Published online Dec 7, 2015. doi: 10.3748/wjg.v21.i45.12976
Peer-review started: May 8, 2015
First decision: July 10, 2015
Revised: August 5, 2015
Accepted: October 13, 2015
Article in press: October 13, 2015
Published online: December 7, 2015
Processing time: 219 Days and 17.6 Hours
Traditionally, perivaterian duodenal perforation can be managed conservatively or surgically. If a large volume of leakage results in fluid collection in the retroperitoneum, surgery may be necessary. Our case met the surgical indication for perivaterian duodenal perforation after endoscopic retrograde cholangiopancreatography (ERCP) with sphincterotomy and endoscopic papillary balloon dilatation. The patient developed a retroperitoneal abscess after the procedures, and a perivaterian perforation was suggested on computed tomography (CT). CT-guided abscess drainage was performed immediately. We unsuccessfully attempted to close the perforation with hemoclips initially. Subsequently, we used fibrin sealant (Tisseel) injection to occlude the perforation. Fibrin sealant injections have been previously used during endoscopy for wound closure and fistula repair. Based on our report, fibrin sealant injection can be considered as an alternative method for the treatment of ERCP-related type II perforations.
Core tip: Perivaterian duodenal perforation can be managed conservatively or surgically. Our patient underwent endoscopic retrograde cholangiopancreatography (ERCP) with sphincterotomy and endoscopic papillary balloon dilatation, and developed a perivaterian duodenal perforation after the procedures. Computed tomography-guided abscess drainage was performed immediately but without improvement, and fibrin sealant (Tisseel) injection was then administered to occlude the perforation. The patient recovered uneventfully. This report shows that fibrin sealant injection can be an alternative method for the treatment of ERCP-related type II perforations.
- Citation: Yang HY, Chen JH. Endoscopic fibrin sealant closure of duodenal perforation after endoscopic retrograde cholangiopancreatography. World J Gastroenterol 2015; 21(45): 12976-12980
- URL: https://www.wjgnet.com/1007-9327/full/v21/i45/12976.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i45.12976
Endoscopic retrograde cholangiopancreatography (ERCP) with sphincterotomy (EST) and/or endoscopic papillary balloon dilatation (EPBD) is commonly used in the treatment of common bile duct (CBD) stones. However, ERCP is an invasive procedure that may lead to potential complications such as pancreatitis, hemorrhage, bowel perforation, and cholangitis. ERCP-related perforations are uncommon with a reported incidence of 0.3%-1.3%[1-3].
There are four types of ERCP-related bowel perforations[4-6]: lateral wall duodenal perforation (Type I), perivaterian perforation (Type II), perforation of the biliary tree (Type III), and retroperitoneal air alone (Type IV). Traditionally, lateral wall duodenal perforations (Type I) tend to be large and usually require surgical intervention[5,7,8]. Other types of perforation can be managed either conservatively or surgically[9,10]. If a large volume of leakage results in a fluid collection in the retroperitoneum, surgery or interventional drainage may be necessary.
Here, we describe a case of a perivaterian duodenal perforation (Type II) after ERCP with EST and EPBD that was successfully sealed with fibrin glue.
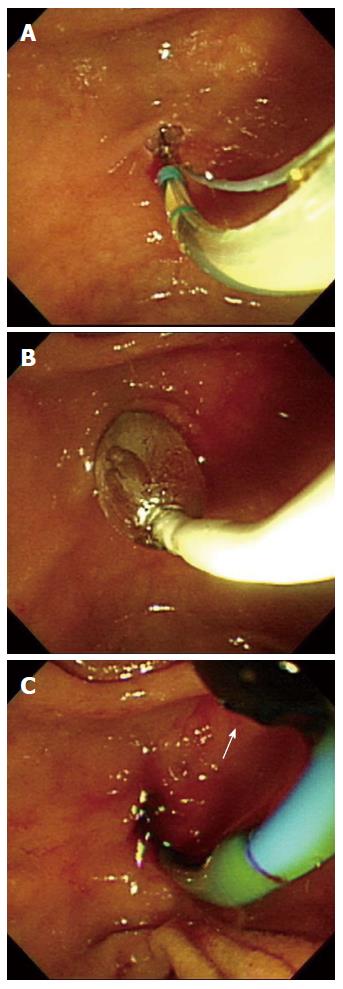
A 70-year-old man who had coronary artery disease and hypertension presented with symptomatic CBD stones and cholangitis. The patient had a history of gallbladder stones with acute cholecystitis and had undergone laparoscopic cholecystectomy 4 years previously. After hospital admission, he underwent ERCP with EST and EPBD (0.8 cm, 8 atm × 3 min), and a black stone was extracted with a balloon catheter (Figure 1A-C).
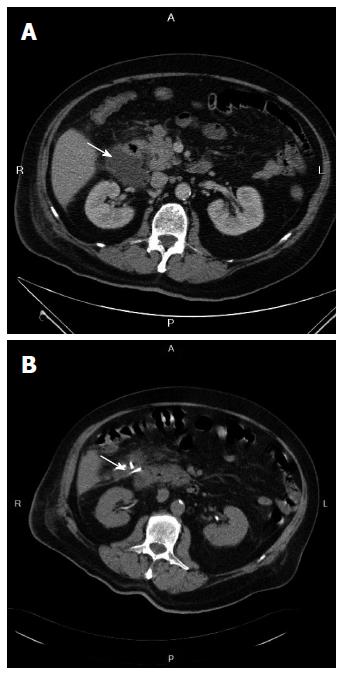
Fever and right flank pain were noted soon after the procedure. Initially, plain abdominal radiography and abdominal ultrasound revealed no obvious free air. Three days later, abdominal ultrasonography and abdominal computed tomography (CT) showed a retroperitoneal abscess (Figure 2A) close to the right lateral wall of the duodenum, suggesting a perivaterian perforation. CT-guided abscess drainage was performed immediately (Figure 2B).
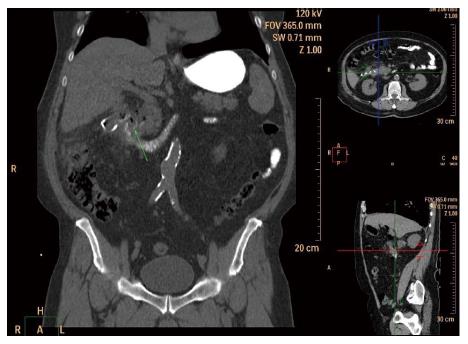
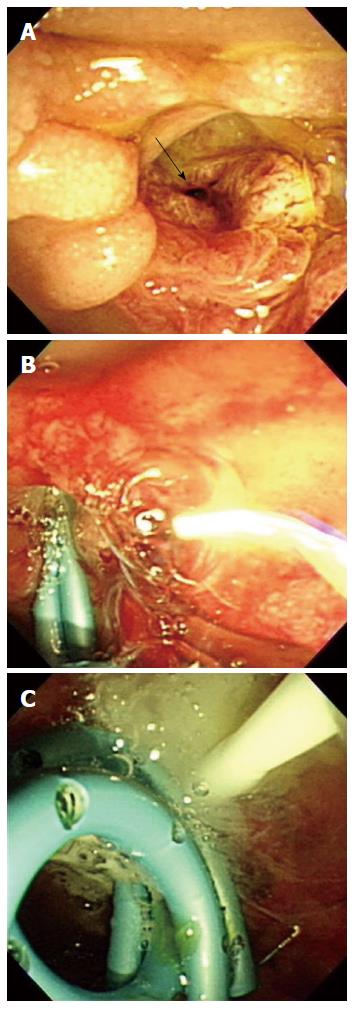
Another abdominal CT scan with oral contrast ingestion was performed on day 10 after ERCP due to persistent drainage of a large amount of purulent material. The scan revealed minimal contrast and air leakage from the duodenum into the right anterior pararenal space (Figure 3). On the same day, ERCP revealed a perforation of the perivaterian duodenum (Figure 4A). We unsuccessfully attempted to close the perforation with hemoclips initially. Subsequently, we used fibrin sealant (Tisseel; Baxter Healthcare, Deerfield, IL, United States) injection to occlude the perforation. Before injection of the fibrin sealant, we placed two 7F double pigtail (5 and 6 cm) plastic biliary stents into the CBD to prevent occlusion of the biliary orifice by the fibrin sealant (Figure 4B). A total of 4 mL Tisseel was injected into the perforation site (Figure 4C).
The patient’s fever had subsided by the day following application of the fibrin sealant, and the amount of purulent drainage decreased from 60-70 to 20 mL/d by day 2 after the procedure. Five days later, the amount of purulent drainage had decreased to < 10 mL/d and the patient’s abdominal discomfort continued to improve. He recovered uneventfully and was discharged on day 14 after fibrin sealant injection. Follow-up CT scan 2 wk later revealed an unremarkable retroperitoneal space without abscess formation or a detectable leak.
We described a case of perivaterian duodenal perforation in a patient after undergoing ERCP with EST and EPBD. He subsequently developed a retroperitoneal abscess that required percutaneous CT-guided drainage. However, his condition did not improve because of a persistent leak from the duodenal perforation. Surgical repair was not desirable because of the patient’s age and comorbidity.
Several endoscopic closure techniques have been described for closure of gastrointestinal perforations including the use of endoclips, fibrin sealant[11,12], endoloops, and the over-the-scope clip system[13]. Most of these approaches have been used for Type I perforations. For Type II perforations, previous studies have suggested conservative treatment first, followed by surgical intervention if conservative treatment fails. In this case, endoscopic repair with hemoclips was initially attempted, but failed. Subsequently, we were able to occlude the perforation without surgical intervention using fibrin sealant (Tisseel) injection.
Tisseel is a fibrin sealant used as an adjunct to hemostasis. It contains human fibrinogen, human factor XIII, aprotinin, polysorbate 80, human thrombin, and calcium chloride. Mixed together, the above ingredients form a cell-free clot that can block the perforation. In contrast to cyanoacrylate mixed with lipiodol, Tisseel has been shown to have tissue-healing properties and to be fully reabsorbed by macrophages and fibroblasts within 2 wk of application[14,15]. Fibrin sealant injections have been previously used during endoscopy for wound closure and fistula repair[16]. Only a few cases of duodenal perforation have been successfully treated with tissue sealant[11,12]. Based on our report, fibrin sealant (Tisseel) injection can be considered as an alternative method for the treatment of ERCP-related Type II perforations.
A 70-year-old man who had coronary artery disease and hypertension presented with epigastralgia for 1 wk, accompanied with skin discoloration and tea color urine.
Common bile duct (CBD)-stone related obstruction jaundice, underwent endoscopic retrograde cholangiopancreatography (ERCP), sphincterectomy and endoscopic papillary balloon dilatation, and stone retrieval by balloon catheter. Fever, abdominal pain and flank pain were found after the procedures. Post-ERCP bowel perforation was found with intra-abdominal abscess formation.
Post-ERCP pancreatitis, bowel perforation, ascending cholangitis, urine track infection or renal stone.
Leukocytosis with left shift and high C-reactive protein level after the procedure. Normal lipase level and liver function tests.
Computed tomography showed periampullary duodenal microperforation-related collection/abscess at the right retroperitoneal space.
The authors placed two 7F double pigtail (5 and 6 cm) plastic biliary stents into the CBD to prevent occlusion of the biliary orifice, then 4 mL fibrin sealant (Tisseel) was injected into the perforation site.
For delayed wound healing of post-ERCP Type II bowel perforation, surgical intervention was needed. Only a few reports have mentioned endoscopic treatment. The authors tried fibrin sealant (Tisseel) injection, which was used for surgical wound healing, and achieved a good outcome.
Fibrin sealant (Tisseel) injection can be considered as an alternative method for the treatment of ERCP-related Type II perforations.
A new technique for the management of post-ERCP perforation is presented. It is well written and illustrated.
P- Reviewer: Kate V S- Editor: Yu J L- Editor: A E- Editor: Wang CH
| 1. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1890] [Cited by in RCA: 2036] [Article Influence: 59.9] [Reference Citation Analysis (1)] |
| 2. | Scarlett PY, Falk GL. The management of perforation of the duodenum following endoscopic sphincterotomy: a proposal for selective therapy. Aust N Z J Surg. 1994;64:843-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Loperfido S, Angelini G, Benedetti G, Chilovi F, Costan F, De Berardinis F, De Bernardin M, Ederle A, Fina P, Fratton A. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998;48:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 801] [Cited by in RCA: 779] [Article Influence: 28.9] [Reference Citation Analysis (1)] |
| 4. | Howard TJ, Tan T, Lehman GA, Sherman S, Madura JA, Fogel E, Swack ML, Kopecky KK. Classification and management of perforations complicating endoscopic sphincterotomy. Surgery. 1999;126:658-663; discussion 664-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 114] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Enns R, Eloubeidi MA, Mergener K, Jowell PS, Branch MS, Pappas TM, Baillie J. ERCP-related perforations: risk factors and management. Endoscopy. 2002;34:293-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 179] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 6. | Stapfer M, Selby RR, Stain SC, Katkhouda N, Parekh D, Jabbour N, Garry D. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg. 2000;232:191-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 238] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 7. | Fatima J, Baron TH, Topazian MD, Houghton SG, Iqbal CW, Ott BJ, Farley DR, Farnell MB, Sarr MG. Pancreaticobiliary and duodenal perforations after periampullary endoscopic procedures: diagnosis and management. Arch Surg. 2007;142:448-454; discussion 454-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 79] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 8. | Masci E, Toti G, Mariani A, Curioni S, Lomazzi A, Dinelli M, Minoli G, Crosta C, Comin U, Fertitta A. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001;96:417-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 625] [Cited by in RCA: 613] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 9. | Park WY, Cho KB, Kim ES, Park KS. A case of ampullary perforation treated with a temporally covered metal stent. Clin Endosc. 2012;45:177-180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Vezakis A, Fragulidis G, Nastos C, Yiallourou A, Polydorou A, Voros D. Closure of a persistent sphincterotomy-related duodenal perforation by placement of a covered self-expandable metallic biliary stent. World J Gastroenterol. 2011;17:4539-4541. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Mutignani M, Iacopini F, Dokas S, Larghi A, Familiari P, Tringali A, Costamagna G. Successful endoscopic closure of a lateral duodenal perforation at ERCP with fibrin glue. Gastrointest Endosc. 2006;63:725-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 38] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Kim KW, Lee TH, Park SH, Son BS, Lee SH, Lee SH, Chung IK, Kim SJ. A primary repair with hemoclips and fibrin glue injection in biliary stent induced duodenal perforation. Korean J Gastrointest Endosc. 2011;42:437-441. |
| 13. | Buffoli F, Grassia R, Iiritano E, Bianchi G, Dizioli P, Staiano T. Endoscopic “retroperitoneal fatpexy” of a large ERCP-related jejunal perforation by using a new over-the-scope clip device in Billroth II anatomy (with video). Gastrointest Endosc. 2012;75:1115-1117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Becker JC, Beckbauer M, Domschke W, Herbst H, Pohle T. Fibrin glue, healing of gastric mucosal injury, and expression of growth factors: results from a human in vivo study. Gastrointest Endosc. 2005;61:560-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Pescatore P, Verbeke C, Härle M, Manegold BC. Fibrin sealing in peptic ulcer bleeding: the fate of the clot. Endoscopy. 1998;30:519-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Petersen B, Barkun A, Carpenter S, Chotiprasidhi P, Chuttani R, Silverman W, Hussain N, Liu J, Taitelbaum G, Ginsberg GG. Tissue adhesives and fibrin glues. Gastrointest Endosc. 2004;60:327-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 86] [Article Influence: 4.1] [Reference Citation Analysis (0)] |