Published online Mar 7, 2015. doi: 10.3748/wjg.v21.i9.2858
Peer-review started: September 13, 2014
First decision: September 27, 2014
Revised: September 30, 2014
Accepted: November 7, 2014
Article in press: November 11, 2014
Published online: March 7, 2015
Processing time: 177 Days and 14.5 Hours
A 65-year-old woman with Budd-Chiari syndrome (BCS) presented with right upper quadrant pain. A computed tomography (CT) scan showed a saccular aneurysm located at the extrahepatic portal vein main branch measuring 3.2 cm in height and 2.5 cm × 2.4 cm in diameter. The aneurysm was thought to be associated with BCS as there was no preceding history of trauma and it had not been present on Doppler ultrasound examination performed 3 years previously. Because of increasing pain and concern for complications due to aneurysm size, the decision was made to relieve the hepatic venous outflow obstruction. Transjugular intrahepatic portosystemic shunt (TIPS) was created without complications. She had complete resolution of her abdominal pain within 2 d and remained asymptomatic after 1 year of follow-up. CT scans obtained after TIPS showed that the aneurysm had decreased in size to 2.4 cm in height and 2.0 cm × 1.9 cm in diameter at 3 mo, and had further decreased to 1.9 cm in height and 1.6 cm × 1.5 cm in diameter at 1 year.
Core tip: Portal vein aneurysm (PVA) is a rare clinical entity defined as abnormal dilation of the portal vein ≥ 2 cm in diameter. Observation is advocated for asymptomatic aneurysms, whereas symptomatic and enlarging aneurysms are recommended for surgery. To date, the utility of transjugular intrahepatic portosystemic shunt (TIPS) for the treatment of PVA has not been described. Herein, we report a case of extrahepatic PVA in a patient with Budd-Chiari syndrome treated with a TIPS.
- Citation: Tsauo J, Li X. Portal vein aneurysm associated with Budd-Chiari syndrome treated with transjugular intrahepatic portosystemic shunt: A case report. World J Gastroenterol 2015; 21(9): 2858-2861
- URL: https://www.wjgnet.com/1007-9327/full/v21/i9/2858.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i9.2858
Portal vein aneurysm (PVA) is a rare clinical entity defined as abnormal dilation of the portal vein ≥ 2 cm in diameter[1]. Since the first report by Barzilai and Kleckner[2] in 1956, < 200 cases have been reported in the literature. Clinical manifestations include abdominal pain, incidental detection, gastrointestinal bleeding, and jaundice[3]. One-third of patients present with complications, including mural thrombosis, compression of adjacent organs, and rupture[3]. Observation is advocated for asymptomatic aneurysms, whereas symptomatic and enlarging aneurysms are recommended for surgery[3]. Aneurysmorrhaphy is the standard treatment of choice; however, portacaval shunt is suggested in the context of portal hypertension due to the high risk of bleeding from direct approach to the aneurysm[4]. Through reduction of portal hypertension and diversion of blood flow away from the aneurysm, portacaval shunt achieved good clinical results in six previously reported cases[3]. Nonetheless, this operation has largely been abandoned since the advent of transjugular intrahepatic portosystemic shunt (TIPS)[5]. To the best of our knowledge, the utility of TIPS for the treatment of PVA has not been described. Herein, we report a case of extrahepatic PVA in a patient with Budd-Chiari syndrome (BCS) treated with a TIPS. A consent has been waived by the Institutional Review Board for the publication of this case report.
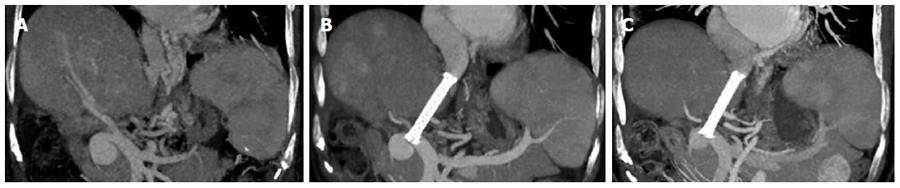
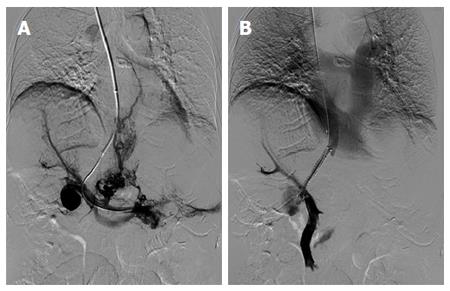
A 65-year-old woman presented with a complaint of right upper quadrant pain. Three years prior, the patient was incidentally diagnosed with idiopathic BCS during health checkup; Doppler ultrasound (US) examination showed obstruction of the middle and left hepatic veins, and investigations for underlying thrombophilia were unremarkable. She was treated with warfarin to maintain an international normalized ratio between 2 and 3, but discontinued after at least 1 year due to non-compliance; the patient did not consult with any doctors for 2 years. She has remained asymptomatic for the past 3 years until recently she started experiencing steadily worsening, intermittent pain in the right upper quadrant of her abdomen, with no associated or alleviating factors. Physical examination was only notable for mild right upper quadrant tenderness. Laboratory tests revealed mildly elevated bilirubin (2.2 mg/dL) and albumin deficit (2.38 g/dL). Her Child-Pugh (CP) score was 8, Model for End-Stage Liver Disease (MELD) score was 11, Rotterdam score was 0.15, and BCS-TIPS prognostic index (BCS-TIPS PI) score was 6.3. A contrast-enhanced computed tomography (CT) scan showed non-visualized middle and left hepatic veins, hepatomegaly with hypertrophy of the caudate lobe, splenomegaly, hepatic venous collaterals, and a saccular aneurysm located at the extrahepatic portal vein main branch measuring 3.2 cm in height and 2.5 cm × 2.4 cm in diameter (Figure 1A). The aneurysm was thought to be associated with BCS as there was no preceding history of trauma and it had not been present on Doppler US examination performed 3 years previously. Although the patient had no ascites or variceal bleeding, the decision was made to create a TIPS to relieve hepatic venous outflow obstruction because of increasing pain and concern for complications due to aneurysm size; direct approach to the aneurysm was not considered due to risk of associated complications in the setting of portal hypertension, and stent-grafting was not considered due to concerns about patency in the settings of hepatic venous outflow obstruction and underlying thrombophilia. After informed consent was obtained, the patient was brought to the interventional radiology suite. The procedure was performed with the patient under conscious sedation. Portal vein access was obtained via the right hepatic vein under fluoroscopy, and portography showed a saccular aneurysm located at the main portal vein, extensive intrahepatic portal vein thrombosis, and small splenorenal varices (Figure 2A). A 10-mm diameter expanded polytetrafluoroethylene (ePTFE) covered stent-graft (Fluency Plus; Bard Peripheral Vascular, Tempe, Arizona, United States) was deployed across the liver parenchymal tract; deploying the stent-graft into the main portal vein trunk to cover the aneurysm neck was not considered because it would obstruct blood flow to the portal vein branches. Completion portography showed a widely patent shunt and markedly decreased aneurysm filling (Figure 2B). The portosystemic pressure gradient (PPG) was decreased from 19 mmHg to 8 mmHg. The patient recovered uneventfully and had complete resolution of her abdominal pain in 2 d. She was discharged on long-term warfarin and remained asymptomatic after 1 year of follow-up. Most recent laboratory tests revealed normal liver function, and Doppler US examination performed at 1, 3, 6, and 12 mo postprocedure confirmed a patent shunt. Her CP score was 5, MELD score was 8, Rotterdam score was 0.12, and TIPS-BCS PI score was 6.1. CT scans showed that the aneurysm had decreased in size to 2.4 cm in height and 2.0 cm × 1.9 cm in diameter at 3 mo after TIPS (Figure 1B), and had further decreased to 1.9 cm in height and 1.6 cm × 1.5 cm in diameter at 1 year (Figure 1C).
BCS is a rare condition characterized by hepatic venous outflow obstruction anywhere between the small hepatic veins and the supra-hepatic inferior vena cava. Clinical manifestations range widely from asymptomatic to liver failure, but most patients present with symptoms related to portal hypertension[6]. Management follows a step-wise strategy, with medical therapy as first-line treatment, angioplasty/stenting as second-line, TIPS as third-line, and liver transplantation as last resort[6]. However, there is controversy as to whether anticipating TIPS in symptomatic patients, before no response to medical therapy appears, could slow disease progression and improve survival[7]. Nonetheless, it is widely recognized that asymptomatic patients should not undergo invasive treatments, because they could remain asymptomatic for an extended period of time owing to development of hepatic venous collaterals[6]. As such, if it had not been for the presence of PVA, our patient would not have required a TIPS.
Although the widespread use of imaging techniques have led to an increase in the number of PVA being discovered over the years, the etiology of these aneurysms remains unclear. The postulated origins include congenital malformation and acquired factors such as portal hypertension, liver disease, pancreatitis, or trauma[8,9]. In the present case, the fact that the PVA had not been present before the diagnosis of BCS was in place is suggestive of an acquired cause. However, interestingly, there has been no report in the literature of PVA in patients with BCS. This is likely due to the rarity of both conditions since portal hypertension irrespective of etiology could theoretically be associated with PVA.
Because of the limited literature, the management algorithm for PVA has been, and will likely continue to be, based on expert opinion and case reports. Surgery has long been the recommended mainstay of treatment, with aneurysmorrhaphy and portacaval shunt respectively adopted as the operation of choice in patients with and without portal hypertension[4]. Nonetheless, less invasive endovascular alternatives to these operations are now widely available. Endovascular coiling is a well-established technique which could be used to treat saccular PVA; however, the risk of this technique in the setting of portal hypertension may be high due to direct approach to the aneurysm. In addition, since coiling may not eliminate the mass effect from an aneurysm, those complicating organ compression are not candidates for this procedure. Another well-established technique which could be used to treat PVA is stent-grafting, although the risk of stent thrombosis is a major concern, particularly in patients with portal hypertension and/or thrombophilia. Portosystemic shunt remains to be the treatment of choice in those with portal hypertension, although portacaval shunt has largely been replaced by the less-invasive TIPS[5]. However, since portosystemic shunt does not specifically treat the aneurysm, no response to therapy may occur (defined as no improvement of symptoms or no reduction in aneurysm size). In these circumstances, more definitive treatment such as aneurysmorrhaphy may be required.
In conclusion, TIPS may be an effective and safe method of treatment for PVA in patients with portal hypertension. In addition, the role of endovascular therapy in the management of PVA is also highlighted.
A 65-year-old woman with Budd-Chiari syndrome (BCS) presented with steadily worsening, intermittent pain in the right upper quadrant of her abdomen, with no associated or alleviating factors.
The portal vein aneurysm was thought to be associated with BCS as there was no preceding history of trauma and it had not been present on Doppler ultrasound examination performed previously.
Laboratory tests revealed mildly elevated bilirubin and albumin deficit.
Contrast-enhanced computed tomography scan showed non-visualized middle and left hepatic veins, hepatomegaly with hypertrophy of the caudate lobe, splenomegaly, hepatic venous collaterals, no ascites, and a saccular aneurysm located at the extrahepatic portal vein main branch measuring 3.2 cm in height and 2.5 cm × 2.4 cm in diameter.
Transjugular intrahepatic portosystemic shunt was performed to relieve hepatic venous outflow obstruction.
To date, the utility of transjugular intrahepatic portosystemic shunt for the treatment of portal vein aneurysm has not been described.
Portal vein aneurysm is a rare clinical entity defined as abnormal dilation of the portal vein ≥ 2 cm in diameter.
Transjugular intrahepatic portosystemic shunt may be an effective and safe method of treatment for portal vein aneurysm in patients with portal hypertension.
This article reports a case of extrahepatic portal vein aneurysm in a patient with BCS treated with a transjugular intrahepatic portosystemic shunt.
P- Reviewer: Fujinaga H, Mortensen C S- Editor: Qi Y L- Editor: Logan S E- Editor: Wang CH
| 1. | Doust BD, Pearce JD. Gray-scale ultrasonic properties of the normal and inflamed pancreas. Radiology. 1976;120:653-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 96] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Barzilai R, Kleckner MS. Hemocholecyst following ruptured aneurysm of portal vein; report of a case. AMA Arch Surg. 1956;72:725-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 116] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Cho SW, Marsh JW, Fontes PA, Daily MF, Nalesnik M, Tublin M, De Vera ME, Geller DA, Gamblin TC. Extrahepatic portal vein aneurysm--report of six patients and review of the literature. J Gastrointest Surg. 2008;12:145-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Ma R, Balakrishnan A, See TC, Liau SS, Praseedom R, Jah A. Extra-hepatic portal vein aneurysm: A case report, overview of the literature and suggested management algorithm. Int J Surg Case Rep. 2012;3:555-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Boyer TD, Haskal ZJ. The Role of Transjugular Intrahepatic Portosystemic Shunt (TIPS) in the Management of Portal Hypertension: update 2009. Hepatology. 2010;51:306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 390] [Cited by in RCA: 405] [Article Influence: 27.0] [Reference Citation Analysis (1)] |
| 6. | Valla DC. Primary Budd-Chiari syndrome. J Hepatol. 2009;50:195-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 207] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 7. | Mancuso A. An update on management of Budd-Chiari syndrome. Ann Hepatol. 2014;13:323-326. [PubMed] |
| 8. | Schild H, Schweden F, Braun B, Lang H. Aneurysm of the superior mesenteric vein. Radiology. 1982;145:641-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Leonsins AJ, SIEW S. Fusiform aneurysmal dilatation of the portal vein. Postgrad Med J. 1960;36:570-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 1.2] [Reference Citation Analysis (0)] |