Published online Dec 14, 2015. doi: 10.3748/wjg.v21.i46.13140
Peer-review started: February 6, 2015
First decision: April 13, 2015
Revised: June 17, 2015
Accepted: August 28, 2015
Article in press: August 31, 2015
Published online: December 14, 2015
Processing time: 308 Days and 22.4 Hours
AIM: To evaluate the use of translumenal pancreatography with placement of endoscopic ultrasonography (EUS)-guided drainage of the pancreatic duct.
METHODS: This study enrolled all consecutive patients between June 2002 and April 2014 who underwent EUS-guided pancreatography and subsequent placement of a drain and had symptomatic retention of fluid in the pancreatic duct after one or more previous unsuccessful attempts at endoscopic retrograde cannulation of the pancreatic duct. In all, 94 patients underwent 111 interventions with one of three different approaches: (1) EUS-endoscopic retrograde drainage with a rendezvous technique; (2) EUS-guided drainage of the pancreatic duct; and (3) EUS-guided, internal, antegrade drainage of the pancreatic duct.
RESULTS: The mean duration of the interventions was 21 min (range, 15-69 min). Mean patient age was 54 years (range, 28-87 years); the M:F sex ratio was 60:34. The technical success rate was 100%, achieving puncture of the pancreatic duct including pancreatography in 94/94 patients. In patients requiring drainage, initial placement of a drain was successful in 47/83 patients (56.6%). Of these, 26 patients underwent transgastric/transbulbar positioning of a stent for retrograde drainage; plastic prostheses were used in 11 and metal stents in 12. A ring drain (antegrade internal drainage) was placed in three of these 26 patients because of anastomotic stenosis after a previous surgical intervention. The remaining 21 patients with successful drain placement had transpapillary drains using the rendezvous technique; the majority (n = 19) received plastic prostheses, and only two received metal stents (covered self-expanding metal stents). The median follow-up time in the 21 patients with transpapillary drainage was 28 mo (range, 1-79 mo), while that of the 26 patients with successful transgastric/transduodenal drainage was 9.5 mo (range, 1-82 mo). Clinical success, as indicated by reduced or absence of further pain after the EUS-guided intervention was achieved in 68/83 patients (81.9%), including several who improved without drainage, but with manipulation of the access route.
CONCLUSION: EUS-guided drainage of the pancreatic duct is a safe, feasible alternative to endoscopic retrograde drainage when the papilla cannot be reached endoscopically or catheterized.
Core tip: Endoscopic ultrasonography-guided drainage of the pancreatic duct (EUPD) can be considered a safe and feasible procedure and an alternative to surgical intervention for a select group of patients. Currently, EUPD remains an experimental clinical procedure, and it should be performed only in experienced hands with great expertise in interventional endoscopy/endoscopic ultrasonography. Further studies are recommended, perhaps in a multi-center design, to finally assess the clinical value of EUPD and to determine general selection criteria of patients for the procedure, as well as criteria for the technical/clinical success.
- Citation: Will U, Reichel A, Fueldner F, Meyer F. Endoscopic ultrasonography-guided drainage for patients with symptomatic obstruction and enlargement of the pancreatic duct. World J Gastroenterol 2015; 21(46): 13140-13151
- URL: https://www.wjgnet.com/1007-9327/full/v21/i46/13140.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i46.13140
Pain is the most frequent symptom in patients with an obstructed and enlarged pancreatic duct, and is associated with considerably reduced subjective well-being. Increased intraductal pressure is regarded as the cause for the signs, symptoms, and complaints, so the therapeutic response is based on attempting endoscopic transpapillary drainage or surgical intervention[1,2].
For patients with symptomatic obstruction and enlargement of the pancreatic duct, in whom pancreatic carcinoma can be excluded, or those with leakage from a postoperative pancreatic fistula, transpapillary endoscopic retrograde pancreatography (ERP), including placement of a drain, has been established as the gold standard of treatment[3-9]. In a certain proportion of these patients, the papilla of Vater (papilla) can be neither catheterized nor reached endoscopically. Specifically, a catheter cannot be introduced into the pancreatic duct via the major or minor papilla in patients with either chronic pancreatitis or pancreas divisum. Postoperatively, where the anatomy in the upper abdomen/gastrointestinal tract has been altered, e.g., after gastrectomy with Roux-en-Y reconstruction or a Kausch-Whipple procedure, the papilla or the anastomotic segment of a hepaticojejunostomy can no longer be reached, or cannot be easily reached via the conventional endoscopic route. Other considerations include patients with considerable perioperative risk factors, such as comorbidities, advanced age, and others, in whom recurrent invasive surgical interventions are necessarily associated with considerable morbidity and mortality. For these select groups of patients, or for patients who refuse to undergo surgical intervention, endoscopic ultrasonography (EUS)-guided internal drainage of the pancreatic duct (EUPD) can be considered a novel, alternative, therapeutic approach[10-22].
The aim of this systematic single-center, observational, clinical study was to reflect on our own daily practice and analyze the indications, technical feasibility, safety, and long-term clinical success of this novel interventional endoscopic technique in a representative number of patients. The primary endpoints of the study were the technical and clinical success rates. The secondary endpoint was the safety of the approach, as characterized by the range and frequency of adverse events and by intervention-related mortality. In particular, we describe our own procedural experiences in comparison with published data from the literature. In addition, we discuss the advantages and disadvantages of the procedure and its relevance for routine clinical practice.
Over a period of almost 12 years (June 2002 to April 2014), all consecutive patients with symptomatic, retained pancreatic ducts after previous unsuccessful ERP who underwent EUS-guided transgastric pancreatography were enrolled in this systematic single-center, observational, clinical study with prospective data collection and retrospective evaluation. The indications for which EUS-guided transgastric pancreatography and drainage were carried out are listed in Table 1.
| Clinical/pathological characteristics | Values |
| Patients, n | 94 |
| Age (yr), mean (range) | 54 (28–87) |
| Sex ratio, M:F | 60:34 |
| Interventions, n | 111 |
| Duration of the procedure (min), mean (range) | 21 (15–69) |
| Indication for EUS-guided pancreatography, n | 94 |
| Indication for EUS-guided drainage, n | 83 |
| Indication for EUPD, n | 94 |
| Chronic pancreatitis | 35 (37.2) |
| Previous surgical intervention with fluid retention in the pancreatic duct | 30 (31.9) |
| Pancreas divisum | 15 (16.0) |
| Disconnected pancreatic tail syndrome | 9 (9.6) |
| Persistent postoperative fistula | 5 (5.3) |
| EUPD, n | 83 |
| Success rate | 47 (56.6) |
| Route of access (n = 47) | |
| Transpapillary | 21 (44.7) |
| Transgastric | 26 (55.3) |
All interventions were performed by the same endoscopist/endosonographer (Will U).
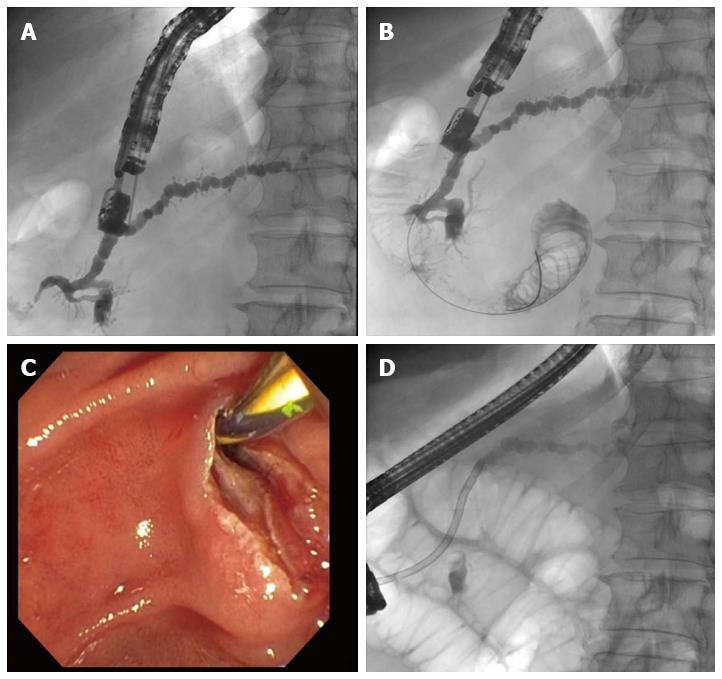
Patients were positioned lying on their left side on a fluoroscopy table for undergoing EUS with a therapeutic longitudinal scanner (EG 3270 United Kingdom; Hitachi, Ltd., Chiyoda, Tokyo, Japan; or GF-UCT 180; Olympus Corp., Shinjuku, Tokyo, Japan). Peri-interventionally, ceftriaxone 2 g was given iv. The pancreatic duct was identified by EUS imaging and was punctured using a 19-G needle (Boston Scientific Corp., Marlborough, MA, United States) via a transgastric or transbulbar route, using the shortest possible distance to minimize the potential for complications. Despite the usually low amount of pancreatic fluid in the duct, a sample of pancreatic juice was obtained whenever possible, for routine cytologic analysis (to check for pancreatic cancer) and microbiologic study (for preparation of any antibiotic therapy required according to the resistogram in the presence of microbial colonization). After this, the pancreatic duct was imaged by the administration of contrast medium under fluoroscopy control (Figure 1). In addition, a 0.035-inch guide wire (Boston Scientific Corp.) was introduced into the pancreatic duct and advanced toward and through the papilla or anastomosis.
EUS-ERP rendezvous technique: If the papilla could be reached endoscopically and the guide wire could be advanced toward and through the papilla from inside the ductal lumen, the echoendoscope was replaced by a duodenoscope. The guide wire was gripped and pulled out further, and then conventional ERP including endoscopic papillotomy (EPT) and placement of a stent was performed (Figure 1).
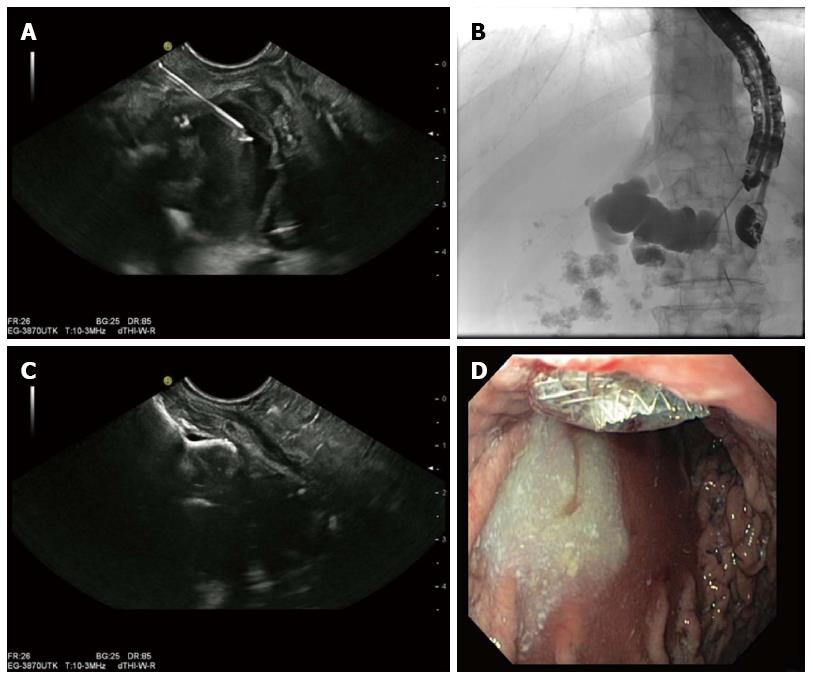
EUS-guided drainage of the pancreatic duct: If it was not possible to advance the guide wire toward or through the papilla, or if the papilla could not be reached using a duodenoscope (e.g., after a previous surgical intervention including Roux-en-Y reconstruction, Kausch-Whipple procedure, or a pylorus-preserving cephalic pancreatoduodenectomy), the guide wire was advanced into the pancreatic duct as far as possible. Via the guide wire, access to the pancreatic duct was created using Will’s high-frequency ring knife (MTW-Endoskopie, Wesel, Germany) (Figure 2) and the duct was dilated with a 6-mm dilatation balloon specific for the biliary tree (Boston Scientific Corp.). The puncture site and the direction and diameter of the pancreatic duct were the relevant criteria for deciding on the type of prosthesis that was finally placed. Correct positioning of the drain was checked endoscopically by observing the intralumenal end of the stent, and regular outflow of contrast medium via the pancreatointestinostomy (or pancreatoduodenostomy) was checked fluoroscopically (Figure 3).
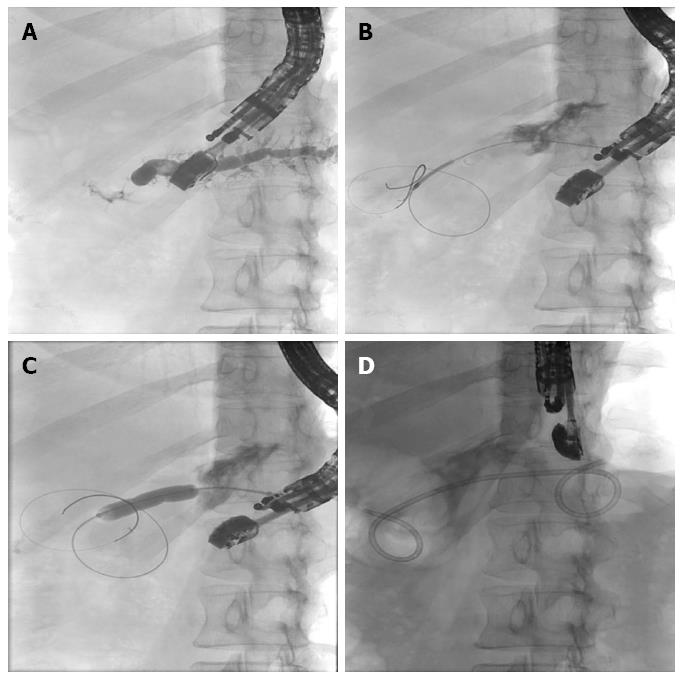
EUS-guided internal antegrade drainage of the pancreatic duct: If advancement of the guide wire through the stenosis succeeds but the papilla (or anastomosis) cannot be reached endoscopically, access is created using Will’s high-frequency ring knife (MTW-Endoskopie). Using the ring knife, the stenotic segment can be reached and dilated with a balloon (6-12 mm). To keep the dilatation effect and further “conditioning” of the channel that has been created, pigtail drainage can be placed (Figure 4).
The implants that were available included: double-pigtail and straight plastic prostheses (diameter, 5-10 Fr; Amsterdam prosthesis, Medi-Globe, Achenmühle, Germany), covered self-expanding metal stents (Boston Scientific Corp.), and AXIOSTM stents (diameter, 10-15 mm; Xlumena, Mountain View, CA, United States). On the 1st postinterventional day, transabdominal ultrasonography was performed to document correct stent location. Air within the pancreatic duct, reduction of the ductal diameter, and/or reduced secretion from the pancreatic fistula (in patients with a fistula) were interpreted as indicating technically successful drainage of the pancreatic duct.
All patients were followed up within 3-6 mo after the intervention. In particular, any new onset of clinical symptoms was assessed. The imaging criteria for adequate drainage were a smaller-diameter pancreatic duct and air within the duct.
Each patient gave written informed consent prior to the intervention. The study was performed according to the recommendations of the 1964 Declaration of Helsinki for Biomedical Research and its later amendments, and according to the standards of the Good Clinical Practice (GCP) and the guidelines of our hospital’s institutional review board.
From June 2002 to April 2014, 111 interventions were performed in 94 patients with the intention of carrying out EUS-guided transgastric pancreatography and drainage. The mean patient age was 54 years (range, 28-87 years). Almost twice as many men as women were enrolled (M:F = 60:34). The mean duration of the procedure was 21 min (range, 15-69 min).
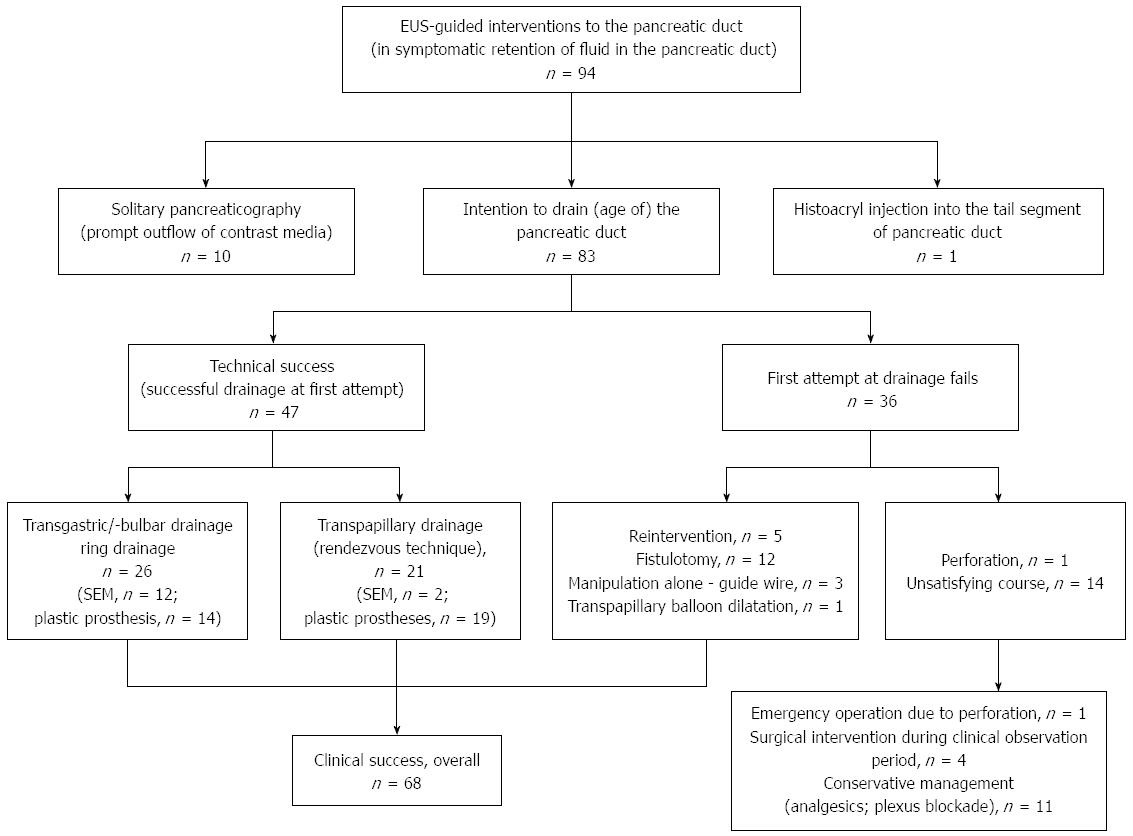
In all 94 patients, puncture of the pancreatic duct including pancreatography was achieved (technical success rate, 100%). However, in ten patients with altered anatomy after previous surgical intervention, no drainage was required because there was sufficient flow of contrast medium through the anastomosis. In one further patient, Histoacryl was injected into the tail segment of the pancreatic duct as a primary procedure because of disconnected pancreatic tail syndrome and a recurrent symptomatic retention cyst, which was drained transmurally during the same endoscopic session. Postinterventionally, there were no complications and the patient was discharged with no further complaints. Unfortunately, this patient did not return for clinical and imaging follow-up (Figure 5).
In the remaining 83 patients in whom obstruction of the pancreatic duct or anastomotic stenosis was found, drainage of the duct was indicated. In all patients, a minimum of two ERP attempts had been made (range, 2-8), all of which failed. Successful placement of drainage upon first attempt was achieved in 47/83 (56.6%) patients. Overall, 26 of the 47 patients underwent transgastric/transbulbar positioning of a stent, whereas in the other 21 patients, drainage was through the papilla using the rendezvous technique. Of the 26 patients undergoing translumenal (retrograde) drainage, plastic prostheses were used in 11 and metal stents in 12. The remaining three of these patients received placement of a ring drain (antegrade internal drainage) because of the presence of an anastomotic stenosis after former surgical intervention. Of the 21 patients with transpapillary drainage, the majority (n = 19) received plastic prostheses; only two received covered self-expanding metal stents.
Of the 47 patients in whom primary placement of drainage was possible, three underwent a total of six reinterventions because of: (1) stent dislocations (n = 2); (2) stent occlusions (n = 2); or (3) unsuccessful positioning of the drainage in a further intervention (n = 2).
The median follow-up time in patients who had undergone placement of transpapillary drainage (n = 21) was 28 mo (range, 1-79 mo). In 8/21 of these patients, the stent was minimally changed once later during the clinical course. In 17/21 patients, drains were removed during the postinterventional time period. In 2/21 patients, prostheses were still in situ postinterventionally. In 1/21 patients, there was a spontaneous dislocation of the prosthesis, but reintervention was not immediately carried out, as the patient reported no complaints. One other patient of the 21 could not be included in the postinterventional follow-up investigation protocol, as he did not attend as requested. The median postinterventional time during which patients had no complaints after successful transpapillary drainage was 12 mo. Interestingly, in five patients, surgical intervention was required because of underlying disease (chronic pancreatitis). In six cases, further endoscopic interventions became necessary because of recurrent complaints and symptoms after removal of the prosthesis, and it was possible to perform these via the conventional route. In one patient, recurrent acute pancreatitis was successfully managed with analgesics alone. In eight patients, no postinterventional complaints, signs, or symptoms occurred.
The 26 patients with successful transgastric/transduodenal drainage did not undergo elective stent change, as there were no complaints and recurrent obstruction or enlargement of the pancreatic duct was not detected. The median follow-up time of these patients was 9.5 mo (range, 1-82 mo). In 15/26 patients, drainage was left in situ because they had no complaints. In four subjects, spontaneous dislocation of the prosthesis occurred; of these, three did not need any further reintervention, as they had not reported any further problems. In one patient, reintervention for placement of ring drainage through the anastomotic stenosis after former surgical intervention became necessary. In seven patients, drainage was removed later on; of these, two patients underwent surgical interventions because of recurrent complaints, two were successfully managed with analgesics, and three were stable (no complaints) after formation of a persistent fistula.
In total, 36/83 patients were not successfully drained by the primary intervention (primary failure rate, 43.4%) (Figure 5). In 5/36 patients, drainage was achieved after reintervention; one patient with a transpapillary plastic prosthesis, three patients with transgastric retrograde drainage (plastic prosthesis, n = 2; covered self-expanding metal stent; n = 1), and one patient with a ring drain as antegrade internal drainage. Three out of 36 patients showed distinct clinical improvement after guide wire manipulation at the pancreatic duct only, despite the failure to achieve placement of a drain (one patient had no problems for 19 mo, one patient with chronic pancreatitis underwent resection of the pancreatic head, and one patient underwent a further intervention with successful transpapillary drainage because of recurrent complaints). One out of 36 patients reported a reduction of signs and symptoms after balloon dilatation only, following a previous unsuccessful attempt to place a drain using the rendezvous technique.
One-third of the patients (12/36) in whom drainage placement had failed showed clinical improvement after additional manipulation at the transgastric access site using a ring knife, combined - if required - with additional balloon dilatation (n = 5). In two of the 12 patients, three reinterventions were necessary for recurrent abdominal pain (including placement of a ring drainage in one patient, and repeat manipulation using a ring knife for a another patient following the failed attempt at drainage placement). Three patients were lost to follow-up. The remaining nine patients developed no further problems in 52 mo.
A total of 15/36 patients had persistent complaints after the failed intervention. One patient needed to undergo urgent surgical intervention (suturing) because of a perforation; this patient underwent resection of the pancreatic head 6 mo later. Four patients underwent the same surgical procedure during a further clinical observation period. In four patients, the procedure was converted to conventional ERP, and this led to reduced complaints during a 60-mo follow-up. The remaining six patients were treated either conservatively (analgesics for symptom control) or using interventional endoscopy (plexus blockade).
Clinical success, as indicated by the reduction or elimination of pain after the EUS-guided intervention, was achieved in 68/83 patients (success rate, 81.9%). For a better clinical success rate, the following technical point may play a substantial role. The most frequent cause for unsuccessful drainage placement is failure to advance the guide wire, or else dislocation of the guide wire, because of the difficulty of the access route. By optimizing (“conditioning”) the access route using a ring knife and - if required - additional balloon dilatation, a more stable access route can be created, facilitating interventions toward/in the pancreatic duct. In addition, fistulotomy alone as the only result of manipulation, even without subsequent placement of drainage, can lead to clinical improvement. Thus, our clinical success rate improved by 20% after the ring knife was introduced to optimize the access route, and marked reductions in the number of reinterventions and adverse events were also seen (Table 2). This needs further thoughtful investigation.
| Intervention period | Clinical success | Re-interventions | Adverse events |
| Before introduction of ring knife (n = 35) | 25 (71.4) | 11 (31.4) | 14 (40.0) |
| After introduction of ring knife (n = 48) | 43 (89.6) | 6 (12.5) | 11 (22.9) |
The median follow-up observation time was 15 mo (range, 1-94 mo); in drainage patients alone it was 9.5 mo (range, 1-82 mo). In total, 17 reinterventions were required for the following reasons: pain (n = 3); stent dislocation (n = 3); stent occlusion (n = 2); and technical problems (n = 9). In addition, one patient needed urgent surgical intervention because of perforation, two patients died of malignant disease (tonsillar carcinoma, n = 1; cancer of unknown primary, n = 1), and two patients had metastasized bronchial carcinoma.
Overall, 12 patients underwent surgical intervention for their underlying disease (chronic pancreatitis).
No pancreatic cancer was found after EUPD, and thus, can be ruled out as a cause of obstruction and enlargement of the pancreatic duct, and considered as an indication for performing EUPD.
Adverse events occurred in 24/111 (21.6%) interventions (Table 3). Of these, bleeding occurred in six patients; in one patient it stopped spontaneously; whereas it was controlled by epinephrine injection and/or clip application in four patients. In one patient, bleeding that led to a large hematoma needed to be externally drained. Moderate pancreatitis occurred in six patients, all of whom improved (no further symptoms) with conservative treatment (e.g., infusion therapy, analgesics). Four patients developed an abscess; internal drainage was placed in two, and external drainage in one, whereas one abscess was drained laparoscopically. Perigastric fluid collections were found in three patients. Conservative antibiotic treatment was successful as indicated by the fact that the fluid collections then reabsorbed spontaneously. One patient needed to undergo urgent surgical intervention because of a perforation. In another patient, a retention cyst occurred after the intervention. No further treatment was necessary because no symptoms were caused. In one patient, aspiration occurred during the intervention, but no operation was necessary as suction and antibiotic therapy prevented any further problems. Two patients with pain had pressure-associated ulcers. After endoscopic shortening of the covered self-expanding metal stents with argon plasma coagulation, the patients had no further complaints. Taken together, there were 2 severe, 20 intermediate, and 2 minor adverse events. There was no intervention-related death (mortality, 0).
| Adverse event | n |
| Major | |
| Perforation | 1 |
| Abscess | 1 |
| Intermediate | |
| Bleeding | 6 |
| Moderate pancreatitis | 6 |
| Abscess | 3 |
| Perigastric fluid | 2 |
| Ulcer caused by pressure | 2 |
| Aspiration | 1 |
| Minor | |
| Perigastric fluid | 1 |
| Retention cyst | 1 |
The main cause of pain in patients with benign retention of fluid in the pancreatic duct is intraductal hypertension[1,2]. Most frequently, chronic pancreatitis with inflammatory stenosis of the duct (ductal system), obstructions due to pancreatolithiasis and pseudocysts, or rupture of the pancreatic duct are the main cause. In addition, inflammatory stenosis of the papilla, anatomic variants (e.g., pancreas divisum), and anastomotic stenosis after previous surgical intervention can lead to obstruction and enlargement of the pancreatic duct. The aim of all types of treatment is, therefore, to lower the intraductal pressure, whether by endoscopic techniques or surgical intervention, to create a draining effect in the pancreatic duct. However, pain has a multifactorial background. While increased intraductal pressure is probably an important factor, it is important to avoid attributing all pain to intraductal pressure alone.
Endoscopic and surgical measures allow success rates from 70% to 90% to be achieved[23-26]. In this context, ERP as a minimally invasive procedure is considered the gold standard versus surgical intervention. However, conventional ERP has limitations in cases where the papilla cannot be reached (due to previous surgical interventions) or a guide wire/catheter cannot be introduced. Until now, this has led to surgical intervention as the only remaining therapeutic option. Now, however, a novel alternative to avoid surgical intervention as the last option is EUPD.
Before EUPD is attempted, malignant tumor growth must be definitively ruled out as a cause of the obstruction and enlargement of the pancreatic duct. If there is any doubt, explorative laparotomy and - if required - surgical resection are recommended to resolve symptomatic obstruction and enlargement of the pancreatic duct. In three studies, 3/20 (15%)[12], 4/36 (11%)[19], and 2/45 (4%)[13] patients were diagnosed with malignant tumor growth. In our own group of patients, no pancreatic cancer was found after EUPD. However, in patients in whom symptoms persist after EUPD, early surgical intervention should be carried out.
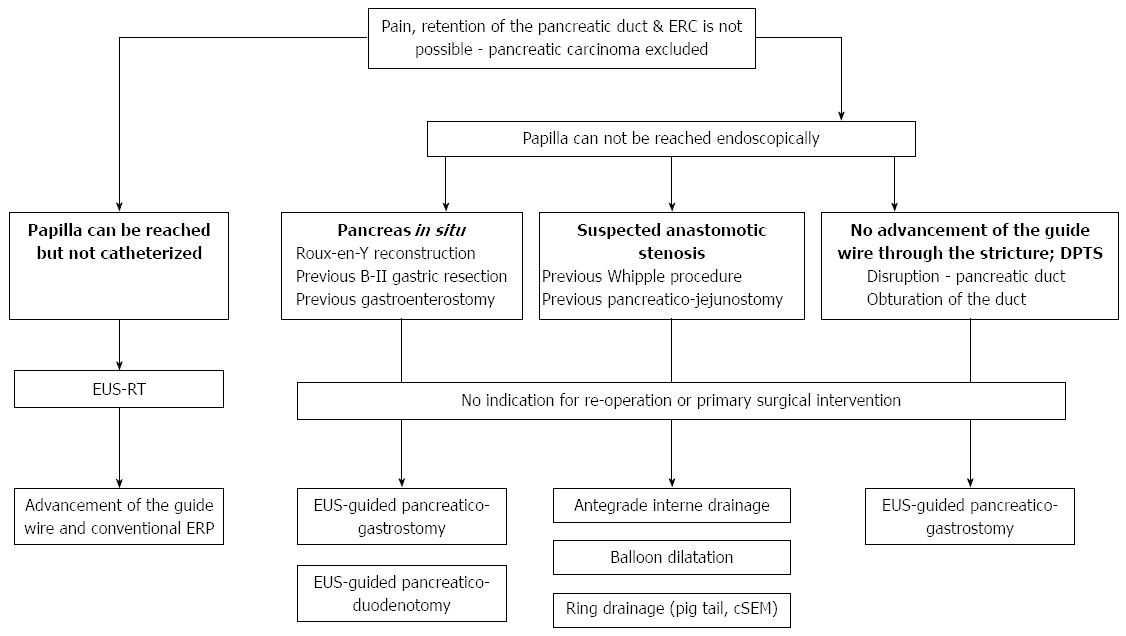
In performing EUPD, there are basically three options (Figure 6): (1) if the papilla can be reached endoscopically but the catheter cannot be introduced, a rendezvous procedure should be used; (2) if the papilla cannot be reached endoscopically, transgastric or transbulbar drainage with ante- or retrograde outflow should be created; and (3) alternatively, if the papilla cannot be reached but the stenotic ductal segment can be passed, internal antegrade drainage can be placed in the form of “ring drainage”.
In the available studies, pancreatography was achieved in almost 100% of cases, as also in the present study; however, the technical success rate varied - sometimes due in part to low case numbers - ranging between 25% and 92%[10-22] (Table 4). The most frequent cause of failed transgastric drainage is the difficulty of the puncture route; for example, often the guide wire cannot be advanced because of fibrotic changes in the pancreatic parenchyma, or because the guide wire dislocates. Using a high-frequency diathermy knife, balloons, bougies, or retrievers, it is usually possible to “stabilize” the access route, giving easier access and making intervention in the pancreatic duct possible. In the present authors’ own experience, the introduction of Will’s ring knife (MTW-Endoskopie) into clinical endoscopic practice has led to a marked rise in the clinical success rate (up to 90%) and, simultaneously, to a fall in the number of reinterventions (from 31% down to 12%), as well as in the adverse event rate (40% down to 22%). In addition to the technical elements, the experience of the investigator is one of the most important factors[13]. For this reason, EUPD should only be carried out in centers with great expertise in ERCP and interventional EUS.
| Ref. | n | Technical success (%) | Clinical success (%) | Adverse events (%) |
| Mallery et al[17], 2004 | 4 | 25 | ND | 25 |
| Will et al[20], 2007 | 14 | 69 | 78 | 15 |
| Kahaleh et al[15], 2007 | 13 | 76 | 69 | 15 |
| Tessier et al[19], 2007 | 36 | 92 | 69 | 14 |
| Brauer et al[11], 2009 | 8 | 88 | 50 | 0 |
| Barkay et al[10], 2010 | 21 | 48 | 100 | 10 |
| Ergun et al[12], 2011 | 20 | 90 | 72 | 19 |
| Will et al[21], 2011 | 65 | 60 | 74 | 15 |
| Shah et al[18], 2012 | 25 | 88 | ND | 16 |
| Kurihara et al[16], 2013 | 14 | 88 | ND | 6 |
| Fuji et al[13], 2013 | 45 | 74 | 83 | 6 |
| Will et al[22], 2013 | 84 | 59 | 78 | 18 |
Clinical long-term success rates ranging from 50% to 100% have been reported in the available literature[10-22] (Table 4). The enormous difference in rates can be explained by the variability of case numbers, which, in some studies, were low. Because of the heterogeneity of the patient groups, it is not really possible to compare the treatment results. However, the success rate of EUPD is comparable to those of ERP or surgical intervention[23-26], as achieved in this study.
In our own group of patients, stents were routinely changed only in patients with transpapillary drainage in order to avoid stent-induced strictures of the pancreatic duct as reported in the literature[27,28]. Elective stent change was not regularly scheduled in patients with transgastric drainage; if the patient was free of complaints, signs, and symptoms, and if postinterventional imaging showed characteristics of adequate drainage (e.g., the pancreatic duct no longer showed obstruction/enlargement, the duct’s caliber was small, and air bubbles were seen within it), the stent was left in situ.
Stent-associated changes of the pancreatic duct have not yet been observed. Whether a regular change of the stent in case of no complaints is necessary at all is still a matter of debate. Greater case numbers and a long-term follow-up time period for postinterventional observation are required to clarify this point. In a certain proportion of patients (14%; 12/83), sole manipulation at the transgastric access route using a ring knife - in part combined with balloon dilatation - can result in clinical improvement. This can be explained by formation of a chronic fistula or of a neo-ostium, through which overshooting intraductal pressure can be drained. Even after a longer time period of transgastric drainage in situ, a persisting pancreatogastric fistula could still be found after removal of the prosthesis. Whether sole fistulotomy or a temporary stenting can be sufficient, and which factors are the most important, cannot be clarified at present.
Adverse event rates reported in the literature have ranged from 14% to 25%[10-22] (Table 4). So far, no intervention-related death has been reported. Reported adverse events include bleedings, perforations, pancreatitis episodes, and the formation of pseudocysts, all of which were successfully managed conservatively (pancreatic enzyme replacement therapy, analgesics) or by interventional endoscopy.
The strengths of the present study are that it includes the largest number of patients in any published study on EUPD so far, excludes inter-endoscopist variability (depending on perspective, this can be also regarded as a limitation - see below), and reports no intervention-related deaths, indicating appropriate patient selection.
The limitations of the study relate to the incomplete follow-up, the single-center study design and, associated with this, the fact that the experience is that of one single endoscopist.
This study supplies further strong support for EUPD as a safe and practicable procedure that is steadily becoming more established in the daily clinical endoscopic practice of therapeutic EUS. However, it should still be carried out in multidisciplinary centers that provide the back-up possibility of abdominal surgery.
In conclusion, the place of EUPD in the spectrum of therapeutic options for approaching symptomatic obstruction and enlargement of the pancreatic duct cannot be satisfactorily and finally answered at the present time. In the light of current experience, EUPD can be regarded as: (1) a safe and feasible procedure for a select group of patients (in terms of age, comorbidities, altered anatomy after previous surgical intervention, disconnected pancreatic tail syndrome, persistent postoperative fistula, or refusal to undergo further surgical intervention); and (2) an alternative to surgical intervention. Given the limited number of cases in the majority of studies[3-9], it is not currently possible to adequately compare EUPD with established procedures and approaches (such as ER[C]P and surgical intervention) with regard to adverse events and technical or long-term clinical success.
Currently, EUPD is still an experimental clinical procedure and should be performed only by experienced endoscopists with great expertise in interventional endoscopy and EUS. Further prospective studies and, in addition, greater numbers of cases and studies (possibly of multicenter design) are needed to validate and assess technical and clinical success, as well as to allow general recommendations as to which patients are likely to benefit most from EUPD.
For patients with symptomatic obstruction and enlargement of the pancreatic duct, in whom pancreatic carcinoma can be excluded, or those with leakage from a postoperative pancreatic fistula, transpapillary endoscopic retrograde pancreatography (ERP) including placement of a drain has been established as the gold standard of treatment. In particular, increased intraductal pressure is regarded as the cause of signs, symptoms, and complaints, so the therapeutic response is based on attempting endoscopic transpapillary drainage or even surgical intervention.
Endoscopic ultrasonography (EUS)-guided transluminal pancreatography with following internal drainage of the pancreatic duct (EUPD) can be considered a novel alternative therapeutic approach in a certain proportion of patients, including: (1) those in whom the papilla of Vater (papilla) can be neither catheterized (due to chronic pancreatitis or pancreas divisum) nor reached endoscopically (if the anatomy in the upper abdomen/gastrointestinal tract has been altered postoperatively - e.g., after gastrectomy with Roux-en-Y reconstruction, Kausch-Whipple procedure or hepaticojejunostomy); (2) there are considerable perioperative risk factors (comorbidities, advanced age); or (3) patients who refuse to undergo surgical intervention.
The aim of this systematic, single-center, observational, clinical study was to reflect on our own daily practice and analyze the indications, technical feasibility, safety, and long-term clinical success of this novel, interventional, endoscopic technique in a consecutive patient cohort. The primary endpoints of the study were the technical and clinical success rates. Secondary endpoint was the safety of the approach as characterized by the range and frequency of adverse events, and by intervention-related mortality. From the authors’ point of view, EUPD can provide excellent technical and acceptable clinical success rates even in the mid-term time period based on our own initial procedural experiences in comparison with published data from the literature. Derived from this and based on a large representative number of patients, the advantages and disadvantages of the procedure and the relevance for routine clinical practice can extensively be discussed.
EUPD is a safe, feasible, alternative approach to ERP for a select group of patients (in terms of age, comorbidities, altered anatomy after previous surgical intervention, disconnected pancreatic tail syndrome, persistent postoperative fistula, or refusal to undergo further surgical intervention), and an alternative to surgical intervention, but it can only be performed by experienced interventional endoscopists/-sonographers in centers with great expertise in therapeutic EUS, as it is still considered an experimental clinical procedure.
ERP/ERCP is regarded as the gold standard for symptomatic therapy in patients with chronic pancreatitis. EUS-guided transluminal pancreatography with following internal drainage of the pancreatic duct can be considered a novel, minimally invasive technique of interventional endoscopy/EUS and therapeutic alternative for ERCP or even surgical intervention where (1) the anatomy of the upper gastrointestinal tract has been altered by previous surgery; (2) the patient’s surgical risk is high; or (3) the patient has withheld consent.
The place of EUPD in the spectrum of therapeutic options for approaching symptomatic obstruction and enlargement of the pancreatic duct cannot be satisfactorily and finally answered at the present time. In the light of current experience, EUPD can be regarded as a safe and feasible procedure (study-specific results: total, n = 94 patients; procedures, n = 111; technical success rate for pancreatography and drainage, 100% and 56.6%, respectively; adverse event rate, 21.6%; no intervention-related death) for a select group of patients. EUPD deserves further systematic investigation and analysis in studies, possibly with a multicenter design, which needs to include an assessment of the subgroup of patients in whom this treatment is indicated before this novel therapeutic technique can be finally validated and recommended. For example, patients who have previously undergone gastrointestinal surgery or those in whom the papilla cannot be reached endoscopically or catheterized due to severe changes caused by chronic pancreatitis may be, in particular, suited to EUPD. Given the limited number of cases in the majority of studies, adequate comparison of EUPD with established procedures and approaches (such as ERCP and surgical intervention) with regard to adverse events or technical and long-term clinical success is not possible at present. Further prospective studies and, in addition, greater numbers of cases, are needed to validate and assess the technical and clinical success with this procedure, as well as to allow general recommendations as to which patients are likely to benefit most from EUPD.
P- Reviewer: Ammendola M, Cucu D S- Editor: Yu J L- Editor: Filipodia E- Editor: Ma S
| 1. | Ebbehøj N, Borly L, Bülow J, Rasmussen SG, Madsen P, Matzen P, Owre A. Pancreatic tissue fluid pressure in chronic pancreatitis. Relation to pain, morphology, and function. Scand J Gastroenterol. 1990;25:1046-1051. [PubMed] |
| 2. | Widdison AL, Alvarez C, Karanjia ND, Reber HA. Experimental evidence of beneficial effects of ductal decompression in chronic pancreatitis. Endoscopy. 1991;23:151-154. [PubMed] |
| 3. | Chauhan S, Forsmark CE. Pain management in chronic pancreatitis: A treatment algorithm. Best Pract Res Clin Gastroenterol. 2010;24:323-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 49] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Cotton PB. Endoscopic retrograde cholangiopancreatography: maximizing benefits and minimizing risks. Gastrointest Endosc Clin N Am. 2012;22:587-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Díte P, Ruzicka M, Zboril V, Novotný I. A prospective, randomized trial comparing endoscopic and surgical therapy for chronic pancreatitis. Endoscopy. 2003;35:553-558. [PubMed] |
| 6. | Dumonceau JM, Delhaye M, Tringali A, Dominguez-Munoz JE, Poley JW, Arvanitaki M, Costamagna G, Costea F, Devière J, Eisendrath P. Endoscopic treatment of chronic pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2012;44:784-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 188] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 7. | Freeman ML. Complications of endoscopic retrograde cholangiopancreatography: avoidance and management. Gastrointest Endosc Clin N Am. 2012;22:567-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 86] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 8. | Hoffmeister A, Mayerle J, Beglinger C, Büchler MW, Bufler P, Dathe K, Fölsch UR, Friess H, Izbicki J, Kahl S. [S3-Consensus guidelines on definition, etiology, diagnosis and medical, endoscopic and surgical management of chronic pancreatitis German Society of Digestive and Metabolic Diseases (DGVS)]. Z Gastroenterol. 2012;50:1176-1224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Nguyen-Tang T, Dumonceau JM. Endoscopic treatment in chronic pancreatitis, timing, duration and type of intervention. Best Pract Res Clin Gastroenterol. 2010;24:281-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 10. | Barkay O, Sherman S, McHenry L, Yoo BM, Fogel EL, Watkins JL, DeWitt J, Al-Haddad MA, Lehman GA. Therapeutic EUS-assisted endoscopic retrograde pancreatography after failed pancreatic duct cannulation at ERCP. Gastrointest Endosc. 2010;71:1166-1173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 86] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 11. | Brauer BC, Chen YK, Fukami N, Shah RJ. Single-operator EUS-guided cholangiopancreatography for difficult pancreaticobiliary access (with video). Gastrointest Endosc. 2009;70:471-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 93] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 12. | Ergun M, Aouattah T, Gillain C, Gigot JF, Hubert C, Deprez PH. Endoscopic ultrasound-guided transluminal drainage of pancreatic duct obstruction: long-term outcome. Endoscopy. 2011;43:518-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 91] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 13. | Fujii LL, Topazian MD, Abu Dayyeh BK, Baron TH, Chari ST, Farnell MB, Gleeson FC, Gostout CJ, Kendrick ML, Pearson RK. EUS-guided pancreatic duct intervention: outcomes of a single tertiary-care referral center experience. Gastrointest Endosc. 2013;78:854-864.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 14. | Giovannini M. EUS-guided pancreatic duct drainage: ready for prime time? Gastrointest Endosc. 2013;78:865-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Kahaleh M, Hernandez AJ, Tokar J, Adams RB, Shami VM, Yeaton P. EUS-guided pancreaticogastrostomy: analysis of its efficacy to drain inaccessible pancreatic ducts. Gastrointest Endosc. 2007;65:224-230. [PubMed] |
| 16. | Kurihara T, Itoi T, Sofuni A, Itokawa F, Moriyasu F. Endoscopic ultrasonography-guided pancreatic duct drainage after failed endoscopic retrograde cholangiopancreatography in patients with malignant and benign pancreatic duct obstructions. Dig Endosc. 2013;25 Suppl 2:109-116. [PubMed] |
| 17. | Mallery S, Matlock J, Freeman ML. EUS-guided rendezvous drainage of obstructed biliary and pancreatic ducts: Report of 6 cases. Gastrointest Endosc. 2004;59:100-107. [PubMed] |
| 18. | Shah JN, Marson F, Weilert F, Bhat YM, Nguyen-Tang T, Shaw RE, Binmoeller KF. Single-operator, single-session EUS-guided anterograde cholangiopancreatography in failed ERCP or inaccessible papilla. Gastrointest Endosc. 2012;75:56-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 160] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 19. | Tessier G, Bories E, Arvanitakis M, Hittelet A, Pesenti C, Le Moine O, Giovannini M, Devière J. EUS-guided pancreatogastrostomy and pancreatobulbostomy for the treatment of pain in patients with pancreatic ductal dilatation inaccessible for transpapillary endoscopic therapy. Gastrointest Endosc. 2007;65:233-241. [PubMed] |
| 20. | Will U, Fueldner F, Thieme AK, Goldmann B, Gerlach R, Wanzar I, Meyer F. Transgastric pancreatography and EUS-guided drainage of the pancreatic duct. J Hepatobiliary Pancreat Surg. 2007;14:377-382. [PubMed] |
| 21. | Will U, Fueldner F, Goldmann B, Mueller AK, Wanzar I, Meyer F. Successful transgastric pancreaticography and endoscopic ultrasound-guided drainage of a disconnected pancreatic tail syndrome. Therap Adv Gastroenterol. 2011;4:213-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Will U, Füldner F, Reichel A, Meyer F. [EUS-guided drainage of the pancreatic duct (EUPD)--promising therapeutic alternative to surgical intervention in case of symptomatic retention of the pancreatic duct and unsuccessful ERP]. Zentralbl Chir. 2014;139:318-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Cahen DL, Gouma DJ, Nio Y, Rauws EA, Boermeester MA, Busch OR, Stoker J, Laméris JS, Dijkgraaf MG, Huibregtse K. Endoscopic versus surgical drainage of the pancreatic duct in chronic pancreatitis. N Engl J Med. 2007;356:676-684. [PubMed] |
| 24. | Delhaye M, Arvanitakis M, Verset G, Cremer M, Devière J. Long-term clinical outcome after endoscopic pancreatic ductal drainage for patients with painful chronic pancreatitis. Clin Gastroenterol Hepatol. 2004;2:1096-1106. [PubMed] |
| 25. | Eleftherladis N, Dinu F, Delhaye M, Le Moine O, Baize M, Vandermeeren A, Hookey L, Devière J. Long-term outcome after pancreatic stenting in severe chronic pancreatitis. Endoscopy. 2005;37:223-230. [PubMed] |
| 26. | Rösch T, Daniel S, Scholz M, Huibregtse K, Smits M, Schneider T, Ell C, Haber G, Riemann JF, Jakobs R. Endoscopic treatment of chronic pancreatitis: a multicenter study of 1000 patients with long-term follow-up. Endoscopy. 2002;34:765-771. [PubMed] |
| 27. | Smith MT, Sherman S, Ikenberry SO, Hawes RH, Lehman GA. Alterations in pancreatic ductal morphology following polyethylene pancreatic stent therapy. Gastrointest Endosc. 1996;44:268-275. [PubMed] |
| 28. | Kozarek RA. Pancreatic stents can induce ductal changes consistent with chronic pancreatitis. Gastrointest Endosc. 1990;36:93-95. [PubMed] |