Published online Aug 14, 2016. doi: 10.3748/wjg.v22.i30.6864
Peer-review started: March 19, 2016
First decision: April 14, 2016
Revised: May 16, 2016
Accepted: June 13, 2016
Article in press: June 13, 2016
Published online: August 14, 2016
Processing time: 141 Days and 2.5 Hours
Functional constipation (FC) is a significant health problem in children and contrary to common belief, has serious ramifications on the lives of children and their families. It is defined by the Rome criteria which encourage the use of multiple clinical features for diagnosis. FC in children has a high prevalence (0.7%-29%) worldwide, both in developed and developing countries. Biopsychosocial risk factors such as psychological stress, poor dietary habits, obesity and child maltreatment are commonly identified predisposing factors for FC. FC poses a significant healthcare burden on the already overstretched health budgets of many countries in terms of out-patient care, in-patient care, expenditure for investigations and prescriptions. Complications are common and range from minor psychological disturbances, to lower health-related quality of life. FC in children also has a significant impact on families. Many paediatric clinical trials have poor methodological quality, and drugs proved to be useful in adults, are not effective in relieving symptoms in children. A significant proportion of inadequately treated children have similar symptoms as adults. These factors show that constipation is an increasing public health problem across the world with a significant medical, social and economic impact. This article highlights the potential public health impact of FC and the possibility of overcoming this problem by concentrating on modifiable risk factors rather than expending resources on high cost investigations and therapeutic modalities.
Core tip: Constipation is a common problem in children worldwide. Identified risk factors for constipation are equally distributed in both developed and developing countries. Constipation affects the quality of life of affected children and their parents. It also poses a challenge for existing healthcare systems by incurring significant expenditure. These factors indicate that childhood constipation is emerging as a significant public health problem. Attention to careful toilet training, encouraging correct dietary habits, and creating a safer environment for children would curtail the public health impact of functional constipation.
- Citation: Rajindrajith S, Devanarayana NM, Crispus Perera BJ, Benninga MA. Childhood constipation as an emerging public health problem. World J Gastroenterol 2016; 22(30): 6864-6875
- URL: https://www.wjgnet.com/1007-9327/full/v22/i30/6864.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i30.6864
Functional constipation (FC) is a common disorder in children worldwide. Available data show that its prevalence is higher in the South Asian region and in South America, than in any other part of the world[1]. Rapidly changing socio-cultural and political factors such as urbanization, increasing levels of psychological stress, poor parenting skills, civil unrest and child maltreatment, have resulted in a large number of vulnerable children developing constipation (Figure 1)[2]. In this context, childhood constipation is threatening to become a major public health problem across the world.
The possible repercussions are alarming. Although it is not linked to mortality directly, constipation leads to poor health-related quality of life (HRQoL), poor school performance and consequently to deficiencies in education[3]. Clinical care of these children is not optimal due to a lack of understanding regarding the underlying pathophysiological mechanisms and the selection of appropriate therapeutic options. Children who are inadequately cared for are at a risk of developing both physical and psychological complications leading to a heavy burden on already overstretched health budgets[3]. All of these factors indicate that more attention should be focused on this important malady. Despite these facts, public health authorities have not paid sufficient attention to childhood constipation.
In this article we review current data on the epidemiology, predisposing factors, healthcare burden, and effects of constipation on the child and the family to support our hypothesis that FC is a major public health problem.
A healthy childhood is not the mere absence of disease but is a vibrant state of health, characterized by physical, mental and social wellbeing, which helps to achieve childhood growth, development and potential according to the genetic makeup and socio-cultural determinants[4]. During the last few decades, child health indices have greatly improved, including the control of major communicable diseases through immunization, with an approximately 50% reduction in child and neonatal mortality and a significant number of countries achieving the Millennium Development Goals[5,6]. However, a new set of challenges is emerging. These challenges include diseases of multi-factorial aetiologies such as bronchial asthma, obesity, substance abuse and functional gastrointestinal disorders (FGDs).
FGDs in children are clinical entities characterized by recurrent vomiting, chronic recurrent abdominal pain, and disturbed defecation without identifiable structural, anatomical or biochemical anomalies.
FC has high prevalence rates in many parts of the world[1,7]. It is also a significant healthcare burden, more than many other common childhood diseases[8]. It was clearly shown that the HRQoL of children with constipation is low[9]. The precise mechanisms of FC are not well understood and therapeutic options are limited to a few drugs and surgical procedures.
To date, there is no global consensus regarding the definition of constipation in children. Some researchers prefer to use single symptoms such as difficulty in passing stools to define FC[10,11]. Whereas several authorities define FC in children as a combination of different symptoms; the Iowa criteria, PACCT criteria, Rome II criteria, Rome III criteria, and recently the Rome IV criteria. Clearly there is no uniformity in these definitions[12-16] (Table 1). Therefore, epidemiological research based on such heterogeneous criteria has provided a blurred epidemiological picture of FC. When comparing the Rome II with the Rome III definitions for FC in the same population, Devanarayana et al[17] showed a 3-fold change in the prevalence of FC using these criteria (1.4% with Rome II and 4.4% with Rome III). In a clinic based chart review, Burgers et al[18] noted that the Rome III criteria were more sensitive in the diagnosis of FC than Rome II in older children. Contrary to these findings, a study from Thailand found that the Rome II criteria diagnosed FC more effectively than Rome III in young children in whom features of faecal retention were more prominent[19]. Although Rome III criteria state the presence of abdominal/rectal faecal mass as one of the diagnostic criteria, it is extremely difficult to use this criterion in epidemiological studies due to many constraints. Some have suggested that the elimination of this criterion would not make a major difference to the diagnosis of constipation[18,19]. However, these factors leave researchers with the dilemma of which criteria to choose for epidemiological and clinic based surveys.
| Rome II criteria (infants and young children) |
| At least 2 wk of: |
| Scybalous, pebble-like, hard stools for a majority of stools or firm stools two or less times/week; and there is no evidence of structural, endocrine, or metabolic disease. |
| Rome III criteria (children and adolescents) |
| Diagnostic criteria1 must include two or more of the following in a child with a developmental age of at least 4 yr with insufficient criteria for diagnosis of irritable bowel syndrome.: |
| Two or fewer defecations in the toilet per week |
| At least one episode of faecal incontinence per week |
| History of retentive posturing or excessive volitional stool retention |
| History of painful or hard bowel movements |
| Presence of a large faecal mass in the rectum |
| History of large diameter stools which may obstruct the toilet |
| Rome IV criteria (Children and adolescents) |
| Must include 2 or more of the following occurring at least once per week for a minimum of 1 mo with insufficient criteria for a diagnosis of irritable bowel syndrome |
| Two or fewer defecations in the toilet per week in a child with a developmental age of at least 4 yr |
| At least 1 episode of faecal incontinence per week |
| History of retentive posturing or excessive volitional stool retention |
| History of painful or hard bowel movements |
| Presence of a large fecal mass in the rectum |
| History of large diameter stools which may obstruct the toilet |
| After appropriate evaluation, the symptoms cannot be fully explained by another medical condition. |
The current understanding of the definition is also not optimal among clinicians leading to poor acceptance and utilization. In a recent study, van Tilburg et al[20] showed that most paediatric gastroenterologists working in 2 centres in the US had a poor understanding and utilization of the Rome criteria. They showed major discrepancies when using a Rome questionnaire-based diagnosis and the actual clinical diagnosis[20]. Another study reported that approximately 80% of general practitioners had no knowledge of the Rome criteria for diagnosing FGDs[21]. In a survey of paediatric care providers in Saudi Arabia, it was noted that only 60% of clinicians were aware of the Rome criteria for the diagnosis of FC[22]. Therefore, it is imperative to redefine childhood FC using a consensus archetype agreed by healthcare professionals living in different parts of the world.
Paediatric researchers have shown that a child with FC may suffer from other FGDs simultaneously. A study from the United States found that only 19% of patients with a FGD qualified for a single diagnosis when using the Rome III criteria[20]. In another study, 29% and 5% had two and three Rome III diagnoses, respectively[23]. With such frequent overlapping diagnoses, it is sometimes difficult and quite arbitrary to separate FC from other FGDs.
The worldwide prevalence of childhood FC is rising. Studies from the United States have found that 10% of children and adolescents suffer from chronic constipation[24]. Studies from Europe showed prevalence rates ranging from 0.7% in infants and young children in Italy to 15% among children in Greece[25-28]. Although it is commonly believed that constipation is more prevalent in the Western world, recent epidemiological data suggest otherwise. Two studies from Brazil revealed disturbingly high prevalence rates of over 20% of constipation in 1 to 10 year olds[11,29]. Prevalence rates of FC in Ecuador, Colombia, and El Salvador are 11.8%, 13% and 10% respectively[30-32]. More worrying data are emerging from newly developed economies of Asia. In Taiwan, around one third of children in elementary schools suffer from FC[33]. In Hong Kong and South Korea, FC has been reported in 12% to 28% of children, indicating that constipation is also a problem in Asia[34-36]. Similarly, developing nations in Asia, such as Sri Lanka has also noted that 7% to 15% of schoolchildren suffer from FC[37]. These data underscore the magnitude of the disease burden and the public health threat FC poses for the future.
Predisposing factors for constipation are highly prevalent in many parts of the world (Table 2). Psychological stress is a well-established entity that predisposes children to develop FC. In a school-based survey in Sri Lanka, it was noted that home and school related psychological stress predispose children to FC[38]. Inan et al[39], also showed that physical or psychological trauma, siblings with health problems and those with other personal health problems lead to the development of FC. Due to the current competitive lifestyle, circumstances force parents to leave their children with grand-parents, domestic helpers or day care centres for long hours. This may have a negative impact on the development of regular bowel habits and good toilet routines. Furthermore, factors such as spending long periods completing homework and lack of sleep, have also been suggested as possible risk factors in the development of FC in children[34].
| Psychological stress |
| Home related |
| School related |
| Siblings with health problems |
| Not living with either parents |
| Low social class |
| Poor child rearing styles |
| Dietary problems |
| Diet low in fibre |
| Cow’s milk protein |
| Not having regular meals with parents |
| Consumption of junk food |
| Childhood obesity |
| Child maltreatment |
| Physical abuse |
| Sexual abuse |
| Emotional abuse |
| Civil unrest (exposure to war) |
Civil unrest, domestic political disturbances and warfare are known to be associated with FGDs. Internal displacement, hunger, poverty, lack of basic needs including toilet facilities are inevitable consequences of a full scale civil war. In this context, a study from Sri Lanka reported a higher prevalence of FC in children living in war affected zones[40]. Klooker et al[41], also noted that children exposed to the Second World War had a higher tendency to develop IBS as adults. Although the exact mechanisms are not entirely understood, it is possible that under such circumstances, stress mediated alterations of both the brain-gut axis as well as the hypothalamo-pituitary-adrenal axis contribute to the development of abnormal colonic and rectal function, leading to the development of constipation or IBS[42].
A Dutch study showed that older children with parents having high autonomy scores had a considerably lower defecation frequency than children with parents scoring in the reference group. Furthermore, a higher frequency of faecal incontinence was noted when parents scored high on the autonomy scale and self-pity scores[43].
It is well known that dietary factors predispose children to FC. Dietary fibre is in the forefront of this. It is recommended that the diet of children should contain significant amounts of fibre [age (years) + 5 g/d]. Several studies have clearly shown an association between diets low in fibre and the development of FC[26,34,35,39]. Inconsistent data exist regarding the association between cow milk protein allergy and the development of FC[44]. Iacono et al[45] found that 68% of children with FC improved following the elimination of cow’s milk from the diet. All the children developed features of FC when milk was reintroduced. Similarly, the study by Daher et al[46] also suggested an association between an allergy to cow’s milk protein and refractory constipation. However, novel data contradict these findings. When assessing the association between cow’s milk allergy and FC in an unselected population, an Italian study noted that the prevalence of atopy was similar in children with FC and controls and an elimination diet did not help children with FC[47]. Another prospective study, using Rome III criteria to diagnose FC in infants, which assessed the association between cow’s milk allergy and FC, could not recruit adequate numbers from a large paediatric population indicating the lack of association[48]. Restriction of cow’s milk is a common practice in children with FC. However, cow’s milk is a commonly available source of protein and restricting it without proper evidence would deprive children of a balance diet.
Consumption of “fast food”, such as fried ingredients including meat and fish, is becoming an increasingly common practice. It has been shown that consumption of “junk food” is associated with constipation[34]. A Chinese study noted that children and adolescents who consumed fast food items had a higher predilection for FGDs[49]. Lack of physical activity has been shown to be another risk factor for lower defecation frequency and FC[39,50,51].
Obesity is a global pandemic[52]. Data from the Asian subcontinent shows that obesity is alarmingly high[53-55]. Several studies have shown that obesity is associated with FC. It was found in a paediatric gastroenterology clinic, that obesity was a risk factor for the development of FC[56]. Another study from the United States, conducted in a general paediatric clinic, also reported that obese children had a higher predilection for FC[57]. Furthermore, morbidly obese Dutch children had a higher prevalence of constipation[58]. However, a recent community-based study from Colombia found no such association[31].
Child maltreatment is another global social welfare problem. In the developed world, 4%-16% of children are physically abused, 5%-10% are sexually abused and 10% are psychologically deprived or neglected[59]. In the developing world prevalence data are even worse as 83% are psychologically abused and 64% are physically abused[60]. A Sri Lankan study reported an association between physical, psychological or sexual abuse and constipation[61]. In addition, children with constipation and a history of abuse have more severe bowel symptoms and higher somatization scores[61].
Child maltreatment leads to severe psychological stress in the child. Stress may lead to permanent alteration in gastro-intestinal motility, visceral sensitivity, alterations in autonomic function and hypothalamo-pituitary-adrenal dysfunction[62]. Studies in adults have noted that patients with FGDs and a history of abuse have abnormal functional magnetic resonance imaging including activation of the anterior mid-cingulate and posterior cingulate cortex with deactivation of the supra-ungual region of the anterior cingulate cortex[63-66]. These changes could be long-lasting and lead to long-standing suffering, extending into adult life.
A study from Iran showed that mothers of children with constipation have a higher tendency to have similar problems[67]. Another study found that parents (P < 0.0001) and siblings (P = 0.009) of children with constipation have a higher predilection for constipation[68]. However, until now linkage studies, association studies and direct gene sequencing have failed to identify mutations in specific genes associated with FC[69].
The role of psychological and emotional components in the aetiology of FC is a matter of debate. Some argue that emotional problems are the result of FC, while others believe that they play an important role in the aetiology. Using the child behavioural checklist a Dutch study noted that these children had a number of abnormal behavioural traits[70]. Other studies showed that these children do have certain abnormal personality traits and have a higher tendency for anxiety disorders[71,72]. These factors may affect their social and family life in an adverse manner. It has been shown that anxiety is associated with a 184% increase in total medical costs and 348% of in-patient costs when compared to depression which resulted in a 97% increase in total medical costs[8]. Therefore, it is apparent that co-morbid psychiatric conditions lead to higher medical costs, and increased public health repercussions.
However, in many of these patients these behaviour problems are mild and disappear after adequate treatment[70]. Referral to a mental health service may only be useful in patients with social withdrawal, low self-esteem, and depressive behaviour due to their defecation disorder.
As a result of infrequent defecation many of these children suffer faecal incontinence, abdominal pain, anal fissures, enuresis and urinary tract infections. Faecal incontinence (FI) is the result of rectal faecal stasis and is reported in approximately 80% of children with FC[73]. These children smell of faeces which can lead to rejection by peers and teachers at school. This may, directly or indirectly, predispose these children to maltreatment. At home, parents and other family members believe that children may be soiling intentionally to upset others or get attention, because they are stressed or have emotional problems[74]. This may result in anger and aggression towards children with FI and may result in disharmony in the family. Moreover, children with constipation-associated FI have lower self-esteem and poorer quality of life than children with constipation alone[75-77]. The Avon longitudinal study found an array of psychological problems among children with FI including separation and generalized anxiety, social phobias, depression and oppositional defiant disorders[78].
The coexistence of FC and urinary tract disorders, including urinary incontinence, lower urinary tract dysfunction and recurrent urinary tract infection is well established[79]. It has been suggested that rectal distention in the constipated child puts direct pressure on the posterior bladder wall. This pressure is thought to lead to bladder overactivity or mechanical compression of the bladder with trigonal irritation, posterior bladder wall invagination, bladder neck and urethral obstruction or distention[80].
HRQoL is an important concept that incorporates the patient perspectives of illness experience and functional status related to a medical condition. Published studies are consistent in showing impaired HRQoL in adults and children with constipation and is not different from organic diseases such as peptic ulcer disease, inflammatory bowel disease or liver disease[77,81-83]. It is noteworthy that children with constipation and FI have even poorer HRQoL compared to children with constipation alone[77]. Bakker et al[84] illustrated that children with constipation had persistent fatigue with significant school absenteeism. It is important to highlight that impaired school functioning could lead to a vicious cycle of psychological stress due to pressures from school, peers and even parents, aggravating the symptoms of constipation. These factors in turn lead to poor education outcomes in children with constipation.
Many believe that a mild disease like constipation does not affect the family. However, researchers in Milwaukee, United States who interviewed children with constipation and their parents, reported that the parents expressed their feelings as “mad, angry, worried, upset, nervous and embarrassed”[85]. Chinese data on the family impact of chronic constipation, showed that parents of children with FC have poor HRQoL and that constipation had a significant negative impact on parental communication, family functioning, family daily activity and relationships. Parents of children with FC were also noted to have constant worries about their children[86].
Healthcare burden and medical costs of a disease are good indicators which help to understand its public health perspective. Although it is difficult to precisely calculate all direct and indirect medical costs, a large body of literature from the United States has analysed this problem.
In a birth cohort study of young children, Chitkara et al[87] found that medical visits for constipation were the highest among all gastrointestinal diseases. Compared to other common diseases such as childhood asthma and migraine, children with constipation demand and need more medical attention, even as much as 7 times higher than asthma and 3 times higher than migraine[88]. Studying subjects in a birth cohort (5-21 years) in Minnesota, United States, it was found that more children and young adults with constipation visited the emergency department and outpatient clinics, and needed in-ward care compared to controls. Although the estimated inpatient cost is similar, the outpatient cost for children with constipation is higher than controls[8].
In a cross-sectional study using an Expenditure Panel Survey Database, it was noted that children with constipation used more health services than children without constipation. It was estimated that the federal government spent an additional 3.9 billion/year caring for children with constipation[88]. In another study from the United States, Park et al[89] studied the KID database (kids inpatient sample database) which includes discharge patterns from 44 states. The authors noted that the number of children hospitalized with constipation had risen by 112% from 1997 to 2009. In addition, the cost of inpatient care for constipation had increased by 221.5% during the same period without a significant increase in the length of stay in hospital. Corban et al[90] reported the results of a study in which they analysed the national emergency department sample records for emergency room visits for faecal impaction and found a sizeable percentage (10.5%) of children of all age ranges present to emergency units across the United States with faecal impaction.
Similarly, in Australia (Victoria region), the mean annual in-patient cost was 5.5 million dollars for children with constipation as the primary diagnosis[91]. Even though, further data from other countries are needed for a clearer picture, these data indicate that constipation is a costly medical condition and a large percentage of public funds are being spent on children with constipation.
The traditional bio-medical paradigm always demands a linear cause for a particular disease. Therefore, it is common to investigate children with constipation for “organic diseases”. Disorders which are commonly thought to be associated with chronic constipation are hypothyroidism, coeliac disease, hypercalcaemia, lead poisoning, and Hirschsprung disease. Although it has been shown that constipation is an uncommon clinical presentation of hypothyroidism and the majority of patients with hypothyroidism have normal bowel habits, it is still common practice for many clinicians to investigate children for thyroid dysfunction[92].
In a retrospective cohort study, Chogle and Saps[93] studied 7472 children diagnosed with constipation. The numbers screened for coeliac disease, hypothyroidism, hypercalcaemia and lead poisoning were 1731, 2332, 4651 and 3, respectively. The total costs for these tests were 4.7 million United States dollars with a mean charge for investigating one patient of $1014. Only 2 (0.08%) children, diagnosed with hypothyroidism, had constipation as the presenting feature. Twelve of 14 children with hypothyroidism had growth retardation, abdominal pain, vomiting or a combination of these features, in addition to constipation[93]. These facts clearly indicate that the majority of children with organic diseases show other abnormalities during clinical evaluation. Although this study highlighted the money spent on investigating children with FC, it also shows the low prevalence of diseases that most clinicians consider an organic cause of constipation.
The North American and European Societies of Pediatric Gastroenterology, Hepatology and Nutrition guideline and the guideline from the National Institute for Clinical Excellence in the United Kingdom do not recommend routine laboratory testing for hypothyroidism, coeliac disease, and hypercalcaemia and the routine use of abdominal radiography in children with constipation in the absence of alarm symptoms[94,95]. Furthermore these guidelines clearly illustrate that other invasive tests such as rectal biopsy, ano-rectal manometry, and barium studies serve no purpose in the day-to-day clinical management[94]. These tests are costly and incur a substantial drain on the healthcare systems.
The patho-physiological mechanisms underlying constipation are not straightforward and are often entangled in bio-psycho-social factors. In younger children stool withholding due to pain and fear contributes to the development of constipation in at least 50% of cases. In older children, at least in a subset (25%), slow transit constipation was detected[96]. It has been shown that children with slow transit constipation have low levels of vasoactive intestinal peptide and substance P in their colonic musculature[97]. Histological evaluation of colonic specimens from children with slow transit constipation showed abnormalities suggestive of generalized abnormalities in interstitial cells of Cajal, enteric nerves or musculature[98,99]. In addition, poor toilet training, psychological difficulties, child maltreatment and dietary factors may interact with each other in a complex manner, contributing to the development of constipation. This multi-factorial nature leads to an inability to develop a clear biological lead or a marker for constipation.
Methodological aspects of clinical trials of constipation are not satisfactory. In a systematic review, Pijpers et al[100] studied the methodological qualities of currently available clinical trials up to 2008, using the Delphi Guideline. They found methodological shortcomings in the majority of studies including no concealment of treatment allocation (61%), lack of homogeneity in control and treatment arms (71%), no blinding of assessors (57%), and no intention-to-treat analysis (75%). The overall methodological quality score was 4.8 out of a possible maximum of 10 and only 36% of studies had a score of over 6 points[100]. The studies included also had significant variability and poor definition for treatment success. Most of the commonly used drugs such as lactulose, senna and bisacodyl have not been tested in randomised controlled trials in children. Even the clinical studies of newly found popular drugs such as polyethylene glycol cannot be pooled to generate quality evidence as researchers have used a number of different preparations in children (PEG, PEG with electrolytes, etc.).
This poses a major challenge in clinical practice as clinicians struggle to choose drugs. Poor pharmacological interventions lead to inadequate therapeutic response and considerable suffering in children with severe constipation.
In addition, some of the clinical trials conducted in children with constipation using novel therapeutic agents which work well with adults, have shown disappointing results. A recent study on prucalopride in children with constipation showed no efficacy compared to a placebo[101]. It is possible that different pathophysiological mechanisms operate in children with predominant stool withholding, leading to poor efficacy of these drugs in children. No published clinical trials are available to assess the efficacy of other drugs such as lubiprostone and linaclotide which are effective in adults. The public health challenge that both clinicians and researchers are facing is how to encourage further investment from both governments and private partners, on children with constipation, as the results are disappointing from their point of view.
Finally, almost all clinical trials and consensus guidelines on the management of constipation are from the Western hemisphere. This is despite the fact that the dietary patterns, the living and environmental conditions are completely different in many parts of the world and therefore cannot be compared with the Western lifestyle. In addition, there could be genetic variations in the metabolism of drugs that may eventually lead to poor response. Paediatricians and paediatric gastroenterologists, particularly from Asia and Africa, should perform more research in this area and contribute in the understanding of FC in children.
The general belief that FC is self-limiting is not supported by several long-term follow-up studies. A systematic review found that only approximately 50% of all children with constipation followed for 6-12 mo after therapy were doing well without laxatives[102]. Bongers et al[103] followed 401 Dutch children with constipation for more than 10 years and showed that good clinical outcomes, despite intensive treatment strategies, were achieved by only 80% of patients at 16 years of age. In this study, poor long-term clinical outcomes were associated with older age at onset, longer delay between symptom onset and first visit to subspecialty clinic, and lower defecation frequency at study entry. Another study reported that a history of childhood constipation was a predictor of IBS in adulthood[104].
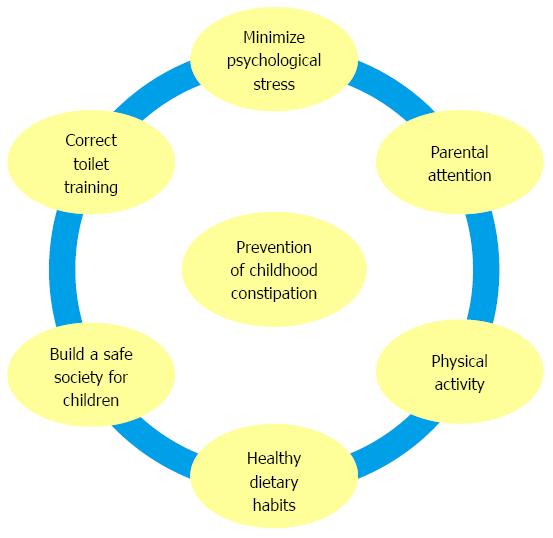
Families should be provided with guidance and recommendations on the prevention, early recognition, and early intervention of constipation in children (Figure 2). Poor toilet training is a well-known cause of constipation in children[105-108]. The presence of hard stools and painful defecation during toilet training could lead to withholding and delay the completion of toilet training[107]. Raising public awareness on proper toilet training is the first step in preventing constipation. Furthermore, training parents and children to have a healthy balanced diet with the recommended amount of fibre and avoiding consumption of “junk food” is another important step[34,94,95]. Lifestyles with proper dietary habits and regular physical activity would help to reduce the risk of constipation[51,95]. It is imperative to understand that, in the current competitive society, parents are forced to work more and spend less time with their children[34]. Parental attention, attachment, correct parenting styles and helping children to develop desirable core lifestyles by setting an example of healthy living, are equally valuable[43]. In addition, relieving psychological stress created by the competitive nature of current schools by providing more educational opportunities for children, caring for them and providing safer pathways in society would be another useful step in preventing and minimizing related suffering due to childhood constipation.
In the last decade, significant progress had been made in understanding the pathophysiology and treatment of childhood constipation. However, more work is needed during the next decade to minimize the public health impact of FC. Prevalence studies performed in rural and non-rural areas, especially in Africa, are lacking and need to be performed to understand the magnitude of the problem and identify risk factors in these parts of the world. Focusing away from the traditional hospital-based interventions, preventive studies using toilet training, training healthcare professionals to recognize the features of constipation early and encouraging correct dietary habits and lifestyle at the community level are needed to identify simpler and pragmatic approaches to prevent childhood constipation. As an alternative to the popular approach of conducting sophisticated investigations and clinical trials in tertiary care centres, clinicians and researchers should perform clinical trials in primary and secondary care settings where most of these children are being cared for. While concentrating on developing novel drugs, older and cheaper drugs such as bisacodyl, senna and lactulose should be evaluated in clinical trials, as these drugs could minimize healthcare expenditure. Clinical trials of new drugs should also be conducted in non-western countries, where the prevalence of constipation is growing and there is possible variation in their response. Clinicians, researchers and public health authorities need to unite in this campaign to prevent the growing global public health problem of childhood functional constipation.
The authors would like to acknowledge Dr. AP Fernando for his contribution to the development of the figures in this article.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Sri Lanka
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Falletto E, Maffei HV, Tosetti C S- Editor: Gong ZM L- Editor: Webster JR E- Editor: Ma S
| 1. | Mugie SM, Benninga MA, Di Lorenzo C. Epidemiology of constipation in children and adults: a systematic review. Best Pract Res Clin Gastroenterol. 2011;25:3-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 665] [Cited by in RCA: 567] [Article Influence: 40.5] [Reference Citation Analysis (0)] |
| 2. | Rajindrajith S, Devanarayana NM, Benninga MA. Defecation disorders in Children: Constipation and functional fecal incontinence. Text Book of Pediatric Gastroenterology, Hepatology, and Nutrition. New York: Springer Science 2015; 234-47. |
| 3. | Kovacic K, Sood MR, Mugie S, Di Lorenzo C, Nurko S, Heinz N, Ponnambalam A, Beesley C, Sanghavi R, Silverman AH. A multicenter study on childhood constipation and fecal incontinence: effects on quality of life. J Pediatr. 2015;166:1482-1487.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 77] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 4. | Bircher J. Towards a dynamic definition of health and disease. Med Health Care Philos. 2005;8:335-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 101] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 5. | Millennium Development Goals Report. Text Book of Pediatric Gastroenterology, Hepatology, and Nutrition. New York: United Nations 2014; 24-27. |
| 6. | Wallace AS, Ryman TK, Dietz V. Overview of global, regional, and national routine vaccination coverage trends and growth patterns from 1980 to 2009: implications for vaccine-preventable disease eradication and elimination initiatives. J Infect Dis. 2014;210 Suppl 1:S514-S522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | van den Berg MM, Benninga MA, Di Lorenzo C. Epidemiology of childhood constipation: a systematic review. Am J Gastroenterol. 2006;101:2401-2409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 416] [Cited by in RCA: 414] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 8. | Choung RS, Shah ND, Chitkara D, Branda ME, Van Tilburg MA, Whitehead WE, Katusic SK, Locke GR, Talley NJ. Direct medical costs of constipation from childhood to early adulthood: a population-based birth cohort study. J Pediatr Gastroenterol Nutr. 2011;52:47-54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 9. | Belsey J, Greenfield S, Candy D, Geraint M. Systematic review: impact of constipation on quality of life in adults and children. Aliment Pharmacol Ther. 2010;31:938-949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 425] [Cited by in RCA: 232] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 10. | Hyams J, Colletti R, Faure C, Gabriel-Martinez E, Maffei HV, Morais MB, Hock QS, Vandenplas Y. Functional gastrointestinal disorders: Working Group Report of the First World Congress of Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr. 2002;35 Suppl 2:S110-S117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 54] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | de Araújo Sant’Anna AM, Calçado AC. Constipation in school-aged children at public schools in Rio de Janeiro, Brazil. J Pediatr Gastroenterol Nutr. 1999;29:190-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 48] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Loening-Baucke V. Modulation of abnormal defecation dynamics by biofeedback treatment in chronically constipated children with encopresis. J Pediatr. 1990;116:214-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 122] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Benninga M, Candy DC, Catto-Smith AG, Clayden G, Loening-Baucke V, Di Lorenzo C, Nurko S, Staiano A. The Paris Consensus on Childhood Constipation Terminology (PACCT) Group. J Pediatr Gastroenterol Nutr. 2005;40:273-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 138] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 14. | Rasquin-Weber A, Hyman PE, Cucchiara S, Fleisher DR, Hyams JS, Milla PJ, Staiano A. Childhood functional gastrointestinal disorders. Gut. 1999;45 Suppl 2:II60-II68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 279] [Cited by in RCA: 291] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 15. | Rasquin A, Di Lorenzo C, Forbes D, Guiraldes E, Hyams JS, Staiano A, Walker LS. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2006;130:1527-1537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1150] [Cited by in RCA: 1077] [Article Influence: 56.7] [Reference Citation Analysis (6)] |
| 16. | Hyams JS, Di Lorenzo C, Saps M, Shulman RJ, Staiano A, van Tilburg M. Functional Disorders: Children and Adolescents. Gastroenterology. 2016; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 809] [Cited by in RCA: 812] [Article Influence: 90.2] [Reference Citation Analysis (5)] |
| 17. | Devanarayana NM, Adhikari C, Pannala W, Rajindrajith S. Prevalence of functional gastrointestinal diseases in a cohort of Sri Lankan adolescents: comparison between Rome II and Rome III criteria. J Trop Pediatr. 2011;57:34-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 101] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 18. | Burgers R, Levin AD, Di Lorenzo C, Dijkgraaf MG, Benninga MA. Functional defecation disorders in children: comparing the Rome II with the Rome III criteria. J Pediatr. 2012;161:615-20.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 19. | Osatakul S, Puetpaiboon A. Use of Rome II versus Rome III criteria for diagnosis of functional constipation in young children. Pediatr Int. 2014;56:83-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | van Tilburg MA, Squires M, Blois-Martin N, Leiby A, Langseder A. Test of the child/adolescent Rome III criteria: agreement with physician diagnosis and daily symptoms. Neurogastroenterol Motil. 2013;25:302-e246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Lea R, Hopkins V, Hastleton J, Houghton LA, Whorwell PJ. Diagnostic criteria for irritable bowel syndrome: utility and applicability in clinical practice. Digestion. 2004;70:210-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Hasosah M, Telmesani A, Al-Binali A, Sarkhi A, Alghamdi S, Alquair K, Alturaiki M, Alanazi A, Alsahafi A, Alzaben A. Knowledge and practice styles of pediatricians in Saudi Arabia regarding childhood constipation. J Pediatr Gastroenterol Nutr. 2013;57:85-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Helgeland H, Flagstad G, Grøtta J, Vandvik PO, Kristensen H, Markestad T. Diagnosing pediatric functional abdominal pain in children (4-15 years old) according to the Rome III Criteria: results from a Norwegian prospective study. J Pediatr Gastroenterol Nutr. 2009;49:309-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 82] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 24. | Wald ER, Di Lorenzo C, Cipriani L, Colborn DK, Burgers R, Wald A. Bowel habits and toilet training in a diverse population of children. J Pediatr Gastroenterol Nutr. 2009;48:294-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 25. | Kiefte-de Jong JC, Escher JC, Arends LR, Jaddoe VW, Hofman A, Raat H, Moll HA. Infant nutritional factors and functional constipation in childhood: the Generation R study. Am J Gastroenterol. 2010;105:940-945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 26. | Roma E, Adamidis D, Nikolara R, Constantopoulos A, Messaritakis J. Diet and chronic constipation in children: the role of fiber. J Pediatr Gastroenterol Nutr. 1999;28:169-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 88] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 27. | Miele E, Simeone D, Marino A, Greco L, Auricchio R, Novek SJ, Staiano A. Functional gastrointestinal disorders in children: an Italian prospective survey. Pediatrics. 2004;114:73-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 121] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 28. | Iacono G, Merolla R, D’Amico D, Bonci E, Cavataio F, Di Prima L, Scalici C, Indinnimeo L, Averna MR, Carroccio A. Gastrointestinal symptoms in infancy: a population-based prospective study. Dig Liver Dis. 2005;37:432-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 120] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 29. | Del Ciampo IR, Galvão LC, Del Ciampo LA, Fernandes MI. [Prevalence of chronic constipation in children at a primary health care unit]. J Pediatr (Rio J). 2002;78:497-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 30. | Játiva E, Velasco-Benítez CA, Koppen IJ, Játiva-Cabezas Z, Saps M. Prevalence of Functional Gastrointestinal Disorders in Schoolchildren in Ecuador. J Pediatr Gastroenterol Nutr. 2016;63:25-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 31. | Koppen IJ, Velasco-Benítez CA, Benninga MA, Di Lorenzo C, Saps M. Is There an Association between Functional Constipation and Excessive Bodyweight in Children? J Pediatr. 2016;171:178-182.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 32. | Zablah R, Velasco-Benítez CA, Merlos I, Bonilla S, Saps M. Prevalence of functional gastrointestinal disorders in school-aged children in El Salvador. Rev Gastroenterol Mex. 2015;80:186-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 33. | Wu TC, Chen LK, Pan WH, Tang RB, Hwang SJ, Wu L, Eugene James F, Chen PH. Constipation in Taiwan elementary school students: a nationwide survey. J Chin Med Assoc. 2011;74:57-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 34. | Tam YH, Li AM, So HK, Shit KY, Pang KK, Wong YS, Tsui SY, Mou JW, Chan KW, Lee KH. Socioenvironmental factors associated with constipation in Hong Kong children and Rome III criteria. J Pediatr Gastroenterol Nutr. 2012;55:56-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 35. | Lee WT, Ip KS, Chan JS, Lui NW, Young BW. Increased prevalence of constipation in pre-school children is attributable to under-consumption of plant foods: A community-based study. J Paediatr Child Health. 2008;44:170-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 61] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 36. | Cho SJ, Ahn YJ, Kim EY, Rho YI, Yang ES, Park YB, Moon KR. The prevalence and associate factors of constipation in the school-aged children. Korean J Pediatr Gastroenterol Nutri. 2003;6:26-32. |
| 37. | Rajindrajith S, Devanarayana NM, Adhikari C, Pannala W, Benninga MA. Constipation in children: an epidemiological study in Sri Lanka using Rome III criteria. Arch Dis Child. 2012;97:43-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 38. | Devanarayana NM, Rajindrajith S. Association between constipation and stressful life events in a cohort of Sri Lankan children and adolescents. J Trop Pediatr. 2010;56:144-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 39. | Inan M, Aydiner CY, Tokuc B, Aksu B, Ayvaz S, Ayhan S, Ceylan T, Basaran UN. Factors associated with childhood constipation. J Paediatr Child Health. 2007;43:700-706. [PubMed] |
| 40. | Rajindrajith S, Mettananda S, Devanarayana NM. Constipation during and after the civil war in Sri Lanka: a paediatric study. J Trop Pediatr. 2011;57:439-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 41. | Klooker TK, Braak B, Painter RC, de Rooij SR, van Elburg RM, van den Wijngaard RM, Roseboom TJ, Boeckxstaens GE. Exposure to severe wartime conditions in early life is associated with an increased risk of irritable bowel syndrome: a population-based cohort study. Am J Gastroenterol. 2009;104:2250-2256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 66] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 42. | Videlock EJ, Adeyemo M, Licudine A, Hirano M, Ohning G, Mayer M, Mayer EA, Chang L. Childhood trauma is associated with hypothalamic-pituitary-adrenal axis responsiveness in irritable bowel syndrome. Gastroenterology. 2009;137:1954-1962. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 159] [Cited by in RCA: 149] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 43. | van Dijk M, de Vries GJ, Last BF, Benninga MA, Grootenhuis MA. Parental child-rearing attitudes are associated with functional constipation in childhood. Arch Dis Child. 2015;100:329-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 44. | Carroccio A, Iacono G. Review article: Chronic constipation and food hypersensitivity--an intriguing relationship. Aliment Pharmacol Ther. 2006;24:1295-1304. [PubMed] |
| 45. | Iacono G, Cavataio F, Montalto G, Florena A, Tumminello M, Soresi M, Notarbartolo A, Carroccio A. Intolerance of cow’s milk and chronic constipation in children. N Engl J Med. 1998;339:1100-1104. [PubMed] |
| 46. | Daher S, Tahan S, Solé D, Naspitz CK, Da Silva Patrício FR, Neto UF, De Morais MB. Cow’s milk protein intolerance and chronic constipation in children. Pediatr Allergy Immunol. 2001;12:339-342. [PubMed] |
| 47. | Simeone D, Miele E, Boccia G, Marino A, Troncone R, Staiano A. Prevalence of atopy in children with chronic constipation. Arch Dis Child. 2008;93:1044-1047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 48. | Bergmann MM, Caubet JC, McLin V, Belli DC, Schäppi MG, Eigenmann PA. Common colic, gastroesophageal reflux and constipation in infants under 6 months of age do not necessitate an allergy work-up. Pediatr Allergy Immunol. 2014;25:410-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 49. | Zhou H, Yao M, Cheng GY, Chen YP, Li DG. Prevalence and associated factors of functional gastrointestinal disorders and bowel habits in Chinese adolescents: a school-based study. J Pediatr Gastroenterol Nutr. 2011;53:168-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 50. | Driessen LM, Kiefte-de Jong JC, Wijtzes A, de Vries SI, Jaddoe VW, Hofman A, Raat H, Moll HA. Preschool physical activity and functional constipation: the Generation R study. J Pediatr Gastroenterol Nutr. 2013;57:768-774. [PubMed] |
| 51. | Chien LY, Liou YM, Chang P. Low defaecation frequency in Taiwanese adolescents: association with dietary intake, physical activity and sedentary behaviour. J Paediatr Child Health. 2011;47:381-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 52. | Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, Gortmaker SL. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378:804-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2895] [Cited by in RCA: 2946] [Article Influence: 210.4] [Reference Citation Analysis (0)] |
| 53. | Jiang XX, Hardy LL, Baur LA, Ding D, Wang L, Shi HJ. High prevalence of overweight and obesity among inner city Chinese children in Shanghai, 2011. Ann Hum Biol. 2014;41:469-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 54. | Bulbul T, Hoque M. Prevalence of childhood obesity and overweight in Bangladesh: findings from a countrywide epidemiological study. BMC Pediatr. 2014;14:86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 55. | Wickramasinghe VP, Arambepola C, Bandara P, Abeysekera M, Kuruppu S, Dilshan P, Dissanayake BS. Distribution of obesity-related metabolic markers among 5-15 year old children from an urban area of Sri Lanka. Ann Hum Biol. 2013;40:168-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 56. | Teitelbaum JE, Sinha P, Micale M, Yeung S, Jaeger J. Obesity is related to multiple functional abdominal diseases. J Pediatr. 2009;154:444-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 57. | Phatak UP, Pashankar DS. Prevalence of functional gastrointestinal disorders in obese and overweight children. Int J Obes (Lond). 2014;38:1324-1327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 58. | vd Baan-Slootweg OH, Liem O, Bekkali N, van Aalderen WM, Rijcken TH, Di Lorenzo C, Benninga MA. Constipation and colonic transit times in children with morbid obesity. J Pediatr Gastroenterol Nutr. 2011;52:442-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 59. | Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373:68-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2388] [Cited by in RCA: 2184] [Article Influence: 136.5] [Reference Citation Analysis (0)] |
| 60. | Akmatov MK. Child abuse in 28 developing and transitional countries--results from the Multiple Indicator Cluster Surveys. Int J Epidemiol. 2011;40:219-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 143] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 61. | Rajindrajith S, Devanarayana NM, Lakmini C, Subasinghe V, de Silva DG, Benninga MA. Association between child maltreatment and constipation: a school-based survey using Rome III criteria. J Pediatr Gastroenterol Nutr. 2014;58:486-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 62. | Chang L. The role of stress on physiologic responses and clinical symptoms in irritable bowel syndrome. Gastroenterology. 2011;140:761-765. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 188] [Cited by in RCA: 182] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 63. | Drossman DA. Abuse, trauma, and GI illness: is there a link? Am J Gastroenterol. 2011;106:14-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 91] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 64. | Ringel Y, Drossman DA, Leserman J, Lin W, Liu H, Voget BA, Whitehead WE. IBS diagnosis and a history of abuse have synergistic effect on the perigenual cingulate activation in response to rectal distention. Gastroenterology. 2003;124:A531. [DOI] [Full Text] |
| 65. | Ringel Y, Drossman DA, Turkington TG, Bradshaw B, Hawk TC, Bangdiwala S, Coleman RE, Whitehead WE. Regional brain activation in response to rectal distension in patients with irritable bowel syndrome and the effect of a history of abuse. Dig Dis Sci. 2003;48:1774-1781. [PubMed] |
| 66. | Ringel Y, Drossman DA, Leserman JL, Suyenobu BY, Wilber K, Lin W, Whitehead WE, Naliboff BD, Berman S, Mayer EA. Effect of abuse history on pain reports and brain responses to aversive visceral stimulation: an FMRI study. Gastroenterology. 2008;134:396-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 110] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 67. | Dehghani SM, Moravej H, Rajaei E, Javaherizadeh H. Evaluation of familial aggregation, vegetable consumption, legumes consumption, and physical activity on functional constipation in families of children with functional constipation versus children without constipation. Prz Gastroenterol. 2015;10:89-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 68. | Ostwani W, Dolan J, Elitsur Y. Familial clustering of habitual constipation: a prospective study in children from West Virginia. J Pediatr Gastroenterol Nutr. 2010;50:287-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 69. | Peeters B, Benninga MA, Hennekam RC. Childhood constipation; an overview of genetic studies and associated syndromes. Best Pract Res Clin Gastroenterol. 2011;25:73-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 70. | Benninga MA, Voskuijl WP, Akkerhuis GW, Taminiau JA, Büller HA. Colonic transit times and behaviour profiles in children with defecation disorders. Arch Dis Child. 2004;89:13-16. [PubMed] |
| 71. | Ranasinghe N, Devanarayana NM, Benninga MA, van Dijk M, Rajindrajith S. Psychological maladjustment and quality of life in adolescents with constipation. Arch Dis Child. 2016; Epub ahead of print. [PubMed] |
| 72. | Waters AM, Schilpzand E, Bell C, Walker LS, Baber K. Functional gastrointestinal symptoms in children with anxiety disorders. J Abnorm Child Psychol. 2013;41:151-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 73. | Rajindrajith S, Devanarayana NM, Benninga MA. Constipation-associated and nonretentive fecal incontinence in children and adolescents: an epidemiological survey in Sri Lanka. J Pediatr Gastroenterol Nutr. 2010;51:472-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 74. | van Tilburg MA, Squires M, Blois-Martin N, Williams C, Benninga MA, Peeters B, Ulshen M. Parental knowledge of fecal incontinence in children. J Pediatr Gastroenterol Nutr. 2012;55:283-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 75. | Bree F, Tillement JP, Sebille B. Propranolol binding to human serum proteins studied by high-performance liquid chromatography. J Chromatogr. 1986;375:416-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 76. | Owens-Stively JA. Self-esteem and compliance in encopretic children. Child Psychiatry Hum Dev. 1987;18:13-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 77. | Rajindrajith S, Devanarayana NM, Weerasooriya L, Hathagoda W, Benninga MA. Quality of life and somatic symptoms in children with constipation: a school-based study. J Pediatr. 2013;163:1069-1072.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 58] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 78. | Joinson C, Heron J, Butler U, von Gontard A. Psychological differences between children with and without soiling problems. Pediatrics. 2006;117:1575-1584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 122] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 79. | Dehghani SM, Basiratnia M, Matin M, Hamidpour L, Haghighat M, Imanieh MH. Urinary tract infection and enuresis in children with chronic functional constipation. Iran J Kidney Dis. 2013;7:363-366. [PubMed] |
| 80. | Burgers RE, Mugie SM, Chase J, Cooper CS, von Gontard A, Rittig CS, Homsy Y, Bauer SB, Benninga MA. Management of functional constipation in children with lower urinary tract symptoms: report from the Standardization Committee of the International Children’s Continence Society. J Urol. 2013;190:29-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 86] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 81. | Youssef NN, Langseder AL, Verga BJ, Mones RL, Rosh JR. Chronic childhood constipation is associated with impaired quality of life: a case-controlled study. J Pediatr Gastroenterol Nutr. 2005;41:56-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 154] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 82. | El-Serag HB, Olden K, Bjorkman D. Health-related quality of life among persons with irritable bowel syndrome: a systematic review. Aliment Pharmacol Ther. 2002;16:1171-1185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 205] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 83. | Clarke MC, Chow CS, Chase JW, Gibb S, Hutson JM, Southwell BR. Quality of life in children with slow transit constipation. J Pediatr Surg. 2008;43:320-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 59] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 84. | Bakker RJ, van de Putte EM, Kuis W, Sinnema G. Risk factors for persistent fatigue with significant school absence in children and adolescents. Pediatrics. 2009;124:e89-e95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 85. | Kaugars AS, Silverman A, Kinservik M, Heinze S, Reinemann L, Sander M, Schneider B, Sood M. Families’ perspectives on the effect of constipation and fecal incontinence on quality of life. J Pediatr Gastroenterol Nutr. 2010;51:747-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 86. | Wang C, Shang L, Zhang Y, Tian J, Wang B, Yang X, Sun L, Du C, Jiang X, Xu Y. Impact of functional constipation on health-related quality of life in preschool children and their families in Xi’an, China. PLoS One. 2013;8:e77273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 87. | Chitkara DK, Camilleri M, Zinsmeister AR, Burton D, El-Youssef M, Freese D, Walker L, Stephens D. Gastric sensory and motor dysfunction in adolescents with functional dyspepsia. J Pediatr. 2005;146:500-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 53] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 88. | Liem O, Harman J, Benninga M, Kelleher K, Mousa H, Di Lorenzo C. Health utilization and cost impact of childhood constipation in the United States. J Pediatr. 2009;154:258-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 200] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 89. | Park R, Mikami S, LeClair J, Bollom A, Lembo C, Sethi S, Lembo A, Jones M, Cheng V, Friedlander E. Inpatient burden of childhood functional GI disorders in the USA: an analysis of national trends in the USA from 1997 to 2009. Neurogastroenterol Motil. 2015;27:684-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 69] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 90. | Corban C, Sommers T, Sengupta N, Jones M, Cheng V, Friedlander E, Bollom A, Lembo A. Fecal Impaction in the Emergency Department: An Analysis of Frequency and Associated Charges in 2011. J Clin Gastroenterol. 2016;50:572-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (2)] |
| 91. | Ansari H, Ansari Z, Lim T, Hutson JM, Southwell BR. Factors relating to hospitalisation and economic burden of paediatric constipation in the state of Victoria, Australia, 2002-2009. J Paediatr Child Health. 2014;50:993-999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 92. | Bennett WE, Heuckeroth RO. Hypothyroidism is a rare cause of isolated constipation. J Pediatr Gastroenterol Nutr. 2012;54:285-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 93. | Chogle A, Saps M. Yield and cost of performing screening tests for constipation in children. Can J Gastroenterol. 2013;27:e35-e38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 94. | Tabbers MM, DiLorenzo C, Berger MY, Faure C, Langendam MW, Nurko S, Staiano A, Vandenplas Y, Benninga MA. Evaluation and treatment of functional constipation in infants and children: evidence-based recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr. 2014;58:258-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 545] [Cited by in RCA: 636] [Article Influence: 57.8] [Reference Citation Analysis (0)] |
| 95. | NICE clinical guideline 99. NICE guideline on constipation in children and young people. May 2010. Available from: https://www.nice.org.uk/guidance/cg99/resources/guidance-constipation-in-childrenand-young-people-pdf. |
| 96. | Benninga MA, Büller HA, Tytgat GN, Akkermans LM, Bossuyt PM, Taminiau JA. Colonic transit time in constipated children: does pediatric slow-transit constipation exist? J Pediatr Gastroenterol Nutr. 1996;23:241-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 97] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 97. | King SK, Sutcliffe JR, Ong SY, Lee M, Koh TL, Wong SQ, Farmer PJ, Peck CJ, Stanton MP, Keck J. Substance P and vasoactive intestinal peptide are reduced in right transverse colon in pediatric slow-transit constipation. Neurogastroenterol Motil. 2010;22:883-92, e234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 98. | van den Berg MM, Di Lorenzo C, Mousa HM, Benninga MA, Boeckxstaens GE, Luquette M. Morphological changes of the enteric nervous system, interstitial cells of cajal, and smooth muscle in children with colonic motility disorders. J Pediatr Gastroenterol Nutr. 2009;48:22-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 99. | Giorgio V, Borrelli O, Smith VV, Rampling D, Köglmeier J, Shah N, Thapar N, Curry J, Lindley KJ. High-resolution colonic manometry accurately predicts colonic neuromuscular pathological phenotype in pediatric slow transit constipation. Neurogastroenterol Motil. 2013;25:70-8.e8-70-8.e9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 100. | Pijpers MA, Tabbers MM, Benninga MA, Berger MY. Currently recommended treatments of childhood constipation are not evidence based: a systematic literature review on the effect of laxative treatment and dietary measures. Arch Dis Child. 2009;94:117-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 67] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 101. | Mugie SM, Korczowski B, Bodi P, Green A, Kerstens R, Ausma J, Ruth M, Levine A, Benninga MA. Prucalopride is no more effective than placebo for children with functional constipation. Gastroenterology. 2014;147:1285-1295.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 71] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 102. | Pijpers MA, Bongers ME, Benninga MA, Berger MY. Functional constipation in children: a systematic review on prognosis and predictive factors. J Pediatr Gastroenterol Nutr. 2010;50:256-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 101] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 103. | Bongers ME, van Wijk MP, Reitsma JB, Benninga MA. Long-term prognosis for childhood constipation: clinical outcomes in adulthood. Pediatrics. 2010;126:e156-e162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 149] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 104. | Khan S, Campo J, Bridge JA, Chiappetta LC, Wald A, di Lorenzo C. Long-term outcome of functional childhood constipation. Dig Dis Sci. 2007;52:64-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (3)] |
| 105. | Blum NJ, Taubman B, Nemeth N. Relationship between age at initiation of toilet training and duration of training: a prospective study. Pediatrics. 2003;111:810-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 77] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 106. | Niemczyk J, Equit M, El Khatib D, von Gontard A. Toilet refusal syndrome in preschool children: do different subtypes exist? J Pediatr Gastroenterol Nutr. 2014;58:303-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 107. | Borowitz SM, Cox DJ, Tam A, Ritterband LM, Sutphen JL, Penberthy JK. Precipitants of constipation during early childhood. J Am Board Fam Pract. 2003;16:213-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 61] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 108. | Blum NJ, Taubman B, Nemeth N. During toilet training, constipation occurs before stool toileting refusal. Pediatrics. 2004;113:e520-e522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 31] [Article Influence: 1.5] [Reference Citation Analysis (0)] |