Published online Nov 7, 2016. doi: 10.3748/wjg.v22.i41.9196
Peer-review started: June 22, 2016
First decision: August 8, 2016
Revised: August 20, 2016
Accepted: September 14, 2016
Article in press: September 14, 2016
Published online: November 7, 2016
Processing time: 137 Days and 17.5 Hours
To simplify the diagnostic criteria for superficial esophageal squamous cell carcinoma (SESCC) on Narrow Band Imaging combined with magnifying endoscopy (NBI-ME).
This study was based on the post-hoc analysis of a randomized controlled trial. We performed NBI-ME for 147 patients with present or a history of squamous cell carcinoma in the head and neck, or esophagus between January 2009 and June 2011. Two expert endoscopists detected 89 lesions that were suspicious for SESCC lesions, which had been prospectively evaluated for the following 6 NBI-ME findings in real time: “intervascular background coloration”; “proliferation of intrapapillary capillary loops (IPCL)”; and “dilation”, “tortuosity”, “change in caliber”, and “various shapes (VS)” of IPCLs (i.e., Inoue’s tetrad criteria). The histologic examination of specimens was defined as the gold standard for diagnosis. A stepwise logistic regression analysis was used to identify candidates for the simplified criteria from among the 6 NBI-ME findings for diagnosing SESCCs. We evaluated diagnostic performance of the simplified criteria compared with that of Inoue’s criteria.
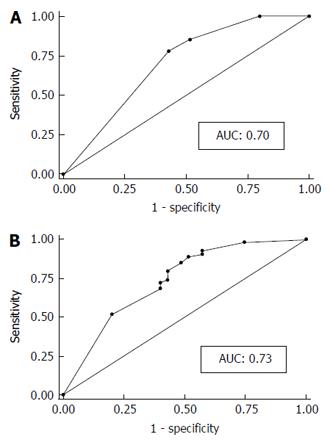
Fifty-four lesions (65%) were histologically diagnosed as SESCCs and the others as low-grade intraepithelial neoplasia or inflammation. In the univariate analysis, proliferation, tortuosity, change in caliber, and VS were significantly associated with SESCC (P < 0.01). The combination of VS and proliferation was statistically extracted from the 6 NBI-ME findings by using the stepwise logistic regression model. We defined the combination of VS and proliferation as simplified dyad criteria for SESCC. The areas under the curve of the simplified dyad criteria and Inoue’s tetrad criteria were 0.70 and 0.73, respectively. No significant difference was shown between them. The sensitivity, specificity, and accuracy of diagnosis for SESCC were 77.8%, 57.1%, 69.7% and 51.9%, 80.0%, 62.9% for the simplified dyad criteria and Inoue’s tetrad criteria, respectively.
The combination of proliferation and VS may serve as simplified criteria for the diagnosis of SESCC using NBI-ME.
Core tip: Narrow Band Imaging combined with magnifying endoscopy (NBI-ME) significantly improves the diagnostic accuracy for superficial esophageal squamous cell carcinoma (SESCC). However, currently used NBI-ME diagnostic criteria may confuse endoscopists and inhibit the widespread use of NBI-ME. The findings of this study suggest that simplified dyad criteria composed of the presence of “proliferation of intrapapillary capillary loops (IPCL)” and “various shapes (VS) of IPCLs” had comparable diagnostic performance to Inoue’s tetrad criteria, which are the most popular diagnostic criteria for SESCC. Proliferation and VS may serve as simplified NBI-ME criteria for diagnosing SESCC.
- Citation: Dobashi A, Goda K, Yoshimura N, Ohya TR, Kato M, Sumiyama K, Matsushima M, Hirooka S, Ikegami M, Tajiri H. Simplified criteria for diagnosing superficial esophageal squamous neoplasms using Narrow Band Imaging magnifying endoscopy. World J Gastroenterol 2016; 22(41): 9196-9204
- URL: https://www.wjgnet.com/1007-9327/full/v22/i41/9196.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i41.9196
Esophageal cancer is one of the most common cancers, and the number of deaths related to esophageal cancer ranks sixth worldwide[1]. The histology of esophageal cancer mainly consists of squamous cell carcinoma (SCC) and adenocarcinoma. Especially in developing countries and Asian countries, SCC accounts for about 90% of esophageal cancer[2]. Esophageal cancer at an advanced stage brings a dismal prognosis; thus, the detection of esophageal cancer at an early stage is needed to obtain a higher quality of life and better prognosis[3,4].
However, it is difficult to detect esophageal SCC at an early stage using white light imaging endoscopy (WLI), because most of the superficial esophageal SCCs (SESCC) appear flat and/or isochromatic[4]. Lugol staining has high sensitivity for the detection of SESCCs but low specificity, as well as the potential for adverse effects including severe discomfort and allergic reaction[5].
Narrow Band Imaging (NBI) is a revolutionary technology utilizing optical imaged-enhanced endoscopy for diagnosing SESCCs[6,7]. The NBI can visualize a SESCC clearly as a well-demarcated brownish area without the use of Lugol staining. However, the brownish appearance occasionally represents a false-positive SESCC, because esophageal mucosa with inflammation also appears brown under NBI[8,9].
In the normal esophageal mucosa, loop-like vessels arise from the subepithelial capillary network beneath the epithelium. These microvessels are inside the epithelial papillae and named “intrapapillary capillary loops (IPCLs)”[6]. The IPCLs or abnormal microvessels in the superficial layer of the lesion are clearly visualized on magnifying endoscopy in combination with NBI.
SESCC lesions have abnormal microvessels with severe irregularity. The severe irregularity is defined as having morphological changes as follows: “dilation”, “tortuosity”, “change in caliber”, and “various shapes (VS)”[6,10]. When SCC invades up to the lamina propria mucosae, the abnormal microvessels with severe irregularity show a loop-like formation. When the tumor invasion reaches the muscularis mucosae or shallowly invades the submucosae, abnormal microvessels show no loop-like formation that has a stretched and markedly elongated transformation. The tumor deeply invading the submucosae has abnormal vessels with severe dilation and green color. Thus, the identification of IPCLs and abnormal microvessels can contribute to accurate diagnosis and reduced false-positive results in the diagnosis of SESCC[6,8]. Previous studies have shown a significantly higher diagnostic accuracy for SESCC with NBI combined with magnifying endoscopy (NBI-ME) when compared with WLI and Lugol chromoendoscopy[4,8].
NBI-ME is not widely used despite its high diagnostic performance[11]. Previous studies proposed a total of 6 NBI-ME findings that are significantly suggestive of SESCC. The 6 NBI-ME findings comprise complicated diagnostic criteria that may prove confusing for general endoscopists and prevent the widespread application of NBI-ME[4,6,12,13]. We considered that simplifying the NBI-ME diagnostic criteria. It may overcome the issues on NBI-ME if the NBI-ME diagnostic criteria can be simplified. The aim of this study was to identify NBI-ME findings for construction of simplified criteria for diagnosing SESCC.
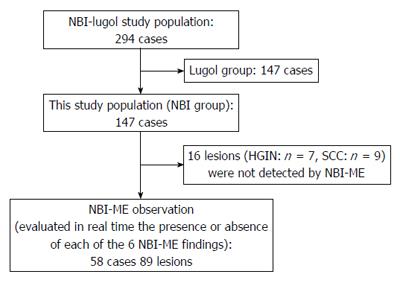
This study was carried out as a post-hoc analysis by using the data from our previous study of RCT (NBI-Lugol study)[8]. The NBI-Lugol study was approved by the institutional review board at the Jikei University School of Medicine and was compliant with the Declaration of Helsinki. The patients who had a histologically confirmed present or past history of SCC in the head and neck, or esophagus from January 2009 to June 2011 were randomly assigned to the NBI group (n = 147) or Lugol group (n = 147). Only patients in the NBI group underwent the NBI-ME inspection. Therefore, the data from NBI group patients was analyzed in this study (Figure 1). The exclusion criteria in the NBI-Lugol study were as follows: (1) prior esophagectomy; (2) history of chemotherapy or radiotherapy for SESCC; (3) recent history of chemotherapy for any malignancy; (4) history of intolerance to Lugol chromoendoscopy or allergic reaction to iodine; (5) concurrent presentation of an esophageal varix; (6) current pregnancy in women; and (7) contraindication to stopping antiplatelet or anticoagulant medication.
NBI-ME was performed using a high-definition magnifying endoscope (GIF-H260Z; Olympus, Tokyo, Japan) and a 19-inch high-resolution liquid-crystal monitor (OEV19H, Olympus). The combination of the endoscope and the monitor enabled endoscopic examination at a maximum magnification of 90-fold. A black rubber attachment (MB-46, Olympus) was mounted on the tip of the endoscope to maintain an adequate distance between the tip of the endoscope and the targeted lesion. The NBI-ME inspections were all performed by two experts (Goda K or Yoshimura N) who both had experience in NBI-ME observation of more than 200 SESCC cases.
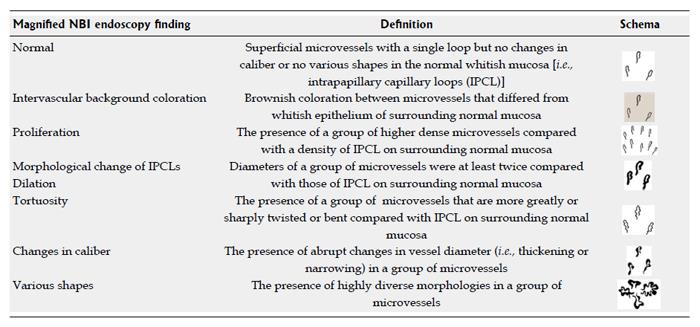
Under NBI without magnification, we detected all well-demarcated brownish areas > 5 mm in diameter and non-brownish areas with elevation or depression that were suspicious for SESCC. Once the suspicious lesion was detected, we performed further inspection subsequently by adding magnification with NBI (i.e., NBI-ME), and the suspicious lesions was evaluated in real time the presence or absence of each of the 6 NBI-ME findings (Figure 2). Finally, we applied Lugol solution, and biopsies were taken from all target lesions that were detected under NBI and irregularly shaped lesions > 5 mm diameter identified with Lugol staining. The biopsied lesions were removed by endoscopic or surgical resection if histology demonstrated high-grade intraepithelial neoplasia (HGIN) or SCC. We analyzed lesions that were detected by NBI inspection and excluded lesions that were detected only by Lugol chromoendoscopy in this study.
NBI enhances the contrast between microvessels and background mucosa in the esophagus, so that microvessels can be observed clearly using NBI-ME[6]. Inoue et al[6,12-14] observed the last branch of the superficial vascular structures in the esophagus and named it the IPCL. Moreover, they proposed a close relationship between morphological changes of IPCLs and histological atypia. The lesions were highly suspicious for SESCC in the lesions had the four following morphological changes: “dilation,”“tortuosity,”“change in caliber,” and “VS” (i.e., Inoue’s tetrad criteria)[6,12,15]. Inoue’s tetrad criteria are the most popular NBI-ME diagnostic criteria for SESCC[10].
Proliferation[8,16,17] and intervascular background coloration (IBC) (i.e., background coloration[18,19], brownish epithelium[13,20,21], and inter-vascular brownish epithelium[8,16]) are also NBI-ME findings strongly suggestive of SECCC. These 6 NBI-ME findings were prospectively evaluated in the NBI-Lugol study[8]. The definitions of the NBI-ME findings are listed in Figure 2.
The primary goal was to identify a minimal number of NBI-ME criteria for SESCC. The secondary goal was to evaluate diagnostic performance of the simplified criteria compared to Inoue’s tetrad criteria.
The histology from biopsied or endoscopically/surgically resected specimens was evaluated by a pathologist (Ikegami M) who was experienced in diagnosing early esophageal cancers and blinded to any endoscopic findings. The histological diagnosis was established according to the Japanese classification of esophageal cancer[22]. SESCC was histologically defined as HGIN or SCC invading up to the submucosa. If the histology results were different between the biopsied and resected specimens in the same lesion, the worse histology was considered the final histology of the lesion.
To assess the relationship between each NBI-ME finding and the diagnosis of SESCC, the Pearson χ2 test was used for comparisons of variables in a univariate analysis. We did not perform a multivariate analysis because a stepwise logistic regression analysis was used to estimate the association between histologically determined SESCC and the 6 NBI-ME findings, as well as to identify the best combination of NBI-ME findings for diagnosing SESCC.
The associations were evaluated in terms of odds ratio with 95%CI. The diagnostic performances of the simplified and Inoue’s tetrad criteria were evaluated by means of the area under the curve (AUC) from the receiver operating characteristic (ROC) curve. The diagnostic values (sensitivity, specificity, and overall accuracy) were calculated based on the per lesion analysis. Categorical variables were compared using the χ2 test or Fisher’s exact test. Statistical significance was defined as a two-tailed P value of < 0.01. Stata Version 11 software (Stata Corp, College Station, Texas, United States) was used for all statistical analyses.
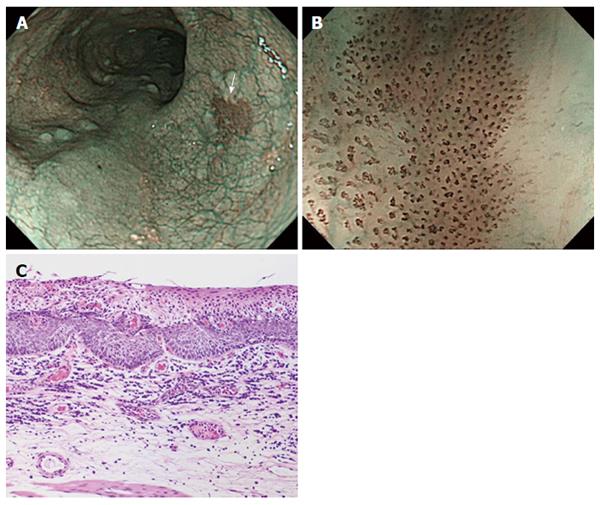
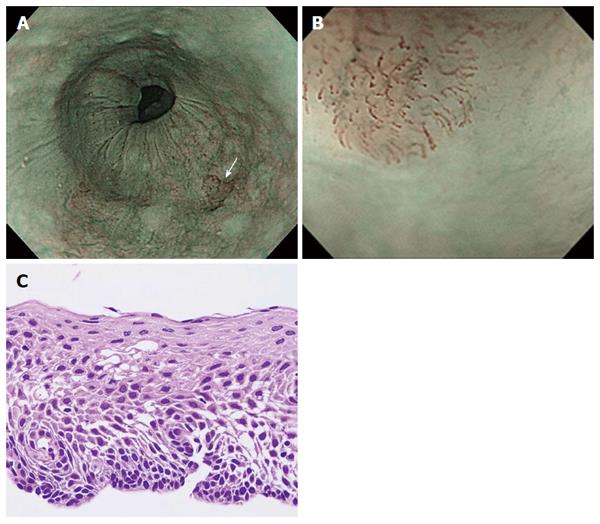
The demographics of patients and lesions are listed Table 1. The median age of patients was 67 year-old, and 88% of patients were male. Eighty-five patients had a history of head and neck SCCs, while seventy-four had a history of SESCCs. The median lesion size was 15 mm. The histology of 54 lesions (65%) was SESCC, 27 were low-grade intraepithelial neoplasia (LGIN), and 8 were inflammation. In the 54 SESCC lesions, the median diameter was 19 mm, the majority (87%) had a flat appearance (0-IIb) on endoscopy, and more than half of the SESCCs (59%) were confined to the lamina propria mucosae and treated with endoscopic resection (Figures 3 and 4).
| Number of patients | n= 147 |
| Age (yr), median (range) | 67 (39-86) |
| Male, n (%) | 130 (88%) |
| History of cancers (head and neck/esophagus) | 85/74 |
| Drinking history | |
| Number of drinkers | 134 |
| Drinking duration (yr), median (range) | 40 (10-68) |
| Number of flushers | 102 |
| Smoking history | |
| Number of smokers | 129 |
| Smoking (yr), median (range) | 35 (3-70) |
| Number of lesions | 89 |
| Diameter of lesions (mm), median (range) | 15 (4-100) |
| Histology (SCC/HGIN/LGIN/inflammation) | 48/6/27/8 |
| Superficial esophageal squamous cell carcinoma (including HGIN) | 54 |
| Diameter (mm), median (range) | 19 (4-100) |
| Macroscopic type; n, (0-I/0-IIa/0-IIb/0-IIc /0-III) | 5/2/25/21/1 |
| Depth of invasion; n, (HGIN/EP, LP/MM- SM1/SM2/unknown1) | 3/29/7/3/12 |
| Treatment; n, (ER/SR/CRT/others) | 32/11/5/6 |
In the univariate analysis (Table 2), proliferation, tortuosity, change in caliber, and VS were significantly associated with SESCC (P < 0.01). The combination of VS and proliferation was statistically extracted from the 6 NBI-ME findings by using a stepwise logistic regression model. We defined the combination of VS and proliferation as a simplified “dyad criteria” for the NBI-ME diagnosis of SESCC.
| NBI-ME findings | Esophagitis | LGIN | SESCC | Odds ratio (95%CI) | P value |
| (n = 8) | (n = 27) | (n = 54) | |||
| IBC | 1 (13) | 19 (70) | 45 (83) | 3.3 (1.2-8.9) | NS |
| Proliferation | 3 (38) | 21 (78) | 50 (93) | 5.0 (1.4-17.5) | < 0.01 |
| Dilatation | 3 (38) | 20 (74) | 48 (89) | 3.6 (1.2-11.1) | NS |
| Tortuosity | 2 (25) | 14 (52) | 44 (81) | 5.2 (2.0-13.6) | < 0.01 |
| Change in caliber | 2 (25) | 6 (22) | 31 (57) | 4.5 (1.7-11.8) | < 0.01 |
| Various shapes | 3 (38) | 14 (52) | 46 (85) | 5.4 (2.0-14.8) | < 0.01 |
The diagnostic performance of the simplified dyad criteria was compared with that of Inoue’s tetrad criteria using the ROC curve. The AUC of the simplified dyad criteria and Inoue’s tetrad criteria were 0.70 (95%CI: 0.60-0.80) and 0.73 (95%CI: 0.63-0.84), respectively. No significant difference was shown between them (Figure 5).
The sensitivity of a brownish area alone and simplified dyad criteria for diagnosing SESCC were 92.6% and 77.8%. There was no difference between them. The specificity of the simplified dyad criteria was significantly greater than that of a brownish area alone (P < 0.01, Table 3). There was no difference between the specificity of simplified dyad criteria and that of Inoue’s criteria (57.1% vs 80.0%).
Using the data from the RCT (NBI-Lugol study) and a stepwise logistic regression model, VS and proliferation were extracted from the 6 NBI-ME findings that had been reported to be strongly suggestive of SESCC[6,8,13]. VS and proliferation might be candidates for simplified criteria with diagnostic performance comparable to Inoue’s tetrad criteria.
We evaluated 6 NBI-ME findings that have been previously reported as useful for diagnosing SESCC[6,8,13]. The 6 NBI-ME findings can be divided into the following three categories: 4 morphological changes (i.e., dilation, tortuosity, change in caliber, VS), an increasing number of IPCLs (proliferation), and color change of background mucosa (i.e., IBC). VS was statistically extracted as one of the simplified dyad criteria for the prediction of SESCC. VS may be indicative of the presence of the other 3 morphological changes of IPCLs, because 95% of the lesions with VS also had dilation, tortuosity, or change in caliber. Thus, VS may more efficiently represent 3 morphological changes of IPCLs.
In contrast, proliferation is not related to IPCL morphology but to newly developed microvasculature. A previous study showed that vasculature increases during the early phases of cancer development[23]. Kumagai et al[24] already indicated that the microvessel density in SESCC gradually increased in proportion to the depth by using immunohistochemical staining with CD34 and CD105. Their study will support our result that proliferation of IPCLs is one of two highly suggestive NBI-ME findings to diagnose SESCC. This may be the reason why proliferation was extracted as the other factor of the simplified dyad criteria. Proliferation may complement the diagnostic value of IPCL morphological changes, including VS. Thus, it seemed reasonable that these two findings based on IPCL morphology and newly developed microvasculature were the best combination for diagnosing SESCC.
Several studies have shown a close relationship between IBC and SESCC[18-21]; however, IBC was not extracted from the 6 NBI-ME findings and not included in the simplified dyad criteria. IBC might be caused by an extravascular component of hemoglobin that is produced within tumor cells[25], as well as thinning of the keratinous layer or epithelium caused by neoplastic cell proliferation[19]. LGIN cells may be the source of the hemoglobin, while intraepithelial infiltration of inflammatory cells may cause the thinning the keratinous layer or epithelium. Thus, LGIN and esophageal mucosa with inflammation may demonstrate IBC, and this may be the reason why IBC was not extracted in this study.
A brownish area is a reliable landmark in the detection of SESCC, as the presence of a brownish area alone showed a very high sensitivity (92.6%). However, since SESCC detection based on a brownish area alone involved a high false-positive rate as seen in a previous study[8,9], the specificity of a brownish area was considerably low (8.6%) in this study. Simplified and Inoue’s criteria showed a much higher specificity but lower sensitivity than the presence of a brownish area alone. As with Inoue’s tetrad criteria, the simplified dyad criteria of NBI-ME will reduce the high false-positive rate of a brownish area alone.
Concerning the esophagus, we propose an ideal endoscopic examination as follows. Initially, we should pay attention to elevated or depressed lesions and brownish areas using an NBI non-magnifying endoscopy. We then evaluate for the presence of VS and proliferation under NBI-ME for all suspicious lesions. This strategy may allow endoscopists to detect and discriminate SESCC from inflammation and LGIN easily, quickly, and accurately. The dyad criteria may enable a simplified diagnosis of SESCC and lead to widespread use of the NBI-ME.
This study has several limitations. First, this is a retrospective study based on statistical analysis. A prospective study with a clinical setting is needed to validate these study results. Second, NBI-ME findings were evaluated only by expert endoscopists. The diagnostic utility of the simplified dyad criteria should be validated by non-experts as well as experts. Finally, the lesions detected only by Lugol chromoendoscopy were not included in this study. However, it may not affect the results, as the number of SESCCs only detected by Lugol chromoendoscopy was small.
In conclusion, the combination of VS and proliferation may be considered simplified criteria for diagnosis of SESCC based on NBI-ME findings.
A part of this paper was presented as an oral presentation at the United European Gastroenterology Week, October 12-16th, 2013 in Berlin, Germany.
The prognosis of patients with esophageal squamous cell carcinoma (SCC) is improved if the tumor is detected at an early stage. The usefulness of Narrow Band Imaging combined with magnifying endoscopy (NBI-ME) for early detection and characterization of superficial esophageal SCC (SESCC) has been previously reported. However, NBI-ME is somewhat limited in clinical application because the current criteria for NBI-ME findings are complicated. Thus, simplified criteria are needed.
The following 6 NBI-ME findings have been reported as significant diagnostic markers for SESCCs: “dilation”, “tortuosity”, “change in caliber”, “various shapes (VS)”, “proliferation” of intrapapillary capillary loops (IPCLs), and “intervascular background coloration”. No reports have provided simplified criteria for diagnosing SESCC by using NBI-ME. The goal of this study was to simplify the diagnostic criteria.
If simplified criteria are newly created, the process of diagnosing SESCCs using NBI-ME would be facilitated, which would result in widespread use of magnifying endoscopy.
The simplified dyad criteria were compatible in diagnostic performance to Inoue’s tetrad criteria. If a brownish area or other suspicious lesion is found during NBI endoscopy without magnification, the simplified criteria may be useful to differentiate a neoplasia from a non-neoplastic lesion.
NBI is a revolutionary optical image-enhanced technology. NBI enhances the contrast between the microvessels and background mucosa in the esophagus. Thus, visibility of the microvessels is improved when NBI is combined with magnifying endoscopy. Inoue’s tetrad criteria are the most popular NBI-ME diagnostic criteria for SESCC and consist of the four following morphological changes: “dilation”, “tortuosity”, “change in caliber”, and “VS” of IPCLs. On the other hand, the simplified criteria are composed of proliferation and VS of IPCLs.
The authors pointed out the difficulty of Inoue’s tetrad criteria and proposed simplified diagnostic criteria for the changes of the IPCL. From the statistical analysis, the authors extracted “various shapes” from the tetrad criteria as the most significant parameter for the prediction of SESCC. In addition, the authors also focused on the “proliferation of the IPCLs” and proposed simplified criteria by combining the “VS of the IPCLs” and “proliferation of the IPCLs”.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Kumagai Y, Surucu E S- Editor: Yu J L- Editor: A E- Editor: Zhang FF
| 1. | Ferlay J, Soerjomataram I, Ervik M, Dikshit , R , Eser S, Mathers C, Rebelo M, Parkin DM, Forman D. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. Lyon, France: International Agency for Research on Cancer 2013; Available from: http://globocan.iarc.fr, accessed on 18/12/2013. |
| 2. | Pickens A, Orringer MB. Geographical distribution and racial disparity in esophageal cancer. Ann Thorac Surg. 2003;76:S1367-S1369. [PubMed] |
| 3. | Daly JM, Karnell LH, Menck HR. National Cancer Data Base report on esophageal carcinoma. Cancer. 1996;78:1820-1828. [PubMed] |
| 4. | Muto M, Minashi K, Yano T, Saito Y, Oda I, Nonaka S, Omori T, Sugiura H, Goda K, Kaise M. Early detection of superficial squamous cell carcinoma in the head and neck region and esophagus by narrow band imaging: a multicenter randomized controlled trial. J Clin Oncol. 2010;28:1566-1572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 427] [Cited by in RCA: 523] [Article Influence: 34.9] [Reference Citation Analysis (0)] |
| 5. | Meyer V, Burtin P, Bour B, Blanchi A, Cales P, Oberti F, Person B, Croue A, Dohn S, Benoit R. Endoscopic detection of early esophageal cancer in a high-risk population: does Lugol staining improve videoendoscopy? Gastrointest Endosc. 1997;45:480-484. [PubMed] |
| 6. | Yoshida T, Inoue H, Usui S, Satodate H, Fukami N, Kudo SE. Narrow-band imaging system with magnifying endoscopy for superficial esophageal lesions. Gastrointest Endosc. 2004;59:288-295. [PubMed] |
| 7. | Muto M, Katada C, Sano Y, Yoshida S. Narrow band imaging: a new diagnostic approach to visualize angiogenesis in superficial neoplasia. Clin Gastroenterol Hepatol. 2005;3:S16-S20. [PubMed] |
| 8. | Goda K, Dobashi A, Yoshimura N, Kato M, Aihara H, Sumiyama K, Toyoizumi H, Kato T, Ikegami M, Tajiri H. Narrow-Band Imaging Magnifying Endoscopy versus Lugol Chromoendoscopy with Pink-Color Sign Assessment in the Diagnosis of Superficial Esophageal Squamous Neoplasms: A Randomised Noninferiority Trial. Gastroenterol Res Pract. 2015;2015:639462. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 9. | Lee CT, Chang CY, Lee YC, Tai CM, Wang WL, Tseng PH, Hwang JC, Hwang TZ, Wang CC, Lin JT. Narrow-band imaging with magnifying endoscopy for the screening of esophageal cancer in patients with primary head and neck cancers. Endoscopy. 2010;42:613-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 101] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 10. | Oyama T, Inoue H, Arima M, Momma K, Omori T, Ishihara R, Hirasawa D, Takeuchi M, Tomori A, Goda K. Prediction of the invasion depth of superficial squamous cell carcinoma based on microvessel morphology: magnifying endoscopic classification of the Japan Esophageal Society. Esophagus. 2016;In press. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 159] [Cited by in RCA: 223] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 11. | Goda K, Dobashi A, Tajiri H. Perspectives on narrow-band imaging endoscopy for superficial squamous neoplasms of the orohypopharynx and esophagus. Dig Endosc. 2014;26 Suppl 1:1-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Inoue H, Honda T, Nagai K. Ultra-high magnification endoscopic observation of carcinoma in situ. Dig Endosc. 1997;1:16-18. [RCA] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 117] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 13. | Ishihara R, Inoue T, Uedo N, Yamamoto S, Kawada N, Tsujii Y, Kanzaki H, Hanafusa M, Hanaoka N, Takeuchi Y. Significance of each narrow-band imaging finding in diagnosing squamous mucosal high-grade neoplasia of the esophagus. J Gastroenterol Hepatol. 2010;25:1410-1415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 57] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 14. | Kumagai Y, Inoue H, Nagai K, Kawano T, Iwai T. Magnifying endoscopy, stereoscopic microscopy, and the microvascular architecture of superficial esophageal carcinoma. Endoscopy. 2002;34:369-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 164] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 15. | Sato H, Inoue H, Ikeda H, Sato C, Onimaru M, Hayee B, Phlanusi C, Santi EG, Kobayashi Y, Kudo SE. Utility of intrapapillary capillary loops seen on magnifying narrow-band imaging in estimating invasive depth of esophageal squamous cell carcinoma. Endoscopy. 2015;47:122-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 16. | Yoshimura N, Goda K, Tajiri H, Yoshida Y, Kato T, Seino Y, Ikegami M, Urashima M. Diagnostic utility of narrow-band imaging endoscopy for pharyngeal superficial carcinoma. World J Gastroenterol. 2011;17:4999-5006. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Goda K, Dobashi A, Yoshimura N, Aihara H, Kato M, Sumiyama K, Toyoizumi H, Kato T, Saijo H, Ikegami M. Dual-focus versus conventional magnification endoscopy for the diagnosis of superficial squamous neoplasms in the pharynx and esophagus: a randomized trial. Endoscopy. 2016;48:321-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 18. | Minami H, Inoue H, Ikeda H, Satodate H, Hamatani S, Nakao K, Kudo SE. Usefulness of Background Coloration in Detection of Esophago-Pharyngeal Lesions Using NBI Magnification. Gastroenterol Res Pract. 2012;2012:529782. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Takahashi M, Shimizu Y, Ono M, Suzuki M, Omori S, Yoshida T, Mori Y, Nakagawa M, Ono S, Nakagawa S. Endoscopic diagnosis of early neoplasia of the esophagus with narrow band imaging: correlations among background coloration and iodine staining findings. J Gastroenterol Hepatol. 2014;29:762-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 20. | Mochizuki Y, Saito Y, Kobori A, Ban H, Shioya M, Nishimura T, Inatomi O, Bamba S, Tsujikawa T, Ishida M. Magnified endoscopy combined with narrow band imaging of minimal superficial esophageal neoplasia-indicators to differentiate intraepithelial neoplasias. J Gastrointest Cancer. 2012;43:599-606. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Kanzaki H, Ishihara R, Ishiguro S, Nagai K, Matsui F, Yamashina T, Ohta T, Yamamoto S, Hanaoka N, Hanafusa M. Histological features responsible for brownish epithelium in squamous neoplasia of the esophagus by narrow band imaging. J Gastroenterol Hepatol. 2013;28:274-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Japan Esophageal Society. Japanese Classification of Esophageal Cancer, 10th edition. Tokyo, Japan: Kanehara & Co Ltd 2007; . |
| 23. | Kumagai Y, Toi M, Inoue H. Dynamism of tumour vasculature in the early phase of cancer progression: outcomes from oesophageal cancer research. Lancet Oncol. 2002;3:604-610. [PubMed] |
| 24. | Kumagai Y, Sobajima J, Higashi M, Ishiguro T, Fukuchi M, Ishibashi K, Baba H, Mochiki E, Yakabi K, Kawano T. Angiogenesis in superficial esophageal squamous cell carcinoma: assessment of microvessel density based on immunostaining for CD34 and CD105. Jpn J Clin Oncol. 2014;44:526-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 25. | Minami H, Isomoto H, Nakayama T, Hayashi T, Yamaguchi N, Matsushima K, Akazawa Y, Ohnita K, Takeshima F, Inoue H. Background coloration of squamous epithelium in esophago-pharyngeal squamous cell carcinoma: what causes the color change? PLoS One. 2014;9:e85553. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |