Published online Jul 7, 2016. doi: 10.3748/wjg.v22.i25.5642
Peer-review started: March 25, 2016
First decision: April 14, 2016
Revised: May 2, 2016
Accepted: May 23, 2016
Article in press: May 23, 2016
Published online: July 7, 2016
Processing time: 101 Days and 21 Hours
Patients with inflammatory bowel disease are known to have a high demand of recurrent evaluation for therapy and disease activity. Further, the risk of developing cancer during the disease progression is increasing from year to year. New, mostly non-radiant, quick to perform and quantitative methods are challenging, conventional endoscopy with biopsy as gold standard. Especially, new physical imaging approaches utilizing light and sound waves have facilitated the development of advanced functional and molecular modalities. Besides these advantages they hold the promise to predict personalized therapeutic responses and to spare frequent invasive procedures. Within this article we highlight their potential for initial diagnosis, assessment of disease activity and surveillance of cancer development in established techniques and recent advances such as wide-view full-spectrum endoscopy, chromoendoscopy, autofluorescence endoscopy, endocytoscopy, confocal laser endoscopy, multiphoton endoscopy, molecular imaging endoscopy, B-mode and Doppler ultrasound, contrast-enhanced ultrasound, ultrasound molecular imaging, and elastography.
Core tip: Patients with inflammatory bowel disease are known to have a high demand of recurrent evaluation for therapy and disease activity. Further, the risk of developing cancer during disease progression is growing from year to year. Especially, new physical imaging approaches utilizing light and sound waves have facilitated the development of endoscopic techniques. Within this article we highlight their potential for initial diagnosis, assessment of disease activity and surveillance of cancer development in established techniques and recent advances such as wide-view full-spectrum endoscopy, chromoendoscopy, autofluorescence endoscopy, endocytoscopy, confocal laser endoscopy, multiphoton endoscopy, molecular imaging endoscopy, B-mode and Doppler ultrasound, contrast-enhanced ultrasound, ultrasound molecular imaging, and elastography.
- Citation: Knieling F, Waldner MJ. Light and sound - emerging imaging techniques for inflammatory bowel disease. World J Gastroenterol 2016; 22(25): 5642-5654
- URL: https://www.wjgnet.com/1007-9327/full/v22/i25/5642.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i25.5642
Inflammatory bowel disease (IBD) is a group of chronic inflammatory diseases seen in 1 of 200 to 500 individuals[1]. The pathophysiology of the two major subtypes, Crohn’s Disease and ulcerative colitis, is still not completely understood[2]. The course of disease is marked by relapses of chronic inflammation and accompanied by severe symptoms, like bloody stool, abdominal pain and weight loss[3]. The assessment of disease extent is still a substantial challenge for clinicians, but it is crucial for successful treatment. The absence of endoscopic activity, e.g., mucosal healing or histologic remission, might even better guarantee long-term success compared to conventional clinical outcome measures[4-6]. Studies demonstrated that higher rates of mucosal healing might be achieved with higher frequency of assessment of endoscopic disease activity and adjustments to medical therapy[7,8]. It is still questionable, if patients adhere to intensive invasive endoscopic procedures[9]. Facing a high economic burden[10] together with globally increasing rates of pediatric IBD[11] raising concerns for potential risks and harmful procedures[12], we urgently need modalities to easily and quickly assess the extent of disease. Furthermore, these modalities need to account and detect precursor lesion in these patients knowing to bear an increasing risk of colitis associated cancer development[13,14]. As light and sound are very different waves in their physical behavior, both can be used to generate new insights into a bright variety of diseases. We provide a review focused on recent imaging advances based on sound and light wave technologies, which are already or are about to be translated into routine clinical use for inflammatory bowel disease.
International consensus guidelines and recommendations for inflammatory bowel disease, including its surveillance and management of dysplasia, point out important aspects concerning imaging are summarized in Table 1[15-18].
| Initial diagnosis and follow-up | Colonoscopy with ileoscopy is recommended for the initial evaluation of inflammatory bowel disease (IBD) and for the differentiation IBD subtypes |
| Sampling of mucosal biopsy specimens from multiple sites during the initial endoscopic evaluation of IBD is recommended | |
| Flexible sigmoidoscopy should be performed in patients with IBD when colonoscopy is contraindicated | |
| Radiological imaging techniques are complementary to endoscopic assessment. Cross-sectional imaging offers the opportunity to detect and stage inflammatory, obstructive and fistulizing Crohn's disease (CD) and is fundamental at first diagnosis to stage disease and to monitor follow-up | |
| Ultrasound (US) is a well-tolerated and radiation-free imaging technique, particularly for the terminal ileum and the colon. Examinations are impaired by gas-filled bowel and by large body habitus | |
| US is able to detect signs of Crohn's disease and has high and comparable diagnostic accuracy at the initial presentation of terminal ileal CD | |
| US can be used to assess disease activity in Crohn's disease of the terminal ileum | |
| US imaging is an adjunct to endoscopy for diagnosis of colonic IBD | |
| Transabdominal US has a high accuracy for assessing the activity and severity of Crohn’s colitis; the performance in UC is less clear; the accuracy of monitoring therapy in colonic Crohn's disease is not well defined | |
| Surveillance and management of dysplasia | It is recommended that all patients with UC or CD colitis undergo a screening colonoscopy 8 yr after disease onset to re-evaluate extent of disease and initiate surveillance for colorectal neoplasia |
| It is recommended to perform surveillance colonoscopy every 1 to 3 yr beginning after 8 yr of disease in patients with UC with macroscopic or histologic evidence of inflammation proximal to and including the sigmoid colon and for patients with Crohn’s colitis with greater than one-third of colon involvement | |
| If white-light colonoscopy is performed in case of surveillance, high definition (HD) is recommended rather than standard definition (SD) | |
| If surveillance is performed with SD colonoscopy, chromoendoscopy is recommended rather than white-light | |
| If performing surveillance with HD colonoscopy, chromoendoscopy is suggested rather than white-light colonoscopy | |
| If performing surveillance with SD colonoscopy, narrow-band imaging (NBI) is not suggested in place of white-light | |
| If performing surveillance with high-definition colonoscopy, NBI is not suggested in place of white-light | |
| If performing surveillance with image-enhanced HD colonoscopy, NBI is not suggested in place of chromoendoscopy | |
| Management of dysplasia discovered on surveillance colonoscopy | After complete removal of endoscopically resectable polypoid dysplastic lesions, surveillance colonoscopy is recommended rather than colectomy |
| After complete removal of endoscopically resectable nonpolypoid dysplastic lesions, surveillance colonoscopy is suggested rather than colectomy | |
| For patients with endoscopically invisible dysplasia (confirmed by a gastrointestinal pathologist), referral is suggested to an endoscopist with expertise in IBD surveillance using chromoendoscopy with high-definition colonoscopy |
Initial diagnosis, follow-up and surveillance are the major keys for clinical management of IBD. Up to now, endoscopy is representing the major backbone to compete in all disciplines. New imaging modalities are lining up to complement this technique with easy applicable, non-invasive and quantitative approaches, to individually improve patients’ care.
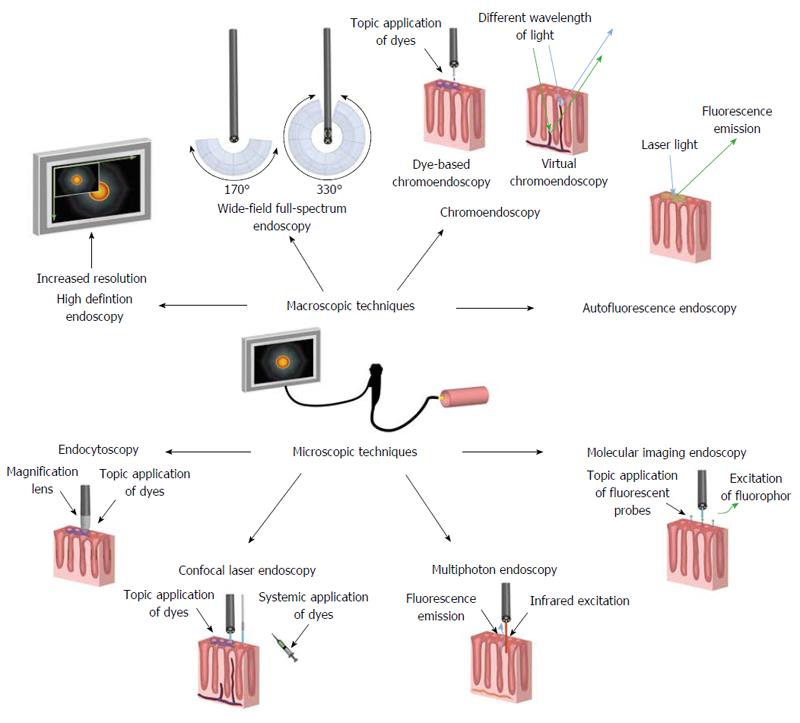
Since the first endoscopy was performed by Kussmaul A in 1868, its technique and application has greatly expanded. Especially during recent years, new technological developments are further improving the diagnostic accuracy for wide-spread (pre-)clinical applications. Some of the most important techniques will be shortly described in this section:
Standard definition (SD) endoscopy offers images in a 4:3 aspect ratio, reaching up to 270000 to 410000 pixels, while high definition (HD) or high resolution endoscopy presents images with 850000 to 1 million pixels. It is clear that high resolution endoscopy results in visualization of a more detailed mucosa[19].
Usually, standard forward-viewing colonoscopes visualize the intestinal surface using an optical system from tip with an angle of view up to 170°. The wide-view full-spectrum endoscopy provides an extended view with a 330° angle. This platform was first tested in an in vitro model, suggesting better detection rates for polyps[20]. Further, its applicability was also verified in small cohorts to show feasibility, performing at a 100% caecal intubation rate and providing high evaluation scores from patients and endoscopists[21].
Chromoendoscopy uses various dyes, endoscopic optical and computer-based software to enhance image quality and to visualize the mucosal architecture. One first approach was reported by Tada et al[22] and since then, different agents for topic application have been approved (methylene blue, toluidine blue, and cresyl violet, indigo carmine, acetic acid, Congo red, phenol red)[23]. By using this technique, an enhancement of the mucosal surface could be achieved to augment superficial patterns and the contrast of pathologic versus normal mucosa[24]. In order to further improve the visualization high-definition resolution was additionally introduced to this technique.
Narrow-band imaging (NBI) or virtual chromoendoscopy, is a comparable software based approach utilizing light of specific wavelength in green and blue spectra to enhance the vascular pattern of the mucosa. As hemoglobin is known to have a peak light absorption at these wavelengths, an optical filtered image can then display the capillaries on the surface and in the submucosa in different colors[25,26].
Depended on the biochemical composition of the visualized tissue, this technique utilizes intensity laser light to induce and generate autofluorescent light spectra[27]. Strong endogenous fluorochromes such as collagen, elastin, nicotinamide adenine dinucleotide (NAD), flavin adenine dinucleotide (FAD), lipofuscin, tryptophan, and keratin can be detected[28]. Most studies used 370 nm excitation light and collected fluorescence in the range 400-700 nm[29,30]. Fluorescence imaging is able to identify suspect lesion with high sensitivity, especially when it is used in the detection of suspect polyps[31,32].
Whereas wide-field endoscopy enables the identification of suspect lesions or inflamed areas of the mucosa during the endoscopic procedure, microscopic evaluation of tissue samples is still required for a definitive diagnosis. As this can delay a definitive treatment up to several days, the development of in vivo endomicroscopic imaging techniques has been one of the major aims of endoscopic research during recent years. Whereas some techniques are already used in clinical practice, others are still in development as subsequently described.
Endocytoscopy (EC) is based on contact light microscopy to the superficial layer of the mucosa. The technology uses fixed-focus and high-power objective lenses[33]. In order to prepare an ideal environment for imaging, washing the surface together with N-acetylcysteine for mucolysis is recommended[34]. EC requires prestaining with absorptive topic agents like the combination of crystal violet and methylene blue[35]. For example, EC was used to examine esophageal tissue to identify superficial esophageal carcinomas[36] or bladder cancer cells[37].
Confocal laser colonoscopy (CLE) is either based on the integration of a confocal laser microscope into the distal tip (ISC-1000/EC3870CIK, Pentax Corporation, Tokyo, Japan) or the utilization of a small probe, which can be introduced through the working channel (Cellvizio, Mauna Kea Technologies, Paris, France). During the procedure, a laser is delivering the excitation light to the surface of the mucosa providing in-vivo histology at a magnification of 1000-fold[38]. As compared to chromoendoscopy, CLE also relies on the topic or systemic application of fluorescence agents[39]. Kiesslich et al[38] demonstrated that this technique may be helpful to avoid repeated colonoscopies, because target lesions could be analyzed more rapidly in vivo during colonoscopy. As a side note: Pentax has already discontinued its product.
Multiphoton microscopy (MPM) has been widely used as an in vivo imaging technique for basic research. In comparison with single photon excitation during confocal microscopy, MPM provides a superior effective resolution in thick tissue samples and an increased penetration depth[40]. Fluorescence imaging is therefore based on the molecular absorption of 2 infrared photons at the same time. First, by generating a second harmonic generation, a nonlinear scattering effect, fibers of collagen-I could be imaged. Second, autofluorescence can be detected from NADH-rich epithelial cells or FAD bearing immune cells. Because this effect is only occurring in a small volume of the focus images could be easily combined to a 3D-image stack[41]. Compared to confocal laser endomicroscopy, this technique is not restricted by the detection of exogenous fluorophores and can easily visualize the subcellular level of gastrointestinal diseases[41]. Until know, there is no MP-endoscope developed for clinical use, but pre-clinical systems have been already described[42].
To further improve the quality of endoscopic imaging, subcellular/molecular information were acquired by adding molecular targeted compounds such as antibodies, peptides or nano particles for specific detection[43]. Liu et al[44] could show that a specific octapeptide conjugated with Cy5.5 excited at 671 nm allowed near infrared (NIR) fluorescence detection at 696 to 736 nm, which was supposed to be specific for colonic adenomas and achieved sub-cellular resolution images. This general concept was also applied to adenomas/polyps, which are known to highly express the signaling molecule VEGF-A, which is supposed to be involved in vascular growth and maturation as well as tumor growth[45,46]. The feasibility to visualize small tumors in real time during colonoscopy could be demonstrated using NIR fluorescence endoscopy[47]. An overview of all described technologies for endoscopic imaging is given in Figure 1.
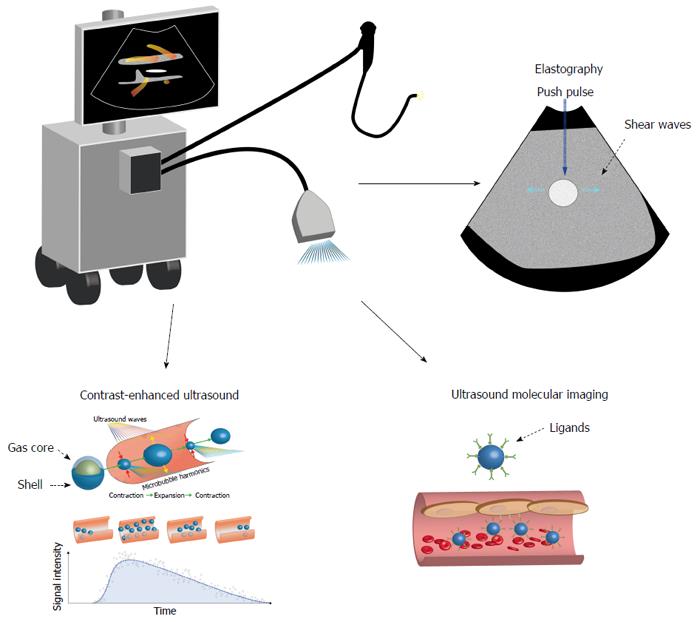
Ultrasound (US) has an important role and great potential in imaging the intestine in children and adults[48]. In some countries, e.g., the United States, it is still far less important than CT imaging, which faces a relative increase of 47.3% from 2007-2010 for non-head application[49]. Compared to US, CT provides the rapid evaluation of bowel and mesentery as well cross-sectional assessment of abdominal and pelvic organs including major vessels[50]. In contrast, US is non-invasive, low cost, easily repeatable and does not rise concerns about radiation exposure in children and young adults[51].
US is a non-invasive, not radiant, and well tolerated modality. The window of imaging is limited by intestinal air or deep organs; therefore, fasting before imaging may be helpful[52]. US for IBD imaging requires the use of high-frequency (5-17 MHz) linear transducers in order to increase spatial resolution and to allow adequate assessment of bowel diameter and of different intestinal layers[53]. Authors recommend a systematic approach to visualize sites of inflammation including the upper and lower, right and left abdominal quadrants[51]. Usually the transabdominal imaging is less invasive, but endoscopic or endosonographic approaches have also been described in pre-clinical[54] and clinical settings[55].
Contrast-enhanced ultrasound utilized gas-filled coated microbubbles to image vascularity. Currently, its major domain is focal liver lesion diagnostics[56] and it is also frequently applied to vascular or cardiac diagnostics[57,58].
Due to its fast liver and renal independent pulmonary clearing, these microbubbles have superior pharmacologic profile in patients with a complicated medical history[59,60]. Diagnostic accuracy[56,61-64], pharmacological safety[65], and cost efficiency in comparison to other conventional imaging modalities[66] has been widely proven. Further, quantitative parameters could be easily derived by secondary software quantification[67,68]. This technique was already applied in the follow-up of anti-vascular treatments in renal cell carcinoma[69], hepatocellular carcinoma[70,71] or cholangiocellular carcinoma[72].
A further evolution of the aforementioned technique is ultrasound molecular imaging (UMI) or targeted molecular ultrasound. Both, CEUS and UMI, have in common that they use small gas-filled microbubbles to image vascularization. Further, UMI contrast agents have coupled a ligand to their outer shell to target specific endothelial molecules of interest[73]. Pre-clinical systems have been applied to detect cancer neovascularization in prostate using VEGFR-2[74] or P- and E-selectins in acute myocardial ischemia[75]. Until now, a clinical translation has not been achieved yet.
Another “contrast-agent-free” modality is ultrasound elastography. It is a non-invasive imaging approach to evaluate tissue hardness[76,77]. A transducer generates forced push pulses to displace targeted tissues at a specified depth. This displacement causes orthogonal shear waves, which can be detected as they propagate through the tissue of interest[77]. The distance traveled by the generated shear and the time provides an estimate of shear wave velocity and tissue hardness (m/s)[78]. The shear wave velocity corresponds to the tissues’ ability to resist deformation and increases with increasing tissue hardness[77]. This has been exemplary studied in liver fibrosis[79], focal liver lesions[80], and thyroid nodules[81]. An overview all described technologies for ultrasound imaging is given in Figure 2.
The identification of distinct patterns of mucosal inflammation has been one part of the initial diagnosis of IBD for decades. Whereas inflammation in Crohn’s disease (CD) presents with aphthous ulcers, cobble stoning, serpiginous ulcers, and the possibility of strictures in the terminal ileum; erythema, edema, bleeding and increased granularity of the colonic mucosa can be observed in UC. Despite these characteristic signs, endoscopy alone does not allow the definitive diagnosis of CD or UC and therefore relies on additional signs in microscopy such as granuloma formation in CD or crypt abscesses in UC. Despite the above-mentioned technological advantages of wide-field endoscopy during recent years, none of these technologies, including the techniques described above, have so far been shown to improve the initial diagnosis of IBD alone. However, first results show some advantage for the additional usage of confocal endomicroscopy. Although limited by its penetration depth, it is capable of visualizing disease-specific microscopic patterns, known from histopathology, to differentiate between UC and CD[82]. Findings in CD showed significantly more discontinuous inflammation, increased focal cryptitis, and discontinuous crypt architectural abnormality compared to UC, which was associated with severe, widespread crypt distortion, decreased crypt density, and frankly irregular surface[82]. In addition to CLE, also EC has been used for the microscopic evaluation of IBD. However, although EC was able to reliably distinguish between single inflammatory cells, it is not clear, whether it can be used for the initial diagnosis and differentiation of IBD subtypes[83]. In conclusion, microscopic endoscopic techniques still lack in clear evidence to be able to visualize distinct disease patterns such as granulomas in CD.
In contrast to the initial diagnosis of IBD, more data are available regarding the use of new endoscopic imaging techniques for monitoring disease activity in IBD patients. Based on a prospective randomized trial, chromoendoscopy showed a higher diagnostic performance to assess the extent and severity of the inflammatory activity in UC when compared to conventional colonoscopy[84]. For NBI, Kudo et al[85] found that mucosal vascular patterns in UC presenting with obscure configuration showed significantly more inflammatory cell infiltrates, increased goblet cell depletion, and basal plasmacytosis. This group also described the key features of different stages of activity in UC imaged with NBI[86]. In a small pilot study the concept of angiogenesis in IBD was also assessed to demonstrate that positive appearance on NBI showed increase in angiogenesis or vessel density[87]. By using the principle of digital post-processing in real-time (virtual chromoendoscopy, i-Scan), inflammatory extent and activity compared with histology showed an overall agreement of 48.71% and 53.85% (white-light) and 92.31% and 89.74% (i-Scan)[88]. Also endomicroscopic techniques have been tested to grade activity in IBD. For instance, CLE is able to provide information equivalent to conventional histology, showing distinct alterations in active and non-active UC patients compared to normal controls[89]. Li et al[90] demonstrated that a classification based on crypt architecture and fluorescein leakage with CLE showed good correlations with histological results in UC. The strong ability of visualizing abnormalities on a cellular level, underling the possibility to assess mucosal healing, was demonstrated by showing distinct vascular and tissue alterations in even endoscopically (magnified) normal appearing colonic mucosa in patients with UC in the state of remission[91].
For CD, a CD Endomicroscopic Activity Score (CDEAS) was proposed, which is consisting of six parameters: crypt number (increased or decreased), crypt distortion, micro erosions, cellular infiltrate, vascularity, and number of goblet cells (increased or decreased)[92]. Interestingly, the authors found a strong correlation of CDEAS and CRP to underline the potential as a disease activity predictor in CD[92]. EC is also capable to visualize different histopathological features. In a pilot trial Neumann et al[92] found a concordance with histopathology for grading intestinal disease activity reaching to 100%[83]. In order to visualize histology in real-time without the use of dies a comparable approach might be achieved with MPM[41]. The implementation into an endoscopic device shall be a helpful to create images of tissue in subcellular resolution[42,93,94]. An overview of selected studies is given in Table 2.
| Ref. | Technique | No. of patients | Findings |
| Kiesslich et al[84], 2003 | CE | 165 | Agreement with histology: 84.5% (72 of 84) vs 60% (49 of 81) |
| Kudo et al[85], 2009 | NBI | 30 | Obscure mucosal vascular pattern is associated with inflammatory cell infiltrates (26% vs 0%), goblet cell depletion (32% vs 5%), and basal plasmacytosis (2% vs 21%) |
| Danese et al[87], 2010 | NBI | 14 | Positive appearance on NBI correlated with increase in angiogenesis or vessel density |
| Neumann et al[88], 2013 | Virtual CE (i-Scan) | 78 | Inflammatory extent and activity accordance with the histological results: 48.71% and 53.85% (white-light) and 92.31% and 89.74% (i-Scan) |
| Watanabe et al[89], 2008 | CLE | 17 | Distinct alterations in active and non-active UC patients compared to histology |
| Li et al[90], 2010 | CLE | 73 | Crypt architecture and fluorescein leakage with CLE correlate with histological results |
| Neumann et al[92], 2012 | CLE | 54 | CDEAS consisting of six parameters: crypt number, crypt distortion, micro erosions, cellular infiltrate, vascularity, and number of goblet cells |
| Strong correlation of CDEAS and CRP |
In addition to monitoring disease activity, CLE techniques have also been used to predict the response to biological therapy in IBD. In a recent pilot study performed by Atreya et al[95], molecular-targeted confocal endomicroscopy prior to the initiation of anti-tumor necrosis factor (TNF) alpha therapy was used to evaluate the subsequent therapeutic response in 25 CD patients. The authors used a topical fluorescent anti-TNF-antibody to visualize membrane-bound TNF[95]. It was shown that patients with high numbers of membrane-bound TNF on inflammatory cells show higher short-term response rates, higher rates of mucosal healing and lower inflammatory scores during anti-TNF-therapy even after one year. This molecular targeted approach demonstrates an ideal example how personalized medicine, including innovative imaging strategies and targeted therapies, could be applied to IBD[6].
One main focus of the majority of new techniques is set to surveillance and detection of dysplasia in IBD. It is very well established that HD endoscopy is superior to SD endoscopy in detecting dysplastic lesions and cancer. In fact, a 3-fold higher detection rate with HD endoscopy was observed when compared to SD endoscopy in IBD[96].
Displaying an ever bigger field of view in high-resolution wide-view full-spectrum endoscopy could perform at an adenoma miss rate significantly lower compared to standard forward-viewing endoscopy: 5/67 (7%) vs 20/49 (41%) (P < 0.0001)[97]. By almost doubling the displayed window and reducing blind corners, this approach might also help to improve visualization of inflammation mucosa and suspects lesions in IBD. However, this approach is also not yet implemented for IBD and the greatest benefit is by now still attributed to chromoendoscopy in the setting of surveillance. In fact, chromoendoscopy allows the discrimination of hyperplastic/non-adenomatous polyps from adenomatous polyps at a sensitivity and specificity of 93% and 95% respectively[98]. A meta-analysis from six trials could show that dye-based chromoendoscopy has medium to high sensitivity and high diagnostic accuracy for detection of dysplastic lesions in UC[99]. This has led to the recommendation that this procedure together with targeted biopsies is preferred as a surveillance procedure in IBD patients in US and European guidelines[100-103].
In contrast, virtual chromoendoscopy (such as NBI) could not show any advantage to standard white-light endoscopy in terms of improved adenoma detection rate, e.g., authors concluded that this technique likely will not contribute to a reduction in adenoma miss rates[25]. On the other hand, NBI may improve pathology diagnosis for diminutive colorectal polyps were 92.8% (95%CI: 90.4%-94.8%) and patients could be already informed of the results at discharge[26]. Comparing this to dye-based techniques, NBI was found to have a lower dysplasia detection rate[15]. This is the reason why dye-based approaches still remain recommend by international guidelines[100-103]. Suspect polyps presented with different characteristics in autofluorescence endoscopy: they showed fluorescence intensity maxima at approximately 460 nm, while normal colon was found to have larger fluorescence intensity compared to adenoma by a factor varying between 2-9 x[29,30]. As demonstrated in patients with Barrett’s esophagus, CLE is highly capable in detecting intraepithelial neoplasia[104] 21741642. This approach combined with chromoendoscopy leads to an increase of 4.75-fold in detecting neoplasias while 50% fewer biopsy specimens (P = 0.008) were required in the colon[105]. As stated for wide-view full-spectrum endoscopy these techniques are not (yet) translated into clinical routine use; especially for patients with IBD.
In contrast to endoscopic imaging techniques, other imaging techniques including CT, MRI, scintigraphy and US are mainly used to evaluate the extend of disease and disease activity in IBD patients. All imaging strategies are based on the identification of distinct morphological characteristics. These include the assessment of mucosal alterations, transmural involvement and extra intestinal manifestations.
So far, no single imaging technique is considered as diagnostic gold standard[51]. Even if MRI seems to perform at a better sensitivity, US is a useful, noninvasive radiation free imaging technique for the initial diagnostic if IBD is suspected[106,107]. If ultrasound is compared to X-ray or endoscopic results by disease localization it shows higher diagnostic performance for inflammatory conditions of the ileum and sigmoid/descending colon than in the rectum, duodenum and proximal jejunum[108]. There are no data published, but it has been estimated that approximately 6 mo and 100 examinations are needed to gain proficiency in performing bowel US[106,109]. A meta-analysis on different modalities for the diagnosis of IBD on a per-patient basis showed high sensitivity and specificity for US, MRI, scintigraphy, and CT as well[110]. In fact, the authors could not show significant differences in diagnostic accuracy among the imaging techniques and concluded that a diagnostic modality without ionizing radiation should be preferred if possible. By measuring the wall thickness and longitudinal extent of pathologically altered bowel segments it was found that US is not strictly associated with clinical activity[111]. In contrast, Limberg demonstrated that assessment with color Doppler/Duplex ultrasonography is helpful and offers a noninvasive and indirect mean of assessing disease activity in intestinal inflammation[112]. Active CD lesions were found to have increased blood flow on preoperative color Doppler US correlating with greater vascularity and numbers of inflammatory leukocytes upon histology[113]. The authors concluded that Doppler US is capable of characterizing the inflammatory activity of CD small-intestinal lesions. The same was shown in children, where mucosal or transmural hypervascularity was not specific and color Doppler sonography could be correlated with different etiological inflammatory bowel processes[114]. Taken away the advantage of being a transabdominal and non-invasive technique, but being closer to the mucosa, ultrasound can also be used to image from inside the body. In this way, endosonography was able to differentiate UC from CD by a sensitivity of 92.3% showing a good correlation with histological inflammation scores (UC: r = 0.43; CD: r = 0.69)[55].
Romanini et al[115] used a quantitative approach after ultrasound contrast application in order to visualize vascular changes and to correlate disease activity with histologic vascular density. The group described cut-off values to distinguish between active and inactive disease, such as peak enhancement (> 40.5%) or regional blood flow (> 54.8 mL/min)[115]. Further, perfusion analysis one month after starting treatment can provide prognostic information regarding treatment efficiency in CD[116]. The major advantage of CEUS is that the use of this technique is already approved so it can already be used.
Furthermore, CEUS can be used for molecular targeted imaging, possibly allowing additional information regarding disease activity. Up to now, molecular approaches are limited to pre-clinical settings. Deshpande et al[117] could show that targeted contrast-enhanced US imaging enables noninvasive in vivo quantification and can be used for monitoring P-selectin expression in mice with induced chemical colitis. As selectins are glycoproteins expressed during the first phase of leukocyte adherence, it seems a favorable marker for detection of early inflammatory processes[118]. Consequently, it has been shown that this approach might be a promising modality for assessing and monitoring active inflammation in IBD[119], both in early and chronic IBD models. The introduction of antibodies targeting α4β7-integrin leukocyte trafficking has now also become a new major target in IBD therapy[120]. That is why this approach seems to be an ideal tool to assess endothelial expression of emerging molecular targets aiming leukocyte trafficking in IBD therapy.
As ongoing inflammation drives intestinal fibrosis[121], ultrasonic electrography might have a valuable role in this scenario. As demonstrated in a rat model elastography, is feasible able to distinguish acutely inflamed from fibrotic intestine[78,122]. This has been translated to human ex vivo tissue[123] and clinical observations[124,125], which found that increased shear wave velocity corresponds to increase in tissue fibrosis and stricturing disease. In a pilot study in children, this modality combined with hydrosonography appears to be able to predict the presence of complications or increased disease activity[126].
In the recent decade the utilization of light and sound waves has greatly expanded in imaging modalities for the evaluation of IBD. Many of them are still waiting to gain entrance into clinical studies and applications. If the focus has been initially set to detection of dysplastic lesions, now new modalities are coming up to also assess initial presentation of the disease or its activity in follow-up. Interestingly, more and more morphological approaches are silently replaced by functional or molecular imaging modalities, which resemble more closely the pathophysiology and therapeutic interventions in IBD.
Manuscript Source: Invited manuscript
Specialty Type: Gastroenterology and Hepatology
Country of Origin: Germany
Peer-Review Report Classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Manguso F, Jarry A S- Editor: Ma YJ L- Editor: A E- Editor: Wang CH
| 1. | Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, Benchimol EI, Panaccione R, Ghosh S, Barkema HW. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46-54.e42; quiz e30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3789] [Cited by in RCA: 3524] [Article Influence: 271.1] [Reference Citation Analysis (5)] |
| 2. | Chidlow JH, Langston W, Greer JJ, Ostanin D, Abdelbaqi M, Houghton J, Senthilkumar A, Shukla D, Mazar AP, Grisham MB. Differential angiogenic regulation of experimental colitis. Am J Pathol. 2006;169:2014-2030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 109] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 3. | Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009;361:2066-2078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1967] [Cited by in RCA: 2198] [Article Influence: 137.4] [Reference Citation Analysis (6)] |
| 4. | Lichtenstein GR, Rutgeerts P. Importance of mucosal healing in ulcerative colitis. Inflamm Bowel Dis. 2010;16:338-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 175] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 5. | Rutgeerts P, Vermeire S, Van Assche G. Mucosal healing in inflammatory bowel disease: impossible ideal or therapeutic target? Gut. 2007;56:453-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 224] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 6. | Neurath MF, Travis SP. Mucosal healing in inflammatory bowel diseases: a systematic review. Gut. 2012;61:1619-1635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 676] [Cited by in RCA: 661] [Article Influence: 50.8] [Reference Citation Analysis (0)] |
| 7. | Bouguen G, Levesque BG, Pola S, Evans E, Sandborn WJ. Endoscopic assessment and treating to target increase the likelihood of mucosal healing in patients with Crohn’s disease. Clin Gastroenterol Hepatol. 2014;12:978-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 102] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 8. | Bouguen G, Levesque BG, Pola S, Evans E, Sandborn WJ. Feasibility of endoscopic assessment and treating to target to achieve mucosal healing in ulcerative colitis. Inflamm Bowel Dis. 2014;20:231-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Rogler G, Vavricka SR, Biedermann L. Integrating Imaging into Clinical Practice in Inflammatory Bowel Disease. Dig Dis. 2015;33 Suppl 1:37-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Benchimol EI, Fortinsky KJ, Gozdyra P, Van den Heuvel M, Van Limbergen J, Griffiths AM. Epidemiology of pediatric inflammatory bowel disease: a systematic review of international trends. Inflamm Bowel Dis. 2011;17:423-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 749] [Cited by in RCA: 711] [Article Influence: 50.8] [Reference Citation Analysis (0)] |
| 11. | Yu AP, Cabanilla LA, Wu EQ, Mulani PM, Chao J. The costs of Crohn’s disease in the United States and other Western countries: a systematic review. Curr Med Res Opin. 2008;24:319-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 149] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 12. | Haas K, Rubesova E, Bass D. Role of imaging in the evaluation of inflammatory bowel disease: How much is too much? World J Radiol. 2016;8:124-131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Bernstein CN, Blanchard JF, Kliewer E, Wajda A. Cancer risk in patients with inflammatory bowel disease: a population-based study. Cancer. 2001;91:854-862. [PubMed] |
| 14. | Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001;48:526-535. [PubMed] |
| 15. | Laine L, Kaltenbach T, Barkun A, McQuaid KR, Subramanian V, Soetikno R. SCENIC international consensus statement on surveillance and management of dysplasia in inflammatory bowel disease. Gastrointest Endosc. 2015;81:489-501.e26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 270] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 16. | Laine L, Kaltenbach T, Barkun A, McQuaid KR, Subramanian V, Soetikno R. SCENIC international consensus statement on surveillance and management of dysplasia in inflammatory bowel disease. Gastroenterology. 2015;148:639-651.e28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 390] [Article Influence: 39.0] [Reference Citation Analysis (0)] |
| 17. | American Society for Gastrointestinal Endoscopy Standards of Practice Committee, Shergill AK, Lightdale JR, Bruining DH, Acosta RD, Chandrasekhara V, Chathadi KV, Decker GA, Early DS, Evans JA, Fanelli RD, Fisher DA, Fonkalsrud L, Foley K, Hwang JH, Jue TL, Khashab MA, Muthusamy VR, Pasha SF, Saltzman JR, Sharaf R, Cash BD, DeWitt JM. The role of endoscopy in inflammatory bowel disease. Gastrointest Endosc. 2015;81:1101-1121.e1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 259] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 18. | Panes J, Bouhnik Y, Reinisch W, Stoker J, Taylor SA, Baumgart DC, Danese S, Halligan S, Marincek B, Matos C. Imaging techniques for assessment of inflammatory bowel disease: joint ECCO and ESGAR evidence-based consensus guidelines. J Crohns Colitis. 2013;7:556-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 539] [Cited by in RCA: 476] [Article Influence: 39.7] [Reference Citation Analysis (0)] |
| 19. | Udagawa T, Minami A, Okada F. Development of magnifying video endoscopes with high resolution. Dig Endosc. 2001;13:163-169. |
| 20. | Gralnek IM, Carr-Locke DL, Segol O, Halpern Z, Siersema PD, Sloyer A, Fenster J, Lewis BS, Santo E, Suissa A. Comparison of standard forward-viewing mode versus ultrawide-viewing mode of a novel colonoscopy platform: a prospective, multicenter study in the detection of simulated polyps in an in vitro colon model (with video). Gastrointest Endosc. 2013;77:472-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 21. | Gralnek IM, Segol O, Suissa A, Siersema PD, Carr-Locke DL, Halpern Z, Santo E, Domanov S. A prospective cohort study evaluating a novel colonoscopy platform featuring full-spectrum endoscopy. Endoscopy. 2013;45:697-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 22. | Tada M, Misaki F, Kawai K. A new approach to the observation of minute changes of the colonic mucosa by means of magnifying colonoscope, type CF-MB-M (Olympus). Gastrointest Endosc. 1978;24:146-147. [PubMed] |
| 23. | Mönkemüller K, Fry LC, Zimmermann L, Mania A, Zabielski M, Jovanovic I. Advanced endoscopic imaging methods for colon neoplasia. Dig Dis. 2010;28:629-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 24. | Wallace MB, Kiesslich R. Advances in endoscopic imaging of colorectal neoplasia. Gastroenterology. 2010;138:2140-2150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 89] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 25. | Adler A, Aschenbeck J, Yenerim T, Mayr M, Aminalai A, Drossel R, Schröder A, Scheel M, Wiedenmann B, Rösch T. Narrow-band versus white-light high definition television endoscopic imaging for screening colonoscopy: a prospective randomized trial. Gastroenterology. 2009;136:410-6.e1; quiz 715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 143] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 26. | Kaltenbach T, Rastogi A, Rouse RV, McQuaid KR, Sato T, Bansal A, Kosek JC, Soetikno R. Real-time optical diagnosis for diminutive colorectal polyps using narrow-band imaging: the VALID randomised clinical trial. Gut. 2015;64:1569-1577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 27. | Kapadia CR, Cutruzzola FW, O’Brien KM, Stetz ML, Enriquez R, Deckelbaum LI. Laser-induced fluorescence spectroscopy of human colonic mucosa. Detection of adenomatous transformation. Gastroenterology. 1990;99:150-157. [PubMed] |
| 28. | Jocham D, Stepp H, Waidelich R. Photodynamic diagnosis in urology: state-of-the-art. Eur Urol. 2008;53:1138-1148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 166] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 29. | Cothren RM, Richards-Kortum R, Sivak MV, Fitzmaurice M, Rava RP, Boyce GA, Doxtader M, Blackman R, Ivanc TB, Hayes GB. Gastrointestinal tissue diagnosis by laser-induced fluorescence spectroscopy at endoscopy. Gastrointest Endosc. 1990;36:105-111. [PubMed] |
| 30. | Cothren RM, Sivak MV, Van Dam J, Petras RE, Fitzmaurice M, Crawford JM, Wu J, Brennan JF, Rava RP, Manoharan R. Detection of dysplasia at colonoscopy using laser-induced fluorescence: a blinded study. Gastrointest Endosc. 1996;44:168-176. [PubMed] |
| 31. | Wang TD, Crawford JM, Feld MS, Wang Y, Itzkan I, Van Dam J. In vivo identification of colonic dysplasia using fluorescence endoscopic imaging. Gastrointest Endosc. 1999;49:447-455. [PubMed] |
| 32. | McCallum AL, Jenkins JT, Gillen D, Molloy RG. Evaluation of autofluorescence colonoscopy for the detection and diagnosis of colonic polyps. Gastrointest Endosc. 2008;68:283-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 33. | ASGE Technology Committee, Kwon RS, Wong Kee Song LM, Adler DG, Conway JD, Diehl DL, Farraye FA, Kantsevoy SV, Kaul V, Kethu SR, Mamula P, Pedrosa MC, Rodriguez SA, Tierney WM. Endocytoscopy. Gastrointest Endosc. 2009;70:610-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 34. | Neumann H, Kudo SE, Kiesslich R, Neurath MF. Advanced colonoscopic imaging using endocytoscopy. Dig Endosc. 2015;27:232-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 35. | Ichimasa K, Kudo SE, Mori Y, Wakamura K, Ikehara N, Kutsukawa M, Takeda K, Misawa M, Kudo T, Miyachi H. Double staining with crystal violet and methylene blue is appropriate for colonic endocytoscopy: an in vivo prospective pilot study. Dig Endosc. 2014;26:403-408. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 36. | Kumagai Y, Monma K, Kawada K. Magnifying chromoendoscopy of the esophagus: in-vivo pathological diagnosis using an endocytoscopy system. Endoscopy. 2004;36:590-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 112] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 37. | Ohigashi T, Kozakai N, Mizuno R, Miyajima A, Murai M. Endocytoscopy: novel endoscopic imaging technology for in-situ observation of bladder cancer cells. J Endourol. 2006;20:698-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 38. | Kiesslich R, Burg J, Vieth M, Gnaendiger J, Enders M, Delaney P, Polglase A, McLaren W, Janell D, Thomas S. Confocal laser endoscopy for diagnosing intraepithelial neoplasias and colorectal cancer in vivo. Gastroenterology. 2004;127:706-713. [PubMed] |
| 39. | Neumann H, Kiesslich R, Wallace MB, Neurath MF. Confocal laser endomicroscopy: technical advances and clinical applications. Gastroenterology. 2010;139:388-92, 392.e1-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 175] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 40. | Zipfel WR, Williams RM, Webb WW. Nonlinear magic: multiphoton microscopy in the biosciences. Nat Biotechnol. 2003;21:1369-1377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2935] [Cited by in RCA: 2274] [Article Influence: 103.4] [Reference Citation Analysis (0)] |
| 41. | Schürmann S, Foersch S, Atreya R, Neumann H, Friedrich O, Neurath MF, Waldner MJ. Label-free imaging of inflammatory bowel disease using multiphoton microscopy. Gastroenterology. 2013;145:514-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 42. | Rivera DR, Brown CM, Ouzounov DG, Pavlova I, Kobat D, Webb WW, Xu C. Compact and flexible raster scanning multiphoton endoscope capable of imaging unstained tissue. Proc Natl Acad Sci USA. 2011;108:17598-17603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 150] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 43. | Goetz M, Wang TD. Molecular imaging in gastrointestinal endoscopy. Gastroenterology. 2010;138:828-33.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 107] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 44. | Liu Z, Miller SJ, Joshi BP, Wang TD. In vivo targeting of colonic dysplasia on fluorescence endoscopy with near-infrared octapeptide. Gut. 2013;62:395-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 45. | Waldner MJ, Wirtz S, Jefremow A, Warntjen M, Neufert C, Atreya R, Becker C, Weigmann B, Vieth M, Rose-John S. VEGF receptor signaling links inflammation and tumorigenesis in colitis-associated cancer. J Exp Med. 2010;207:2855-2868. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 116] [Cited by in RCA: 162] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 46. | Foersch S, Sperka T, Lindner C, Taut A, Rudolph KL, Breier G, Boxberger F, Rau TT, Hartmann A, Stürzl M. VEGFR2 Signaling Prevents Colorectal Cancer Cell Senescence to Promote Tumorigenesis in Mice With Colitis. Gastroenterology. 2015;149:177-189.e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 47. | Tjalma JJ, Garcia-Allende PB, Hartmans E, Terwisscha van Scheltinga AG, Boersma-van Ek W, Glatz J, Koch M, van Herwaarden YJ, Bisseling TM, Nagtegaal ID. Molecular Fluorescence Endoscopy Targeting Vascular Endothelial Growth Factor A for Improved Colorectal Polyp Detection. J Nucl Med. 2016;57:480-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 48. | Jasinski R, Rubin JM, Beezhold C, Aisen A. Ultrasound examination of the colon. J Clin Ultrasound. 1981;9:206-208. [PubMed] |
| 49. | Hussein W, Mullins PM, Alghamdi K, Sarani B, Pines JM. Trends in advanced computed tomography use for injured patients in United States emergency departments: 2007-2010. Acad Emerg Med. 2015;22:663-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 50. | Maturen KE, Wasnik AP, Kamaya A, Dillman JR, Kaza RK, Pandya A, Maheshwary RK. Ultrasound imaging of bowel pathology: technique and keys to diagnosis in the acute abdomen. AJR Am J Roentgenol. 2011;197:W1067-W1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 51. | Strobel D, Goertz RS, Bernatik T. Diagnostics in inflammatory bowel disease: ultrasound. World J Gastroenterol. 2011;17:3192-3197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 43] [Reference Citation Analysis (0)] |
| 52. | Pinto PN, Chojniak R, Cohen MP, Yu LS, Queiroz-Andrade M, Bitencourt AG. Comparison of three types of preparations for abdominal sonography. J Clin Ultrasound. 2011;39:203-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 53. | Nylund K, Hausken T, Gilja OH. Ultrasound and inflammatory bowel disease. Ultrasound Q. 2010;26:3-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 54. | de Britto MA, Soletti RC, Schanaider A, Madi K, de Souza HS, Machado JC. Endoluminal ultrasound biomicroscopy as a reliable tool for in vivo assessment of colonic inflammation in rats. Int J Colorectal Dis. 2013;28:1613-1620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 55. | Ellrichmann M, Wietzke-Braun P, Dhar S, Nikolaus S, Arlt A, Bethge J, Kuehbacher T, Wintermeyer L, Balschun K, Klapper W. Endoscopic ultrasound of the colon for the differentiation of Crohn’s disease and ulcerative colitis in comparison with healthy controls. Aliment Pharmacol Ther. 2014;39:823-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 56. | Strobel D, Seitz K, Blank W, Schuler A, Dietrich C, von Herbay A, Friedrich-Rust M, Kunze G, Becker D, Will U. Contrast-enhanced ultrasound for the characterization of focal liver lesions--diagnostic accuracy in clinical practice (DEGUM multicenter trial). Ultraschall Med. 2008;29:499-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 176] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 57. | Piscaglia F, Nolsøe C, Dietrich CF, Cosgrove DO, Gilja OH, Bachmann Nielsen M, Albrecht T, Barozzi L, Bertolotto M, Catalano O. The EFSUMB Guidelines and Recommendations on the Clinical Practice of Contrast Enhanced Ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med. 2012;33:33-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 721] [Cited by in RCA: 678] [Article Influence: 52.2] [Reference Citation Analysis (0)] |
| 58. | Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsøe CP, Piscaglia F, Wilson SR, Barr RG, Chammas MC. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver--update 2012: a WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultraschall Med. 2013;34:11-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 223] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 59. | Schneider M. SonoVue, a new ultrasound contrast agent. Eur Radiol. 1999;9 Suppl 3:S347-S348. [PubMed] |
| 60. | Morel DR, Schwieger I, Hohn L, Terrettaz J, Llull JB, Cornioley YA, Schneider M. Human pharmacokinetics and safety evaluation of SonoVue, a new contrast agent for ultrasound imaging. Invest Radiol. 2000;35:80-85. [PubMed] |
| 61. | Friedrich-Rust M, Klopffleisch T, Nierhoff J, Herrmann E, Vermehren J, Schneider MD, Zeuzem S, Bojunga J. Contrast-Enhanced Ultrasound for the differentiation of benign and malignant focal liver lesions: a meta-analysis. Liver Int. 2013;33:739-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 93] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 62. | Guang Y, Xie L, Ding H, Cai A, Huang Y. Diagnosis value of focal liver lesions with SonoVue®-enhanced ultrasound compared with contrast-enhanced computed tomography and contrast-enhanced MRI: a meta-analysis. J Cancer Res Clin Oncol. 2011;137:1595-1605. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 63. | Wang C, Yu C, Yang F, Yang G. Diagnostic accuracy of contrast-enhanced ultrasound for renal cell carcinoma: a meta-analysis. Tumour Biol. 2014;35:6343-6350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 64. | D’Onofrio M, Biagioli E, Gerardi C, Canestrini S, Rulli E, Crosara S, De Robertis R, Floriani I. Diagnostic performance of contrast-enhanced ultrasound (CEUS) and contrast-enhanced endoscopic ultrasound (ECEUS) for the differentiation of pancreatic lesions: a systematic review and meta-analysis. Ultraschall Med. 2014;35:515-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 65. | Piscaglia F, Bolondi L; Italian Society for Ultrasound in Medicine and Biology (SIUMB) Study Group on Ultrasound Contrast Agents. The safety of Sonovue in abdominal applications: retrospective analysis of 23188 investigations. Ultrasound Med Biol. 2006;32:1369-1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 596] [Cited by in RCA: 532] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 66. | Westwood M, Joore M, Grutters J, Redekop K, Armstrong N, Lee K, Gloy V, Raatz H, Misso K, Severens J. Contrast-enhanced ultrasound using SonoVue® (sulphur hexafluoride microbubbles) compared with contrast-enhanced computed tomography and contrast-enhanced magnetic resonance imaging for the characterisation of focal liver lesions and detection of liver metastases: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2013;17:1-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 109] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 67. | Girlich C, Jung EM, Iesalnieks I, Schreyer AG, Zorger N, Strauch U, Schacherer D. Quantitative assessment of bowel wall vascularisation in Crohn’s disease with contrast-enhanced ultrasound and perfusion analysis. Clin Hemorheol Microcirc. 2009;43:141-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 68. | Girlich C, Schacherer D, Jung EM, Schreyer A, Büttner R. Comparison between a clinical activity index (Harvey-Bradshaw-Index), laboratory inflammation markers and quantitative assessment of bowel wall vascularization by contrast-enhanced ultrasound in Crohn’s disease. Eur J Radiol. 2012;81:1105-1109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 69. | Lassau N, Koscielny S, Albiges L, Chami L, Benatsou B, Chebil M, Roche A, Escudier BJ. Metastatic renal cell carcinoma treated with sunitinib: early evaluation of treatment response using dynamic contrast-enhanced ultrasonography. Clin Cancer Res. 2010;16:1216-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 137] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 70. | Lassau N, Koscielny S, Chami L, Chebil M, Benatsou B, Roche A, Ducreux M, Malka D, Boige V. Advanced hepatocellular carcinoma: early evaluation of response to bevacizumab therapy at dynamic contrast-enhanced US with quantification--preliminary results. Radiology. 2011;258:291-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 158] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 71. | Knieling F, Waldner MJ, Goertz RS, Zopf S, Wildner D, Neurath MF, Bernatik T, Strobel D. Early response to anti-tumoral treatment in hepatocellular carcinoma--can quantitative contrast-enhanced ultrasound predict outcome? Ultraschall Med. 2013;34:38-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 72. | Wildner D, Pfeifer L, Goertz RS, Bernatik T, Sturm J, Neurath MF, Strobel D. Dynamic contrast-enhanced ultrasound (DCE-US) for the characterization of hepatocellular carcinoma and cholangiocellular carcinoma. Ultraschall Med. 2014;35:522-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 62] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 73. | Lindner JR. Contrast ultrasound molecular imaging of inflammation in cardiovascular disease. Cardiovasc Res. 2009;84:182-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 74. | Tardy I, Pochon S, Theraulaz M, Emmel P, Passantino L, Tranquart F, Schneider M. Ultrasound molecular imaging of VEGFR2 in a rat prostate tumor model using BR55. Invest Radiol. 2010;45:573-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 91] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 75. | Hyvelin JM, Tardy I, Bettinger T, von Wronski M, Costa M, Emmel P, Colevret D, Bussat P, Lassus A, Botteron C. Ultrasound molecular imaging of transient acute myocardial ischemia with a clinically translatable P- and E-selectin targeted contrast agent: correlation with the expression of selectins. Invest Radiol. 2014;49:224-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 76. | Ophir J, Céspedes I, Ponnekanti H, Yazdi Y, Li X. Elastography: a quantitative method for imaging the elasticity of biological tissues. Ultrason Imaging. 1991;13:111-134. [PubMed] |
| 77. | Palmeri ML, Nightingale KR. Acoustic radiation force-based elasticity imaging methods. Interface Focus. 2011;1:553-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 123] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 78. | Dillman JR, Stidham RW, Higgins PD, Moons DS, Johnson LA, Rubin JM. US elastography-derived shear wave velocity helps distinguish acutely inflamed from fibrotic bowel in a Crohn disease animal model. Radiology. 2013;267:757-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 79. | Friedrich-Rust M, Nierhoff J, Lupsor M, Sporea I, Fierbinteanu-Braticevici C, Strobel D, Takahashi H, Yoneda M, Suda T, Zeuzem S. Performance of Acoustic Radiation Force Impulse imaging for the staging of liver fibrosis: a pooled meta-analysis. J Viral Hepat. 2012;19:e212-e219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 355] [Cited by in RCA: 363] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 80. | Park H, Park JY, Kim do Y, Ahn SH, Chon CY, Han KH, Kim SU. Characterization of focal liver masses using acoustic radiation force impulse elastography. World J Gastroenterol. 2013;19:219-226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 46] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 81. | Liu BJ, Li DD, Xu HX, Guo LH, Zhang YF, Xu JM, Liu C, Liu LN, Li XL, Xu XH. Quantitative Shear Wave Velocity Measurement on Acoustic Radiation Force Impulse Elastography for Differential Diagnosis between Benign and Malignant Thyroid Nodules: A Meta-analysis. Ultrasound Med Biol. 2015;41:3035-3043. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 82. | Tontini GE, Mudter J, Vieth M, Atreya R, Günther C, Zopf Y, Wildner D, Kiesslich R, Vecchi M, Neurath MF. Confocal laser endomicroscopy for the differential diagnosis of ulcerative colitis and Crohn’s disease: a pilot study. Endoscopy. 2015;47:437-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 83. | Neumann H, Vieth M, Neurath MF, Atreya R. Endocytoscopy allows accurate in vivo differentiation of mucosal inflammatory cells in IBD: a pilot study. Inflamm Bowel Dis. 2013;19:356-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 84. | Kiesslich R, Fritsch J, Holtmann M, Koehler HH, Stolte M, Kanzler S, Nafe B, Jung M, Galle PR, Neurath MF. Methylene blue-aided chromoendoscopy for the detection of intraepithelial neoplasia and colon cancer in ulcerative colitis. Gastroenterology. 2003;124:880-888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 616] [Cited by in RCA: 557] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 85. | Kudo T, Matsumoto T, Esaki M, Yao T, Iida M. Mucosal vascular pattern in ulcerative colitis: observations using narrow band imaging colonoscopy with special reference to histologic inflammation. Int J Colorectal Dis. 2009;24:495-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 86. | Esaki M, Kubokura N, Kudo T, Matsumoto T. Endoscopic findings under narrow band imaging colonoscopy in ulcerative colitis. Dig Endosc. 2011;23 Suppl 1:140-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 87. | Danese S, Fiorino G, Angelucci E, Vetrano S, Pagano N, Rando G, Spinelli A, Malesci A, Repici A. Narrow-band imaging endoscopy to assess mucosal angiogenesis in inflammatory bowel disease: a pilot study. World J Gastroenterol. 2010;16:2396-2400. [PubMed] |
| 88. | Neumann H, Vieth M, Günther C, Neufert C, Kiesslich R, Grauer M, Atreya R, Neurath MF. Virtual chromoendoscopy for prediction of severity and disease extent in patients with inflammatory bowel disease: a randomized controlled study. Inflamm Bowel Dis. 2013;19:1935-1942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 89. | Watanabe O, Ando T, Maeda O, Hasegawa M, Ishikawa D, Ishiguro K, Ohmiya N, Niwa Y, Goto H. Confocal endomicroscopy in patients with ulcerative colitis. J Gastroenterol Hepatol. 2008;23 Suppl 2:S286-S290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 59] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 90. | Li CQ, Xie XJ, Yu T, Gu XM, Zuo XL, Zhou CJ, Huang WQ, Chen H, Li YQ. Classification of inflammation activity in ulcerative colitis by confocal laser endomicroscopy. Am J Gastroenterol. 2010;105:1391-1396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 119] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 91. | Macé V, Ahluwalia A, Coron E, Le Rhun M, Boureille A, Bossard C, Mosnier JF, Matysiak-Budnik T, Tarnawski AS. Confocal laser endomicroscopy: a new gold standard for the assessment of mucosal healing in ulcerative colitis. J Gastroenterol Hepatol. 2015;30 Suppl 1:85-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 92. | Neumann H, Vieth M, Atreya R, Grauer M, Siebler J, Bernatik T, Neurath MF, Mudter J. Assessment of Crohn’s disease activity by confocal laser endomicroscopy. Inflamm Bowel Dis. 2012;18:2261-2269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 73] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 93. | Myaing MT, MacDonald DJ, Li X. Fiber-optic scanning two-photon fluorescence endoscope. Opt Lett. 2006;31:1076-1078. [PubMed] |
| 94. | Wu Y, Leng Y, Xi J, Li X. Scanning all-fiber-optic endomicroscopy system for 3D nonlinear optical imaging of biological tissues. Opt Express. 2009;17:7907-7915. [PubMed] |
| 95. | Atreya R, Neumann H, Neufert C, Waldner MJ, Billmeier U, Zopf Y, Willma M, App C, Münster T, Kessler H. In vivo imaging using fluorescent antibodies to tumor necrosis factor predicts therapeutic response in Crohn’s disease. Nat Med. 2014;20:313-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 294] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 96. | Subramanian V, Ramappa V, Telakis E, Mannath J, Jawhari AU, Hawkey CJ, Ragunath K. Comparison of high definition with standard white light endoscopy for detection of dysplastic lesions during surveillance colonoscopy in patients with colonic inflammatory bowel disease. Inflamm Bowel Dis. 2013;19:350-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 98] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 97. | Gralnek IM, Siersema PD, Halpern Z, Segol O, Melhem A, Suissa A, Santo E, Sloyer A, Fenster J, Moons LM. Standard forward-viewing colonoscopy versus full-spectrum endoscopy: an international, multicentre, randomised, tandem colonoscopy trial. Lancet Oncol. 2014;15:353-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 171] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 98. | Axelrad AM, Fleischer DE, Geller AJ, Nguyen CC, Lewis JH, Al-Kawas FH, Avigan MI, Montgomery EA, Benjamin SB. High-resolution chromoendoscopy for the diagnosis of diminutive colon polyps: implications for colon cancer screening. Gastroenterology. 1996;110:1253-1258. [PubMed] |
| 99. | Wu L, Li P, Wu J, Cao Y, Gao F. The diagnostic accuracy of chromoendoscopy for dysplasia in ulcerative colitis: meta-analysis of six randomized controlled trials. Colorectal Dis. 2012;14:416-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 100. | Van Assche G, Dignass A, Bokemeyer B, Danese S, Gionchetti P, Moser G, Beaugerie L, Gomollón F, Häuser W, Herrlinger K. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 3: special situations. J Crohns Colitis. 2013;7:1-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 381] [Cited by in RCA: 339] [Article Influence: 28.3] [Reference Citation Analysis (0)] |
| 101. | Farraye FA, Odze RD, Eaden J, Itzkowitz SH, McCabe RP, Dassopoulos T, Lewis JD, Ullman TA, James T, McLeod R. AGA medical position statement on the diagnosis and management of colorectal neoplasia in inflammatory bowel disease. Gastroenterology. 2010;138:738-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 367] [Cited by in RCA: 379] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 102. | Cairns SR, Scholefield JH, Steele RJ, Dunlop MG, Thomas HJ, Evans GD, Eaden JA, Rutter MD, Atkin WP, Saunders BP. Guidelines for colorectal cancer screening and surveillance in moderate and high risk groups (update from 2002). Gut. 2010;59:666-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 897] [Cited by in RCA: 808] [Article Influence: 53.9] [Reference Citation Analysis (2)] |
| 103. | Annese V, Daperno M, Rutter MD, Amiot A, Bossuyt P, East J, Ferrante M, Götz M, Katsanos KH, Kießlich R. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis. 2013;7:982-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 640] [Cited by in RCA: 584] [Article Influence: 48.7] [Reference Citation Analysis (1)] |
| 104. | Sharma P, Meining AR, Coron E, Lightdale CJ, Wolfsen HC, Bansal A, Bajbouj M, Galmiche JP, Abrams JA, Rastogi A. Real-time increased detection of neoplastic tissue in Barrett’s esophagus with probe-based confocal laser endomicroscopy: final results of an international multicenter, prospective, randomized, controlled trial. Gastrointest Endosc. 2011;74:465-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 210] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 105. | Kiesslich R, Goetz M, Lammersdorf K, Schneider C, Burg J, Stolte M, Vieth M, Nafe B, Galle PR, Neurath MF. Chromoscopy-guided endomicroscopy increases the diagnostic yield of intraepithelial neoplasia in ulcerative colitis. Gastroenterology. 2007;132:874-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 383] [Cited by in RCA: 376] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 106. | Calabrese E, Maaser C, Zorzi F, Kannengiesser K, Hanauer SB, Bruining DH, Iacucci M, Maconi G, Novak KL, Panaccione R. Bowel Ultrasonography in the Management of Crohn’s Disease. A Review with Recommendations of an International Panel of Experts. Inflamm Bowel Dis. 2016;22:1168-1183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 127] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 107. | Castiglione F, Mainenti PP, De Palma GD, Testa A, Bucci L, Pesce G, Camera L, Diaferia M, Rea M, Caporaso N. Noninvasive diagnosis of small bowel Crohn’s disease: direct comparison of bowel sonography and magnetic resonance enterography. Inflamm Bowel Dis. 2013;19:991-998. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 108. | Parente F, Greco S, Molteni M, Cucino C, Maconi G, Sampietro GM, Danelli PG, Cristaldi M, Bianco R, Gallus S. Role of early ultrasound in detecting inflammatory intestinal disorders and identifying their anatomical location within the bowel. Aliment Pharmacol Ther. 2003;18:1009-1016. [PubMed] |
| 109. | Condino G, Calabrese E, Zorzi F, Onali S, Lolli E, De Biasio F, Ascolani M, Pallone F, Biancone L. Anti-TNF-alpha treatments and obstructive symptoms in Crohn’s disease: a prospective study. Dig Liver Dis. 2013;45:258-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 110. | Horsthuis K, Bipat S, Bennink RJ, Stoker J. Inflammatory bowel disease diagnosed with US, MR, scintigraphy, and CT: meta-analysis of prospective studies. Radiology. 2008;247:64-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 436] [Cited by in RCA: 431] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 111. | Mayer D, Reinshagen M, Mason RA, Muche R, von Tirpitz C, Eckelt D, Adler G, Beckh K, Kratzer W. Sonographic measurement of thickened bowel wall segments as a quantitative parameter for activity in inflammatory bowel disease. Z Gastroenterol. 2000;38:295-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 112. | Limberg B. [Diagnosis of chronic inflammatory bowel disease by ultrasonography]. Z Gastroenterol. 1999;37:495-508. [PubMed] |
| 113. | Sasaki T, Kunisaki R, Kinoshita H, Kimura H, Kodera T, Nozawa A, Hanzawa A, Shibata N, Yonezawa H, Miyajima E. Doppler ultrasound findings correlate with tissue vascularity and inflammation in surgical pathology specimens from patients with small intestinal Crohn’s disease. BMC Res Notes. 2014;7:363. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (1)] |
| 114. | Quillin SP, Siegel MJ. Gastrointestinal inflammation in children: color Doppler ultrasonography. J Ultrasound Med. 1994;13:751-756. [PubMed] |
| 115. | Romanini L, Passamonti M, Navarria M, Lanzarotto F, Villanacci V, Grazioli L, Calliada F, Maroldi R. Quantitative analysis of contrast-enhanced ultrasonography of the bowel wall can predict disease activity in inflammatory bowel disease. Eur J Radiol. 2014;83:1317-1323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 116. | Saevik F, Nylund K, Hausken T, Ødegaard S, Gilja OH. Bowel perfusion measured with dynamic contrast-enhanced ultrasound predicts treatment outcome in patients with Crohn’s disease. Inflamm Bowel Dis. 2014;20:2029-2037. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 117. | Deshpande N, Lutz AM, Ren Y, Foygel K, Tian L, Schneider M, Pai R, Pasricha PJ, Willmann JK. Quantification and monitoring of inflammation in murine inflammatory bowel disease with targeted contrast-enhanced US. Radiology. 2012;262:172-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 63] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 118. | Vestweber D. How leukocytes cross the vascular endothelium. Nat Rev Immunol. 2015;15:692-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 459] [Cited by in RCA: 599] [Article Influence: 59.9] [Reference Citation Analysis (0)] |
| 119. | Machtaler S, Knieling F, Luong R, Tian L, Willmann JK. Assessment of Inflammation in an Acute on Chronic Model of Inflammatory Bowel Disease with Ultrasound Molecular Imaging. Theranostics. 2015;5:1175-1186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 120. | Sandborn WJ, Feagan BG, Rutgeerts P, Hanauer S, Colombel JF, Sands BE, Lukas M, Fedorak RN, Lee S, Bressler B. Vedolizumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2013;369:711-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1416] [Cited by in RCA: 1564] [Article Influence: 130.3] [Reference Citation Analysis (1)] |
| 121. | Latella G, Di Gregorio J, Flati V, Rieder F, Lawrance IC. Mechanisms of initiation and progression of intestinal fibrosis in IBD. Scand J Gastroenterol. 2015;50:53-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 139] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 122. | Kim K, Johnson LA, Jia C, Joyce JC, Rangwalla S, Higgins PD, Rubin JM. Noninvasive ultrasound elasticity imaging (UEI) of Crohn’s disease: animal model. Ultrasound Med Biol. 2008;34:902-912. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 61] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 123. | Dillman JR, Stidham RW, Higgins PD, Moons DS, Johnson LA, Keshavarzi NR, Rubin JM. Ultrasound shear wave elastography helps discriminate low-grade from high-grade bowel wall fibrosis in ex vivo human intestinal specimens. J Ultrasound Med. 2014;33:2115-2123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 79] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 124. | Baumgart DC, Müller HP, Grittner U, Metzke D, Fischer A, Guckelberger O, Pascher A, Sack I, Vieth M, Rudolph B. US-based Real-time Elastography for the Detection of Fibrotic Gut Tissue in Patients with Stricturing Crohn Disease. Radiology. 2015;275:889-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 96] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 125. | Ishikawa D, Ando T, Watanabe O, Ishiguro K, Maeda O, Miyake N, Nakamura M, Miyahara R, Ohmiya N, Hirooka Y. Images of colonic real-time tissue sonoelastography correlate with those of colonoscopy and may predict response to therapy in patients with ulcerative colitis. BMC Gastroenterol. 2011;11:29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 126. | Fufezan O, Asavoaie C, Tamas A, Farcau D, Serban D. Bowel elastography - a pilot study for developing an elastographic scoring system to evaluate disease activity in pediatric Crohn’s disease. Med Ultrason. 2015;17:422-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |