Published online Feb 28, 2015. doi: 10.3748/wjg.v21.i8.2381
Peer-review started: July 16, 2014
First decision: August 27, 2014
Revised: September 11, 2014
Accepted: October 21, 2014
Article in press: October 21, 2014
Published online: February 28, 2015
Processing time: 227 Days and 2.8 Hours
AIM: To report our experience with single-port laparoscopic surgery (SPLS) for sigmoid volvulus (SV).
METHODS: Between October 2009 and April 2013, 10 patients underwent SPLS for SV. SPLS was performed transumbilically or through a predetermined stoma site. Conventional straight and rigid-type laparoscopic instruments were used. After intracorporeal, segmental resection of the affected sigmoid colon, the specimen was extracted through the single-incision site. Patient demographics and perioperative data were analyzed.
RESULTS: SPLS for SV was successful in all 10 patients (4, resection and primary anastomosis; 6, Hartmann’s procedure). The median operative time and postoperative hospitalization period were 168 (range, 85-315) min and 6.5 (range, 4-29) d, respectively. No intraoperative complications were noted; there were 2 postoperative complications, including 1 anastomotic leak.
CONCLUSION: SPLS was a safe and feasible therapeutic approach for SV, when performed by a surgeon experienced in conventional laparoscopic surgery.
Core tip: This paper describes our novel approach to single port laparoscopic surgery (SPLS) in patients with sigmoid volvulus (SV). Ever since minimally invasive surgery was pioneered, few reports have mentioned laparoscopic management of SV, and to our knowledge, reports on the management of SV using SPLS are even less common. Minimally invasive surgery is ideally suited for SV patients who, in developed nations, are typically elderly individuals with significant comorbidities. Despite the study limitations, our results provide support for the use of SPLS in SV patients.
- Citation: Choi BJ, Jeong WJ, Kim SJ, Lee SC. Single-port laparoscopic surgery for sigmoid volvulus. World J Gastroenterol 2015; 21(8): 2381-2386
- URL: https://www.wjgnet.com/1007-9327/full/v21/i8/2381.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i8.2381
In developing countries, sigmoid volvulus (SV) is a common cause of colon obstruction[1], but it is relatively rare in North America and Western Europe where it most commonly affects elderly patients[2]. Treatment typically involves appropriate resuscitation and non-operative decompression. In most cases, elective sigmoid resection follows because of the extremely high recurrence rate. The laparoscopic treatment of SV seems to be an attractive option because such minimal access surgery reduces surgical stress in elderly and frail patients. Additionally, the elongated colon and mesentery require little mobilization, allowing easy accomplishment of resection with primary anastomosis (RPA). However, since laparoscopic sigmoidectomy for SV was introduced in 1992, only a few publications have reported the feasibility and efficacy of this laparoscopic treatment for SV[3-8]. Recently, single-port laparoscopic surgery (SPLS) has emerged as a subtype of laparoscopy, maximizing the benefits of laparoscopic surgery. Since its introduction for the treatment of appendicitis and cholecystitis[9,10], SPLS has been widely used in various surgical cases. However, to our knowledge, reports on the management of SV using SPLS are rare. In this report, we have reviewed our experience with SPLS for the treatment of SV patients, and assessed the feasibility and efficacy of this technique.
Between August 2009 and August 2013, 11 SV patients underwent surgical treatment at Daejeon St. Mary Hospital, Daejeon, Korea. SPLS was performed by one surgeon in 10 consecutive SV patients; the current study retrospectively analyzed the data collected from these patients. The patients provided written informed consent prior to undergoing SPLS. The study was approved by the Institutional Review Board of Daejeon St. Mary’s Hospital (IRB code: DC14RISI0036). All patients were diagnosed with SV based on their medical history and plain abdominal radiographs, and the diagnoses were confirmed using computed tomography.
Patients with emergent conditions such as failed colonoscopic decompression or ischemic bowel were included. However, we excluded patients with evidence of bowel perforation or hemodynamic instability. Sigmoidoscopic detorsioning and rectal tube decompression were initially performed for all patients. The patients undergoing SPLS included 4 elective cases and 4 recurrent cases, after colonoscopic decompression, and 2 patients with failed decompression, including 1 with ischemic changes. Patient-controlled analgesia (PCA) was used during the immediate postoperative period. If needed, additional analgesics were also administered intravenously. One patient had a history of abdominal surgery (laparoscopic anterior resection due to sigmoid colon cancer). Patient demographics, perioperative outcomes, and morbidities were evaluated.
For the elective operations, a 2.5-3.0 cm, vertical incision was made at the umbilicus. When a Hartmann’s procedure was planned, an approximately 3.0 cm, left lower quadrant transverse incision was made at the selected colostomy site to introduce a single port. The abdomen was penetrated under direct vision using the Hansson technique. We used a homemade glove port, comprising an ALEXIS wound retractor and a surgical glove. Next, a commercial single-port (Octo port; Dalim, Seoul, Korea) was utilized. Pneumoperitoneum was established by insufflating the abdominal cavity to a pressure of 12 mmHg. A rigid laparoscope and instruments were used.
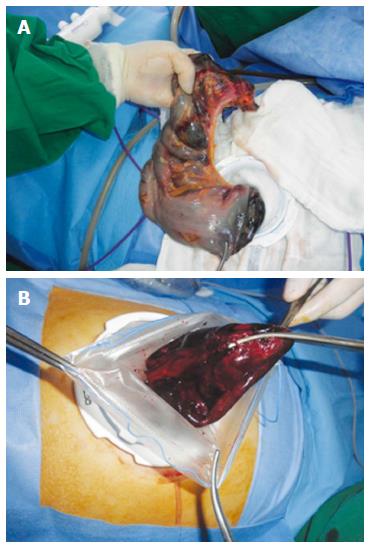
In cases of RPA, a surgical procedure similar to a multi-port laparoscopic sigmoid colectomy was performed. The redundant sigmoid colon, with its long, narrow-based mesentery, was mobilized using a medial approach. The inferior mesenteric vessels were dissected and ligated using a 5-mm Hemolock. The upper rectum was mobilized and transected using a linear stapler. The divided sigmoid loop was delivered using a pull-through pattern via the umbilical incision; the redundant part was resected (Figure 1A). The anvil of a circular stapler was secured to the proximal end of the bowel, the prepared colon was returned to the abdominal cavity, and the peritoneal cavity was re-insufflated. An end-to-end anastomosis was then performed through the anus.
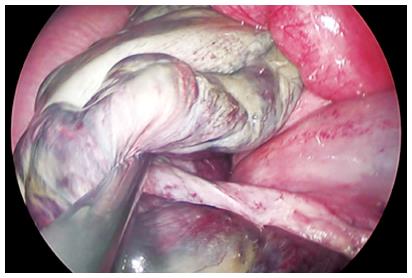
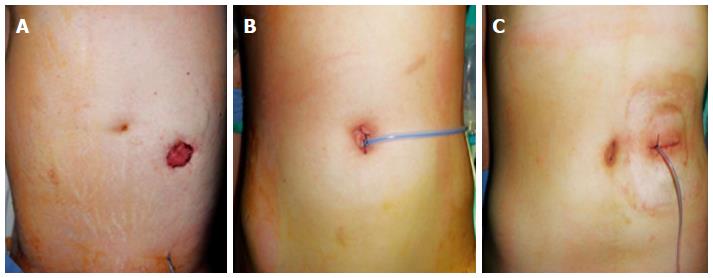
In patients undergoing Hartmann’s procedure, the distended sigmoid colon and long loop were visualized laparoscopically (Figure 2), and the distended bowel was decompressed using a trans-anal rectal tube or anal trocar insertion, or relieved by endo-needle puncture aspiration. After untwisting the rotated sigmoid loop, mobilization and dissection of the sigmoid mesocolon were performed in a manner similar to an RPA. However, unlike RPA, proximal colon resection was performed intracorporeally using another linear stapler, and the resected bowel loop was enveloped in a Lap-bag (Sejong Medical, Paju, Korea) and removed through the incision site (Figure 1B). The proximal stump was pulled out laparoscopically via the single-port site and an end-colostomy was established with maturation. Thus, in cases involving Hartmann’s procedure, no incision scar remained besides the colostomy site (Figure 3A).
The patient demographics and operative methods are shown in Table 1. The study included 7 men and 3 women, with a median age of 59.5 (range, 21-86) years and a median body mass index of 23.2 (range, 18.2-26.1) kg/m2. The perioperative data are shown in Table 2; SPLS for SV was successful in all patients. The median operative time and postoperative hospitalization period were 168 (range, 85-315) min and 6.5 (range, 4-29) d, respectively. The median time between surgery and the resumption of oral intake was 2.5 (range, 1-6) d. PCA was administered in all cases, with only 1 patient requiring additional analgesia. None of the patients demonstrated intraoperative complications. There was one postoperative anastomotic leak that was treated using single-port laparoscopic peritoneal lavage and Hartmann’s colostomy on postoperative day 3. The patient showed ileus and delayed recovery, but was finally discharged 26 d after the reoperation in good condition.
| Patient | Age (yr) | Sex | BMI (kg/m2) | Comorbidity | Mobility status | Endoscopic decompression | Operative method |
| 1 | 52 | M | 20.4 | Chronic alcoholic | - | Success | Elective RPA |
| 2 | 59 | M | 24.3 | Visual disability | Institutionalized | Success | Elective RPA |
| 3 | 21 | M | 25.6 | Intellectual disability | Institutionalized | Fair | Hartmann’s procedure |
| 4 | 36 | F | 24.2 | Schizophrenia | Institutionalized | Success | Semi-elective RPA |
| 5 | 70 | F | 22.2 | History of CVA, diabetes mellitus, Hypertension | Bedbound | Recurrence × 2 | Hartmann’s procedure |
| 6 | 60 | M | 21.3 | - | - | Success | Elective PRA |
| 7 | 86 | M | 18.2 | - | - | Fair | Hartmann’s procedure |
| 8 | 76 | M | 25.4 | History of CVA, Hypertension | Wheelchair-bound | Recurrence × 3 | Hartmann’s procedure |
| 9 | 43 | F | 20.3 | Schizophrenia | Institutionalized | Recurrence ≥ 4 | Hartmann’s procedure |
| 10 | 72 | M | 26.1 | Parkinson’s disease, asthma | Wheelchair-bound | Recurrence ≥ 4 | Hartmann’s procedure |
| Patient | Operative method | Operative time (min) | Time to oral intake (d) | Postoperative length of stay (d) | Postoperative complications |
| 1 | Elective RPA | 170 | 3 | 7 | - |
| 2 | Elective RPA | 225 | 2 | 6 | - |
| 3 | Hartmann’s procedure | 315 | 3 | 10 | Postoperative ileus |
| 4 | Semi-elective RPA | 90 | 3 | 6 | - |
| 5 | Hartmann’s procedure | 120 | 3 | 8 | - |
| 6 | Elective PRA | 250 | 6 | 29 | Anastomotic leakage, postoperative ileus |
| 7 | Hartmann’s procedure | 220 | 2 | 8 | - |
| 8 | Hartmann’s procedure | 105 | 1 | 4 | - |
| 9 | Hartmann’s procedure | 85 | 1 | 4 | - |
| 10 | Hartmann’s procedure | 165 | 1 | 4 | - |
During the median follow-up period of 17.5 (range, 8-55) mo, there were no recurrences or mortalities. Five of the 7 patients undergoing Hartmann’s procedure also underwent reversal of colostomy after a median period of 5 (range, 3-8) mo. We did not perform reversal of colostomy in 2 patients after consultation with their families; 1 patient was bedridden due to a cerebrovascular accident and had a percutaneous endoscopic gastrostomy and tracheostomy tube, and the other required a wheel chair for mobility due to Parkinson disease, and refused a colostomy closure operation. There were no stoma-related complications. Anastomosis site leakage occurred after stoma closure in 1 patient, who was subsequently treated by resection and re-anastomosis without fecal diversion, and discharged 7 d after the reoperation. Additionally, there were 2 wound infections after the stoma closure, but these were conservatively managed.
SV is the wrapping of the sigmoid colon around itself and its mesentery[2]. Factors associated with an increased risk include a redundant and mobile sigmoid colon with a narrow base at the mesenteric root, chronic constipation, advanced age, and institutionalized neuropsychiatric patients taking antipsychotic or anti-Parkinson drugs[11,12]. SV management involves endoscopic obstruction relief, rectal tube decompression, and prevention of recurrence through resection of the sigmoid colon[13]. Several studies have reported the surgical treatment of SV[13-15], and recently, laparoscopic attempts to minimize the surgical trauma and facilitate patient recovery have been occasionally reported[5,7,16]. Matsuoka et al[17] reported using reduced-port laparoscopic surgery in SV patients, and recommended that such minimal surgery be considered for elderly patients having high preoperative risks. Single-port laparoscopic sigmoid colectomy is not a new technique, with consistent reporting of the technique being used in patients with malignancies or benign conditions, such as rectal prolapse[18]. We have experience conducting single-port laparoscopic sigmoid colectomy for malignancies and using SPLS for dilated bowels caused by small bowel obstructions[19,20]. Therefore, we expected that SPLS could be safely and effectively performed in SV patients. In the current study, we evaluated 10 consecutive patients who underwent SPLS for SV and who obtained acceptable results.
As expected, the difficulties encountered during the initial stages of SPLS in the present patients included limited working space and manipulation of the long, dilated sigmoid colon. Intraoperative decompression of the dilated colon and the preparations for mesenteric dissection were elaborate and time-consuming. However, once the colon was decompressed, sigmoid resection was performed relatively easily. As mentioned by Liang et al[5], the medial to lateral approach was efficient for dissecting the sigmoid colon. Additionally, since SV is a benign disease, there was no need to mobilize the colon.
In this study, nonoperative decompression was successful in 8 of the 10 patients. However, 4 of the 8 patients who refused the subsequent surgical procedure, and were discharged, developed recurrent disease; 3 of the 4 patients with recurrence later underwent semi-elective surgery and 1 required emergent surgery after repeated colonoscopic decompressions. We performed Hartmann’s procedure in the 3 patients with recurrence who underwent semi-elective surgery and who had viable colons. These 3 patients had ambulatory disorders as well as serious co-morbidities, leading to the decision to perform the 2-stage operation, after discussion with the patients and their families. The patients undergoing Hartmann’s procedure actually had a shorter median operative time and shorter hospitalization period than those undergoing RPA (197.5 min vs 142.5 min and 6.5 d vs 6 d, respectively). One of the reasons for selecting Hartmann’s procedure in patients with recurrent SV was the large differences in the diameters of proximal and distal ends of the colon; anastomotic safety may decrease in patients with significantly different colon end diameters[15]. Additionally, a sigmoid resection performed through a left lower quadrant single incision at the proposed colostomy site was previously reported as an innovative minimal access technique for treating SV in debilitated patients with fecal incontinence[21].
SPLS was successfully completed in all patients; none required conversion to open laparotomy or switching to a multiport laparoscopic surgery. In two other series of 9 and 14 SV patients who underwent laparoscopic sigmoidectomy, the operative times were 115 (range, 45-145) min and 194.6 ± 32.4 min, respectively[5,7]. Our operative time (median, 168 min; range 85-315 min) was comparable. Our patients also demonstrated good postoperative recovery. With respect to analgesia, lengths of stay, and time to postoperative oral intake, the patients in our series did not demonstrate an improvement compared with patients in studies using conventional laparoscopic SV treatment[5,7,22]. Additionally, we did not experience any intraoperative complications such as bowel injuries or uncontrollable bleeding; only 2 postoperative complications were observed. One patient developed postoperative ileus, which was released after nasogastric tube drainage for 3 d. Anastomotic leakage occurred in one patient. Ironically, this patient was 1 of the 2 who did not have any comorbidities and 1 of 3 with normal mobility. The only suspicious risk factor for anastomotic dehiscence in this patient was the relatively large difference between the diameters and wall thicknesses of the proximal and distal colon ends. The reoperation was performed using SPLS through the present colostomy site, and the patient recovered well. None of the patients developed a wound infection, which is the most common postoperative complication after laparotomy for SV management[22,23]. However, wound infections occurred in 2 of the 5 patients who underwent colostomy closures. We performed the colostomy closures using SPLS, with the colostomy site acting as the single-port site. Thus, although there was a high rate of wound infections after colostomy closure, the wound problems associated with these small stoma site closures were milder and easier to manage than those occurring in the larger wound incisions associated with laparotomies. The vertical incision over the umbilicus or transverse scar after reversal of Hartmann’s procedure also showed excellent cosmetic benefits (Figure 3).
We acknowledge several study limitations, including the retrospective nature of the study, limited sample size, and patient selection bias. The patients had low body mass indexes, and only 1 patient had a history of abdominal surgery. However, SV is a rare disease, and we performed SPLS for all our consecutive SV patients. Thus, these data will be useful for experienced surgeons who plan single-port laparoscopic colectomies in various practice settings.
In conclusion, SPLS for SV management was safe and feasible in terms of minimal surgical complications and rapid recovery. In addition to the cosmetic advantages, the decrease in the incision numbers and lengths showed the technique’s potential for reducing postoperative pain and decreasing the incidence of postoperative wound infections among elderly and chronically ill patients. SPLS appears to be a reasonable option for the treatment of SV when performed by an experienced SPLS surgeon. Thus, more experience and prospective studies are required to confirm the utility of this technique.
Minimally invasive surgery seems to be ideally suited for sigmoid volvulus (SV) patients who, in developed nations, are typically elderly individuals with significant comorbidities.
Since the advent of minimally invasive surgery, there have been few reports of the laparoscopic management of SV, and very few reports have described the management of SV using single-port laparoscopic surgery (SPLS).
This retrospective study assessed the efficacy and safety of SV management using a single port laparoscopic technique. This technique is less invasive than commonly used methods, with comparable safety and efficacy.
These data will be useful for experienced surgeons who plan single port laparoscopic colectomies in various practice settings. The results of this study could be the basis for prospective comparative studies in the future.
SV is the wrapping of the sigmoid colon around itself and its mesentery. SPLS has emerged as a subtype of laparoscopy, maximizing the benefits of laparoscopic surgery. SPLS for SV was performed transumbilically or through a predetermined stoma site.
This is a retrospective study of 10 patients who underwent single port laproscopic sigmoid resection. This study includes 6 Hartmann's procedures, and 3 of them were performed in semi-elective condition as well.
P- Reviewer: Balaban YH, Li XL, Shah OJ S- Editor: Qi Y L- Editor: A E- Editor: Wang CH
| 1. | Bagarani M, Conde AS, Longo R, Italiano A, Terenzi A, Venuto G. Sigmoid volvulus in west Africa: a prospective study on surgical treatments. Dis Colon Rectum. 1993;36:186-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 40] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Raveenthiran V, Madiba TE, Atamanalp SS, De U. Volvulus of the sigmoid colon. Colorectal Dis. 2010;12:e1-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 72] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Sundin JA, Wasson D, McMillen MM, Ballantyne GH. Laparoscopic-assisted sigmoid colectomy for sigmoid volvulus. Surg Laparosc Endosc. 1992;2:353-358. [PubMed] |
| 4. | Targarona EM, D’Ambra M, Agusti AG, Trias M. Multimedia article. Laparoscopic treatment of chronic sigmoid volvulus in a young adult. Surg Endosc. 2005;19:1155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Liang JT, Lai HS, Lee PH. Elective laparoscopically assisted sigmoidectomy for the sigmoid volvulus. Surg Endosc. 2006;20:1772-1773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 34] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Liu KK, Leung MW, Wong BP, Chao NS, Chung KW, Kwok WK. Minimal access surgery for sigmoid volvulus in children. Pediatr Surg Int. 2006;22:1007-1008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Cartwright-Terry T, Phillips S, Greenslade GL, Dixon AR. Laparoscopy in the management of closed loop sigmoid volvulus. Colorectal Dis. 2008;10:370-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Choi SI, Lee SH. Laproscopic management of sigmoid volvlus for which endoscopic reduction had failed. J Korean Soc Coloproctol. 2008;24:390-393. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Pelosi MA, Pelosi MA. Laparoscopic appendectomy using a single umbilical puncture (minilaparoscopy). J Reprod Med. 1992;37:588-594. [PubMed] |
| 10. | Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg. 1997;84:695. [PubMed] |
| 11. | Kuzu MA, Aşlar AK, Soran A, Polat A, Topcu O, Hengirmen S. Emergent resection for acute sigmoid volvulus: results of 106 consecutive cases. Dis Colon Rectum. 2002;45:1085-1090. [PubMed] |
| 12. | Safioleas M, Chatziconstantinou C, Felekouras E, Stamatakos M, Papaconstantinou I, Smirnis A, Safioleas P, Kostakis A. Clinical considerations and therapeutic strategy for sigmoid volvulus in the elderly: a study of 33 cases. World J Gastroenterol. 2007;13:921-924. [PubMed] |
| 13. | Coban S, Yilmaz M, Terzi A, Yildiz F, Ozgor D, Ara C, Yologlu S, Kirimlioglu V. Resection and primary anastomosis with or without modified blow-hole colostomy for sigmoid volvulus. World J Gastroenterol. 2008;14:5590-5594; discussion 5593. [PubMed] |
| 14. | Gurel M, Alic B, Bac B, Keles C, Akgun Y, Boylu S. Intraoperative colonic irrigation in the treatment of acute sigmoid volvulus. Br J Surg. 1989;76:957-958. [PubMed] |
| 15. | Akcan A, Akyildiz H, Artis T, Yilmaz N, Sozuer E. Feasibility of single-stage resection and primary anastomosis in patients with acute noncomplicated sigmoid volvulus. Am J Surg. 2007;193:421-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Gordon-Weeks AN, Lorenzi B, Lim J, Cristaldi M. Laparoscopic-assisted endoscopic sigmoidopexy: a new surgical option for sigmoid volvulus. Dis Colon Rectum. 2011;54:645-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Matsuoka T, Osawa N, Yoh T, Hirakawa K. Umbilical incision laparoscopic surgery with one assist port for an elderly patient with recurrent sigmoid volvulus. BMJ Case Rep. 2012;2012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Adair J, Gromski MA, Nagle D. Single-incision laparoscopic sigmoidectomy and rectopexy case series. Am J Surg. 2011;202:243-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Kim SJ, Ryu GO, Choi BJ, Kim JG, Lee KJ, Lee SC, Oh ST. The short-term outcomes of conventional and single-port laparoscopic surgery for colorectal cancer. Ann Surg. 2011;254:933-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 125] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 20. | Choi BJ, Kim SJ, Lee SC, Lee JI. Single-port laparoscopic treatment of small bowel obstruction. Am J Surg. 2014;208:470-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Alhindawi R, Kelly N, Holubar S. Incisionless Hartmann’s procedure: an innovative minimal access technique for surgical treatment of sigmoid volvulus in debilitated patients with faecal incontinence. Tech Coloproctol. 2008;12:337-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Atamanalp SS. Treatment of sigmoid volvulus: a single-center experience of 952 patients over 46.5 years. Tech Coloproctol. 2013;17:561-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 23. | Raveenthiran V. Restorative resection of unprepared left-colon in gangrenous vs. viable sigmoid volvulus. Int J Colorectal Dis. 2004;19:258-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |