Published online Mar 7, 2015. doi: 10.3748/wjg.v21.i9.2836
Peer-review started: August 24, 2014
First decision: September 17, 2014
Revised: December 8, 2014
Accepted: January 8, 2015
Article in press: January 8, 2015
Published online: March 7, 2015
Processing time: 197 Days and 5.5 Hours
A 26-year-old man presented with migrated right lower abdominal pain and without any history of hematological systemic diseases. Blood routine test showed a leukocyte count of 22.74 × 109/L, with 91.4% neutrophils, and a platelet count of 4 × 109/L before admission. The case question was whether the team should proceed with surgery. Obviously, a differential diagnosis is essential before making such a decision. Acute appendicitis was easily diagnosed based on clinical findings, including migrating abdominal pain, a leukocyte count of 22.74 × 109/L and the result of abdominal computed tomography scan. However, it was not clear whether the severe thrombocytopenia was primary or secondary. So smear of peripheral blood and aspiration of bone marrow were ordered to exclude hematological diseases. Neither of the tests indicated obvious pathological hematological changes. There was no hepatosplenomegaly found by ultrasound examination of the liver and spleen. Therefore, operative intervention may be a unique clinical scenario in acute severe appendicitis patients with secondary thrombocytopenia.
Core tip: Should acute appendicitis with severe thrombocytopenia be operated? There are no reports about this clinical scenario. Acute appendicitis was diagnosed based on clinical findings, which included migrating right lower abdominal pain, a leukocyte count of 22.74 × 109/L and the result of abdominal computed tomography scan. However, we were not sure whether the severe thrombocytopenia was primary or secondary in nature. So smear of peripheral blood and aspiration of bone marrow were ordered to exclude the primary thrombocytopenia. Neither examination indicated any pathological changes in the hematological system. There was no hepatosplenomegaly found by ultrasound examination of the liver and spleen. Therefore, there were no contradictions for acute appendicitis patients with thrombocytopenia.
- Citation: Zhang HH, Gu GL, Zhang XY, Fan Q, Wang XY, Wei XM. Non-surgical contraindication for acute appendicitis with secondary thrombocytopenia: A case report. World J Gastroenterol 2015; 21(9): 2836-2839
- URL: https://www.wjgnet.com/1007-9327/full/v21/i9/2836.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i9.2836
Thrombocytopenia is an unusually complication which often caused by some viral infections, such as Epstein-Barr virus (EBV), cytomegalovirus (CMV), mumps, varicella, human immunodeficiency virus (HIV) and hepatitis[1,2]. Severe thrombocytopenia induced by appendicitis has been rarely reported. Here, we will give a case report of appendicitis-induced thrombocytopenia. The patient was in a healthy condition before treating with appendectomy successfully.
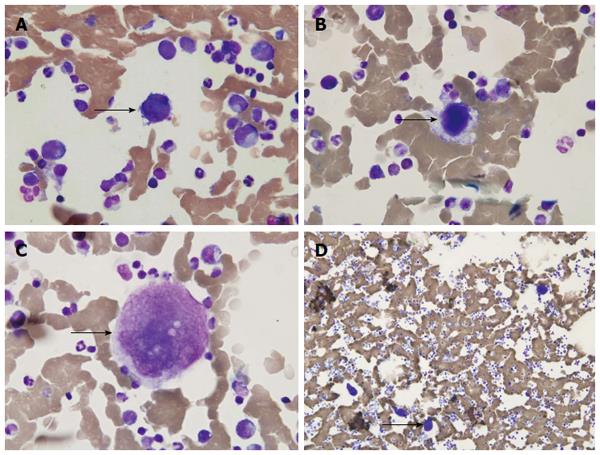
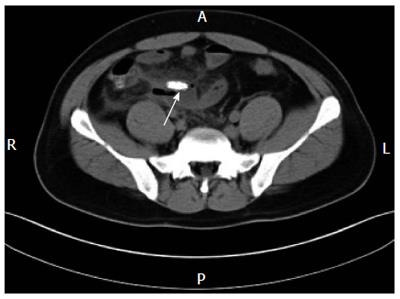
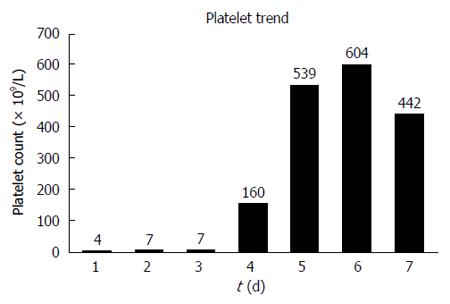
A 26-year-old, previously good, young man presented with migrating right lower abdominal pain without any history of hematological diseases. Three days before admission, he found episodes of left upper abdominal pain without any fever, loss of appetite, or fatigue. Two days before admission, he found episodes of right lower abdominal pain. He had no important inducing factors such as transfusions, heparin use or alcohol or drug abuse. Physical examination showed that he had a high fever, the temperature is 38.8 °C, tenderness in the right lower quadrant, and no petechiae on the extremities of limb. Ultrasound examination showed no lymphadenopathy or hepatosplenomegaly. Blood routine test showed a leukocyte count of 22.74 × 109/L, with 91.4% neutrophils, 4.8% monocytes and 3.7% lymphocytes, especially found many mono-nuclear cells with aberrant large nuclei, which showed atypical forms (about 16%). The hemoglobin level showed normal, was 16.8 g/L. The platelet count showed abnormal extremely, was 4 × 109/L and 7 × 109/L (normal, 100 × 109/L - 300 × 109/L) before admission. In order to rule out thrombocyte aggregation induced by EDTA, the platelet count was evaluated on citrate-anti-coagulated blood. Both results showed same as being decreased. Both renal and liver tests and coagulation panels showed normal, except for a blood sugar value of 7.3 mmol (normal, 3.6-6.1 mmol), uric acid content of 604 × 10-6 mol/L (normal, 155 × 10-6 mol/L - 428 × 10-6 mol/L), fibrinogen level of 9.3 g/L (normal, 1.8-4.8 g/L), and D-D of 746 ng/mL (normal, 0-255 ng/mL). Platelet size was found increased in the smear examination of peripheral blood. A bone marrow aspiration slide showed good smear staining and active proliferation with a hypercellular marrow and an abnormally represented megakaryocytic cell line. There were a total of 856 megakaryocytic cells, 50 of which were chosen for classification, including 5 immature megakaryocytes, 42 granular megakaryocytes, and 3 naked nucleus megakaryocytes. Productive megakaryocyte platelets were rare and scattered under the microscope. There were no obvious pathological changes in the erythroid and myeloid cell lines. Many atypical lymphocytes were seen but no parasites (Figure 1). Abdominal computed tomography (CT) scan showed the fecalith around the ileocecal junction in right lower abdomen (Figure 2). After the appendectomy, the platelet count was 7 × 109/L on the first day after operation, 7 × 109/L on the second day after operation, and 160 × 109/L on the fourth day after operation (Figure 3). The patient was cured and discharged from the hospital 1 wk after the surgery.
Should acute appendicitis with severe thrombocytopenia be operated on? There is no literature regarding this clinical dilemma. Acute severe appendicitis without surgery may result in appendicular perforation, which can lead to diffuse peritonitis or induce infectious shock, both of which can cause death. However, surgery on acute severe appendicitis in the presence of severe thrombocytopenia may cause uncontrollable bleeding in the incision or the epidural space, and the latter in particular can cause paraplegia, which is a severe complication of anesthesia. Therefore, the dilemma is how to address acute appendicitis with severe thrombocytopenia. In this case, the platelet count showed abnormal extremely, was 4 × 109/L and 7 × 109/L respectively before admission, which is far below the contraindicated level (70 × 109/L) for abdominal surgery. Obviously, establishing a differential diagnosis is essential before making a final decision. Acute appendicitis with migrating right low abdominal pain, a leukocyte count of 22.74 × 109/L, with 91.4% neutrophils, and a abdominal CT scan that shows the fecalith around the ileocecal junction in the right lower abdomen made the diagnosis relatively easy. Was the thrombocytopenia primary or secondary in this case? At first, the answer was not clear. So smear of peripheral blood and aspiration of bone marrow were ordered to exclude hematological diseases. Both examination results showed that the hematological system had no obvious pathological changes. A bone marrow aspiration slide showed that there were many megakaryocytic cells, which may have been due to severe infection, and that there was an active bone marrow proliferation. There was no hepatosplenomegaly found by ultrasound examination of the liver and spleen. Except for the above two aspects, we included EBV, mumps, varicella, HIV, CMV, chronic liver disease and Dengue fever in our differential diagnosis[3,4]. As for operative preparation and cooperation, the general anesthesia management should be determined, platelet transfusions should be used preoperatively and intravenous immunoglobulin should be given during the perioperative period.
In conclusion, our case underscores the fact that appendicitis-induced severe thrombocytopenia is not a surgical contraindication. Furthermore, operative intervention may be the unique clinical scenario in acute severe appendicitis patients with severe thrombocytopenia when the diagnosis has been confirmed and there is an extensive differential diagnosis.
A 26-year-old man presented with migrated right lower bellyache and with very lower platelet count which is far below the contraindicated level (70 × 109/L) for abdominal surgery.
Acute appendicitis with severe secondary thrombocytopenia
Primary thrombocytopenia usually caused by hematological system diseases and secondary thrombocytopenia usually caused by some viral infections and severe general infections.
The patient had elevated hematological values for neutrophil count (22.4 × 109/L) but very lower platelet count (4 × 109/L).
For the case, computed tomography scan showed a hyperdense shadow located in the right lower abdominal cavity.
For the case, bone marrow aspiration histological and pathological examination showed bone marrow proliferation activity and many megakaryocytic cells, which may be led by severe infection.
The patient was successfully treated with appendectomy.
Very few cases of acute appendicitis with severe secondary thrombocytopenia have been reported in the literature. The clinical and pathological characteristics of secondary thrombocytopenia caused by appendicitis remain unclear, laboratory diagnosis of secondary thrombocytopenia is not sure and the treatment of acute appendicitis with severe secondary thrombocytopenia is not sure.
Thrombocytopenia is an unusually complication which often caused by some viral infections, such as Epstein-Barr virus, cytomegalovirus, mumps, varicella, human immunodeficiency virus and hepatitis. Sometimes, severe general infections, such as acute appendicitis, especially without correct diagnosis and successful treatment in time, often caused severe secondary thrombocytopenia.
This case report presents the clinical characteristics of secondary thrombocytopenia caused by appendicitis and also discusses the treatment of acute appendicitis with severe secondary thrombocytopenia. We recommend that acute appendicitis with severe secondary thrombocytopenia should be given operation.
The authors have described the case of acute appendicitis with severe secondary thrombocytopenia that showed operative intervention was the unique clinical scenario when diagnosis is sure and differential diagnosis is nearly all around.
P- Reviewer: Mullan MJ S- Editor: Yu J L- Editor: A E- Editor: Wang CH
| 1. | Mandell GL, Douglas RG Jr, Bennett JE. Principles and practice of cytomegalovirus infection in an immunocompetent host. 5th ed. New York: Churchill Livingstone; . |
| 2. | Arruda VR, Rossi CL, Nogueira E, Annicchino-Bizzacchi JM, Costa FF, Costa SC. Cytomegalovirus infection as cause of severe thrombocytopenia in a nonimmunosuppressed patient. Acta Haematol. 1997;98:228-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Giannini EG. Review article: thrombocytopenia in chronic liver disease and pharmacologic treatment options. Aliment Pharmacol Ther. 2006;23:1055-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 136] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 4. | McFarlane ME, Plummer JM, Leake PA, Powell L, Chand V, Chung S, Tulloch K. Dengue fever mimicking acute appendicitis: A case report. Int J Surg Case Rep. 2013;4:1032-1034. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |