Published online Aug 14, 2016. doi: 10.3748/wjg.v22.i30.6955
Peer-review started: December 19, 2015
First decision: January 13, 2016
Revised: February 3, 2016
Accepted: March 1, 2016
Article in press: March 1, 2016
Published online: August 14, 2016
Processing time: 231 Days and 13.5 Hours
Despite the ongoing decrease in the frequency of complications after hepatectomy, biliary fistulas still occur and are associated with high morbidity and mortality rates. Here, we report on an unusual technique for managing biliary fistula following left hepatectomy in a patient in whom the right posterior segmental duct joined the left hepatic duct. The biliary fistula was treated with a combined radiologic and endoscopic procedure based on the “rendezvous technique”. The clinical outcome was good, and reoperation was not required.
Core tip: Despite the ongoing decrease in the frequency of complications after hepatectomy, biliary fistulas still occur and are associated with high morbidity and mortality rates. In most literature reports, surgical treatment is the gold standard for management of biliary fistula but is associated with greater morbidity. We report on an unusual technique for managing biliary fistula following left hepatectomy in a patient in whom the right posterior segmental duct joined the left hepatic duct. The biliary fistula was treated with a combined radiologic and endoscopic procedure based on the “rendezvous technique” without the need for reoperation.
- Citation: Gracient A, Rebibo L, Delcenserie R, Yzet T, Regimbeau JM. Combined radiologic and endoscopic treatment (using the “rendezvous technique”) of a biliary fistula following left hepatectomy. World J Gastroenterol 2016; 22(30): 6955-6959
- URL: https://www.wjgnet.com/1007-9327/full/v22/i30/6955.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i30.6955
Thanks to better surgical techniques, anatomical knowledge and pre- and perioperative support, post-hepatectomy morbidity and mortality rates have fallen over the last 20 years.
Nevertheless, post-hepatectomy complications still occur. In particular, biliary fistula is present in 3%-10% of cases and is a real problem; reoperation of these patients is associated with a morbidity rate of 70%[1] and a mortality rate of around 7%[2]. Improved endoscopic and radiologic procedures have opened the way to less invasive treatments of fistulae[3]. Here, we report on the use of a combined radiologic and endoscopic procedure (based on the “rendezvous technique”) to treat biliary fistula following left hepatectomy in a patient in whom the right posterior segmental duct (RPSD) joined the left hepatic duct (LHD).
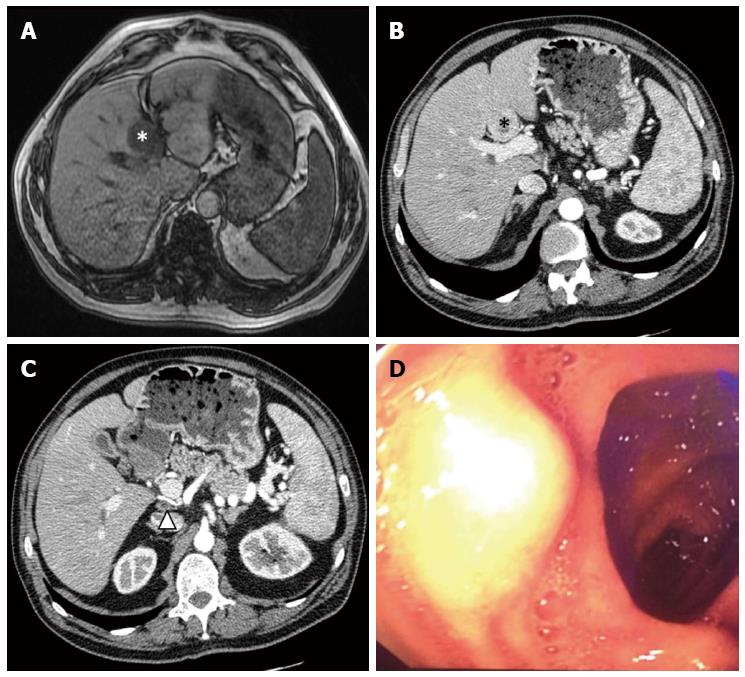
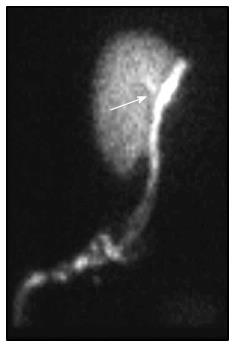
A 66-year-old man was referred to our institution for duodenal gastrinoma revealed by Zollinger-Ellison syndrome. Pre-operative endoscopic ultrasonography showed a tumor on the superior flexure and in a single retroportal lymph node. An endoscopic biopsy revealed the gastrinoma. A contrast-enhanced computed tomography (CT) scan of the abdomen evidenced a single lesion on segment IV of the liver, and a liver biopsy confirmed the presence of metastases of gastrinoma. Magnetic resonance imaging (MRI) of the liver showed that a metastasis had invaded the LHD (Figure 1). Octreotide scintigraphy confirmed uptake by the retroportal node and the liver metastasis.
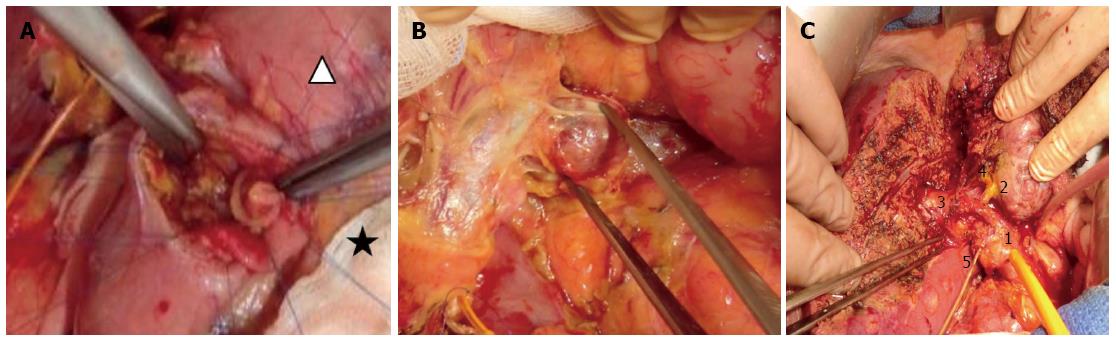
Before performing laparotomic surgery, an upper endoscopy enabled us to locate the gastrinoma. The surgical procedure started with a Kocher maneuver, in order to mobilize the first and second parts of the duodenum. Next, a duodenotomy on the superior duodenal flexure gave us access to the duodenal gastrinoma, which was then resected. The duodenotomy was then closed in two steps (using 3/0 monofilament, non-absorbable suture) via two half running sutures in the mucosal and then serosal planes. Lymphadenectomy was performed after closure of the duodenotomy (Figure 2).
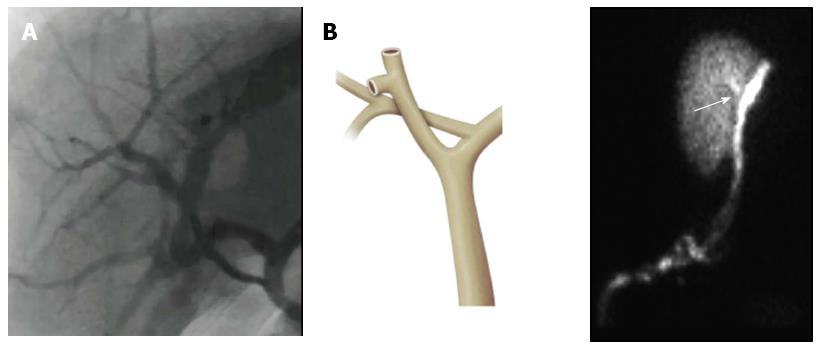
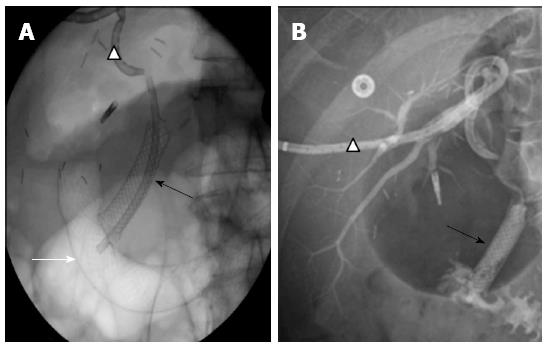
Prior to the left hepatectomy, intra-operative cholangiography evidenced dilatation of the RPSD and the LHD and revealed confluence between these two ducts (Figure 3). Careful dissection enabled us to isolate the RPSD and its junction with the LHD. After bile duct isolation, various clamping maneuvers were performed (with intra-operative cholangiography), in order to check that the anterior and posterior sections of the right hepatic duct were intact (Figure 4). Left hepatectomy was performed with conservation of the RPSD, by clamping the LHD above the confluence. To check for leakage after left hepatectomy, we performed a methylene blue test. The left hepatectomy was performed without reconstructing the biliary ducts (which would have required hepaticojejunal anastomosis of the RPSD, for example).
The patient’s post-operative condition suggested the presence of a biliary fistula, which was diagnosed on post-operative day 10 and drained by inserting an external drain through an old drainage orifice; this also enabled irrigation of the biliary fistula. The fistula was well tolerated and did not require immediate reoperation. A contrast-enhanced CT scan of the abdomen and hepatobiliary scintigraphy confirmed the presence of a biliary fistula on the RPSD (Figure 5).
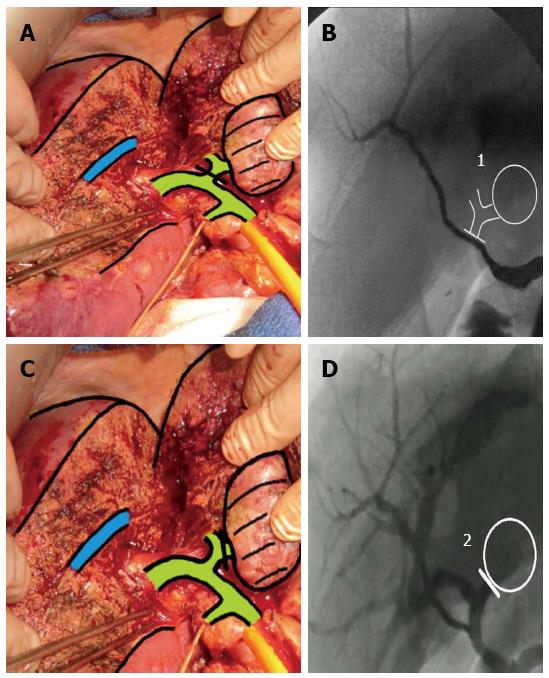
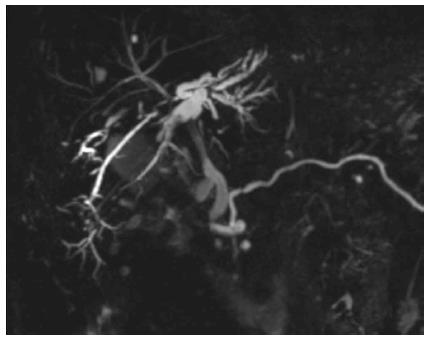
After a multidisciplinary team meeting (involving the surgeons, an endoscopist and a radiologist), we selected a combined radiologic and endoscopic treatment using the “rendezvous technique”. Firstly, the excluded RPSD was drained with an 8.5 French percutaneous catheter (Cook Ireland Ltd, Limerick, Ireland). Next, drainage allowed us to subsequently catheterize the main hepatic duct (via a transhepatic approach) and create a new prosthetic duct (using a percutaneous catheter). An 8-cm biliary fully-covered self-expanding metal stent (Zilver®, Cook Ireland Ltd) was inserted, in order to decrease pressure on the biliary duct. In order to avoid migration, a 14-cm duodenal covered stent (Hanarostent®, Life Partners Europe, Bagnolet, France) was positioned next to the biliary stent’s distal portion. Next, a 12-cm, 8.5 French plastic Cotton-Leung biliary stent (Cook Ireland Ltd) was placed into the covered self-expanding metal stent through the duodenal stent (in order to avoid migration of the latter) and located next to the inlet of the external drain (Figure 6). After bile flow through the external drain had fallen significantly (by day 7 following the combined procedure), the drain was clamped and then removed a few days later. The stents were removed 45 d after their implementation. One year after stent removal, the patient was symptom-free and clinical biochemical tests confirmed the absence of cholestasis. MRI of the liver showed a moderately dilated RPSD (Figure 7).
With an incidence of between 3% and 10%, biliary fistulas are common complications of hepatectomy[4-8]. The risk of biliary fistula is greater still in patients with an anatomic variation. In our patient, the RPSD joined the LHD; this corresponds to D1 in the Couinaud classification, and is present in 6% to 16.8% of individuals[2,9,10].
The intra-operative discovery of this anatomic variation left us with two possible solutions: (1) left hepatectomy with maintenance of the RPSD; and (2) hepaticojejunal anastomosis and resection of the confluence between the RPSD and the LHD. We chose not to perform hepaticojejunal anastomosis on the RPSD because of (1) its difficulty in the present case; and (2) the satisfactory results of an intra-operative methylene blue test and intra-operative cholangiography (as recommended[2]). We observed complete opacification of the RPSD after a clamping maneuver and thus the absence of biliary stenosis or fistula[11]. The occurrence of a late biliary fistula (type D, according to Nagano’s classification[12]) in the RPSD was probably due to necrosis caused during coagulation, since there was no leakage in the methylene blue test and no particular signs of leakage on the intra-operative cholangiography after completion of the left hepatectomy. In retrospect, this should have prompted us to perform hepaticojejunal anastomosis.
Treatment of this type of complication is challenging. An endoscopic approach is often associated with better outcomes and lower morbidity than further surgery[13,14]. After discussing the case with our endoscopist and our radiologist, we considered that a rendezvous technique was feasible - even through reoperation is the recommended treatment for this type of post-operative complication[12,15]. The absence of biliary peritonitis and good overall tolerance of the biliary fistula prompted us to implement the combined endoscopic and radiologic approach.
In conclusion, we reported on the peri-operative adaptation of a surgical technique during left hepatectomy in a patient with an anatomic variation. Post-operative treatment using the rendezvous technique was feasible for an experienced team of surgeons.
A 66-year-old man was managed for biliary fistula following left hepatectomy in a patient in whom the right posterior biliary segmental duct joined the left hepatic duct.
Abdominal pain and fever.
Post-operative abscess or hematoma.
Patient had biological inflammatory syndrome.
Post-operative collection next to the confluence of the right posterior segmental duct.
All pathological findings were normal for biliary fistula.
Combined radiologic and endoscopic treatment using the “rendezvous technique” using multiple stents.
Biliary fistula after hepatectomy is a common complication. The risk of biliary fistula is greater in patients with an anatomic variation.
Biliary fistula following hepatectomy is associated with a high morbidity and mortality. Reoperation is usually required.
Post-operative treatment of post-operative biliary fistula following hepatectomy is feasible using the rendezvous technique and allows for avoidance of reoperation.
This is a well written, concise and elegant description of a new technique for management of complications. The intra-operative images are of excellent quality.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Galvão FH, Hii MW, Sanal MG, Wang DS S- Editor: Gong ZM L- Editor: Filipodia E- Editor: Ma S
| 1. | Pace RF, Blenkharn JI, Edwards WJ, Orloff M, Blumgart LH, Benjamin IS. Intra-abdominal sepsis after hepatic resection. Ann Surg. 1989;209:302-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 58] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Lo CM, Fan ST, Liu CL, Lai EC, Wong J. Biliary complications after hepatic resection: risk factors, management, and outcome. Arch Surg. 1998;133:156-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 116] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 3. | Farhat S, Bourrier A, Gaudric M, Dousset B, Scatton O, Chaussade S, Prat F. Endoscopic treatment of biliary fistulas after complex liver resection. Ann Surg. 2011;253:88-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Capussotti L, Ferrero A, Viganò L, Sgotto E, Muratore A, Polastri R. Bile leakage and liver resection: Where is the risk? Arch Surg. 2006;141:690-694; discussion 695. [PubMed] |
| 5. | Lam CM, Lo CM, Liu CL, Fan ST. Biliary complications during liver resection. World J Surg. 2001;25:1273-1276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 47] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Guillaud A, Pery C, Campillo B, Lourdais A, Sulpice L, Boudjema K. Incidence and predictive factors of clinically relevant bile leakage in the modern era of liver resections. HPB (Oxford). 2013;15:224-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 74] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 7. | Tanaka S, Hirohashi K, Tanaka H, Shuto T, Lee SH, Kubo S, Takemura S, Yamamoto T, Uenishi T, Kinoshita H. Incidence and management of bile leakage after hepatic resection for malignant hepatic tumors. J Am Coll Surg. 2002;195:484-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 128] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 8. | Yamashita Y, Hamatsu T, Rikimaru T, Tanaka S, Shirabe K, Shimada M, Sugimachi K. Bile leakage after hepatic resection. Ann Surg. 2001;233:45-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 255] [Article Influence: 10.6] [Reference Citation Analysis (2)] |
| 9. | Valette PJ, De Baere T. [Biliary and vascular anatomy of the liver]. J Radiol. 2002;83:221-234. [PubMed] |
| 10. | Kitagawa Y, Nimura Y, Hayakawa N, Kamiya J, Nagino M, Uesaka K, Oda K, Ohta A, Jan YY, Cheng LP. Intrahepatic segmental bile duct patterns in hepatolithiasis: a comparative cholangiographic study between Taiwan and Japan. J Hepatobiliary Pancreat Surg. 2003;10:377-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Nimura Y. [Percutaneous transhepatic cholangioscopy: technics and clinical studies]. Nihon Rinsho. 1984;42:2222-2227. [PubMed] |
| 12. | Nagano Y, Togo S, Tanaka K, Masui H, Endo I, Sekido H, Nagahori K, Shimada H. Risk factors and management of bile leakage after hepatic resection. World J Surg. 2003;27:695-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 137] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 13. | Eum YO, Park JK, Chun J, Lee SH, Ryu JK, Kim YT, Yoon YB, Yoon CJ, Han HS, Hwang JH. Non-surgical treatment of post-surgical bile duct injury: clinical implications and outcomes. World J Gastroenterol. 2014;20:6924-6931. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 25] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Fatima J, Barton JG, Grotz TE, Geng Z, Harmsen WS, Huebner M, Baron TH, Kendrick ML, Donohue JH, Que FG. Is there a role for endoscopic therapy as a definitive treatment for post-laparoscopic bile duct injuries? J Am Coll Surg. 2010;211:495-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Honoré C, Vibert E, Hoti E, Azoulay D, Adam R, Castaing D. Management of excluded segmental bile duct leakage following liver resection. HPB (Oxford). 2009;11:364-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |