Published online Jun 14, 2016. doi: 10.3748/wjg.v22.i22.5297
Peer-review started: February 7, 2016
First decision: January 13, 2016
Revised: March 6, 2016
Accepted: April 7, 2016
Article in press: April 7, 2016
Published online: June 14, 2016
Processing time: 178 Days and 14.2 Hours
Development of portal vein tumor thrombus deteriorates the prognosis of hepatocellular carcinoma, while surgical treatment can offer a promising prognosis for selected patients. However, the possibility of residual lesions in portal vein after conventional thrombectomy is a main risk factor leading to postoperative recurrence. Therefore, ensuring the complete removal of tumor thrombus during operation is critical to improve prognosis. For the first time, we report here one case of hepatocellular carcinoma with portal vein tumor thrombus in which cystoscope was successfully applied as a substitute of intravascular endoscope to visualize the cavity of the portal vein. The patient was a 61-year-old man with a 7-cm tumor in the right lobe of the liver, with tumor thrombus invading the right branch and adjacent to the conjunction of the portal vein. After removal of the tumor, the Olympus CYF-VA2 cystoscope was used to check the portal vein from the opening stump of the right branch of the portal vein. In this case, residual thrombus tissue was found near the opening stump and the conjunction of the portal vein. The residual lesion was carefully retrieved from the stump after retraction of the cystoscope. The procedure was repeated until no residual lesion was found. The whole duration time of thrombectomy was 22.5 (15 + 7.5) min. The patient was free from recurrence at 8 months after the procedure. Our work indicated that the cystoscope is a suitable substitute, with a proper size and function to check the portal vein system and ensure the curability of thrombectomy. Although well-designed clinic trails are still needed, this procedure may further improve the postoperative prognosis of hepatocellular carcinoma with portal vein tumor thrombus.
Core tip: Inability to ensure the curability of the thrombectomy has been a main obstacle to improving postoperative prognosis of hepatocellular carcinoma with portal vein tumor thrombus, especially for cases with invasion in the main trunk of the portal vein. In this report, we firstly applied the cystoscope as an intravascular endoscope to investigate the cavity of the portal vein after primary tumor removal. The cystoscope offered a clear view of the portal vein cavity from the main trunk to the secondary branch, indicating its suitability as a substitute with a proper size and function to check the portal vein system.
- Citation: Li N, Wei XB, Cheng SQ. Application of cystoscope in surgical treatment of hepatocellular carcinoma with portal vein tumor thrombus. World J Gastroenterol 2016; 22(22): 5297-5300
- URL: https://www.wjgnet.com/1007-9327/full/v22/i22/5297.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i22.5297
Hepatocellular carcinoma (HCC) has a propensity to invade the intrahepatic vasculature, especially the portal vein system, leading to the formation of portal vein tumor thrombus (PVTT). PVTT is the most important significant factor for a poor prognosis, with a median survival of only 2.7 mo if patients are untreated[1]. Although sorafenib was recommended by the Barcelona Clinic Liver Cancer (BCLC) guideline as the only therapy for these patients, recent studies have demonstrated that surgical resection may offer a more promising prognosis for selected HCC patients with PVTT[2,3].
In the surgical operation, when the PVTT and tumor could not be resected en-bloc, thrombectomy was carried out after the removal of tumor. Theoretically, when thrombectomy was performed, squeezing or fragmenting the tumor thrombus could not be avoided, which would increase the risk of scattering tumor tissue within the portal vein cavity. What’s more, there will be a possibility of residual PVTT tissues adhering to the inner wall of the portal vein even after careful extraction[4-6]. Those factors may lead to the early intrahepatic recurrence of tumor or PVTT[6]. Therefore, ensuring the complete removal of PVTT during operation is critical to improving the prognosis. With the development of endoscopy, it is theoretically ideal to achieve this goal by direct visual observation under intravascular endoscope. However, to the best of our knowledge, there is currently no angioscope specially designed for the portal vein system. Here, we describe one case of an HCC patient with PVTT in which the cystoscope was successfully applied as a substitute to the intravascular endoscope to visualize the cavity of the portal vein.
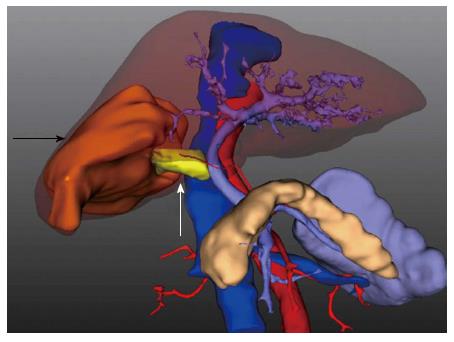
This study was approved by our Institutional Review Board and written informed consent was obtained from the patient for this research. A 61-year-old man with hepatitis B virus infection presented to our department with a 7-cm HCC in the right lobe of the liver, with tumor thrombus that had invaded the right branch and was adjacent to the conjunction of the portal vein. Figure 1 shows a 3D reconstruction of the tumor and PVTT. The patient had Child-Pugh class A liver function and the other laboratory tests were normal. Intraoperative assessment confirmed the preoperative diagnosis. During operation, Pringle’s maneuver was applied distal to the PVTT to occlude the blood inflow using a clamp/unclamp cycle of 15 min/5 min. According to characteristics of the tumor and the PVTT, a right semi-hepatectomy was carried out with a clamp crushing method.
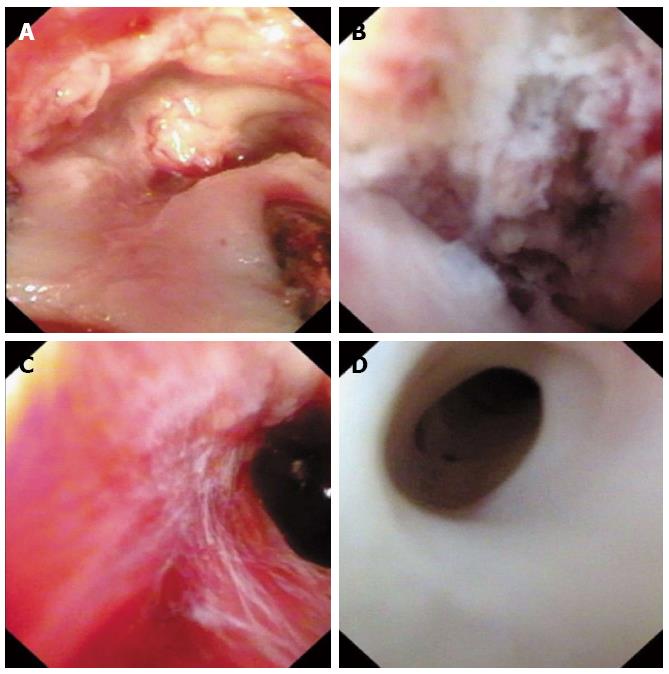
After removal of the tumor, the Olympus CYF-VA2 cystoscope was used to check the portal vein. First, the streamlined tip was inserted into the opening stump on the right branch of the portal vein. The function of flush-and-suction was used to keep the field of view clear. In this case, scattered PVTT tissue was found near the opening stump. Further inspection revealed a residual lesion near the conjunction of the portal vein (Figure 2A and B). Then, the cystoscope was retracted from the stump and the residual PVTT was carefully retrieved using a clamp. After that, the portal vein cavity was reexamined meticulously from the main trunk to the left secondary branch by bending the flexible tip and drawing the insertion tube in and out. The procedure was repeated until no residual lesion was found (Figure 2C and D). Then, the stump was closed using a continuous suture. The whole duration time of the thrombectomy was 22.5 (15 + 7.5) min. The patient was discharged home without complications on postoperative day 7 and was free from recurrence at 8 mo after the procedure when the last follow-up was attended.
Curative resection of tumor and complete removal of PVTT is essential to improve the oncological prognosis of HCC patients with PVTT. For PVTT confined to the ipsilateral branch of the portal vein, en-bloc resection of the ipsilateral portal vein branch containing the tumor thrombus has been recommended, whenever the liver remnant is sufficient[4,7]. However, for patients with PVTT extending to the main portal trunk, or patients with insufficient liver remnant after en-bloc resection, thrombectomy would be inevitably carried out after resection of the primary tumor. Patients who underwent thrombectomy have been reported to have a poor prognosis, with a 6-mo PVTT recurrence rate of 63.8% and the 1-year intrahepatic recurrence rate of 78.8%[4]. For these patients, residual or disseminated tumor thrombus in portal vein may be a significant risk factor leading to the high recurrence rate[6]. Therefore, it is crucial to eliminate the risk of residual thrombus while performing thrombectomy. Fortunately, the portal vein has no blood flow inside during the application of Pringle’s maneuver, allowing the possibility of endoscopic inspection. In this case, the cystoscope we used could view the portal vein cavity clearly from the main trunk to the secondary branch, indicating it is a suitable substitute with a proper size and function to check the portal vein system. Despite the possibility that a microscopic lesion may still exist, this procedure theoretically eliminated the possibility of a residual and scattered macroscopic tumor thrombus in the portal vein and further ensured curability of the thrombectomy. This procedure may further improve the postoperative prognosis of HCC with PVTT. It will also be worthwhile to carry out a well-designed clinical trail to measure the significance of intravascular endoscopy to prove the postoperative prognosis of HCC with PVTT.
A 61-year-old man presented to our department with a 7-cm hepatocellular carcinoma (HCC) in the right lobe of the liver, with tumor thrombus invading the right branch and adjacent to the conjunction of the portal vein.
Using a cystoscope to check the portal vein cavity after removal of the tumor in surgical treatment of HCC with portal vein tumor thrombus (PVTT).
PVTT means “portal vein tumor thrombus”.
The cystoscope we used could view the portal vein cavity clearly from the main trunk to the secondary branch, indicating it is a suitable substitute with a proper size and function to check the portal vein system in the surgical treatment of HCC with PVTT.
This is a novel idea to ensure the curability of hepatectomy for HCC with PVTT. The effectiveness of the treatment will require a well-designed clinical trail to further confirm.
P- Reviewer: Peltec A, Sirin G S- Editor: Qi Y L- Editor: Filipodia E- Editor: Ma S
| 1. | Llovet JM, Bustamante J, Castells A, Vilana R, Ayuso Mdel C, Sala M, Brú C, Rodés J, Bruix J. Natural history of untreated nonsurgical hepatocellular carcinoma: rationale for the design and evaluation of therapeutic trials. Hepatology. 1999;29:62-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 839] [Cited by in RCA: 906] [Article Influence: 34.8] [Reference Citation Analysis (1)] |
| 2. | Shi J, Lai EC, Li N, Guo WX, Xue J, Lau WY, Wu MC, Cheng SQ. Surgical treatment of hepatocellular carcinoma with portal vein tumor thrombus. Ann Surg Oncol. 2010;17:2073-2080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 222] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 3. | Shi J, Lai EC, Li N, Guo WX, Xue J, Lau WY, Wu MC, Cheng SQ. A new classification for hepatocellular carcinoma with portal vein tumor thrombus. J Hepatobiliary Pancreat Sci. 2011;18:74-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 147] [Article Influence: 10.5] [Reference Citation Analysis (1)] |
| 4. | Chen XP, Qiu FZ, Wu ZD, Zhang ZW, Huang ZY, Chen YF, Zhang BX, He SQ, Zhang WG. Effects of location and extension of portal vein tumor thrombus on long-term outcomes of surgical treatment for hepatocellular carcinoma. Ann Surg Oncol. 2006;13:940-946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 110] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 5. | Ikai I, Yamamoto Y, Yamamoto N, Terajima H, Hatano E, Shimahara Y, Yamaoka Y. Results of hepatic resection for hepatocellular carcinoma invading major portal and/or hepatic veins. Surg Oncol Clin N Am. 2003;12:65-75, ix. [PubMed] |
| 6. | Inoue Y, Hasegawa K, Ishizawa T, Aoki T, Sano K, Beck Y, Imamura H, Sugawara Y, Kokudo N, Makuuchi M. Is there any difference in survival according to the portal tumor thrombectomy method in patients with hepatocellular carcinoma? Surgery. 2009;145:9-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 72] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 7. | Chok KS, Cheung TT, Chan SC, Poon RT, Fan ST, Lo CM. Surgical outcomes in hepatocellular carcinoma patients with portal vein tumor thrombosis. World J Surg. 2014;38:490-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 76] [Article Influence: 6.9] [Reference Citation Analysis (0)] |