Published online Feb 28, 2015. doi: 10.3748/wjg.v21.i8.2534
Peer-review started: May 17, 2014
First decision: June 10, 2014
Revised: June 20, 2014
Accepted: August 28, 2014
Article in press: August 28, 2014
Published online: February 28, 2015
Processing time: 287 Days and 0.7 Hours
AIM: To compare the effect of endoscopic variceal ligation (EVL) with that of endoscopic injection sclerotherapy (EIS) in the treatment of patients with esophageal variceal bleeding.
METHODS: We performed a systematic literature search of multiple online electronic databases. Meta-analysis was conducted to evaluate risk ratio (RR) and 95% confidence interval (CI) of combined studies for the treatment of patients with esophageal variceal bleeding between EVL and EIS.
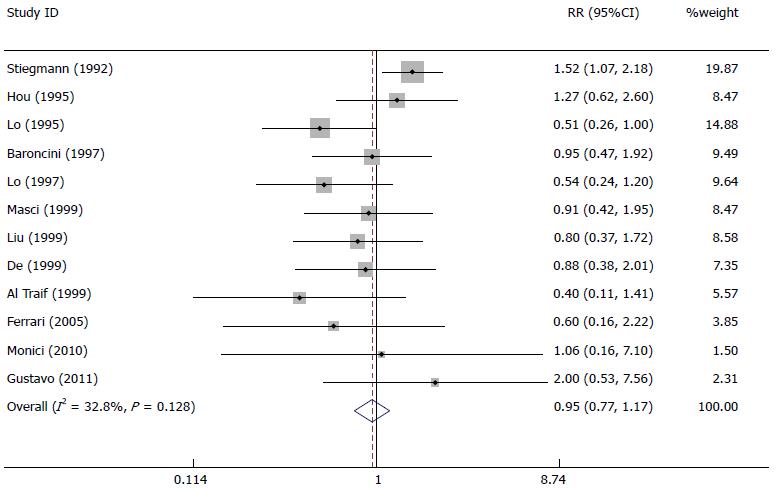
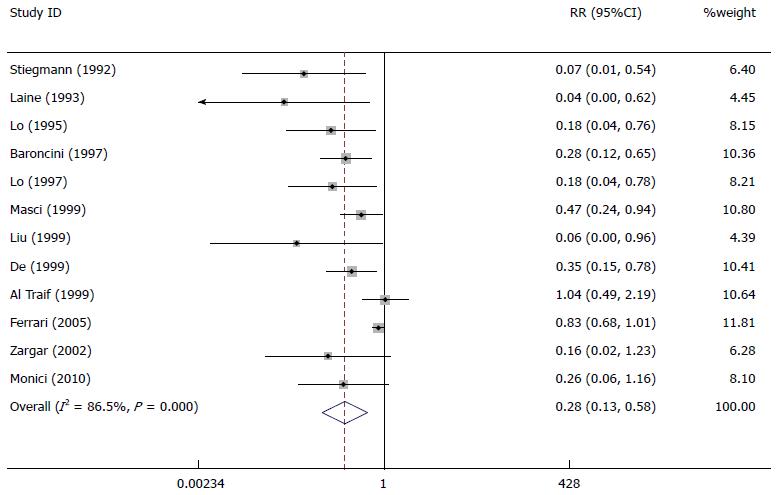
RESULTS: Fourteen studies comprising 1236 patients were included in the meta-analysis. The rebleeding rate in actively bleeding varices patients in the EVL group was significantly lower than that in the EIS group (RR = 0.68, 95%CI: 0.57-0.81). The variceal eradication rate in actively bleeding varices patients in the EVL group was significantly higher than that in the EIS group (RR = 1.06, 95%CI: 1.01-1.12). There was no significant difference about mortality rate between the EVL group and EIS group (RR = 0.95, 95%CI: 0.77-1.17). The rate of complications in actively bleeding varices patients in the EVL group was significantly lower than that in the EIS group (RR = 0.28, 95%CI: 0.13-0.58).
CONCLUSION: Our meta-analysis has found that EVL is better than EIS in terms of the lower rates of rebleeding, complications, and the higher rate of variceal eradication. Therefore, EVL is the first choice for esophageal variceal bleeding.
Core tip: We performed a meta-analysis to evaluate risk ratio and 95% confidence interval (CI) of combined studies for the treatment of patients with esophageal variceal bleeding between endoscopic variceal ligation (EVL) and endoscopic injection sclerotherapy (EIS). Our meta-analysis has found that EVL is better than EIS in terms of the lower rates of rebleeding, complications, and the higher rate of variceal eradication. Therefore, EVL is the first choice for esophageal variceal bleeding.
- Citation: Dai C, Liu WX, Jiang M, Sun MJ. Endoscopic variceal ligation compared with endoscopic injection sclerotherapy for treatment of esophageal variceal hemorrhage: A meta-analysis. World J Gastroenterol 2015; 21(8): 2534-2541
- URL: https://www.wjgnet.com/1007-9327/full/v21/i8/2534.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i8.2534
Esophageal variceal bleeding is the most common (as many as 30%) in all patients presenting with upper gastrointestinal tract hemorrhage[1]. Acute esophageal variceal bleeding is an intractable complication of portal hypertension. Patients with esophageal variceal bleeding have higher rates of rebleeding, complications, and death than patients with nonvariceal bleeding such as ulcer bleeding[2-5]. Traditional measures have included balloon tamponade, vasoconstrictors, and surgical intervention, but these measures did not significantly reduce the rate of rebleeding, complications and improve survival.
Endoscopic injection sclerotherapy (EIS) has been gradually applied to the management of esophageal variceal bleeding since the mid-1970s[6]. And EIS performed as the first effective measure proved to be superior to vasoconstrictors or balloon tamponade in the control of acute esophageal variceal bleeding[7-9]. However, EIS is associated with some complications such as adverse pulmonary and renal effects, esophageal ulceration, stricture, perforation, and death[10]. Complications occur in up to 40% of patients, and treatment-related death in 1% to 2%.
Endoscopic variceal ligation (EVL) was introduced in 1986[11], and it is now considered by many clinicians to be the treatment of choice for patients with esophageal variceal bleeding. In theory, this purely mechanical method of obliterating varices should produce no systemic sequelae, and since the quantity of tissue ligated is limited by the design of the device, it should also result in few complications involving the esophageal wall[12]. The incidence of complications, such as pneumonia and esophageal stricture, which were associated with EVL was very low[13,14]. Some randomized controlled trials indicated that EVL is at least as effective and safe as EIS. Now EVL has been gradually adopted to substitute for EIS in the treatment of esophageal variceal bleeding.
Some randomized controlled trials have compared EVL with EIS in terms of sessions required to achieve variceal obliteration, rebleeding rate, mortality rate and complication rate[12,15-26]. However, all of those studies comprised only a small number of patients with active variceal bleeding, and have come to conflicting conclusions.
To critically appraise and synthesize the current evidence on endoscopic therapy for esophageal variceal bleeding, we conducted a meta-analysis combining the results of randomized controlled trials that compared EVL with EIS, and thus provided a quantitative estimate of the risk of rebleeding, mortality, complications and variceal eradication.
We developed and adhered to a standard protocol for study identification, inclusion, and data abstraction in the conduct of this meta-analysis. We performed a systematic literature search of the following electronic databases: MEDLINE (1950-2014), EMBASE (1947-2014), Cochrane library (1993-2014), Web of Science (1900-2014), and PubMed (1950-2014). Bibliographies from relevant gastrointestinal meetings including Digestive Disease Week, The Annual Meeting of the American College of Gastroenterology, and United European Gastroenterology Week during years 2000-2014 were manually searched for relevant studies. Medical subject headings for our literature review included “esophageal varices”, “esophageal variceal bleeding “, “variceal bleeding “, “endoscopic injection sclerotherapy”, “EIS”, “endoscopic variceal ligation”, and “EVL”. Citations from identified articles were then cross-referenced for completeness.
Inclusion criteria included: (1) studies used a case-control, nested case-control, cross-sectional, and cohort study design; (2) the study was a randomized controlled comparison of EIS and EVL; (3) the study population was composed of patients with esophageal variceal bleeding; and (4) outcome measures were the rate of rebleeding, mortality, complications or variceal eradication.
We performed the data extraction via a standardized data extraction form, collecting information on the author, publication year, country, number of cases, mean age of patients in the EVL group and EIS group, Child-Pugh grade, and etiology. The outcome of the analysis was the risk ratio (RR) of rebleeding, mortality, complications or variceal eradication in the EIS group vs the EVL group. Study references and citations were collected in EndNote X4 software application. All studies were reviewed by two investigators (Dai C and Liu WX) to assess eligibility. The data of studies which meet our eligibility criteria were independently analyzed by two investigators. The collected information included author, publication year, country, number of cases, mean age of patients in the EVL group and EIS group, Child-Pugh grade (A/B/C), etiology (alcoholic/viral/others), complications, and follow-up. Discordant results were adjudicated by the senior author (Sun MJ). The paired agreement among the authors was 0.998. The methodological quality of each trial was assessed using the following criteria: study design, method of esophageal variceal bleeding diagnosis and method of patient enrollment.
The presence of inter-study heterogeneity was calculated by the χ2-based Q-test, and significance was set at the P < 0.10 level. The inconsistency index (I2) was calculated to assess the variation caused by the heterogeneity. If heterogeneity was observed among the studies, the random-effects model was used to estimate the pooled RR (the DerSimonian and Laird method). Otherwise, the fixed-effects model was adopted (the Mantel-Haenszel method). Summary RR and 95% confidence interval (CI) were used to describe the risk of rebleeding, mortality, complications and variceal eradication in the EIS group vs the EVL group. Publication bias was assessed by funnel plot analysis. Meta-analysis was done using STATA 12.0.
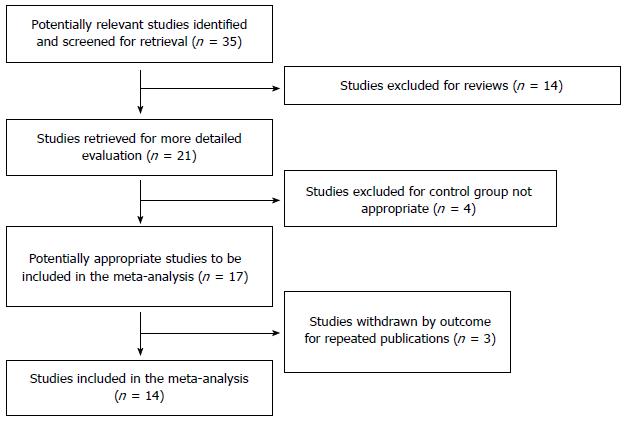
Our meta-analysis identified a total of 35 studies. After carefully cross-referencing the titles, abstracts and keywords, potentially relevant studies were evaluated for potential inclusion (Figure 1). Ultimately, 17 studies were reviewed in detail, of which 14 met inclusion criteria and were included in the meta-analysis. Details regarding the included studies, including author, publication year, country, number of cases, mean age of patients in the EVL group and EIS group, Child-Pugh grade (A/B/C), etiology (alcoholic/viral/others), complications, and follow-up, can be found in Table 1. The study sizes ranged from 46 to 134 and the mean age ranged from 6 to 73 years. The mean follow-up period ranged from 6 to 34 mo. More than 80% of patients had cirrhosis. The proportion of patients with alcoholic cirrhosis ranged from 1.7% to 81%, and viral cirrhosis ranged from 0% to 84%. The proportion of patients with Child A liver disease ranged from 7% to 81%, Child B liver disease from 3.7% to 60%, and Child C liver disease from 0% to 59%.
| Ref. | Year | Country | No. of cases | EVL mean age (yr) | EIS mean age (yr) | Child-Pugh grade (A/B/C) | Etiology (alcoholic/viral/others) | Complications | Follow-up |
| Stiegmann et al[12] | 1992 | United States | 129 | 51 ± 13 | 53 ± 13 | 42/62/25 | 105/- | Esophageal strictures, and other infections | 10 mo |
| Laine et al[15] | 1993 | United States | 77 | 44 ± 1 | 48 ± 2 | 13/46/18 | 61/0/16 | Esophageal strictures and esophageal ulcers | 3 mo |
| Hou et al[16] | 1995 | China | 134 | 60.1 ± 12.1 | 61.0 ± 11.7 | 32/50/52 | 22/90/22 | Esophageal strictures and esophageal ulcers | 3 mo |
| Lo et al[17] | 1995 | China | 120 | 57 ± 13 | 54 ± 12 | 16/46/58 | 27/- | Esophageal strictures and esophageal ulcers | 295 ± 120 d (EIS); 310 ± 105d (EVL) |
| Baroncini et al[19] | 1997 | Italy | 111 | 63.0 ± 9.1 | 61.4 ± 9.8 | 35/46/30 | 15/93/3 | Esophageal strictures and esophageal ulcers | 3 mo |
| Lo et al[20] | 1997 | China | 71 | 53 ± 15 | 55 ± 13 | 5/24/42 | 20/46/5 | Esophageal strictures and esophageal ulcers | 1 mo |
| Al Traif et al[27] | 1999 | Saudi Arabia | 60 | 48.2 ± 3.5 | 49.4 ± 3.2 | 22/23/15 | 1/35/24 | Esophageal strictures and esophageal ulcers | 3 mo |
| Masci et al[22] | 1999 | Italy | 100 | 59.5 | 63.8 | 33/43/24 | - | Esophageal strictures and esophageal ulcers | 3 mo |
| Liu et al[28] | 1999 | China | 81 | 48.2 ± 8.5 | 50.1 ± 9.1 | 73/3/5 | 14/48/19 | Esophageal strictures and esophageal ulcers | 3 mo |
| de la Peña et al[29] | 1999 | Spain | 88 | 59 | 59 | 21/44/23 | 58/21/9 | Esophageal strictures and esophageal ulcers | 3 wk |
| Zargar et al[24] | 2002 | India | 49 | 9.1 ± 2.7 | 9.5 ± 2.8 | - | - | Esophageal strictures and esophageal ulcers | 3 mo |
| Ferrari et al[25] | 2005 | Brazil | 46 | 49.1 ± 13.2 | 49.3 ± 10.7 | 17/22/7 | 22/18/6 | Esophageal strictures and esophageal ulcers | 1 yr |
| Monici et al[26] | 2010 | Brazil | 70 | 48.5 | 47.8 | 57/13/0 | 20/24/26 | Esophageal strictures and esophageal ulcers | 1 mo |
| Luz et al[30] | 2011 | Brazil | 100 | 54.48 | 50.24 | 5/43/35 | 36/34/30 | Esophageal strictures and esophageal ulcers | 6 wk |
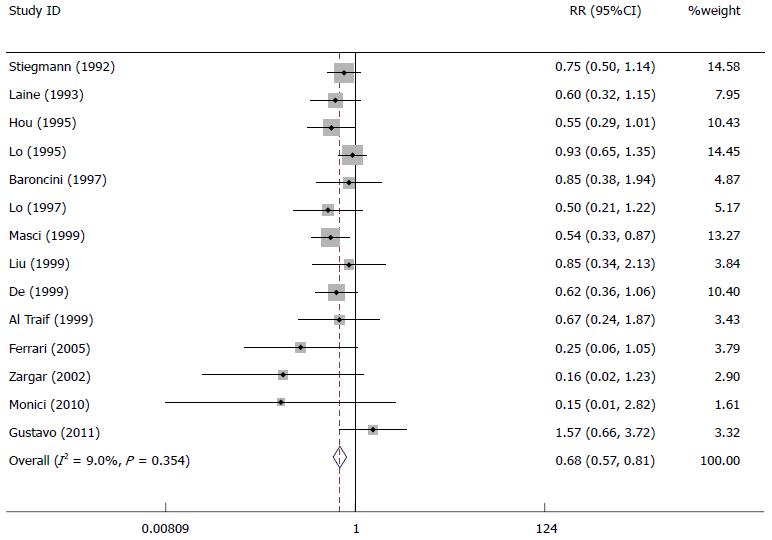
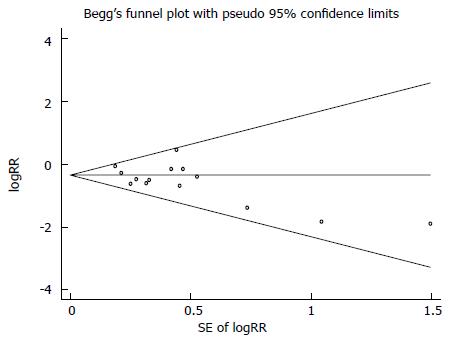
Fourteen studies in the meta-analysis included 1236 patients with esophageal variceal bleeding. The rebleeding rate in actively bleeding varices patients in the EVL group was significantly lower than that in the EIS group (RR = 0.68, 95%CI: 0.57-0.81) (Figure 2), suggesting that the rebleeding in esophageal variceal bleeding patients was more likely to occur in the EIS group compared with the EVL group. There was statistically significant homogeneity (P = 0.354). The funnel plot (Figure 3) was generally symmetrical, showing no evidence of publication bias (Begg’s test, Z = 1.31, P = 0.189).
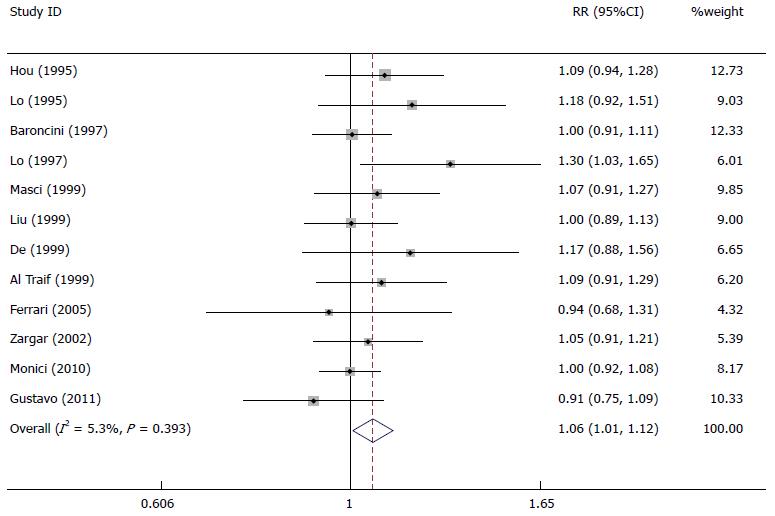
The variceal eradication rate in actively bleeding varices patients in the EVL group was significantly higher than that in the EIS group (RR = 1.06, 95%CI: 1.01-1.12) (Figure 4), suggesting that EVL was more effective in the variceal eradication in esophageal variceal bleeding patients than EIS.
There was no significant difference about mortality rate between the EVL group and EIS group (RR = 0.95, 95%CI: 0.77-1.17) (Figure 5). At the same time, the rate of complications in actively bleeding varices patients in the EVL group was significantly lower than that in the EIS group (RR = 0.28; 95%CI: 0.13-0.58) (Figure 6). Bleeding from treatment-induced ulcers, esophageal perforation and strictures were less frequently in patients treated by EVL, but the difference was not statistically significant. There were significant differences between the two therapies in the proportion of pulmonary infections or episodes of spontaneous bacterial peritonitis.
The purpose of this meta-analysis was to compare the effects of EVL with EIS in the treatment of patients with esophageal variceal bleeding. By synthesizing all available data from previous studies, the meta-analysis provide a more precise estimate than the results which can be obtained from all individual studies. The overall rebleeding rate in the EVL group of these studies was 21.7%, while the rebleeding rate in the EIS group was 33.1%. Although only one of these studies (Masci, 1999) showed a significantly lower rebleeding rate in the EVL group than in the EIS group, other studies showed different results. From the results of our meta-analysis, we have found that the rebleeding rate in EVL group was significantly lower than that in the EIS group (Figure 2). The main reason of rebleeding was varices or treatment-induced ulcers.
EVL requires placement of an opaque cylinder in front of the endoscope. This therapy can affect the endoscopic vision. Visualization is very important for treatment in a patient with esophageal variceal bleeding, and may be more impaired when treating by EVL than by EIS. Although the visualization of EIS is better than that of EVL, our meta-analysis shows that EVL achieved a higher variceal eradication rate than EIS in these studies (Figure 4). In the future, the opaque cylinder will be replaced by a clear plastic cylinder which can provide better visualization in patients with esophageal variceal bleeding.
We have not only assessed the efficacy of EIS and EVL, but also evaluated the complications and side effects. The mortality seen with EVL in these studies was 22.8%, while the mortality with EIS was 24.6%. Our meta-analysis shows that there was no significant difference about mortality rate between the EVL group and EIS group (Figure 5). Some studies have demonstrated that prevention of esophageal variceal bleeding by surgical therapy or medical treatment does not necessarily decrease mortality and improve survival. Deaths due to bleeding or other causes occurred less frequently in the EVL group than in the EIS group. Local complications such as esophageal strictures were less common in the EVL group than in the EIS group (Figure 6). There were no significant differences about systemic complications such as pulmonary infections and bacterial peritonitis in the two groups.
The costs of the equipment and material required for EVL or EIS in esophageal variceal bleeding are similar. In addition to cost differentials that may occur in relation to differences in efficacy (variceal eradication and rebleeding) or complications (local complications and systemic complications), substantial cost savings is likely if the treatment requires fewer endoscopic treatment sessions. However, an in-depth economic evaluation is warranted to carefully evaluate all of the costs and consequences of these two treatments in the management of patients with esophageal variceal bleeding.
Our meta-analysis has several limitations. First, our meta-analysis has included some studies from different countries which have ethnic differences. Second, the etiology and severity of esophageal varices in these studies were different. Third, these medical institutions in the included studies have different medical facilities and medical technology, so the treatment for esophageal variceal bleeding such as EVL and EIS may lead to different results.
In conclusion, on the basis of lower rates of rebleeding, mortality, and complications (local complications and systemic complications) and higher rates of variceal eradication, our meta-analysis has found that EVL should be considered the appropriate endoscopic treatment option for patients with esophageal variceal bleeding. Of course, further large-scale randomized controlled trials will be helpful in more firmly establishing the efficacy of EVL for patients with esophageal variceal bleeding.
Esophageal variceal bleeding is the most common (as many as 30%) in all patients presenting with upper gastrointestinal tract hemorrhage. Acute esophageal variceal bleeding is an intractable complication of portal hypertension. Traditional measures have included balloon tamponade, vasoconstrictors, and surgical intervention, but these measures did not significantly reduce the rate of rebleeding, complications and improve survival.
Some randomized controlled trials have compared endoscopic variceal ligation (EVL) with endoscopic injection sclerotherapy (EIS) in terms of sessions required to achieve variceal obliteration, rebleeding rate, mortality rate and complication rate. However, all of those studies comprised only a small number of patients with active variceal bleeding, and have come to conflicting conclusions.
Based on this meta-analysis, the rebleeding rate and the complication rate in actively bleeding varices patients in the EVL group were significantly lower than those in the EIS group. The variceal eradication rate in actively bleeding varices patients in the EVL group was significantly higher than that in the EIS group. There was no significant difference about mortality rate between the EVL group and EIS group.
EVL is better than EIS in terms of the lower rates of rebleeding, complications, and the higher rate of variceal eradication. Therefore, EVL is the first choice for esophageal variceal bleeding.
EIS has been gradually applied to the management of esophageal variceal bleeding since the mid-1970s. EIS performed as the first effective measure proved to be superior to vasoconstrictors or balloon tamponade in the control of acute esophageal variceal bleeding. EVL was introduced in 1986 and was a purely mechanical method of obliterating varices.
This is a good meta-analysis on the endoscopic treatment of bleeding esophageal varices. The authors present a systematic review and meta-analysis to answer the question of preferred treatment modality for patients presenting with variceal bleeding. The primary therapies compared in this study are EVL and EIS. The meta-analysis shows the benefit of EVL compared to EIS in terms of significantly lower rebleeding rates and comparable mortality.
P- Reviewer: Barkin JA, Fiori E, Sofi A S- Editor: Qi Y L- Editor: Wang TQ E- Editor: Zhang DN
| 1. | Laine L. Upper gastrointestinal tract hemorrhage. West J Med. 1991;155:274-279. [PubMed] |
| 2. | Gilbert DA, Silverstein FE, Tedesco FJ. National ASGE survey on upper gastrointestinal bleeding: complications of endoscopy. Dig Dis Sci. 1981;26:55S-59S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 45] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Gilbert DA, Silverstein FE, Tedesco FJ, Buenger NK, Persing J. The national ASGE survey on upper gastrointestinal bleeding. III. Endoscopy in upper gastrointestinal bleeding. Gastrointest Endosc. 1981;27:94-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 107] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Silverstein FE, Gilbert DA, Tedesco FJ, Buenger NK, Persing J. The national ASGE survey on upper gastrointestinal bleeding. II. Clinical prognostic factors. Gastrointest Endosc. 1981;27:80-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 220] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Silverstein FE, Gilbert DA, Tedesco FJ, Buenger NK, Persing J. The national ASGE survey on upper gastrointestinal bleeding. I. Study design and baseline data. Gastrointest Endosc. 1981;27:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 130] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Infante-Rivard C, Esnaola S, Villeneuve JP. Role of endoscopic variceal sclerotherapy in the long-term management of variceal bleeding: a meta-analysis. Gastroenterology. 1989;96:1087-1092. [PubMed] |
| 7. | Terblanche J, Bornman PC, Kahn D, Kirsh RE. Sclerotherapy in acute variceal bleeding: technique and results. Endoscopy. 1986;18 Suppl 2:23-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Paquet KJ, Feussner H. Endoscopic sclerosis and esophageal balloon tamponade in acute hemorrhage from esophagogastric varices: a prospective controlled randomized trial. Hepatology. 1985;5:580-583. [PubMed] |
| 9. | Westaby D, Hayes PC, Gimson AE, Polson RJ, Williams R. Controlled clinical trial of injection sclerotherapy for active variceal bleeding. Hepatology. 1989;9:274-277. [PubMed] |
| 10. | Schuman BM, Beckman JW, Tedesco FJ, Griffin JW, Assad RT. Complications of endoscopic injection sclerotherapy: a review. Am J Gastroenterol. 1987;82:823-830. [PubMed] |
| 11. | Van Stiegmann G, Cambre T, Sun JH. A new endoscopic elastic band ligating device. Gastrointest Endosc. 1986;32:230-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 162] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 12. | Stiegmann GV, Goff JS, Michaletz-Onody PA, Korula J, Lieberman D, Saeed ZA, Reveille RM, Sun JH, Lowenstein SR. Endoscopic sclerotherapy as compared with endoscopic ligation for bleeding esophageal varices. N Engl J Med. 1992;326:1527-1532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 504] [Cited by in RCA: 415] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 13. | Tedesco FJ. Endoscopic ligation of esophageal varices: an endoscopist’s opinion. Hepatology. 1990;12:783-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Van Stiegmann G, Goff JS, Sun JH, Hruza D, Reveille RM. Endoscopic ligation of esophageal varices. Am J Surg. 1990;159:21-5; discussion 25-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 54] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Laine L, el-Newihi HM, Migikovsky B, Sloane R, Garcia F. Endoscopic ligation compared with sclerotherapy for the treatment of bleeding esophageal varices. Ann Intern Med. 1993;119:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 203] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 16. | Hou MC, Lin HC, Kuo BI, Chen CH, Lee FY, Lee SD. Comparison of endoscopic variceal injection sclerotherapy and ligation for the treatment of esophageal variceal hemorrhage: a prospective randomized trial. Hepatology. 1995;21:1517-1522. [PubMed] |
| 17. | Lo GH, Lai KH, Cheng JS, Hwu JH, Chang CF, Chen SM, Chiang HT. A prospective, randomized trial of sclerotherapy versus ligation in the management of bleeding esophageal varices. Hepatology. 1995;22:466-471. [PubMed] |
| 18. | Laine L, Stein C, Sharma V. Randomized comparison of ligation versus ligation plus sclerotherapy in patients with bleeding esophageal varices. Gastroenterology. 1996;110:529-533. [PubMed] |
| 19. | Baroncini D, Milandri GL, Borioni D, Piemontese A, Cennamo V, Billi P, Dal Monte PP, D’Imperio N. A prospective randomized trial of sclerotherapy versus ligation in the elective treatment of bleeding esophageal varices. Endoscopy. 1997;29:235-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 97] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 20. | Lo GH, Lai KH, Cheng JS, Lin CK, Huang JS, Hsu PI, Chiang HT. Emergency banding ligation versus sclerotherapy for the control of active bleeding from esophageal varices. Hepatology. 1997;25:1101-1104. [PubMed] |
| 21. | Djurdjevic D, Janosevic S, Dapcevic B, Vukcevic V, Djordjevic D, Svorcan P, Grgov S. Combined ligation and sclerotherapy versus ligation alone for eradication of bleeding esophageal varices: a randomized and prospective trial. Endoscopy. 1999;31:286-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Masci E, Stigliano R, Mariani A, Bertoni G, Baroncini D, Cennamo V, Micheletti G, Casetti T, Tansini P, Buscarini E. Prospective multicenter randomized trial comparing banding ligation with sclerotherapy of esophageal varices. Hepatogastroenterology. 1999;46:1769-1773. [PubMed] |
| 23. | Mohamed AR, Gadour M, Ghandour Z, al Karawi M. Endoscopic management for bleeding esophageal varices: sclerotherapy versus sclerotherapy plus band ligation versus band ligation alone. One year experience at a main hospital in Saudi Arabia. Hepatogastroenterology. 1999;46:967-970. [PubMed] |
| 24. | Zargar SA, Javid G, Khan BA, Yattoo GN, Shah AH, Gulzar GM, Singh J, Rehman BU, Din Z. Endoscopic ligation compared with sclerotherapy for bleeding esophageal varices in children with extrahepatic portal venous obstruction. Hepatology. 2002;36:666-672. [PubMed] |
| 25. | Ferrari AP, de Paulo GA, de Macedo CM, Araújo I, Della Libera E. Efficacy of absolute alcohol injection compared with band ligation in the eradication of esophageal varices. Arq Gastroenterol. 2005;42:72-76. [PubMed] |
| 26. | Monici LT, Meirelles-Santos JO, Soares EC, Mesquita MA, Zeitune JM, Montes CG, Almeida JR, Yamanaka A, Magna LA. Microwave coagulation versus sclerotherapy after band ligation to prevent recurrence of high risk of bleeding esophageal varices in Child-Pugh’s A and B patients. J Gastroenterol. 2010;45:204-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 27. | Al Traif I, Fachartz FS, Al Jumah A, Al Johani M, al-Omair A, al-Bakr F, al-Knawy B, el-Hafi A, Khan MH. Randomized trial of ligation versus combined ligation and sclerotherapy for bleeding esophageal varices. Gastrointest Endosc. 1999;50:1-6. [PubMed] |
| 28. | Liu DL, Huo JR, Wu XP. Comparative clinical study of ligation versus sclerotherapy in the treatment of bleeding esophageal varices. Hunan Yixue. 1999;16:90-91. |
| 29. | de la Peña J, Rivero M, Sanchez E, Fábrega E, Crespo J, Pons-Romero F. Variceal ligation compared with endoscopic sclerotherapy for variceal hemorrhage: prospective randomized trial. Gastrointest Endosc. 1999;49:417-423. [PubMed] |
| 30. | Luz GO, Maluf-Filho F, Matuguma SE, Hondo FY, Ide E, Melo JM, Cheng S, Sakai P. Comparison between endoscopic sclerotherapy and band ligation for hemostasis of acute variceal bleeding. World J Gastrointest Endosc. 2011;3:95-100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |