Published online Feb 28, 2015. doi: 10.3748/wjg.v21.i8.2490
Peer-review started: August 24, 2014
First decision: September 27, 2014
Revised: October 29, 2014
Accepted: December 8, 2014
Article in press: December 8, 2014
Published online: February 28, 2015
Processing time: 188 Days and 6.3 Hours
AIM: To compare the effects and postoperative complications between tissue selecting therapy stapler (TST) and Milligan-Morgan hemorrhoidectomy (M-M).
METHODS: Four hundred and eighty patients with severe prolapsing hemorrhoids, who were admitted to the Shenyang Coloproctology Hospital between 2009 and 2012, were randomly divided into observation (n = 240) and control (n = 240) groups. Hemorrhoidectomies were performed with TST in the observation group and with the M-M technique in the control group. The therapeutic effects, operation security, and postoperative complications in the two groups were compared. The immediate and long-term complications were assessed according to corresponding criteria. Pain was assessed on a visual analogue scale. The efficacy was assessed by specialized criteria. The follow-up was conducted one year after the operation.
RESULTS: The total effective rates of the observation and control groups were 99.5% (217/218) and 98.6% (218/221) respectively; the difference was not statistically significant (P = 0.322). Their were significant differences between observation and control groups in intraoperative blood loss (5.07 ± 1.14 vs 2.45 ± 0.57, P = 0.000), pain (12 h after the surgery: 5.08 ± 1.62 vs 7.19 ± 2.01, P = 0.000; at first dressing change: 2.64 ± 0.87 vs 4.34 ± 1.15, P = 0.000; first defecation: 3.91 ± 1.47 vs 5.63 ± 1.98, P = 0.001), urine retention (n = 22 vs n = 47, P = 0.001), anal pendant expansion after the surgery (2.35 ± 0.56 vs 5.16 ± 1.42, P = 0.000), operation time (18.3 ± 5.6 min vs 29.5 ± 8.2 min, P = 0.000), and the length of hospital stay (5.3 ± 0.6 d vs 11.4 ± 1.8 d, P = 0.000). Moreover TST showed significant reductions compared to M-M in the rates of long-term complications such as fecal incontinence (n = 3 vs n = 16, P = 0.003), difficult bowel movement (n = 1 vs n = 9, P = 0.011), intractable pain (n = 2 vs n = 12, P = 0.007), and anal discharge (n = 3 vs n = 23, P = 0.000).
CONCLUSION: TST for severe prolapsing hemorrhoids is a satisfactory technique for more rapid recovery, lower complication rates, and higher operation security.
Core tip: Tissue selecting therapy staplers are increasingly used in clinics as a minimally invasive technique for treating hemorrhoids, based on the formation mechanism and physiologic and pathologic structural changes of hemorrhoids. This method protects anal cushions and functions. In this study, 480 patients with severe prolapsing hemorrhoids, who were admitted to the Shenyang Anorectal Hospital, were treated with this method or by Milligan-Morgan hemorrhoidectomy. The efficacy of both methods was assessed one year after the operation. The therapeutic effects, operation security, and postoperative complications from the two treatment methods were compared.
- Citation: Wang ZG, Zhang Y, Zeng XD, Zhang TH, Zhu QD, Liu DL, Qiao YY, Mu N, Yin ZT. Clinical observations on the treatment of prolapsing hemorrhoids with tissue selecting therapy. World J Gastroenterol 2015; 21(8): 2490-2496
- URL: https://www.wjgnet.com/1007-9327/full/v21/i8/2490.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i8.2490
Hemorrhoids, especially severe prolapsing hemorrhoids, have always been over-treated to various degrees; yet, surgery is one of the important treatments for hemorrhoids. Based on clinical practice, it is assumed that surgery is effective for severe prolapsing hemorrhoids. However, it is difficult to deal with the postoperative complications such as fecal urgency and anal stenosis. Milligan-Morgan hemorrhoidectomy (M-M), though wildly practiced, has some disadvantages such as postoperative pain and a long period of convalescence[1]. In 1998, Longo[2], an Italian expert, reported the treatment of hemorrhoids with a procedure for prolapse and hemorrhoids (PPH). Since then, PPH has been widely used in clinical practice and achieved desirable efficacy; yet, its side effects have been reported in recent years[3]. Tissue selecting therapy stapler (TST) is a minimally invasive technique for hemorrhoids, which is based on the formation mechanism and physiologic and pathologic structural changes of hemorrhoids, that has gradually been applied in the clinic[4,5]. This method is used to protect anal cushions and functions. This clinical trial was conducted to compare the efficacy and complications associated with TST in comparison to M-M.
A total of 480 male and female patients with severe prolapsing hemorrhoids, who were admitted in Shenyang Anorectal Hospital between 2009 and 2012, were randomly divided into observation (n = 24; aged 19-84 years) and control (n = 240; aged 18-75 years) groups. Patients in the observation group underwent TST, whereas those in the control group received M-M. The patients who met the following criteria were included in the study: (1) grade III-IV mixed prolapsing hemorrhoids[6]; (2) 18-84 years-old; (3) hemorrhoids confirmed by colonoscopy, anorectal manometry, and anorectal ultrasound to the exclusion of other colorectal disorders and dysfunctions (e.g., tumor, inflammatory bowel disease, anismus, fecal incontinence); (4) without severe primary diseases of the cardiovascular system, liver, kidneys, hematopoietic system and so on; and (5) without chronic constipation.
All the participants underwent routine exams such as blood routine, coagulation tests, liver function test, kidney function test, immunologic indices, color ultrasound of the liver, gallbladder and spleen, chest X-ray and electrocardiogram. The night before the operation, they received intestinal cleaning with 73.69 g polyethylene glycol-electrolyte powder diluted in 2000 mL lukewarm boiled water. During the operation, sacral anesthesia and lithotomy position were adopted.
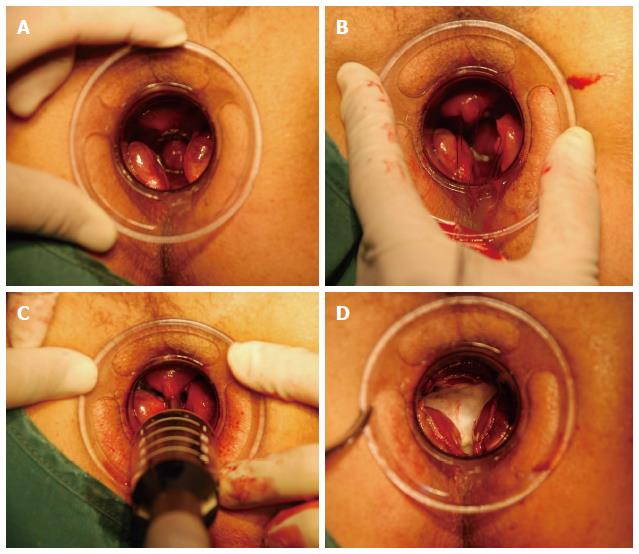
The surgery was performed in the following steps[5]: (1) the suitable anoscope was chosen based on the number and location of hemorrhoids; (2) the anoscope was inserted into the anus after appropriate anal dilatation. Then, the introducer was withdrawn, the mucosa above the prolapsing hemorrhoids was exposed and the anoscope was fixed (Figure 1A); (3) a 2-0 absorbable suture string was used for purse-string suture. The string was placed 3-4 cm above the dentate line. The specific location of the string was determined by the degree of relaxation of the rectal mucosa. The most suitable one should be 2 cm below the window of the anoscope (Figure 1B); (4) the circular stapler was opened to its maximum. Its anvil was positioned in the rectum. The string was pulled from the holes in both sides of the stapler by a suture threader and stretched with proper strength; meanwhile, the stapler was tightened and the gun was fired. Thirty seconds later, the stapler was removed (Figure 1C); (5) the mucosal bridges were dissected. Then, the staple line was inspected. A figure-eight suture with absorbable strings was applied to ensure hemostasis if bleeding occurred along the line; (6) the removed tissue underwent pathologic exams (Figure 1D); and (7) the skin tags of external hemorrhoids were removed.
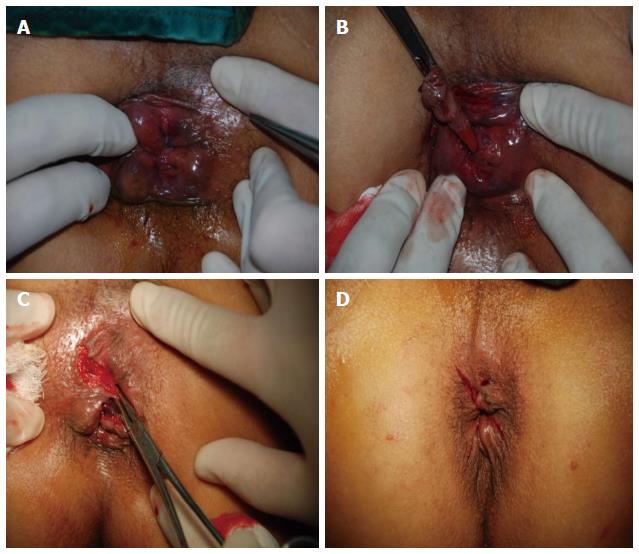
The operation was performed in the following steps: (1) the number and location of hemorrhoids was observed (Figure 2A); (2) an appropriate anal dilatation was performed; (3) clamped by a hemostat vertically, the external hemorrhoids were dissected along the dentate line and the internal hemorrhoids were ligated where enough mucosal bridges were left (0.5-1.0 cm) (Figure 2B and C); (4) the wound was repaired and the bleeding was stopped (Figure 2D); (5) gauze was used to ensure hemostasis; and (6) the removed tissue underwent pathologic exams.
The efficacy was assessed one year after the operation and defined as: (1) recovery: prolapse symptoms completely disappeared; (2) effectiveness: < 50% prolapse symptoms persisted; and (3) ineffectiveness: > 50% prolapse symptoms persisted[7].
Criteria for evaluating immediate complications include: (1) pain was evaluated by the visual analogue scale (VAS)[8] (score 0 = no pain, score 10 = severe pain) at three time points after the operation (local pain 12 h later, during the first dressing change the next morning, and during the first defecation); (2) intraoperative blood loss (0 = no blood loss; 1 = 1-5 mL; 2 = 6-10 mL; 3 = 11-15 mL; 4 = 16-20 mL; 5 = 21-25 mL; 6 = 26-30 mL; 7 = 31-35 mL; 8 = > 35 mL[7]); (3) operation time (min); (4) urine retention (use of urethral catheterization due to inability to voluntarily urinate within 24 h after the operation[9]); (5) anal pendant expansion after operation was evaluated by VAS[8]; and (6) the length of hospital stay (d).
Telephone follow-up was performed to determine whether the participants had the following symptoms: (1) rectal and vaginal fistula; (2) fecal incontinence (a lack of control over defecation, leading to involuntary loss of gas or stool); (3) difficult bowel movement (a condition in which the anus and/or rectum is less than two fingers wide so the stool is narrowed); (4) intractable pain (long-term pain caused by scar or foreign body after the surgery); and (5) anal discharge (wet anus or anal discharge caused by the scar left by the surgery). Between the surgery and follow-up, all the return visits for the above complications were recorded. The participants were required to pay a return visit if they were found suffering from the above complications during the follow-up.
One year after the surgery, telephone follow-up was applied to conduct a satisfaction survey on the surgery: satisfied, somewhat satisfied, not satisfied.
The data were analyzed by SPSS version 13.0 (SPSS Inc., Chicago, IL, United States). Measurement data are expressed as mean ± standard deviation. Student’s t test was used for the comparison between the two groups, and a χ2 test was applied for comparing count data between the two groups. P < 0.05 was deemed statistically significant.
The TST and M-M groups were comparable, and no statistical differences were found between them regarding gender, age, or hemorrhoids grading (Table 1). The total effective rates of the TST and M-M groups were 99.5% (217/218) and 98.6% (218/221) respectively; the difference was not statistically significant (P = 0.322) (Table 2).
| Characteristic | TST group(n = 240) | M-M group(n = 240) | t orχ2 | P value |
| Age | 44.2 ± 16.5 | 45.7 ± 15.6 | 0.682 | 0.891 |
| Gender (male/female) | 123/117 | 119/121 | 0.133 | 0.715 |
| Hemorrhoids grading (III/IV) | 155/85 | 171/69 | 2.448 | 0.118 |
| Case history (yr) | 7.2 (0.5-17.0) | 6.8 (0.4-20) | 0.591 | 0.895 |
| Completed follow-up (n) | 218 | 221 |
| Group | Recovery | Effectiveness | Ineffectiveness |
| Tissue selecting therapy stapler | 210 | 7 | 1.000 |
| Milligan-Morgan hemorrhoidectomy | 208 | 10 | 3.000 |
| χ2 | 0.982 | ||
| P value | 0.322 |
The comparison between the two groups showed significant reductions in postoperative pain, intraoperative blood loss, urine retention, anal pendant expansion, operation time, and length of hospital stay in the TST group compared to M-M (all P < 0.01) (Table 3).
| Complication | TST group(n = 240) | M–M group(n = 240) | t orχ2 | P value |
| Postoperative pain (VAS) | ||||
| 12 h after the surgery | 5.08 ± 1.62 | 7.19 ± 2.01 | 9.451 | 0.000 |
| During first dressing change | 2.64 ± 0.87 | 4.34 ± 1.15 | 11.231 | 0.000 |
| During first defecation | 3.91 ± 1.47 | 5.63 ± 1.98 | 4.211 | 0.001 |
| Intraoperative blood loss | 2.45 ± 0.57 | 5.07 ± 1.14 | 13.246 | 0.000 |
| Urine retention after the surgery (n) | 22 | 47 | 10.579 | 0.001 |
| Anal pendant expansion after the surgery (VAS) | 2.35 ± 0.56 | 5.16 ± 1.42 | 12.781 | 0.000 |
| Operation time (min) | 18.3 ± 5.6 | 29.5 ± 8.2 | 7.439 | 0.000 |
| The length of hospital stay (d) | 5.3 ± 0.6 | 11.4 ± 1.8 | 11.651 | 0.000 |
The follow-up showed that no participants in either group had rectal or vaginal fistulas, and the rates of fecal incontinence, difficult bowel movement, intractable pain, and anal discharge were significantly lower in the TST group compared to the M-M group (all P < 0.05) (Table 4).
| Complication | TST Group(n = 218) | M-M Group(n = 221) | χ2 | P value |
| Rectal and vaginal fistula | 0 | 0 | ||
| Fecal incontinence | 3 | 16 | 9.110 | 0.003 |
| Difficult bowel movement | 1 | 9 | 6.438 | 0.011 |
| Intractable pain | 2 | 12 | 7.285 | 0.007 |
| Anal discharge | 3 | 23 | 16.065 | 0.000 |
The results of satisfaction survey indicated that the total satisfaction rate of TST group was significantly higher than that of M-M group (P < 0.01) (Table 5).
| Group | Satisfied | Somewhat satisfied | Not satisfied |
| Tissue selecting therapy stapler | 212 | 4 | 2 |
| Milligan-Morgan hemorrhoidectomy | 173 | 35 | 13 |
| χ2 | 8.197 | ||
| P value | 0.004 |
Hemorrhoidal disease is a common anal disorder in which anal cushions are pathologically enlarged and shift, and the blood stasis in perianal subcutaneous vascular plexus forms clumps. Its symptoms are pendant expansion, pain, bleeding, incarceration, and so on. Approximately 10%-20% of patients with such disease should undergo surgery[10]. The disease is often over-treated[11,12] as first, it is assumed that patients with hemorrhoidal symptoms must receive surgery. Haas et al[13] found that the hemorrhoidal symptoms in > 80% of operation cases could be eradicated by non-surgical means. Second, new techniques have been abused. Third, eradication of the disease has lead to excessive trauma. For instance, the Whitehead hemorrhoidectomy, devised to eradicate enlarged internal hemorrhoidal tissue, is associated with high rates of mucosal ectropion and anal stricture[14], which are far more distressing than hemorrhoidal disease itself. In recent years, several great changes have taken place in excisional hemorrhoidectomy. The surgery has changed from eradicative therapy (complete excision) to individualized therapy (selective excision)[15]. In 1937, Milligan and Morgan from St. Mark Hospital described a selective technique called the M-M hemorrhoidectomy that can reduce mucosal ectropion and anal stricture. However, it is associated with short-term complications, such as severe postoperative pain, delayed healing of the open wounds, great blood loss, urine retention, anal pendent expansion, and long-term complications, such as fecal incontinence, difficult bowel movement, intractable pain and anal discharge, which have prevented it from widespread use[16].
Since anal cushions were proposed by Thomson[17] in 1975, the understanding of the treatment has also changed radically[18,19]. Based on anal cushions, Longo[20] proposed a procedure for prolapse and hemorrhoids (PPH). Compared with traditional techniques, PPH is associated with less pain and shorter hospital stay[21], though it also has limitations. TST is a minimally invasive technique by which hemorrhoidal mucosa is excised and normal mucosa between hemorrhoids is kept. It is associated with fewer wounds, normal anal functions, and fewer complications[4,5].
This study found no significant difference in efficacy between TST and M-M, indicating that these methods have similar therapeutic effects in the treatment of severe prolapsing hemorrhoids. Secondly, the study has found statistically significant differences between TST and M-M in operating time, the length of hospital stay, postoperative anal pain, intraoperative blood loss, urine retention, and anal pendant expansion after the surgery. These findings show that TST is associated with less pain, a simpler operation, more rapid recovery, less blood loss and fewer complications compared with M-M. Thirdly, this study reveals that TST significant reduces long-term complications such as fecal incontinence, difficult bowel movement, intractable pain, and anal discharge, indicating that TST retains non-pathologic anal cushions without affecting anal functions, thereby avoiding to a great extent fecal urgency and incontinence[22]. Lastly, the results of the satisfaction survey indicate that TST is more acceptable than M-M. He et al[23] reported that the recovery rate of TST in the treatment of 300 patients with mixed hemorrhoids was 100%. Our study also shows that the rate and severity of postoperative pain and anal pendant expansion in TST group was much lower than in the M-M group. TST increased patients’ tolerance to the surgery and lowered the risks so as to cure severe prolapsing hemorrhoids with minimal invasion.
In summary, by TST, hemorrhoidal mucosa is excised and normal mucosa between hemorrhoids is kept. The technique could reduce wounds and complications and protect normal anal functions. Therefore, it is more suitable for the treatment of hemorrhoids. We suggest that TST be more widely used in clinical practice, as it is a safe minimally invasive technique.
Hemorrhoidal disease is due pathologic enlargement and shift of anal cushions and blood stasis in perianal subcutaneous vascular plexus. Milligan-Morgan hemorrhoidectomy (M-M), though wildly practiced, has some disadvantages such as postoperative pain and a long period of convalescence. Tissue selecting therapy stapler (TST) is a minimally invasive technique by which hemorrhoidal mucosa is excised and normal mucosa between hemorrhoids is kept. It is associated with fewer wounds, normal anal functions, and fewer complications.
With the consideration of the anal cushion contributing to the sense and fecal continence, surgeons pursue a modified technique to cut the pathologic anal cushion. TST is a minimally invasive technique by which hemorrhoidal mucosa is excised and normal mucosa between hemorrhoids is kept. It is associated with fewer wounds, normal anal functions and fewer complications.
In this randomized controlled trial, patients with severe prolapsing hemorrhoids were treated with either M-M or TST techniques. The therapeutic effects, operation security, and postoperative complications in the two groups were compared.
Excision of hemorrhoidal mucosa using the TST technique reduces wounds and complications, and protects normal anal functions. Therefore, it is more suitable for the treatment of hemorrhoids with minimal invasion. The results of this study indicate that TST should be more widely used for clinical treatment of prolapsed hemorrhoids.
In this study, the authors compared the therapeutic effects and postoperative complication rates in patients with severe prolapsing hemorrhoids treated with TST and M-M hemorrhoidectomy. Four hundred and eighty patients with severe prolapsing hemorrhoids were included. The study is well designed, and the results are interesting.
P- Reviewer: Ehrenpreis ED S- Editor: Yu J L- Editor: AmEditor E- Editor: Wang CH
| 1. | Argov S, Levandovsky O, Yarhi D. Milligan-Morgan hemorrhoidectomy under local anesthesia - an old operation that stood the test of time. A single-team experience with 2,280 operations. Int J Colorectal Dis. 2012;27:981-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Longo A. Treatment of hemorrhoidal disease by reduction of mucosa and hemorrhoidal prolapse with circular suturing device: a new procedure. Bologna: Munduzzi 1988; 777-784. |
| 3. | Fueglistaler P, Guenin MO, Montali I, Kern B, Peterli R, von Flüe M, Ackermann C. Long-term results after stapled hemorrhoidopexy: high patient satisfaction despite frequent postoperative symptoms. Dis Colon Rectum. 2007;50:204-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Lin HC, He QL, Ren DL, Peng H, Xie SK, Su D, Wang XX. Partial stapled hemorrhoidopexy: a minimally invasive technique for hemorrhoids. Surg Today. 2012;42:868-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Khubchandani IT. H.-C. Lin, D.-L. Ren, Q.-L. He, H. Peng, S.-K. Xie, D. Su, X.-X. Wang: Partial stapled hemorrhoidopexy versus circular stapled hemorrhoidopexy for grade III-IV prolapsing hemorrhoids: a two-year prospective controlled study. Tech Coloproctol. 2012;16:345; discussion 347-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Goligher JC. Surgery of the anus rectum and colon. London: Bailliere, Tindall; 93-149. |
| 7. | Yao LQ, Zhong YS, Sun YH, Ge SY, Liu HB, Zheng LW. Evaluation of the procedure for proplapse and hemorrhoids: three years’ experiences. Zhonghua Waike Zazhi. 2004;7:120-123. |
| 8. | Raahave D, Jepsen LV, Pedersen IK. Primary and repeated stapled hemorrhoidopexy for prolapsing hemorrhoids: follow-up to five years. Dis Colon Rectum. 2008;51:334-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Xu YD, Ren YM, Lin CF. Urine retention after the procedure for proplapse and hemorrhoids. Proc Clin Med. 2008;17:449-450. |
| 10. | Bleday R, Pena JP, Rothenberger DA, Goldberg SM, Buls JG. Symptomatic hemorrhoids: current incidence and complications of operative therapy. Dis Colon Rectum. 1992;35:477-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 151] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 11. | Marc G, Téllez-Ávila F. Current endoscopic ultrasound perspectives from 2013 digestive disease week meeting. Endosc Ultrasound. 2013;2:175-178. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | He Q, Wang C, Xu Y. Current endoscopic ultrasound perspectives from 2012 digestive disease week meeting. Endoscopic Ultrasound. 2012;1:114-116. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Haas PA, Fox TA, Haas GP. The pathogenesis of hemorrhoids. Dis Colon Rectum. 1984;27:442-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 121] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Wolff BG, Culp CE. The Whitehead hemorrhoidectomy. An unjustly maligned procedure. Dis Colon Rectum. 1988;31:587-590. [PubMed] |
| 15. | Laughlan K, Jayne DG, Jackson D, Rupprecht F, Ribaric G. Stapled haemorrhoidopexy compared to Milligan-Morgan and Ferguson haemorrhoidectomy: a systematic review. Int J Colorectal Dis. 2009;24:335-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 64] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 16. | Milligan ETC, Morgan CN, Naughton JLF, Office RR. Surgical anatomy of the anal canal and the operative treatment of hemorrhoids. Lancet. 1937;2:1119-1124. [RCA] [DOI] [Full Text] [Cited by in Crossref: 368] [Cited by in RCA: 263] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Thomson WH. The nature of haemorrhoids. Br J Surg. 1975;62:542-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 440] [Cited by in RCA: 328] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 18. | Guo J, Liu Z, Sun S, Wang S, Ge N, Liu X, Wang G, Liu W. Endosonography-assisted diagnosis and therapy of gastrointestinal submucosal tumors. Endosc Ultrasound. 2013;2:125-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Fusaroli P, Ceroni L, Caletti G. Forward-view Endoscopic Ultrasound: A Systematic Review of Diagnostic and Therapeutic Applications. Endosc Ultrasound. 2013;2:64-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | Longo A. Treatment of hemorrhoidal disease by reduction of mucosa and hemorrhoidal prolapse with a circular suturing device: a new procedure. Rome, Italy: Proceedings of the 6th World Congress of Endoscopic Surgery 1998; 3. |
| 21. | Ren DL, Luo ZB, Zhao J. The procedure for proplapse and hemorrhoids: a clinical experience with 1000 cases. Chin J Surg Integrat Trad West Med. 2005;11:231-236. |
| 22. | Cheetham MJ, Mortensen NJ, Nystrom PO, Kamm MA, Phillips RK. Persistent pain and faecal urgency after stapled haemorrhoidectomy. Lancet. 2000;356:730-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 211] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 23. | He P, Liu N. Treatment of mixed hemorrhoids with TST: a clinical report of 300 cases. J Colorect Anal Surg. 2011;17:175-176. |