Published online Feb 7, 2015. doi: 10.3748/wjg.v21.i5.1663
Peer-review started: June 3, 2014
First decision: August 15, 2014
Revised: September 25, 2014
Accepted: November 19, 2014
Article in press: November 19, 2014
Published online: February 7, 2015
Processing time: 251 Days and 23.3 Hours
This report presents a case involving a unique observation of a high-grade squamous dysplasia involving the entire esophagus. Dysplastic cells were located exclusively in the basal portion of the esophageal squamous epithelium. The findings were documented using histologic analysis of the step-biopsies from the entire esophagus, histologic examination of the esophagectomy-specimen, immunohistochemical analysis, and molecular pathologic analysis of the p53 gene. A minimally invasive total esophagectomy was performed at the Department of Surgery of the University of Cologne, and histologic analysis of the resection specimen confirmed extensive high-grade dysplasia involving the oral resection margin, but no invasive carcinoma. This case does not fit the current World Health Organization (WHO) definition of high-grade squamous cell dysplasia, which requires full-thickness involvement of the squamous epithelium. Thus, the WHO criteria should probably be reconsidered in order to allow for a diagnosis of high-grade dysplasia in cases where dysplastic cells are exclusively located in the basal layer of the esophageal squamous epithelium.
Core tip: An unusual case of high-grade squamous cell dysplasia involving the entire esophagus with dysplastic cells located exclusively in the basal portion of the esophageal squamous epithelium is reported. The analyses of results from step-biopsies of the entire esophagus were obtained using histologic and immunohistochemical analyses. Molecular pathologic analysis showed mutation of the p53 gene. The current World Health Organization (WHO) definition of high-grade squamous dysplasia requires full-thickness involvement of the squamous epithelium, which was not present in the current case. Therefore, we recommend that the WHO criteria should be reconsidered and revised.
- Citation: Sarbia M, Wolfer S, Karimi D, Eimiller A. High-grade dysplasia, restricted to the basal cell layer involving the entire esophagus. World J Gastroenterol 2015; 21(5): 1663-1665
- URL: https://www.wjgnet.com/1007-9327/full/v21/i5/1663.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i5.1663
The current World Health Organization (WHO) classification of tumors of the digestive system classifies precursor lesions of esophageal squamous cell carcinoma as either low-grade or high-grade intraepithelial neoplasia. In a low-grade intraepithelial neoplasia, the cytologic abnormalities are confined to the lower half of the epithelium, whereas the abnormalities in a high-grade intraepithelial neoplasia also involve the upper half of the epithelium with greater cytologic alterations[1]. We present a case of high-grade dysplasia (intraepithelial neoplasia), involving nearly the entire length of the esophagus, which was located in the lower third of the squamous epithelium.
A 63-year-old male with a longstanding history of pipe smoking was admitted for an evaluation by a gastroenterologist. The patient complained of a progressive dysphagia over a period of about ten years. Preliminary endoscopic examination showed a stenosis of the esophagus 15-25 cm from the incisors and a granular whitish discoloration of the entire esophagus (Figure 1). The rest of the upper gastrointestinal tract appeared normal.
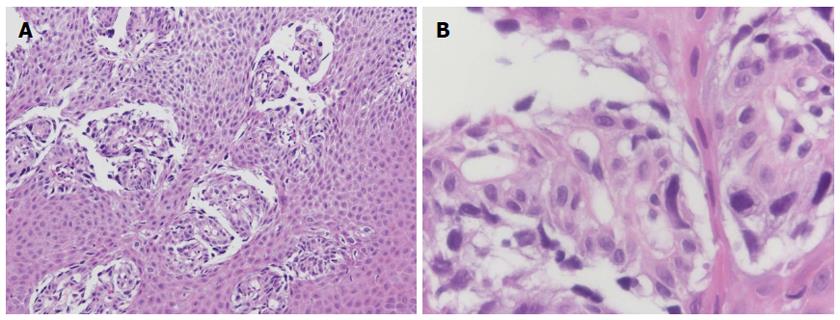
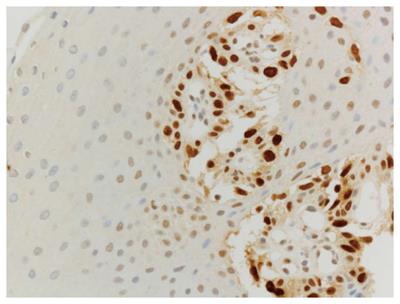
The initial forceps biopsies showed cells with highly atypical nuclei in the basal third of the squamous epithelium, whereas the upper layers were entirely normal (Figure 2). The squamous epithelium showed loss of cell cohesion to the subepithelial stroma. Additionally, the atypical cells were characterized by a poorly cohesive arrangement. In addition to dysplasia, virus-induced changes were considered. However, immunohistochemistry for herpes virus was negative. The atypical cells were positive for p53 (Figure 3). Due to the unusual presentation, doubts on the dysplastic nature of the atypical cells remained. Therefore, molecular analysis for p53-mutation was performed, revealing a point mutation in codon 220, which results in the replacement of a tyrosine by a cysteine. Polymerase chain reaction analysis showed no evidence of herpes simplex virus types 1 and 2. Additional immunohistochemical analysis displayed membranous expression of E-cadherin and β-catenin in the atypical cells. No nuclear expression of β-catenin was found. The atypical cells were positive for cytokeratin 5/6 and 7, but negative for p63. There was no presence of full-thickness involvement or involvement of the upper half of the squamous epithelium by dysplastic cells in any of the biopsies. Additionally, the atypical cells had 100% Ki-67 labeling, indicating high proliferative activity. These findings led to a diagnosis of high-grade squamous cell dysplasia.
A total of 40 quadrant biopsies starting 2.5 cm from the gastroesophageal junction up to 2.5 cm aboral from the upper esophageal sphincter were performed. In 25/40 biopsies, the above-described basal pattern of dysplastic cells was present. The remaining biopsies presented normal esophageal squamous epithelium. There was no indication of either full-thickness involvement of the squamous epithelium by dysplastic cells or invasion of the subepithelial stroma or the submucosa in any of the biopsies.
The patient was then admitted to the Department of Gastrointestinal Endoscopy of the University of Hamburg for consideration for possible endoscopic therapy, which was unsuccessful due to the extension of the process. Subsequently, a minimally invasive total esophagectomy was performed in April 2013 at the Department of Surgery of the University of Cologne. Histologic analysis of the resection specimen showed extensive high-grade dysplasia involving the oral resection margin, but no invasive carcinoma. Fourteen regional lymph nodes were free of tumor tissue.
The unusual cell type described here was characterized as being neoplastic. However, it may be controversial whether the atypical cells are characterized by glandular or squamous differentiation. In our opinion, squamous differentiation was present as indicated by the presence of the spindle-shaped cells, the immunohistochemical demonstration of cytokeratin 5/6 expression, and the extension of the tumor in the esophagus. Thus, if a glandular lesion is to be considered, one would expect to find some glandular precursor lesion such as Barrett’s esophagus. Moreover, the patients’ history of tobacco usage points to a typical squamous cell carcinogenesis in the esophagus.
Esophageal squamous cell dysplasia is usually found adjacent to invasive squamous cell carcinoma and is more frequent in the early than in advanced cancer stages[2]. Squamous dysplasia without concomitant carcinoma in low incidence countries of esophageal cancer, such as Germany, is usually displayed as a small lesion only detectable after meticulous endoscopic examination[3]. Histologic analysis alone does not provide sufficient information regarding the underlying causes for the unusual growth pattern of dysplastic cells. However, it is tempting to speculate that the dysplastic cells, in fact, did not attain the full malignant phenotype, resulting in the dependence on a special niche to support growth and survival. The basal portion of the squamous epithelium is the compartment where the esophageal stem cells are located. Thus, a distinct composition of growth factors and/or the short distance to submucosal blood vessels may support the growth of cells with incomplete malignant capacities[4].
In addition to reporting an unusual case, our observation points to a potential problem in the current WHO definition of esophageal high-grade squamous dysplasia. Thus, a strict adherence to the criteria that demand severe cytologic alterations and involvement of the upper half of the squamous epithelium would not allow the diagnosis of high-grade dysplasia and probably result in substantial underdiagnosis. Therefore, it should be taken into consideration whether the presence of severe cytologic alterations alone are sufficient for diagnosing high-grade squamous dysplasia.
A 63-year-old male with a history of tobacco usage presented with progressive dysphagia.
Esophageal stenosis and discoloration of the esophageal epithelium.
Virus esophagitis, intraepithelial neoplasia.
Squamous high-grade intraepithelial neoplasia.
The patient was treated with a minimally invasive total esophagectomy.
This manuscript is an interesting “case report” with new information.
P- Reviewer: Franzen T, Kim GH, Lee SW S- Editor: Ma YJ L- Editor: A E- Editor: Ma S
| 1. | Montgomery E, Field JK, Boffetta P, Daigo Y, Shimizu M. Squamous cell carcinoma of the esophagus. WHO Classification of Tumours of the Digestive System. Lyon: IARC 2010; 18-24. |
| 2. | Kuwano H. Peculiar histopathologic features of esophageal cancer. Surg Today. 1998;28:573-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Ide E, Carneiro FO, Frazão MS, Chaves DM, Sallum RA, de Moura EG, Sakai P, Cecconello I, Maluf-Filho F. Endoscopic Detection of Early Esophageal Squamous Cell Carcinoma in Patients with Achalasia: Narrow-Band Imaging versus Lugol’s Staining. J Oncol. 2013;2013:736756. [PubMed] |
| 4. | Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000;100:57-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19834] [Cited by in RCA: 19513] [Article Influence: 780.5] [Reference Citation Analysis (0)] |