Published online Feb 14, 2015. doi: 10.3748/wjg.v21.i6.1703
Peer-review started: August 5, 2014
First decision: September 15, 2014
Revised: October 18, 2014
Accepted: December 14, 2014
Article in press: December 16, 2014
Published online: February 14, 2015
Processing time: 190 Days and 20.7 Hours
Roux-en-Y hepaticojejunostomy anastomosis is the treatment of choice for common hepatic duct injury type E2. It has been performed laparoscopically with the advancement of laparoscopic skill. Recently, a telemanipulative robotic surgical system was introduced, providing laparoscopic instruments with wrist-arm technology and 3-dimensional visualization of the operative field. We present a case of 36-year-old female patient who had undergone elective cholecystectomy 2 mo ago for gall stones and had a common bile duct injury during surgery. As the stricture was old and complete it could not be tackled endoscopically. We did a laparoscopic assisted adhesiolysis followed by robotic Roux-en-Y hepaticojejunostomy. No intraoperative complications or technical problems were encountered. Postoperative period was uneventful and she was discharged on the 4th postoperative day. At follow-up, she is doing well without evidence of jaundice or cholangitis. This is the first reported case of robotic hepaticojejunostomy following common bile duct injury. The hybrid technique gives the patient benefit of laparoscopic adhesiolysis and robotic suturing.
Core tip: Robotic surgery has the advantages of a 20 times magnified 3D vision for the surgeon. The intuitive and tremor free accurate movements of the robotic fingers make it an ideal tool to do fine reconstructive surgery. Hepaticojejunostomy is one such surgery specially when done for bile duct injury that occurred during cholecystectomy. We present the first ever reported robotic hepaticojejunostomy for iatrogenic bile duct injury.
- Citation: Prasad A, De S, Mishra P, Tiwari A. Robotic assisted Roux-en-Y hepaticojejunostomy in a post-cholecystectomy type E2 bile duct injury. World J Gastroenterol 2015; 21(6): 1703-1706
- URL: https://www.wjgnet.com/1007-9327/full/v21/i6/1703.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i6.1703
Although seen with any operation involving right upper quadrant dissection, injuries occurring during or following cholecystectomy account for more than 80% of all iatrogenic bile duct injuries. During laparoscopic or open cholecystectomy, injury to the common bile duct is an unusual but devastating complication[1]. Inflammation in the porta, variable biliary anatomy, inappropriate exposure, aggressive attempts at hemostasis, and surgeon inexperience are commonly cited risk factors. Early reports suggested that surgical inexperience, performing less than 20 laparoscopic cholecystectomies, was highly correlated with bile duct injury, evidence has suggested that visual misperception accounts for 97% of iatrogenic biliary injuries and technical skill or knowledge accounts for only 3%. With sufficient cephalad retraction of the gallbladder fundus, the cystic duct overlies the common hepatic duct, running in a parallel path[2]. Without inferolateral traction of the gallbladder infundibulum to dissociate these structures, dissection of the apparent cystic duct may actually include the common hepatic duct, placing it in jeopardy. By retracting Hartmann’s pouch inferolaterally, and opening the triangle of Calot, the cystic duct is displaced from the porta, no longer collinear with the hepatic duct. The use of a 30-degree laparoscope is useful to provide adequate visualization of the critical view of safety during laparoscopic cholecystectomy[3]. Also, in many of these cases, a confirmation bias occurs, in which surgeons tend to rely on evidence that supports their perception while simultaneously discounting visual cues that suggest an alternative explanation. Confirmation bias helps explain why most bile duct injuries are identified in the postoperative setting, not intraoperatively. The multifactorial nature of biliary injury highlights the concept that injury avoidance consists of many levels of protective mechanisms[4]. Surgeon knowledge of biliary anatomy and aberrant anatomy, use of an angled laparoscope, appropriate and directed traction and counter-traction on the gallbladder, sufficient suspicion of findings that discount the current perspective, and converting to an open operation at the earliest suspicion can help decrease the likelihood of biliary injury. Although the use of routine versus selective cholangiography is controversial, evidence has suggested that cholangiography does not completely avoid bile duct injury, but may reduce the incidence and extent of injury[5]. The original analysis of biliary reconstruction was based on the Bismuth classification, and has been modified by Strasberg. Classification of bile duct injuries is determined by location of injury and helps guide later surgical reconstruction[6]. Among postoperative bile duct strictures, types E1 and E2 involve the common hepatic duct but not the bifurcation, with type E1 having a stump of more than 2 cm of the common hepatic duct below the confluence and type E2 being within 2 cm of the confluence. Type E3 strictures occur at the confluence preserving the extrahepatic ducts and, in type E4, the structuring process includes the extrahepatic biliary tree. Type E5 strictures involve aberrant right hepatic duct anatomy, with injury to the aberrant duct and common hepatic duct.
The standard treatment procedure for a type E2 stricture is a resection of the injured segment with mucosa to mucosa anastomosis using a Roux-en-Y jejunal limb[7]. Choledochoduodenostomy is not done because most injuries to the bile duct occur higher in the biliary tree, close to the hilum, thus not allowing for tension-free anastomosis to the duodenum. Recently, many centers have reported their experience with laparoscopic Roux-en-Y hepaticojejunostomy. Although the use of laparoscopy to do the procedure has found to be feasible, most of these reports suggested that these procedures were complicated by technical difficulties. The use of da Vinci Robotic Surgical System helps decrease these technical difficulties. The da Vinci robot provides a three-dimensional vision instead of a two dimensional one through the laparoscope. The Robotic system also provides other advantages like reduction of tremor and scaling of motion which further increase the precision of the procedure. But the biggest advantage is the use wristed instrumentation which provides additional degrees of mobility compared to the restriction of the laparoscopic systems. We used the daVinci robot to do an Roux-en-Y Hepaticojejunostomy in a 36 years old female patient with Type E2 CBD injury post cholecystectomy.
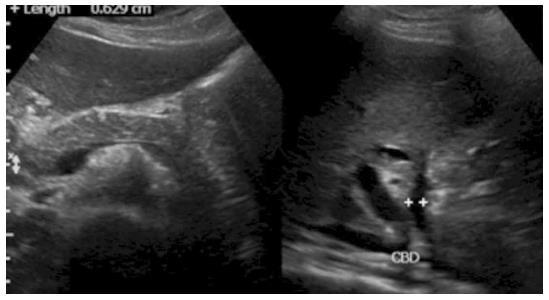
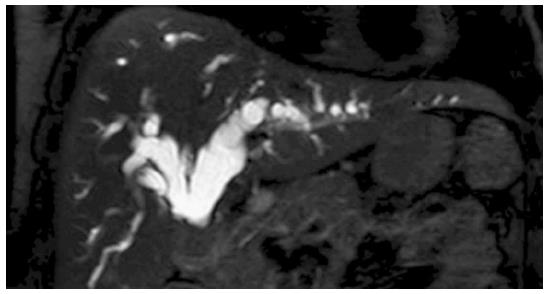
Our patient was a female of 36 years and came to us with multiple episodes of abdominal pain with deep icterus. She gave history of undergoing an elective open cholecystectomy at another hospital two months ago for gall stone disease. Her liver function tests were heavily deranged with high direct bilirubin (> 20 mg/dL) and OT/PT (538/422 mg/dL) and alkaline phosphatase (758 mg/dL). Ultrasonography demonstrated mild hepatomegaly with dilated intrahepatic biliary radicles (Figure 1). An magnetic resonance cholangiopancreatography scan (Figure 2) revealed a tight short segment stricture in the common hepatic duct with gross intrahepatic biliary radical dilatation. Opinion was sought from gastroenterologist who felt that the stricture is not passable by Encoscopic Retrograde Cholangio-Pancreatography and surgical option has to be tried. The patient underwent laparoscopic adhesiolysis and da Vinci robotic Roux En Y hepaticojejunostomy.
After placing the patient in supine position, pneumoperitoneum was created upto 12 mmHg using the Veress needle. Three 5 mm trocars were inserted to carry out the adhesiolysis. We then placed the camera and instruments and the table was placed in reverse Trendelenburg and right up position. This allowed the intestines to fall away from the operating field Alongwith cephalad retraction to the liver the porta hepatis was exposed. Laparoscopic adhesiolysis was done with the help of a suction and cautery. The porta was freed from the duodenum and the transverse colon. Bile was aspirated from the confluence.
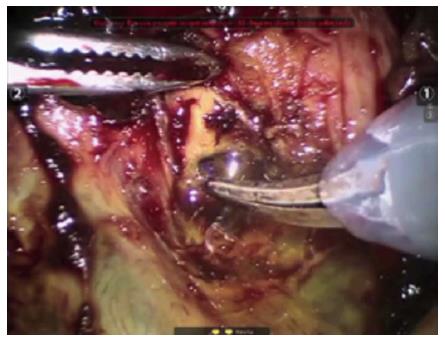
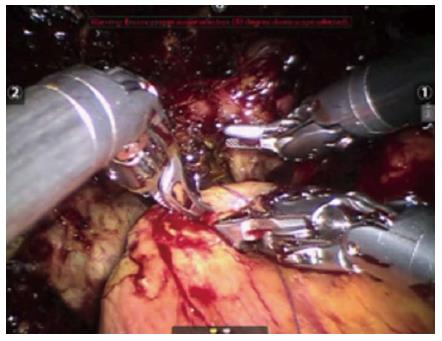
The robot was docked. Three 12-mm robotic trocars for camera and accessory device were applied. The jejunum was divided at 40 cm from the DJ flexure by an endoscopic stapler. Side-to-side enteroenterostomy anastomosis was done with the help of endoscopic stapler. The bile duct was opened (Figure 3) and was anastomosed to a Roux loop of jejunum with an antecolic Roux-en-Y end-to-side hepaticojejunostomy. The anastomoses was made using 3 0 Vicryl sutures at each of the corners (Figure 4). The hepatico-jejunostomy and jejuno-jejunostomy were re-checked for proper lie, bile leak and hemostasis. A drain was placed in the subhepatic region. The fascial and skin incisions were closed.
Postoperatively, the patient was managed conservatively with i.v. antibiotics, analgesics and fluids. The subhepatic drain showed minimal drainage and was removed on second post operative day. She was started on liquids on the third post operative day and progressed to normal diet on the fourth postoperative day. She was discharged without any complications. On follow up, she is doing well without any complaints.
The first uses of laparoscopic surgery were in the field of hepato-biliary surgery i.e., cholecystectomy. Following advancements in the camera and instruments and the increased skill of surgeons, Minimal access surgery has invaded all parts of the body today. But the use of laparoscopy in the field of hepato-biliary surgery still remains restricted to cholecystectomies. This is mostly due to the limited exposure present in the area, along with dense adhesions increasing the risk of visceral injury. The instruments of laparoscopy are rigid in nature with limited degrees of freedom. This coupled with the fulcrum effect of laparoscopy which takes the movement away from the wrist and fingers to the elbow and 2-dimensional imaging, are the main contributors to the limitations of the laparoscopic approach[8]. Robotic surgery becomes a great tool in hepato biliary by overcoming these shortcomings.
The daVinci robot has a three dimensional vision compared to the two dimensional view of the laparoscope which provides for the surgeon to be immersed in the oppressive field. Secondly, the motion scaling and tremor reduction software increase the precision of the surgery and decrease blood loss. However, the main advantage of the da Vinci robot is the use of the wristed instruments for doing fine dissection in areas of dense adhesions and fine suturing of hepaticojejunostomy and jejunojejunostomy anastomoses[9]. It might well be that in the future, advanced hepato biliary procedures like hepaticojejunostomy and Whipple’s procedure may be done by robotic surgery.
Robotic surgery, with its implications in urologic and gynaecologic surgery, has had multiple mention in case reports. A few cases of hepaticojejunostomy for choledochal cysts have also been reported but no reports have been found for a Roux-en-Y hepaticojejunostomy for a biliary injury following cholecystectomy[10,11].
On the other side of the coin, the disadvantages includes the bulky hardware which makes it impossible for the robot to be moved to other theatres. Although the lack of haptic feedback and loss of tactile sensation are propagated by noon believers to be the biggest obstacle, but the magnified three dimensional vision more than compensates for it. Finally, in a country like India, the increased initial cost of the machine along with high maintenance cost prevents it’s penetration into peripheral areas[12]. Although many people advocate a steep learning curve for advanced laparoscopic surgery, but the ease of dissection and suturing techniques with the robotic technique greatly reduce the learning curve.
Finally, we would like to say that the use of robotic surgery has immense scope in hepato biliary surgery with advanced surgeries like hepaticojejunostomy, CBD exploration and pancreaticoduodenectomy being facilitated by the ease of Robotic suturing[13].
Summarising we are reporting a case of 36 years old female with a type E2 biliary injury and the use of daVinci surgical system to create a Roux-en-Y Hepaticojejunostomy. The most technically challenging step of this operation is the creation of the hepaticojejunostomy anastomosis. The daVinci surgical system triumphs over laparoscopy due to the ease of the suturing with the endowristed instruments. This is the first reported case of robotic Roux-en-Y hepaticojejunostomy following common bile duct injury. The hybrid technique gives the patient benefit of laparoscopic adhesiolysis and robotic suturing. But further experience is needed to evaluate the advantages on surgical technique and it is effect on decreased hospital stay for patients.
P- Reviewer: Ogura T, Xu Z S- Editor: Ma YJ L- Editor: A E- Editor: Liu XM
| 1. | Shimura H, Tanaka M, Shimizu S, Mizumoto K. Laparoscopic treatment of congenital choledochal cyst. Surg Endosc. 1998;12:1268-1271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 46] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Tan HL, Shankar KR, Ford WD. Laparoscopic resection of type I choledochal cyst. Surg Endosc. 2003;17:1495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Diao M, Li L, Li Q, Ye M, Cheng W. Single-incision versus conventional laparoscopic cyst excision and Roux-Y hepaticojejunostomy for children with choledochal cysts: a case-control study. World J Surg. 2013;37:1707-1713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Diao M, Li L, Cheng W. Initial experience of single-incision laparoscopic hepaticojejunostomy using conventional instruments for correctable biliary atresia. J Laparoendosc Adv Surg Tech A. 2012;22:615-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Tanaka M, Shimizu S, Mizumoto K, Yokohata K, Chijiiwa K, Yamaguchi K, Ogawa Y. Laparoscopically assisted resection of choledochal cyst and Roux-en-Y reconstruction. Surg Endosc. 2001;15:545-552. [PubMed] |
| 6. | Ballantyne GH, Moll F. The da Vinci telerobotic surgical system: the virtual operative field and telepresence surgery. Surg Clin North Am. 2003;83:1293-1304, vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 153] [Article Influence: 7.3] [Reference Citation Analysis (1)] |
| 7. | Lanfranco AR, Castellanos AE, Desai JP, Meyers WC. Robotic surgery: a current perspective. Ann Surg. 2004;239:14-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 761] [Cited by in RCA: 687] [Article Influence: 32.7] [Reference Citation Analysis (0)] |
| 8. | Horgan S, Vanuno D. Robots in laparoscopic surgery. J Laparoendosc Adv Surg Tech A. 2001;11:415-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 195] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 9. | Hazey JW, Melvin WS. Robot-assisted general surgery. Semin Laparosc Surg. 2004;11:107-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Cadière GB, Himpens J, Germay O, Izizaw R, Degueldre M, Vandromme J, Capelluto E, Bruyns J. Feasibility of robotic laparoscopic surgery: 146 cases. World J Surg. 2001;25:1467-1477. [PubMed] |
| 11. | Woo R, Le D, Albanese CT, Kim SS. Robot-assisted laparoscopic resection of a type I choledochal cyst in a child. J Laparoendosc Adv Surg Tech A. 2006;16:179-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 92] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 12. | Kang CM, Chi HS, Kim JY, Choi GH, Kim KS, Choi JS, Lee WJ, Kim BR. A case of robot-assisted excision of choledochal cyst, hepaticojejunostomy, and extracorporeal Roux-en-y anastomosis using the da Vinci surgical system. Surg Laparosc Endosc Percutan Tech. 2007;17:538-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Meehan JJ, Elliott S, Sandler A. The robotic approach to complex hepatobiliary anomalies in children: preliminary report. J Pediatr Surg. 2007;42:2110-2114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 76] [Article Influence: 4.2] [Reference Citation Analysis (0)] |