Published online Apr 14, 2016. doi: 10.3748/wjg.v22.i14.3875
Peer-review started: August 31, 2015
First decision: September 29, 2015
Revised: October 22, 2015
Accepted: December 12, 2015
Article in press: December 14, 2015
Published online: April 14, 2016
Processing time: 213 Days and 21.1 Hours
Gastrointestinal complications are a frequent cause of morbidity after transplantation and may affect up to 40% of kidney transplant recipients. Here we report a rare case of idiopathic giant esophageal ulcer in a kidney transplant recipient. A 37-year-old female presented with a one-week history of odynophagia and weight loss. Upon admission, the patient presented cold sores, and a quantitative cytomegalovirus polymerase chain reaction was positive (105 copies/mL). An upper endoscopy demonstrated the presence of a giant ulcer. Serological test and tissue biopsies were unable to demonstrate an infectious origin of the ulcer. Immunosuppression was reduced and everolimus was introduced. An empirical i.v. therapy with acyclovir was started, resulting in a dramatic improvement in symptoms and complete healing of the ulcer. Only two cases of idiopathic giant esophageal ulcer in kidney transplant recipients have been reported in the literature; in both cases, steroid therapy was successful without recurrence of symptoms or endoscopic findings.
However, this report suggests that correction of immune imbalance is mandatory to treat such a rare complication.
Core tip: Gastrointestinal complications after kidney transplantation are common and may be associated to an increased risk of serious post-transplant morbidity. Giant esophageal ulcers are very rare and the diagnosis of causality is often delayed. This case illustrates the clinical management of an idiopathic giant ulcer, suggesting the possible role of innate immunity imbalance in the pathogenesis of this rare clinical finding.
- Citation: Veroux M, Aprile G, Amore FF, Corona D, Giaquinta A, Veroux P. Rare cause of odynophagia: Giant esophageal ulcer. World J Gastroenterol 2016; 22(14): 3875-3878
- URL: https://www.wjgnet.com/1007-9327/full/v22/i14/3875.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i14.3875
Gastrointestinal (GI) complications are a frequent cause of morbidity after transplantation and may affect up to 40% of kidney transplant recipients[1-3]. Although most patients present with mild symptoms, such as diarrhea, peptic ulcer and oral lesions, these complications may be severe in approximately 10% of patients and may be associated with a doubled risk of graft loss and patient death[1,2]. Idiopathic giant esophageal ulcers in immunocompromised patients have been described more commonly in patients with acquired immunodeficiency syndrome (AIDS)[4,5]. In this report, we present a rare case of idiopathic giant esophageal ulcer in a kidney transplant patient, responding to acyclovir therapy and reduction of immunosuppression.
A 37-year-old female presented with a 1-wk history of severe odynophagia and epigastric pain, worsening after food intake. She had received a deceased donor kidney transplantation 6 mo prior, and the immunosuppressive regimen consisted of tacrolimus, mycophenolic acid and prednisone. Upon admission, the patient presented cold sores, the leucocytes were 1300/mm3, and a quantitative cytomegalovirus (CMV) polymerase chain reaction (PCR) was positive (105 copies/mL). Graft functionality was slightly impaired (Serum creatinine, 2.1 mg/dL).
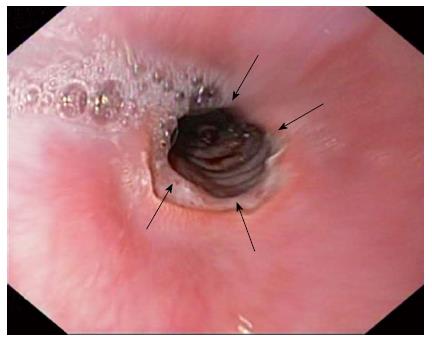
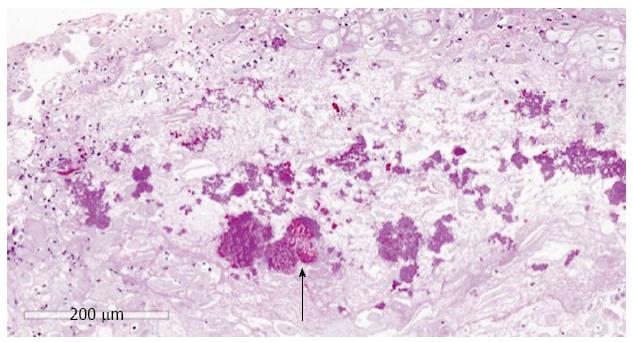
Intravenous ganciclovir therapy (250 mg daily) was immediately started combined with oral acyclovir; mycophenolic acid was discontinued; and tacrolimus was replaced with everolimus, without any beneficial effects. The patient was unable to swallow solid food and lost 8 kg. Upper endoscopy was performed, showing a large ulcer in the distal esophagus measuring 40 mm in diameter (Figure 1). Endoscopic biopsies showed acute inflammation without any viral particles, but with positivity to Candida species (PASD stain) (Figure 2). Her symptoms failed to resolve after two weeks of total parental nutrition, high dose omeprazole (80 mg daily) and fluconazole (200 mg daily). Repeat endoscopy revealed only a slight improvement of the ulcer. Histological examination of biopsy and cytology material for fungal or viral infection was negative, and histochemical studies for CMV, herpes simplex virus (HSV) and adenoviruses were negative and CMV-DNA PCR was negative. Intravenous/empiric therapy with acyclovir (900 mg daily) was started. Her symptoms dramatically improved over 48 h and completely resolved within 10 d, with concomitant partial weight gain (4 kg), and normal leucocytes count (5240/mm3). Repeat endoscopy 10 d after acyclovir treatment revealed near complete resolution of the ulcer (Figure 3). The patient continued oral valganciclovir and acyclovir therapies, without recurrence of symptoms six months after diagnosis and with excellent graft function.
Candida esophagitis is the most common esophageal disorder in renal transplant recipients, and usually occurs in leukopenic or over-immunosuppressed patients within six months after transplantation[1,2]. In most cases, Candida esophagitis is associated with candidal stomatitis and epiglottitis. In general, Candida esophagitis presents with odynophagia, but endoscopic findings are characteristic with multiple small plaques in the upper or mid esophagus. Other causes of esophagitis include CMV or herpes simplex infection. The typical appearance of herpetic esophagitis is represented by multiple vesicular lesions with or without ulcers along the entire esophagus[2]. However, the endoscopic manifestation of herpetic esophagitis may be similar to that of CMV esophagitis, such that diagnosis should be confirmed by cytology, histological examination and viral cultures.
Idiopathic giant ulcers are rarely observed and are more commonly encountered in patients with HIV infection[4,5]. HIV has been observed in ulcer tissue, suggesting that HIV itself could be the direct cause of these lesions[6]. However, it can also be detected in esophageal biopsies from patients with Candida, CMV and HSV esophagitis[5]. Our report and other previous cases[7,8] provide clinical evidence that idiopathic giant esophageal ulcer can occur in the absence of HIV infection, and favor a defect of immunity rather than a virus etiology in the pathogenesis of idiopathic esophageal ulceration[5].
In our report, although the clinical context of the patient suggested a potential CMV-related ulcer, there was no evidence of viral cytopathology as assessed from routine histological or immunohistochemical studies. Furthermore, our patient was on high dose ganciclovir and did not demonstrate any clinical beneficial effect on odynophagia and weight loss because the patient continued to be unable to swallow solid food. Histological finding of fungal infection was most likely related to a direct contamination of the ulcer because there was no evidence of Candida stomatitis or characteristic endoscopic lesions in the esophagus. Moreover, the ulcer failed to improve after a high dose of fluconazole. Histopathological features cannot distinguish idiopathic ulceration from gastroesophageal reflux disease, but the patient presented no endoscopic appearance to suggest reflux disease and her symptoms and esophageal ulceration failed to improve to high dose omeprazole and total parental nutrition. Although the clinical finding of cold sores and the dramatic temporal response to high-dose acyclovir therapy may suggest a herpetic origin for the giant ulcer, we were unable to demonstrate the presence of viral particles using histological or immunohistochemical studies, and routine serological tests for HSV were negative.
There have only been two reports of idiopathic giant esophageal ulcer in kidney transplant recipients[6,7], and both patients were previously subjected to over-immunosuppression to prevent acute rejection episodes. In both cases, steroid therapy was successful without recurrence of symptoms or endoscopic findings. The response to idiopathic esophageal ulcer to steroids is clearly documented in AIDS, with a clinical remission observed in more than 90% of cases[9]. The prednisone regimen consists of 40 mg/d, tapering 10 mg/wk for a 1-mo treatment course. The relapse rate for esophageal ulcers in AIDS treated with steroids is approximately 40%, but retreatment is usually successful.
Leucopenia has been shown to be involved in the pathogenesis of giant ulcer in a kidney transplant recipient[7] as a result of overimmunosuppression. Our report provides the first clinical experience that a combination of reduction in immunosuppression and high-dose of acyclovir may result in a normalization of leucopenia and correction of immune imbalance, leading to rapid healing of the ulcer and a resolution of symptoms.
In conclusion, giant esophageal ulcers are uncommon in kidney transplant recipients and the diagnosis of causality is often delayed. Treatment is often empirical and the aggressive nature of the disease may result in erroneous treatment decision, leading to higher patient morbidity.
The correction of the immune imbalance found in these patients plays a key role in the management of giant esophageal ulcer.
A 37-year-old kidney transplant recipient presented with a 1-wk history of severe odynophagia and epigastric pain, which worsened after food intake.
Cold sores, odynophagia and an inability to swallow solid food.
Candida esophagitis, cytomegalovirus (CMV) or herpes simplex virus esophagitis, esophageal cancer, and gastric cancer.
Leucocytes 1300/mm3, and quantitative CMV-DNA polymerase chain reaction positive (105 copies/mL). Slight increase in serum creatinine (2.1 mg/dL).
Upper endoscopy showed a large ulcer in the distal esophagus measuring 40 mm in diameter.
Acute esophageal inflammation without any viral particles, but with positivity to Candida species.
Reduction of immunosuppression and intravenous/empiric therapy with acyclovir.
Idiopathic giant esophageal ulcer is very uncommon in kidney transplant recipients and it is usually related to over-immunosuppression. Treatment with high-dose steroids might result in complete healing of the ulcer.
Giant idiopathic esophageal ulcer is a rare complication of an immunosuppressed patient, which is related to a defect in immunity rather than a virus etiology in its pathogenesis.
Giant idiopathic esophageal ulcer may be commonly confused for a neoplastic lesion of the esophagus. Treatment is often empirical, but correction of the immune imbalance is mandatory.
This is an interesting case report. Farrell et al reported previously the first case of giant esophageal ulceration responsive to steroids in an immunosuppressed human immunodeficiency virus negative patient. It’s well written and acceptable for publication.
P- Reviewer: Tarnawski A S- Editor: Gong ZM L- Editor: A E- Editor: Ma S
| 1. | Ponticelli C, Passerini P. Gastrointestinal complications in renal transplant recipients. Transpl Int. 2005;18:643-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Gautam A. Gastrointestinal complications following transplantation. Surg Clin North Am. 2006;86:1195-1206, vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Veroux M, Grosso G, Ekser B, Corona D, Giaquinta A, Veroux P. Impact of conversion to a once daily tacrolimus-based regimen in kidney transplant recipients with gastrointestinal complications. Transplantation. 2012;93:895-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Dragean CA, Bogdan I, Azzouzzi K, Goncette L. Giant idiopathic ulcer of esophagus in the context of acquired immunodeficiency syndrome (AIDS). JBR-BTR. 2013;96:72-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Siegmund B, Moos V, Loddenkemper C, Wahnschaffe U, Engelmann E, Zeitz M, Schneider T. Esophageal giant ulcer in primary human immunodeficiency virus infection is associated with an infiltration of activated T cells. Scand J Gastroenterol. 2007;42:890-895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Wilcox CM, Zaki SR, Coffield LM, Greer PW, Schwartz DA. Evaluation of idiopathic esophageal ulceration for human immunodeficiency virus. Mod Pathol. 1995;8:568-572. [PubMed] |
| 7. | Farrell JJ, Cosimi AB, Chung RT. Idiopathic giant esophageal ulcers in a renal transplant patient responsive to steroid therapy. Transplantation. 2000;70:230-232. [PubMed] |
| 8. | van Boekel GA, Volbeda M, van den Hoogen MW, Hilbrands LB, Berden JH. Idiopathic giant oesophageal ulcer and leucopoenia after renal transplantation. Neth J Med. 2012;70:370-373. [PubMed] |
| 9. | Wilcox CM, Schwartz DA, Clark WS. Esophageal ulceration in human immunodeficiency virus infection. Causes, response to therapy, and long-term outcome. Ann Intern Med. 1995;123:143-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 139] [Article Influence: 4.6] [Reference Citation Analysis (0)] |