Published online Dec 14, 2015. doi: 10.3748/wjg.v21.i46.13087
Peer-review started: May 25, 2015
First decision: June 25, 2015
Revised: August 11, 2015
Accepted: September 30, 2015
Article in press: October 8, 2015
Published online: December 14, 2015
Processing time: 198 Days and 20.2 Hours
AIM: To investigate clinical outcomes of chronic hepatitis B (CHB) and liver cirrhosis (LC) patients under whole-course management with lamivudine (LAM).
METHODS: This was a retrospective-prospective cohort study based on two nonrandom cohorts of Chinese patients (LAM group and history control group). Two hundred thirty-eight patients with LAM treatment for at least 12 mo under whole-course management were included in the LAM group. The management measures included regular follow-up and timely adjustment of the therapeutic regimen according to drug-resistance and relapse. Two hundred thirty-eight patients with CHB or LC without any antiviral treatment and with follow-up over 12 mo were included in the history control group. The LAM and control group patients were 1:1 matched by propensity score method to ensure both patients were similar in general datum, sex, age, E antigen, and diagnosis. The incidence rates of endpoint events [LC, hepatocellular carcinoma (HCC), and death] were compared between the LAM and control groups.
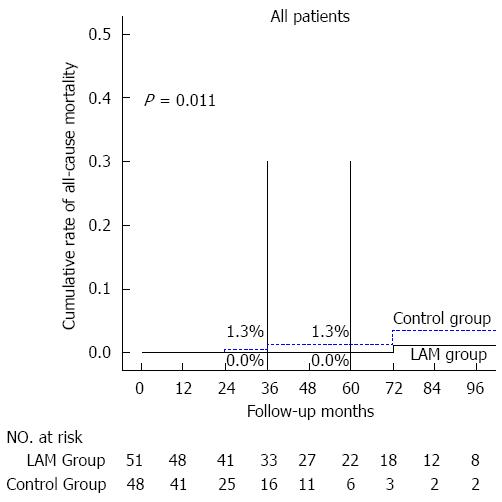
RESULTS: Hepatitis B virus-DNA < 1000 copies per mL rate and rate of alanine transaminase < 1.3 of the upper normal limit in LAM and control groups were 89.1% vs 18.5% (P < 0.05) and 89.8% vs 31.1% (P < 0.05), respectively. Viral breakthrough occurred in 77 patients (32.4%); the one-, three-, and five-year cumulative rates were 6.8%, 33.1%, and 41.3%, respectively. In total, 44.5% (106/238) of patients had once stopped LAM, and 63 (59.4%) of them developed virologic relapse; the relapse rate of patients with and without reaching Asian Pacific Association for the Study of the Liver endpoint criteria were 52.4% and 69.8%, respectively. Six CHB patients in the LAM group developed LC compared to 47 patients in the control group; the three-, and five-year cumulative rates of CHB at baseline of LAM were lower than those of the control group: 0.7% vs 12.0% and 1.8% vs 23.8% (P < 0.01), respectively. The incidence of HCC in CHB at baseline of LAM was lower than that of the control group; the three-, and five-year cumulative rates were 0% vs 3.2% and 1.1% vs 3.2% (P = 0.05), respectively. The incidence of HCC in LC at baseline of LAM was lower than that of the control group: 9.8% (5/51) vs 25.0% (12/48), and the three-, and five-year cumulative rates were 4.5% vs 20.7% and 8.1% vs 37.5% (P < 0.01), respectively. The mortality rate in the LAM group was lower than the control group.
CONCLUSION: Standardized long-term LAM treatment in combination with comprehensive management can reduce the incidence rates of LC and HCC as well as hepatitis B virus-related deaths.
Core tip: Drug resistance and disease relapse are inevitable during long-term lamivudine treatment in some patients. However, as long as standardized procedures in combination with comprehensive management are used, viral replication can be inhibited to a large extent. Thus, liver function in patients can be maintained at a stable status for a long time, and the incidence rates of liver cirrhosis and hepatocellular carcinoma, as well as hepatitis B virus-related deaths, may be reduced.
- Citation: Su MH, Lu AL, Li SH, Zhong SH, Wang BJ, Wu XL, Mo YY, Liang P, Liu ZH, Xie R, He LX, Fu WD, Jiang JN. Long-term lamivudine for chronic hepatitis B and cirrhosis: A real-life cohort study. World J Gastroenterol 2015; 21(46): 13087-13094
- URL: https://www.wjgnet.com/1007-9327/full/v21/i46/13087.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i46.13087
Hepatitis B virus (HBV) infection is a serious global public health problem. There are approximately two billion HBV infections worldwide, of which 3.5-400 million are chronic infections. Nearly one million people die from liver failure each year caused by HBV infection, liver cirrhosis (LC), or hepatocellular carcinoma (HCC)[1].
It has been demonstrated that amelioration of liver necroinflammation or cirrhosis can be achieved with antiviral therapy and inhibition of viral replication[2-5]. Thus, antiviral therapy is fundamentally important in the treatment of chronic hepatitis B (CHB)/LC patients. Two categories of therapeutic agents are currently available for the treatment of CHB: (1) immunomodulatory agents; and (2) oral nucleoside analogues (NAs). Due to its safety, convenience, variety, and fewer side effects, oral NAs are more widely applied than interferon. As one of the representatives of NAs, lamivudine (LAM) is widely used in China, especially in the less-developed areas, because of its low price.
LAM (approved in 1998) has been in application for more than ten years. Research reports suggested that LAM has a high potency in delaying disease progression when used in treatment of CHB/LC patients. However, a variety of situations are possible during clinical practice, including initial treatment, re-treatment, drug resistance, treatment stoppage, and relapse. How and whether these conditions affect the incidence of end-point events are not known. The current study evaluated the efficacy of long-term LAM treatment under the whole-course management in ALT improvement, virologic response, relapse after stopping treatment, and disease progression in CHB/LC patients.
All patients in this study were come from the Department of Infectious Diseases at the First Affiliated Hospital of Guangxi Medical University. The LAM treatment group included patients treated between February 2002 and April 2014. The history control group was comprised of CHB/LC patients from the same department that had been screened as outpatients and inpatients since 1990.
Inclusion criteria: (1) CHB/LC patients; (2) diagnosis met the “Viral Hepatitis Prevention and Control Program” documented in Xi’an meeting in 2000[6] and the Viral Hepatitis Management Guidelines of China in 2005; (3) hepatitis B surface antigen (HBsAg)-positive, abnormal alanine transaminase/aspartate transaminase (ALT/AST), detectable HBV-DNA, or hepatitis B e antigen (HBeAg)-positive and has been followed up at least 1 year; and (4) with LAM initial treatment at least 1 year in the LAM treatment group or without any antiviral treatment for the control group.
Exclusion criteria: co-infection with hepatitis C virus, hepatitis D virus, or human immunodeficiency virus; previous use of any immune inhibitors or oral antiviral agents, or HCC.
Patient profiles: By application of computer software, we established an electronic follow-up platform. The platform is used for storage of the general information, consultation, and experimental data. It also can be used for analysis when needed.
Planning and scheduling: Compliance with therapy was questioned. A clear plan for subjects according to their daily living habit was established. The chronicity and importance of nucleoside drug treatments, the possibility of adverse drug reactions, and precautions with detailed solutions were explained in detail at the beginning of the research.
Follow-up: All of the patients were followed-up periodically by clinic re-examination, letters, or telephone calls. The follow-up content included: (1) patient compliance; (2) symptoms outcome; (3) adverse reactions; (4) evaluation of the curative effect, combining previous experimental results and dosage schedule; (5) formulation of a further treatment plan; and (6) made an appointment for the next review.
The following data were collected: (1) HBV-DNA, HBV serologic makers, and liver function were investigated every month and 3 mo before and after the virologic response; (2) adverse effect: blood routine examination, renal function and creatine kinase; and (3) tumor monitor: liver ultrasound was conducted every 6 mo, alpha fetal protein was examined every 3 mo in HCC high-risk patients, and CT or MRI scans in patients with suspicious nodules.
A consultation and referral treatment system was established by cooperating with the radiology, ultrasonic, pathology, and liver surgery departments, and a clinical laboratory was established for early detection, diagnosis, and treatment of disease during the study.
Rescue therapy (including switching to or adding other NAs) was initiated immediately when LAM resistance was detected.
NA antiviral treatment was initiated immediately in relapse: (1) patients with LC or have aggravating trend (with total bilirubin > 3 times or with liver failure); and (2) patients with tolerable general condition (without LC or liver failure trend), but HBV DNA levels failed to become negative (defined as < 1.0 × 103 copies/mL).
The starting point was defined as when the cohort was established. Outcome events included LC occurrence in CHB patients, HCC occurrence in CHB patients with LC, and HBV-related death occurrence in CHB/LC patients. The primary endpoints were: (1) outcome event occurred; and (2) observed to the last follow-up without occurrence of outcome events.
The study was conducted according to the ethical guidelines of the 1975 Declaration of Helsinki and approved by the Human Ethics Committee of Guangxi Medical University. Informed consent was obtained in writing from each patient.
SPSS 18.0 software (SPSS Inc., Chicago, IL, United States) was used for all statistical analysis. Life-table method and multivariate Cox proportional hazards model (PHM) regression analyses were used to identify the variables/factors determining the clinical endpoint events. Categorical variables were defined as the proportion (%) and were compared by χ2 or Fisher’s exact tests. Continuous variables were defined as the mean ± SD or median (range) and tested with the Student’s t or Mann-Whitney U tests, as appropriate. A P < 0.05 was considered to be statistically significant.
All of the patients in this research were from the Department of Infectious Diseases, the First Affiliated Hospital of Guangxi Medical University. From the initial baseline cohort of 1404 patients established between February 2002 and April 2014, 238 patients met the final inclusion criteria and were included in the LAM group. The history control group was comprised of 238 patients, using 1:1 matching, who were recruited from the clinic, were hospitalized at some point since 1990, and were HBsAg-positive, had abnormal ALT/AST, detectable HBV-DNA or were HBeAg-positive, and have been followed-up at least 1 year.
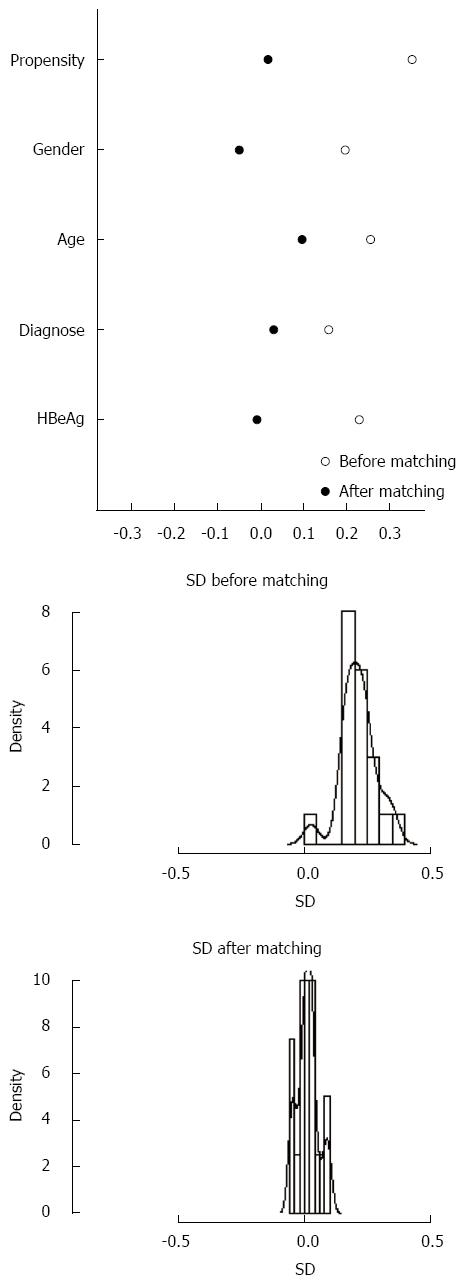
The propensity score method was conducted for matching the history control group; matching factors included: sex, age, baseline HBeAg, and diagnosis. The data distribution scatter diagram was drawn up before and after matching, and showed balanced after matching (P = 0.83) (Figure 1). The baseline characteristics are shown in Table 1.
| Characteristic | LAM group | History control group | ||||
| No. | CHB | LC | No. | CHB | LC | |
| (n = 238) | (n = 187) | (n = 51) | (n = 238) | (n = 190) | (n = 48) | |
| Age (mean ± SD) | 35.9 ± 11.7 | 33.3 ± 10.3 | 45.5 ± 11.6 | 34.7 ± 11.5 | 32.3 ± 9.9 | 44.4 ± 12.0 |
| Sex, n (%) | 197 (74.3) | 149 (70.6) | 48 (88.9) | 197 (74.3) | 153 (72.2) | 44 (83) |
| Base HBeAg-positive, n (%) | 153 (57.7) | 134 (63.5) | 19 (35.2) | 157 (59.2) | 139 (65.6) | 18 (34) |
| Base ALT (U/mL) | 150 | 157 | 124 | 212 | 221 | 173 |
| Base HBV-DNA (copy/mL) | 5.85E+7 | 7.3E+7 | 5.4E+6 | 3.6E+7 | 2.1E+7 | 8.4E+7 |
| Follow-up time (yr) | 5.1 (1.0-13.2) | 5.0 (1.0-13.2) | 5.2 (1.1-11.6) | 3.8 (1.0-17.6) | 3.9 (1.0-17.6) | 3.1 (1.0-15.0) |
Of 238 cases in the LAM group, most (212 patients, 89.1%) achieved undetectable HBV DNA in the last interview within the follow-up period, and 213 patients (89.8%) demonstrated ALT improvement (ALT < 1.3 lower limit of normal). In the history control group, 44 patients (18.5%) achieved undetectable HBV DNA, and 74 patients (31.1%) showed ALT improvement.
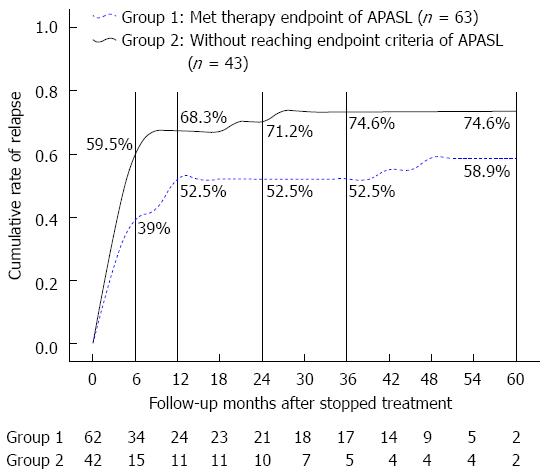
In the LAM group, viral breakthrough occurred in 77 patients (32.4%); the one-, three-, and five-year cumulative rates were 6.8%, 33.1%, and 41.3%, respectively, and the annual rate was 10.5%. There were 106/238 (44.5%) patients that had once stopped LAM, and 63 (59.4%) of these developed virologic relapse. The relapse rates of patients with and without reaching Asian Pacific Association for the Study of the Liver (APASL) endpoint criteria were 52.4% (33/63) and 69.8% (30/43), respectively.
The distribution of cumulative relapse rates after stopping LAM with and without reaching the criteria in month 3, month 6, year 1, year 2, year 3, and year 5 were 24.2% vs 35.3%, 39.0% vs 59.5%, 52.5% vs 68.3%, 52.5% vs 71.2%, 52.5% vs 74.6%, and 58.9% vs 74.6%, respectively (Figure 2).
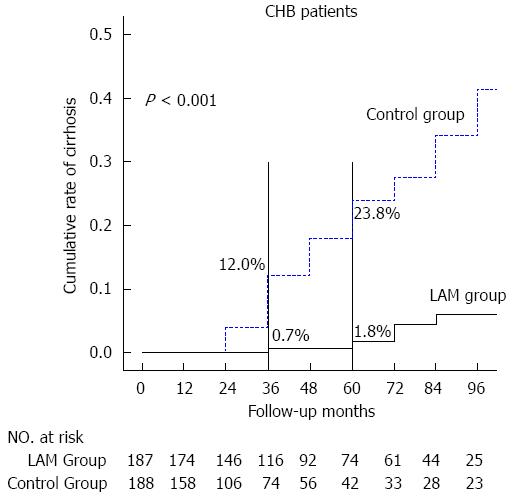
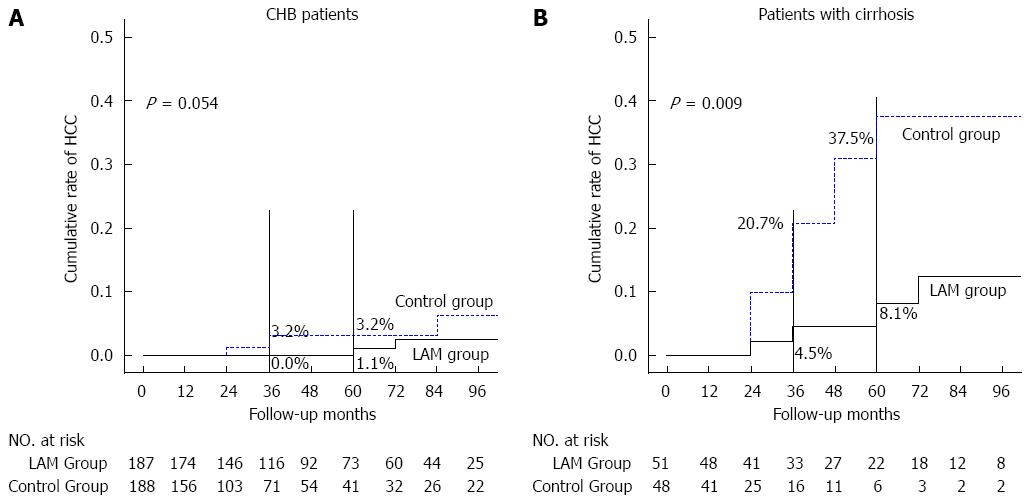
In the LAM group, among the 78.6% (187/238) of CHB patients at baseline, 3.2% (6/187) progressed to LC and 1.1% (2/187) progressed to HCC. Whereas in the history control group, 25.0% (47/190) progressed to LC (P = 0.01) and 3.7% (7/190) progressed to HCC (P = 0.05). Of the 51 (21.4%) LC patients in LAM group and 48 (20.2%) in the history control group at baseline, 5 (9.8%) and 12 (25%) patients, respectively, progressed to HCC (P = 0.09) and the three-, and five-year cumulative rates were 4.5% vs 20.7% and 8.1% vs 37.5% (P < 0.01), respectively. Furthermore, there was 1 (2.0%) patient who died in the LAM group compared to 3 (6.3%) in the history control group (P = 0.01). The disease progressions are listed by life table in Figures 3, 4 and 5.
The Cox PHM was used for multivariate analyses, in which sex, age, stoppage of treatment, family history of hepatitis B, baseline HBeAg, resistance, HBV-DNA, baseline ALT, and baseline diagnosis were evaluated for the prediction of CHB progression in the LAM group. Receiver operating characteristic (ROC) curves were constructed and the area under the ROC curves was also computed. A probability level (P) of 0.05 was chosen for statistical significance.
It was observed that baseline age (RR = 1.115, 95%CI: 1.04-1.196, P < 0.01) and LC (RR = 8.86, 95%CI: 1.17-45.69, P < 0.01) were the independent risk factors of CHB in progression to HCC. LC showed the highest area under the ROC value (8.86, 95%CI: 1.17-45.69, P < 0.01), followed by baseline age (1.12, 95%CI: 1.04-1.20, P < 0.01) (Table 2).
| Factor | Assignment |
| Sex | |
| Male | 1 |
| Female | 0 |
| Age | Age |
| Stop treatment | |
| Stop | 1 |
| Never stop | 0 |
| Family history | |
| No | 0 |
| Unknown | 1 |
| Yes | 2 |
| Baseline HBeAg | |
| HBeAg-negative | 1 |
| HBeAg-positive | 0 |
| Viral breakthrough | |
| Yes | 1 |
| No | 0 |
| Baseline DNA level (copy/mL) | |
| < 104 | 0 |
| 104-99999 | 1 |
| 105-999999 | 2 |
| ≥ 106 | 3 |
| Baseline ALT | ALT (IU/mL) |
| Diagnose | |
| LC | 1 |
| CHB | 0 |
It is reported that amelioration of liver necroinflammation or cirrhosis could be achieved with antiviral therapy by inhibition of viral replication[7,8]. Therefore, antiviral therapy is fundamentally important in the treatment of CHB/LC patients.
The current study aimed to (1) evaluate the efficacy of long-term LAM treatment under the whole-course management in CHB/LC progression; and (2) analyze the related risk factors. The long-term use of LAM treatment resulted in resistance. The resistance rates of CHB patients underwent LAM treatment at one, two, three, four, and five years was 14.7% (4.8%-23.5%), 37.8% (14.3%-65.9%), 49.8% (30.2%-70.5%), 62.0% (52.0%-67.0%), and 70.8%, respectively. Previous reports indicated that the resistance rate rose with the LAM treatment extending[9-12].
In our study, there were 77 (32.4%) patients who developed virologic breakthrough (the annual rate was 10.5%), and the cumulative rates in year 1, year 3 and year 5, were 6.8%, 33.1%, and 41.3%, respectively. The virologic breakthrough rate in our study was consistent with the current rate in China. Stoppage of treatment was inevitable during the long-term antiviral therapy for several reasons, including stoppage for reaching the criteria, economic burden, or pregnancy. However, virologic relapse happened more often with LAM treatment. Luo et al[13] observed 26 patients with average 20-mo LAM treatment, and found a relapse rate of 80.77% (21/26). Wang et al[14] observed 82 HBeAg-positive patients with 24-mo LAM treatment on average, an reported relapse rates in year 1, year 2, year 3, and year 4 of 23.4%, 25%, 25%, and 29.4%, respectively. In our study, 44.5% patients (106/238) had once stopped LAM treatment, and 63 (59.4%) of them developed virologic relapse; the relapse rate of patients with and without reaching APASL endpoint criteria were 52.4% and 69.8%, respectively. Overall, more than half of the CHB patients experienced relapse after stopping treatment. Furthermore, the relapse rate in stop-treatment patients who failed to reach the APASL endpoint criteria was much higher than those reaching APASL endpoint criteria. These results indicate that relapse in CHB/LC patients may be associated with the antiviral therapy duration.
CHB may cause serious events such as LC, liver failure, and HCC without effective control. A number of studies have found that the incidence rate of LC varies from 0.9% to 16.0%, while the HCC incidence rate ranges from 0.3% to 7.2%[15-23].
HBV DNA ≥ 2000 IU/mL is an independent HCC risk factor[24]. Long-term LAM treatment can reverse LC and eventually delay CHB/LC progression. A randomized controlled trial indicated that liver fibrosis and liver dysfunction effectively slow down with long-term LAM treatment[25]. Matsumoto et al[26] also suggested that long-term LAM treatment effectively reduces the incidence of HCC in patients with CHB. The HCC incidence in LC was 3%-6%, significantly higher than non-LC CHB patients[27]. A prospective study followed up CHB/LC patients for 4.5 years; HCC incidence at years 1, 3, 5, 7, and 10 were significantly higher in patients with cirrhosis (8.1%, 17.5%, 43.2%, 46.7%, and 53.4%, respectively) than CHB (1.6%, 3.5%, 3.5%, 7.1%, and 29.6%, respectively), with no difference between ETV and LAM[28]. Kurokawa et al[29] followed up 293 HBV patients for an average of 67.6 mo and found that the cumulative carcinogenesis rate at years 3, 5, and 7 were 2%, 3%, and 5% in patients with CHB and 15%, 30%, and 35% in LC, respectively[30]. Long-term LAM treatment can achieve HBsAg clearance in HBeAg-negative CHB patients.
In our study, there were 187 CHB patients receiving LAM treatment under the whole-course management, with five years follow-up on average. Of these, six patients progressed to LC; the cumulative rates in years 3, 5 and 10 were 0.7%, 1.8%, and 9.8%, respectively. Meanwhile, two patients developed HCC, and the cumulative rates in years 3, 5, and 10 were 0%, 1.1%, and 2.5%, respectively. The average annual rates in progress to LC and HCC were 0.6% and 0.2%, respectively. There were 51 (in the LAM group) and 48 (in the history control group) LC patients at baseline, of which 5 (9.8%) and 12 (25%) progressed to HCC; the average annual rates were 1.9% and 7.5%, while the three- and five-year cumulative rates were 4.5% vs 20.7% and 8.1% vs 37.5%, respectively. The incidence of LC in CHB was significantly lower than in the control group, which indicates that the LAM treatment under whole-course management may be helpful in reducing the development of CHB to LC. Moreover, the HCC incidence in CHB with LC at baseline of the LAM group was also lower than that of the control group. Unfortunately, the relatively small study sample may affect the comparison results, thus, larger sample sizes are necessary in future studies. The cumulative rate and annual rate of HCC and LC in HBV patients was consistent with previous reports, which also suggests the effectiveness of antiviral therapy in CHB.
In conclusion, this study shows that the long-term LAM treatment under whole-course management can achieve undetectable levels of HBV-DNA and normalize ALT levels, and thus, reduce the incidence rates of LC and HCC in CHB/LC patients. Furthermore, this study also indicates that baseline age is an independent risk factor for CHB patients who develop LC, while LC and HbeAg negative, age at baseline are the first and second risk factors for development of HCC, respectively.
Hepatitis B virus (HBV) infection is a serious global public health problem. Nearly one million people die from liver failure each year caused by HBV infection, liver cirrhosis, or hepatocellular carcinoma (HCC). Viral replication is the independent risk factor that leads to progression of disease, thus, antiviral therapy is the key point in treatment of patients with HBV infection.
Research reports suggest lamivudine (LAM) has high potency in delaying the disease progression when used to treat patients with liver cirrhosis (LC) and cancer. However, a variety of situations are possibly during clinical practice, including initial treatment, re-treatment, drug resistance, treatment stoppage, and relapse. Present randomized clinical trials are not sufficient to cover all of these patients.
This study, as a retrospective and perspective analysis, evaluated the efficacy of long-term LAM treatment under the whole-course management in ALT improvement, virologic response, relapse after stoppage of treatment, and disease progression in chronic hepatitis B (CHB)/LC patients.
Long-term LAM treatment combined with the whole-course management may reduce the incidence rates of LC and liver cancer, as well as the death rates related with HBV infection. Old baseline age is the independent risk factor of LC, while cirrhosis diagnosed at baseline is the independent risk factor of liver cancer.
The research is well designed, and the manuscript is good. In this study, the authors investigated the real-life clinical outcomes of CHB and LC patients after LAM treatment under whole-course management. This retrospective-prospective cohort study is based on two nonrandom cohorts of Chinese patients. The authors found that the incidences of HCC in CHB and in LC at baseline of LAM were lower than those of the control group. Viral breakthrough and relapse were inevitable during long-term LAM treatment, the maximum efforts to enable undetectable HBV-DNA levels and normalize alanine transaminase in CHB/LC patients under whole-course management can reduce the incidence rates of LC and HCC.
P- Reviewer: Lion M, Rozzini R S- Editor: Yu J L- Editor: Filipodia E- Editor: Ma S
| 1. | Lavanchy D. Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J Viral Hepat. 2004;11:97-107. [PubMed] |
| 2. | Xu B, Lin L, Xu G, Zhuang Y, Guo Q, Liu Y, Wang H, Zhou X, Wu S, Bao S. Long-term lamivudine treatment achieves regression of advanced liver fibrosis/cirrhosis in patients with chronic hepatitis B. J Gastroenterol Hepatol. 2015;30:372-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Hu P, Zhao GD, Li H, Gao T, Li ST, Tang WL, Zhou HJ, Wang H, Xie Q. [Effects of oral antiviral agents on long-term outcomes of treatment-naive patients with HBV-related decompensated cirrhosis: a retrospective cohort study]. Zhonghua Ganzangbing Zazhi. 2014;22:806-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Berak H, Wasilewski M, Horban A, Stańczak JJ, Cybula A. [Results of 48 weeks lamivudine treatment of patients with chronic hepatitis B and HBeAg (+)]. Przegl Epidemiol. 2006;60:253-257. [PubMed] |
| 5. | Jang JW, Choi JY, Kim YS, Woo HY, Choi SK, Lee CH, Kim TY, Sohn JH, Tak WY, Han KH. Long-term effect of antiviral therapy on disease course after decompensation in patients with hepatitis B virus-related cirrhosis. Hepatology. 2015;61:1809-1820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 118] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 6. | Chinese Society of Hepatology, CMA. Viral hepatitis prevention plan [J]. Zhonghua Ganzangbing Zazhi. 2000;8:324-329. |
| 7. | Papachrysos N, Hytiroglou P, Papalavrentios L, Sinakos E, Kouvelis I, Akriviadis E. Antiviral therapy leads to histological improvement of HBeAg-negative chronic hepatitis B patients. Ann Gastroenterol. 2015;28:374-378. [PubMed] |
| 8. | Sakamoto K, Beppu T, Hayashi H, Nakagawa S, Okabe H, Nitta H, Imai K, Hashimoto D, Chikamoto A, Isiko T. Antiviral therapy and long-term outcome for hepatitis B virus-related hepatocellular carcinoma after curative liver resection in a Japanese cohort. Anticancer Res. 2015;35:1647-1655. [PubMed] |
| 9. | Sun KX, Li J, Zhuang H. Chinese patients with chronic hepatitis b antiviral treatment of drug resistance. Chinese Hepatology. 2011;16:147-149. [DOI] [Full Text] |
| 10. | Jia HY, Lu W, Zheng L, Ying LJ, Yang YD. [Efficacy of lamivudine monotherapy and combination therapy with adefovir dipivoxil for patients with hepatitis B virus-related decompensated cirrhosis]. Zhonghua Ganzangbing Zazhi. 2011;19:84-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Xu H, Chen Y, He LL, Lei BJ, Lei XZ. [Lamivudine-resistant analysis and management for chronic hepatitis B patients with initial lamivudine therapy]. Zhonghua Ganzangbing Zazhi. 2011;19:427-430. [PubMed] |
| 12. | Scotto G, Palumbo E, Fazio V, Cibelli DC, Saracino A, Tartaglia A, Angarano G. Prolonged lamivudine treatment in patients with chronic active anti-HBe-positive hepatitis. Am J Ther. 2006;13:218-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Luo SQ, Zhang LX, Zhang WJ, Cai SP, Gao F. Clinical observation on the relapse of lamivudine withdrawal chronic hepatitis B. Zhonghua Ganzangbing Zazhi. 2005;7:200-202. [DOI] [Full Text] |
| 14. | Wang L, Liu F, Liu YD, Li XY, Wang JB, Zhang ZH, Wang YZ. Stringent cessation criterion results in better durability of lamivudine treatment: a prospective clinical study in hepatitis B e antigen-positive chronic hepatitis B patients. J Viral Hepat. 2010;17:298-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Fattovich G, Brollo L, Giustina G, Noventa F, Pontisso P, Alberti A, Realdi G, Ruol A. Natural history and prognostic factors for chronic hepatitis type B. Gut. 1991;32:294-298. [PubMed] |
| 16. | Liaw YF, Tai DI, Chu CM, Chen TJ. The development of cirrhosis in patients with chronic type B hepatitis: a prospective study. Hepatology. 1988;8:493-496. [PubMed] |
| 17. | Wu G, Zhou W, Zhao Y, Guo S, Wang Z, Zou S, Zhang Q, Ren H, Huang A, Zhang D. [Study on the natural history of chronic hepatitis B]. Zhonghua Ganzangbing Zazhi. 2002;10:46-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 18. | Lin SM, Yu ML, Lee CM, Chien RN, Sheen IS, Chu CM, Liaw YF. Interferon therapy in HBeAg positive chronic hepatitis reduces progression to cirrhosis and hepatocellular carcinoma. J Hepatol. 2007;46:45-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 243] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 19. | Hsu YS, Chien RN, Yeh CT, Sheen IS, Chiou HY, Chu CM, Liaw YF. Long-term outcome after spontaneous HBeAg seroconversion in patients with chronic hepatitis B. Hepatology. 2002;35:1522-1527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 508] [Cited by in RCA: 508] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 20. | Huang H, Zhu TW, Yu XF, Wang GS, Wang JY. The development of cirrhosis in Chinese patients with chronic hepatitis B. Chin J hepatol. 2007;12:437-440. [DOI] [Full Text] |
| 21. | Beasley RP, Hwang LY, Lin CC, Chien CS. Hepatocellular carcinoma and hepatitis B virus. A prospective study of 22 707 men in Taiwan. Lancet. 1981;2:1129-1133. [PubMed] |
| 22. | Di Marco V, Lo Iacono O, Cammà C, Vaccaro A, Giunta M, Martorana G, Fuschi P, Almasio PL, Craxì A. The long-term course of chronic hepatitis B. Hepatology. 1999;30:257-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 164] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 23. | Xu B, Hu DC. A retrospective cohort study on the natural history of chronic hepatitis B in Shanghai, China. Zhonghua Neike Zazhi. 2002;41:384-387. [DOI] [Full Text] |
| 24. | Chu CM, Lin CC, Lin SM, Lin DY, Liaw YF. Viral load, genotypes, and mutants in hepatitis B virus-related hepatocellular carcinoma: special emphasis on patients with early hepatocellular carcinoma. Dig Dis Sci. 2012;57:232-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Liaw YF, Sung JJ, Chow WC, Farrell G, Lee CZ, Yuen H, Tanwandee T, Tao QM, Shue K, Keene ON, Dixon JS, Gray DF, Sabbat J. Lamivudine for patients with chronic hepatitis B and advanced liver disease. N Engl J Med. 2004;351:1521-1531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1739] [Cited by in RCA: 1740] [Article Influence: 82.9] [Reference Citation Analysis (0)] |
| 26. | Matsumoto A, Tanaka E, Rokuhara A, Kiyosawa K, Kumada H, Omata M, Okita K, Hayashi N, Okanoue T, Iino S. Efficacy of lamivudine for preventing hepatocellular carcinoma in chronic hepatitis B: A multicenter retrospective study of 2795 patients. Hepatol Res. 2005;32:173-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 149] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 27. | Liaw YF, Leung N, Kao JH, Piratvisuth T, Gane E, Han KH, Guan R, Lau GK, Locarnini S. Asian-Pacific consensus statement on the management of chronic hepatitis B: a 2008 update. Hepatol Int. 2008;2:263-283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 666] [Cited by in RCA: 743] [Article Influence: 43.7] [Reference Citation Analysis (0)] |
| 28. | Kobashi H, Miyake Y, Ikeda F, Yasunaka T, Nishino K, Moriya A, Kubota J, Nakamura S, Takaki A, Nouso K. Long-term outcome and hepatocellular carcinoma development in chronic hepatitis B or cirrhosis patients after nucleoside analog treatment with entecavir or lamivudine. Hepatol Res. 2011;41:405-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 29. | Kurokawa M, Hiramatsu N, Oze T, Yakushijin T, Miyazaki M, Hosui A, Miyagi T, Yoshida Y, Ishida H, Tatsumi T. Long-term effect of lamivudine treatment on the incidence of hepatocellular carcinoma in patients with hepatitis B virus infection. J Gastroenterol. 2012;47:577-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 30. | Fasano M, Lampertico P, Marzano A, Di Marco V, Niro GA, Brancaccio G, Marengo A, Scotto G, Brunetto MR, Gaeta GB. HBV DNA suppression and HBsAg clearance in HBeAg negative chronic hepatitis B patients on lamivudine therapy for over 5 years. J Hepatol. 2012;56:1254-1258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |