Published online Feb 7, 2015. doi: 10.3748/wjg.v21.i5.1546
Peer-review started: June 16, 2014
First decision: July 21, 2014
Revised: July 29, 2014
Accepted: October 15, 2014
Article in press: October 15, 2014
Published online: February 7, 2015
Processing time: 240 Days and 20.2 Hours
AIM: To evaluate short-type-single-balloon enteroscope (SBE) with passive-bending, high-force transmission functions for endoscopic retrograde cholangiopancreatography (ERCP) in patients with Roux-en-Y anastomosis.
METHODS: Short-type SBE with this technology (SIF-Y0004-V01; working length, 1520 mm; channel diameter, 3.2 mm) was used to perform 50 ERCP procedures in 37 patients with Roux-en-Y anastomosis. The rate of reaching the blind end, time required to reach the blind end, diagnostic and therapeutic success rates, and procedure time and complications were studied retrospectively and compared with the results of 34 sessions of ERCP performed using a short-type SBE without this technology (SIF-Y0004; working length, 1520 mm; channel diameter, 3.2 mm) in 25 patients.
RESULTS: The rate of reaching the blind end was 90% with SIF-Y0004-V01 and 91% with SIF-Y0004 (P = 0.59). The median time required to reach the papilla was significantly shorter with SIF-Y0004-V01 than with SIF-Y0004 (16 min vs 24 min, P = 0.04). The diagnostic success rate was 93% with SIF-Y0004-V01 and 84% with SIF-Y0004 (P = 0.17). The therapeutic success rate was 95% with SIF-Y0004-V01 and 96% with SIF-Y0004 (P = 0.68). The median procedure time was 40 min with SIF-Y0004-V01 and 36 min with SIF-Y0004 (P = 0.50). The incidence of hyperamylasemia was 6.0% in the SIF-Y0004-V01 group and 14.7% in the SIF-Y0004 group (P = 0.723). The incidence of pancreatitis was 0% in the SIF-Y0004-V01 group and 5.9% in the SIF-Y0004 group (P > 0.999). The incidence of gastrointestinal perforation was 2.0% (1/50) in the SIF-Y0004-V01 group and 2.9% (1/34) in the SIF-Y0004 group (P > 0.999).
CONCLUSION: SIF-Y0004-V01 is useful for ERCP in patients with Roux-en-Y anastomosis and may reduce the time required to reach the blind end.
Core tip: We performed endoscopic retrograde cholangiopancreatography (ERCP) with a short-type single-balloon enteroscope with passive-bending and high-force transmission functions (working length, 1520 mm; channel diameter, 3.2 mm), and evaluated its effectiveness and compared results with normal short-type single-balloon enteroscope. This technology is expected to facilitate ERCP after intestinal reconstruction. In our study, the rate of reaching the blind end did not differ, however the median time required to reach the blind end was significantly shorter, and therefore this scope is useful for ERCP in patients with a Roux-en-Y anastomosis.
- Citation: Yamauchi H, Kida M, Okuwaki K, Miyazawa S, Iwai T, Tokunaga S, Takezawa M, Imaizumi H, Koizumi W. Passive-bending, short-type single-balloon enteroscope for endoscopic retrograde cholangiopancreatography in Roux-en-Y anastomosis patients. World J Gastroenterol 2015; 21(5): 1546-1553
- URL: https://www.wjgnet.com/1007-9327/full/v21/i5/1546.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i5.1546
The long-type double-balloon enteroscope (DBE) was introduced by Yamamoto et al[1] for the purpose of diagnosis and treatment of the small intestine. The first report of DBE-assisted endoscopic retrograde cholangiopancreatography (ERCP) was reported by Haruta et al[2] in patients with Roux-en-Y (R-Y) hepaticojejunostomy after liver transplantation.
The advent of the balloon enteroscope has improved the outcomes of ERCP in patients with surgically altered anatomy, and many recent studies have reported that single-balloon endoscope (SBE)-assisted ERCP[3-7] and DBE-assisted ERCP[8-12] are useful[3-15]. However, performing ERCP with a balloon enteroscope can be challenging, and several problems remain to be solved. For example, balloon enteroscopes lack a lifting device, and the narrow channel diameter precludes the use of wide-guided devices. The development of improved models of endoscopes and specialized devices is needed to improve the rate of reaching the papilla of Vater or choledochojejunal anastomosis (the blind end) and to reliably perform treatment procedures.
We evaluated the usefulness of a short-type SBE (SIF-Y0004; working length, 1520 mm; channel diameter, 3.2 mm) in postoperative patients with reconstructed intestines who underwent ERCP[4]. This scope allowed most wire-guided devices to be used and facilitated treatment procedures. Because a short-type SBE has a short working length, a decreased rate of reaching the blind end was a matter of concern. However, the rate of reaching the blind end with a short-type SBE is similar to that with a conventional SBE (SIF-Q260; Olympus Medical Systems)[7]. The rate of reaching the blind end during ERCP in patients who have undergone surgical reconstruction of the bowel with a balloon enteroscope is generally higher than 80%, but differs among hospitals[3,5,6,8,10]. Similar results have been obtained with an SBE and a DBE[13,14]. However, performing ERCP with a balloon enteroscope remains challenging mainly because of two factors: difficulty in reaching the blind end caused by postoperative adhesions and sharp bends at anastomoses, and limited availability of devices that can be used with a balloon enteroscope. To solve these problems, a short-type SBE equipped with passive bending (PB) section and high-force transmission (HFT) functions (SIF-Y0004-V01; working length, 1520 mm; channel diameter, 3.2 mm; Olympus Medical Systems; Tokyo, Japan) was developed.
It was reported that colonoscopes equipped with this technology can pass through the intestine with adhesions or hairpin bends, without distending the intestine, potentially causing less discomfort and speeding the insertion time as compared with a conventional colonoscope[15-18]. This technology is expected to facilitate ERCP after intestinal reconstruction[19]. We evaluated the performance of SIF-Y0004-V01 for ERCP in patients with R-Y anastomosis and compared our results with the outcomes of ERCP performed with SIF-Y0004.
Between June 2011 and January 2014, we performed 84 ERCP procedures in 62 patients with R-Y anastomosis. SIF-Y0004-V01 was used to perform 50 procedures in 37 patients (SIF-Y0004-V01 group), and SIF-Y0004 was used to perform in 34 procedures in 25 patients (SIF-Y0004 group). As for patient characteristics, the number of patients with portal lymph-node metastasis after surgery for gastric cancer was significantly higher in the SIF-Y0004 group (P = 0.005). Factors likely to influence the rate of reaching the blind end, such as abdominal surgery and peritoneal dissemination, did not differ significantly between the groups. The baseline characteristics of the patients are shown in Table 1.
| Characteristic | SIF-Y0004-V01 (n = 50) | SIF-Y0004 (n = 34) | P value | All SBE-assisted ERCP (n = 84) |
| Reconstruction method | ||||
| Roux-en-Y gastrectomy | 34 (68) | 29 (85) | 0.124 | 63 (75) |
| Roux-en-Y hepaticojejunostomy | 16 (32) | 5 (17) | 21 (25) | |
| Age, (yr) (mean ± SD) | 71.4 ± 9.2 | 70.0 ± 11.0 | 0.529 | 70.8 ± 9.9 |
| Sex | ||||
| Male | 40 (80) | 31 (91) | 0.168 | 71 (85) |
| Female | 10 (20) | 3 (9) | 13 (15) | |
| Reasons for surgery | ||||
| Gastric ulcer | 0 (0) | 1 (3) | 0.218 | 1 (1) |
| Duodenum ulcer | 0 (0) | 2 (6) | 0.080 | 2 (2) |
| Carcinoma of the stomach | 32 (64) | 25 (73) | 0.387 | 57 (68) |
| Malignant lymphoma of the stomach | 2 (4) | 0 (0) | 0.238 | 2 (2) |
| Carcinoma of the duodenum | 1 (2) | 0 (0) | 0.407 | 1 (1) |
| Tumors of the pancreas | ||||
| Carcinoma of the pancreas | 3 (6) | 0 (0) | 0.146 | 3 (4) |
| SCN | 1 (2) | 0 (0) | 0.407 | 1 (1) |
| NET | 1 (2) | 0 (0) | 0.407 | 1 (1) |
| Tumors of the biliary tract | ||||
| Carcinoma of the bile duct | 4 (8) | 0 (0) | 0.091 | 4 (5) |
| IPNB | 2 (4) | 3 (9) | 0.345 | 5 (6) |
| Pancreaticobiliary maljunction | 2 (4) | 1 (3) | 0.809 | 3 (4) |
| Congenital choledochal cyst | 0 (0) | 1 (3) | 0.218 | 1 (1) |
| Other | 2 (4) | 1 (3) | 0.809 | 3 (4) |
| Reasons for ERCP | ||||
| AOSC (due to CBD stone) | 0 (0) | 2 (6) | 0.080 | 2 (2) |
| Pancreatitis (due to CBD stone) | 1 (2) | 0 (0) | 0.407 | 1 (1) |
| CBD stone | 26 (52) | 21 (62) | 0.365 | 47 (56) |
| Intrahepatic stone | 10 (20) | 3 (9) | 0.172 | 13 (16) |
| Carcinoma of the pancreas | 2 (4) | 1 (3) | 0.809 | 3 (4) |
| Carcinoma of the gallbladder | 1 (2) | 0 (0) | 0.407 | 1 (1) |
| Cholangiocellular carcinoma | 3 (6) | 0 (0) | 0.146 | 3 (4) |
| IPMN | 0 (0) | 2 (6) | 0.080 | 2 (2) |
| IPNB | 2 (4) | 4 (12) | 0.165 | 6 (7) |
| Pancreaticobiliary maljunction | 1 (2) | 0 (0) | 0.407 | 1 (1) |
| Metastasis of L/n in porta hepatis | 0 (0) | 5 (15) | 0.005 | 5 (6) |
| Stricture of the anastomotic site | 4 (8) | 0 (0) | 0.091 | 4 (5) |
| Other | 1 (2) | 1 (3) | 0.769 | 2 (2) |
| Other abdominal or pelvic surgery | 9 (18) | 10 (29) | 0.236 | 19 (23) |
| Peritoneal metastasis | 0 (0) | 2 (6) | 0.080 | 2 (3) |
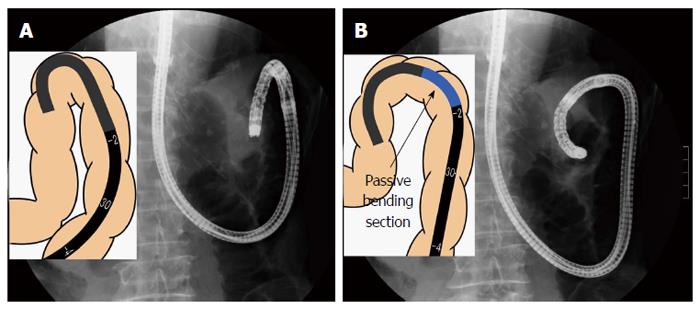
SIF-Y0004-V01 has three new features. First, it has a PB section that only bends passively. When the PB section meets with resistance, such as the reactive force of the intestinal wall, the force applied by the operator is physically transferred at the PB section, pushing the scope tip forward in the lumen. This function is thought to facilitate the passage of the scope through sharp bends in the intestine caused by bowel reconstruction (Figure 1).
Second, SIF-Y0004-V01 has HFT function, which is designed to facilitate the transmission of push and pull forces and rotational torque applied by the operator to the distal end of the scope. Consequently, the scope responds more sensitively to operator handling and is easier to maneuver. HFT is also expected to improve the rate of reaching the blind end and to facilitate accurate cannulation.
Third, SIF-Y0004-V01 has a short working length of 1520 mm and a working channel diameter of 3.2 mm, enabling the use of nearly all devices used to perform conventional ERCP. The use of retrieval baskets or other devices with commercially available balloon enteroscopes require freehand cannulation. In contrast, SIF-Y0004-V01 allows wire-guided lithotripsy and wire-guided intraductal ultrasonography to be easily performed. The placement of up to 8.5 Fr stents is possible.
Table 2 compares the specifications of the endoscopes, including a conventional SBE (SIF-Q260; Olympus Medical Systems). The difference between scopes in this study was the presence or absence of PB and HFT functions. A sliding tube with a working length of 880 mm was used.
| Variable | SIF-Y0004-V01 | SIF-Y0004 | SIF-Q260 |
| Direction of view | Forward viewing | Forward viewing | Forward viewing |
| Angle of view | 120° | 120° | 140° |
| Outer diameter (mm) | |||
| Distal end | 9.2 | 9.2 | 9.2 |
| Insertion end | 9.2 | 9.2 | 9.2 |
| Bending section | |||
| Up/down | 180°/180° | 180°/180° | 180°/180° |
| Right/left | 160°/160° | 160°/160° | 160°/160° |
| Working length (mm) | 1520 | 1520 | 2000 |
| Total length (mm) | 1840 | 1840 | 2345 |
| Working channel diameter (mm) | 3.2 | 3.2 | 2.8 |
| Water jet | Yes | Yes | No |
| Passive bending and high force transmission | Yes | No | No |
Patients were sedated with pethidine (50 mg) and midazolam (3-10 mg), and vital signs were intermittently monitored during all procedures. Propofol was used if necessary. Carbon dioxide insufflation was performed in all patients. The endoscope was inserted with the patient in the prone position, and abdominal compression was applied manually if a scope was technically difficult to insert deeply.
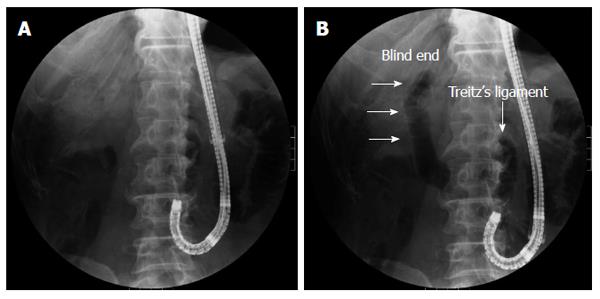
After reaching the intestinal anastomosis, the scope was inserted into either the afferent or efferent loop. Next, the balloon was inflated and then insufflated with CO2. The direction of the insufflated intestine was confirmed radiographically. If the scope is placed into the afferent loop, the blind end is depicted, and the direction of movement becomes clearer. We refer to this procedure as “CO2 inflation guidance” (Figure 2). After reaching the blind end, butylscopolamine (20-40 mg) or glucagon (1-2 mg) was administered as an antispasmodic.
We retrospectively assessed the rate of reaching the blind end, median time required to reach the blind end, diagnostic success rate (defined as the rate of successfully imaging the bile and pancreatic ducts), therapeutic success rate (defined as the rate of successfully completing endoscopic treatment), median procedure time, and complications in patients in the SIF-Y0004-V01 group. The results were then compared with the respective values in patients in the SIF-Y0004 group. Pancreatitis was evaluated according to the 1991 Consensus Guidelines (Cotton Classification)[20]. Hyperamylasemia was defined as a rise in serum amylase levels to more than three times the upper limit of normal. Because a prospective study reported that 25%-50% of patients had hyperamylasemia and 3%-12% had pancreatitis after double-balloon enteroscope via an oral approach[21-23], hyperamylasemia and pancreatitis were assessed in all patients with a pancreas, regardless of whether the blind end was reached. In patients in whom the blind end was not reached, SBE-assisted ERCP was not attempted a second time, except if the patient strongly requested to undergo the procedure again. If SBE-assisted ERCP was unsuccessful, open surgery or percutaneous cholangioscopy was performed.
Five endoscopists performed all endoscopic examinations and procedures. The same operator conducted all procedures from the time of scope insertion to treatment. Endoscopist A, who had the most experience in SBE-assisted ERCP, conducted significantly more ERCP sessions in SIF-Y0004 group than in SIF-Y0004-V01 group (P < 0.01). The number of sessions of ERCP performed by endoscopists B, C, D, and E did not differ between the groups. Patients treated by endoscopist E, who had the least experience, belonged to SIF-Y0004-V01 group (Table 3).
| Endoscopist | SIF-Y0004-V01 (n = 50) | SIF-Y0004 (n = 34) | P value | Experience with SBE-assisted ERCP, n |
| A | 6 (83) | 17 (88) | 0.001 | 56 |
| B | 11 (91) | 8 (88) | 0.872 | 29 |
| C | 13 (85) | 4 (100) | 0.111 | 29 |
| D | 16 (94) | 5 (100) | 0.072 | 26 |
| E | 4 (100) | - | 0.090 | 5 |
Numerical data are presented as mean ± SD, range, or both. Continuous variables were analyzed using a Student’s t-test or Mann-Whitney U test. Categorical variables were analyzed using Fisher’s exact test. P < 0.05 were considered to indicate statistical significance. Statistical analyses were performed using SPSS, version 19 for Windows (IBM Corp., Armonk, NY, United States).
The rate of reaching the blind end was 90% (45/50) in SIF-Y0004-V01 group and 91% (31/34) in SIF-Y0004 group. This difference was not significant (P = 0.586).
The median time required to reach the blind end was significantly shorter in the SIF-Y0004-V01 group (16 min; range: 3-56 min) than in the SIF-Y0004 group (24 min; range: 10-66 min; P = 0.039).
The diagnostic success rate was 93% (42/45) in the SIF-Y0004-V01 group and 84% (26/31) in the SIF-Y0004 group (P = 0.173). For patients with an intact papilla, the success rate was 89% (23/26) in the SIF-Y0004-V01 group and 77% (17/22) in the SIF-Y0004 group (P = 0.258).
The therapeutic success rate was 95% (40/42) in the SIF-Y0004-V01 group and 96% (25/26) in the SIF-Y0004 group (P = 0.676). For patients with an intact papilla, the success rate was 97% (22/23) in the SIF-Y0004-V01 group and 94% (16/17) in the SIF-Y0004 group (P = 0.676).
The mean procedure time was 43.7 min (median 40 min, range: 5-99 min) in the SIF-Y0004-V01 group and 41.5 min (median 36 min, range: 12-125 min) in the SIF-Y0004 group (P = 0.691).
The incidence of hyperamylasemia was 6.0% (3/50) in the SIF-Y0004-V01 group and 14.7% (5/34) in the SIF-Y0004 group (P = 0.723). For patients with an intact papilla, the incidence was 3.5% (1/28) in the SIF-Y0004-V01 group and 10.3% (3/29) in the SIF-Y0004 group (P > 0.999). The incidence of pancreatitis was 0% in the SIF-Y0004-V01 group and 5.9% (2/34) in the SIF-Y0004 group (P > 0.999). For patients in the SIF-Y0004 group with an intact papilla, the incidence of pancreatitis was 8.3% (2/29) (P > 0.999 vs SIF-Y0004-V01 group). The incidence of gastrointestinal perforation was 2.0% (1/50) in the SIF-Y0004-V01 group and 2.9% (1/34) in the SIF-Y0004 group (P > 0.999). Pancreatitis was mild and perforation responded to conservative therapy.
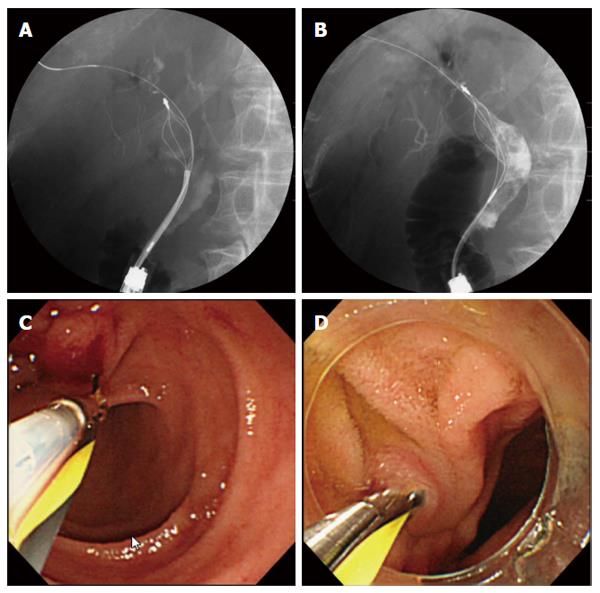
Stone extraction was performed with a wire-guided basket 27 times in the SIF-Y0004-V01 group and 16 times in the SIF-Y0004 group. Wire-guided endoscopic mechanical lithotripsy was performed 2 times in the SIF-Y0004-V01 group. Wire-guided intraductal ultrasonography was performed 8 times in the SIF-Y0004-V01 group and 10 times in the SIF-Y0004 group. These procedures cannot be performed using commercially available balloon enteroscopes (Figure 3).
ERCP in patients with R-Y anastomosis can be challenging because of difficulty in passing through sharp bends at anastomoses, the ligament of Treitz, or postoperative adhesions. Such factors preclude the scope tip from reaching the blind end. Colonoscopes with PB and HFT functions have been reported to reduce pain as compared with conventional colonoscopes, with no appreciable difference in cecal intubation rate[15-18]. Similar to a colonoscope, the presence of PB and HFT functions appeared to facilitate passage of an SBE. However, the rate of reaching the blind end in patients who undergo ERCP after intestinal reconstruction differs among hospitals. Therefore, the use of a SBE with PB and HFT functions may increase the rate of reaching the blind end. In our study, the median time required to reach the blind end was significantly shorter in SIF-Y0004-V01 group, whereas the rate of reaching the blind end did not differ significantly between the groups.
Our study has several important limitations. This study was retrospective with a small sample size. Consequently, some patient characteristics and the endoscopists who performed ERCP differed between the study groups. However, upon comparing the results according to the endoscopists who performed ERCP, the number of sessions of ERCP conducted by endoscopist A, who was most experienced in SBE-assisted ERCP, was significantly higher in the SIF-Y0004 group. Moreover, patients treated by endoscopist E, who had only conducted SBE-assisted ERCP in one patient previously, belonged to the SIF-Y0004-V01 group. Despite these differences, the median time required to reach the blind end was significantly shorter in SIF-Y0004-V01 group. The only difference between the scopes was the insertion section, suggesting that a SBE with PB and HFT functions may be easily inserted to the blind end, even by relatively inexperienced endoscopists.
Further studies are required to confirm our results. However, the results indicate that the PB and HFT functions of SIF-Y0004-V01 facilitate ERCP and may reduce the time required to reach the blind end in patients with R-Y anastomosis.
The authors thank Olympus Medical Systems (Tokyo, Japan) for providing the prototype instruments used in this study.
The use of balloon enteroscopes has improved the outcomes of endoscopic retrograde cholangiopancreatography (ERCP) in patients with a reconstructed intestine. Many studies have suggested that a short-type balloon enteroscope is effective for ERCP in such patients. However, performing ERCP with a balloon enteroscope can be challenging. The development of improved models of endoscopes and specialized devices is needed to improve the rate of reaching the papilla of Vater or choledochojejunal anastomosis and to reliably perform treatment procedures.
Recently, short-type single-balloon enteroscopes (SBE) were developed. These scopes have a working length of 1520 mm and a channel diameter of 3.2 mm, allowing most conventional ERCP devices to be employed. This scope also allows the use of wire-guided devices that could not be passed through enteroscopes with a 2.8 mm channel diameter.
Balloon-enteroscope assisted-ERCP is an important endoscopic breakthrough for the therapeutic management of conventionally inaccessible biliopancreatic ducts. However, several problems remain to be solved. In this study, authors used a newly designed short-type SBE equipped with passive bending section and high-force transmission functions (working length, 1520 mm; channel diameter, 3.2 mm). This scope was developed to improve the rate of reaching the blind end. It was reported that a colonoscope equipped with this technology could pass through the intestine with adhesions or hairpin bends, without distending the intestine, potentially causing less discomfort and speeding the insertion time as compared with a conventional colonoscope. This technology is expected to facilitate ERCP after intestinal reconstruction. The authors in this study evaluated the performance of this scope for ERCP in patients with a Roux-en-Y anastomosis and compared the results with the outcomes of ERCP performed with short-type SBE without these functions.
This study suggests that short-type SBE with passive bending and high-force transmission functions is useful for ERCP in patients with a Roux-en-Y anastomosis and may reduce the time required to reach the blind end.
Roux-en-Y reconstruction of the small intestine is a frequently performed surgical technique in gastrointestinal, hepatobiliary and pancreatic surgeries. The locations of the Vater’s papilla and choledochojejunal anastomosis in most patients who undergo this operation differ from normal positions that are accessible with conventional endoscopes.
The authors investigated the effectiveness of short-type SBE with passive bending and high-force transmission functions for ERCP in patients with altered gastrointestinal anatomy, and concluded that short-type SBE is effective for ERCP in patients with a reconstructed intestine. This study clearly shows the effectiveness of short-type SBE as a clinical trial.
P- Reviewer: Jovanovic P, Sakai Y S- Editor: Gou SX L- Editor: AmEditor E- Editor: Ma S
| 1. | Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 896] [Cited by in RCA: 861] [Article Influence: 35.9] [Reference Citation Analysis (0)] |
| 2. | Haruta H, Yamamoto H, Mizuta K, Kita Y, Uno T, Egami S, Hishikawa S, Sugano K, Kawarasaki H. A case of successful enteroscopic balloon dilation for late anastomotic stricture of choledochojejunostomy after living donor liver transplantation. Liver Transpl. 2005;11:1608-1610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 99] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 3. | Itoi T, Ishii K, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, Tsuji S, Ikeuchi N, Umeda J, Moriyasu F. Single-balloon enteroscopy-assisted ERCP in patients with Billroth II gastrectomy or Roux-en-Y anastomosis (with video). Am J Gastroenterol. 2010;105:93-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 124] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 4. | Saleem A, Baron TH, Gostout CJ, Topazian MD, Levy MJ, Petersen BT, Wong Kee Song LM. Endoscopic retrograde cholangiopancreatography using a single-balloon enteroscope in patients with altered Roux-en-Y anatomy. Endoscopy. 2010;42:656-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 102] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 5. | Wang AY, Sauer BG, Behm BW, Ramanath M, Cox DG, Ellen KL, Shami VM, Kahaleh M. Single-balloon enteroscopy effectively enables diagnostic and therapeutic retrograde cholangiography in patients with surgically altered anatomy. Gastrointest Endosc. 2010;71:641-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 96] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 6. | Yamauchi H, Kida M, Okuwaki K, Miyazawa S, Iwai T, Takezawa M, Kikuchi H, Watanabe M, Imaizumi H, Koizumi W. Short-type single balloon enteroscope for endoscopic retrograde cholangiopancreatography with altered gastrointestinal anatomy. World J Gastroenterol. 2013;19:1728-1735. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 55] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (1)] |
| 7. | Obana T, Fujita N, Ito K, Noda Y, Kobayashi G, Horaguchi J, Koshita S, Kanno Y, Ogawa T, Hashimoto S. Therapeutic endoscopic retrograde cholangiography using a single-balloon enteroscope in patients with Roux-en-Y anastomosis. Dig Endosc. 2013;25:601-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Aabakken L, Bretthauer M, Line PD. Double-balloon enteroscopy for endoscopic retrograde cholangiography in patients with a Roux-en-Y anastomosis. Endoscopy. 2007;39:1068-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Mönkemüller K, Bellutti M, Neumann H, Malfertheiner P. Therapeutic ERCP with the double-balloon enteroscope in patients with Roux-en-Y anastomosis. Gastrointest Endosc. 2008;67:992-996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 10. | Shimatani M, Matsushita M, Takaoka M, Koyabu M, Ikeura T, Kato K, Fukui T, Uchida K, Okazaki K. Effective “short” double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: a large case series. Endoscopy. 2009;41:849-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 161] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 11. | Iwamoto S, Ryozawa S, Yamamoto H, Taba K, Ishigaki N, Harano M, Iwano H, Sakaida I. Double balloon endoscope facilitates endoscopic retrograde cholangiopancreatography in roux-en-y anastomosis patients. Dig Endosc. 2010;22:64-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Itoi T, Ishii K, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, Tsuji S, Ikeuchi N, Fukuzawa K, Moriyasu F. Long- and short-type double-balloon enteroscopy-assisted therapeutic ERCP for intact papilla in patients with a Roux-en-Y anastomosis. Surg Endosc. 2011;25:713-721. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 75] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 13. | Moreels TG, Pelckmans PA. Comparison between double-balloon and single-balloon enteroscopy in therapeutic ERC after Roux-en-Y entero-enteric anastomosis. World J Gastrointest Endosc. 2010;2:314-317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 25] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Shah RJ, Smolkin M, Yen R, Ross A, Kozarek RA, Howell DA, Bakis G, Jonnalagadda SS, Al-Lehibi AA, Hardy A. A multicenter, U.S. experience of single-balloon, double-balloon, and rotational overtube-assisted enteroscopy ERCP in patients with surgically altered pancreaticobiliary anatomy (with video). Gastrointest Endosc. 2013;77:593-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 200] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 15. | Hoff G, Bretthauer M, Huppertz-Hauss G, Sauar J, Paulsen J, Dahler S, Kjellevold Ø. Evaluation of a novel colonoscope designed for easier passage through flexures: a randomized study. Endoscopy. 2005;37:1123-1126. [PubMed] |
| 16. | Garborg KK, Løberg M, Matre J, Holme O, Kalager M, Hoff G, Bretthauer M. Reduced pain during screening colonoscopy with an ultrathin colonoscope: a randomized controlled trial. Endoscopy. 2012;44:740-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Sato K, Ito S, Shigiyama F, Kitagawa T, Hirahata K, Tominaga K, Maetani I. A prospective randomized study on the benefits of a new small-caliber colonoscope. Endoscopy. 2012;44:746-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Mizukami T, Ogata H, Hibi T. “Passive-bending colonoscope” significantly improves cecal intubation in difficult cases. World J Gastroenterol. 2012;18:4454-4456. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Saito Y, Kimura H. Responsive insertion technology. Dig Endosc. 2011;23 Suppl 1:164-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [PubMed] |
| 21. | Kopácová M, Rejchrt S, Tachecí I, Bures J. Hyperamylasemia of uncertain significance associated with oral double-balloon enteroscopy. Gastrointest Endosc. 2007;66:1133-1138. [PubMed] |
| 22. | Pata C, Akyüz U, Erzin Y, Mutlu N, Mercan A, Dirican A. Post-procedure elevated amylase and lipase levels after double-balloon enteroscopy: relations with the double-balloon technique. Dig Dis Sci. 2010;55:1982-1988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Zepeda-Gómez S, Barreto-Zuñiga R, Ponce-de-León S, Meixueiro-Daza A, Herrera-López JA, Camacho J, Tellez-Avila F, Valdovinos-Andraca F, Vargas-Vorackova F. Risk of hyperamylasemia and acute pancreatitis after double-balloon enteroscopy: a prospective study. Endoscopy. 2011;43:766-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |