casali PG, Jost L, Reichardt P, Schlemmer M, Blay JY; ESMO Guidelines Working Group. Gastrointestinal stromal tumours: ESMO clinical recommendations for diagnosis, treatment and follow-up. Ann Oncol. 2009;20 Suppl 4:64-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 119] [Article Influence: 7.9] [Reference Citation Analysis (1)] |
| 11. | Miettinen M, Lasota J. Gastrointestinal stromal tumors: pathology and prognosis at different sites. Semin Diagn Pathol. 2006;23:70-83. [PubMed] |
| 12. | Tanaka J, Oshima T, Hori K, Tomita T, Kim Y, Watari J, Oh K, Hirota S, Matsumoto T, Miwa H. Small gastrointestinal stromal tumor of the stomach showing rapid growth and early metastasis to the liver. Dig Endosc. 2010;22:354-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Mekky MA, Yamao K, Sawaki A, Mizuno N, Hara K, Nafeh MA, Osman AM, Koshikawa T, Yatabe Y, Bhatia V. Diagnostic utility of EUS-guided FNA in patients with gastric submucosal tumors. Gastrointest Endosc. 2010;71:913-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 177] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 14. | Yamada Y, Kida M, Sakaguchi T. A study on myogenic tumors of the upper gastrointestinal tract by endoscopic ultrasonography - with special reference to the differential diagnosis of benign and malignant lesions. Dig Endosc. 1992;4: 396-408. |
| 15. | Collins VP, Loeffler RK, Tivey H. Observations on growth rates of human tumors. Am J Roentgenol Radium Ther Nucl Med. 1956;76:988-1000. [PubMed] |
| 16. | Choi JW, Choi D, Kim KM, Sohn TS, Lee JH, Kim HJ, Lee SJ. Small submucosal tumors of the stomach: differentiation of gastric schwannoma from gastrointestinal stromal tumor with CT. Korean J Radiol. 2012;13:425-433. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 63] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 17. | Kida M, Araki M, Miyazawa S, Ikeda H, Takezawa M, Kikuchi H, Watanabe M, Imaizumi H, Koizumi W. Comparison of diagnostic accuracy of endoscopic ultrasound-guided fine-needle aspiration with 22- and 25-gauge needles in the same patients. J Interv Gastroenterol. 2011;1:102-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 18. | Okubo K, Yamao K, Nakamura T, Tajika M, Sawaki A, Hara K, Kawai H, Yamamura Y, Mochizuki Y, Koshikawa T. Endoscopic ultrasound-guided fine-needle aspiration biopsy for the diagnosis of gastrointestinal stromal tumors in the stomach. J Gastroenterol. 2004;39:747-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 74] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 19. | Binmoeller KF, Shah JN, Bhat YM, Kane SD. Suck-ligate-unroof-biopsy by using a detachable 20-mm loop for the diagnosis and therapy of small subepithelial tumors (with video). Gastrointest Endosc. 2014;79:750-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | de la Serna-Higuera C, Pérez-Miranda M, Díez-Redondo P, Gil-Simón P, Herranz T, Pérez-Martín E, Ochoa C, Caro-Patón A. EUS-guided single-incision needle-knife biopsy: description and results of a new method for tissue sampling of subepithelial GI tumors (with video). Gastrointest Endosc. 2011;74:672-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 21. | Kobara H, Mori H, Fujihara S, Nishiyama N, Kobayashi M, Kamata H, Masaki T. Bloc biopsy by using submucosal endoscopy with a mucosal flap method for gastric subepithelial tumor tissue sampling (with video). Gastrointest Endosc. 2013;77:141-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |