Published online Sep 7, 2015. doi: 10.3748/wjg.v21.i33.9822
Peer-review started: April 23, 2015
First decision: May 18, 2015
Revised: May 26, 2015
Accepted: July 8, 2015
Article in press: July 8, 2015
Published online: September 7, 2015
Processing time: 138 Days and 19.5 Hours
Non-functioning pancreatic neuroendocrine tumors (NF-PNETs) are rare tumors that account for 2% of all pancreatic malignancy. About 60% of NF-PNETs present distant metastases and usually hepatic metastases. However, cutaneous metastases are very rare. Herein, we report our experience with a 60-year-old male who visited our outpatient clinic with a mass on his left hip. An abdominal computerized tomography scan demonstrated not only a left hip mass and an enlarged left inguinal lymph node, but also a huge heterogeneous enhancing mass on the pancreas. Initially, we removed the metastatic lesions, which was a small cell neuroendocrine carcinoma with 50% of the Ki-67 index in the histopathological report. After 3 wk, we performed a total pancreatectomy and a total gastrectomy. Four weeks after the 1st operation, we detected a recurrence at the operative bed on his left hip, and subsequently removed the recurring mass. The patient was receiving chemotherapy based on etoposide and cisplatin treatment.
Core tip: We report the first known case of cutaneous metastasis as an initial presentation of a high grade non-functional pancreatic neuroendocrine tumor treated by surgical resection of both primary and metastatic lesions.
- Citation: Shin WY, Lee KY, Ahn SI, Park SY, Park KM. Cutaneous metastasis as an initial presentation of a non-functioning pancreatic neuroendocrine tumor. World J Gastroenterol 2015; 21(33): 9822-9826
- URL: https://www.wjgnet.com/1007-9327/full/v21/i33/9822.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i33.9822
Non-functioning pancreatic neuroendocrine tumors (NF-PNETs) are rare. Based on the data from the Surveillance, Epidemiology, and End Results (SEER) Program, NF-PNETs account for 2% of pancreatic malignancies. The annual worldwide incidence has been gradually increasing from 1.4 per million in 1973 to 3.0 per million in 2004[1]. Clinically, PNETs are classified as either functional or non-functional tumors[2]. While functioning PNETs might secrete several peptide hormones and cause paraneoplastic symptoms, NF-PNETs do not cause paraneoplastic symptoms and present as symptoms of mass effects, distant metastases, or both. Hence, NF-PNETs are often diagnosed as late secondary due to their vague symptoms and rarity. About 60% of NF-PNETs present distant metastases, which are usually hepatic[1,3,4]. Surgical therapy for NF-PNETs has improved survival outcome of patients with localized and metastatic carcinomas[1,5]. Cytoreductive surgery is recommended for patients with advanced disease/palliation, and is known to increase survival[6,7].
Cutaneous metastasis of NF-PNET is very rare. Notably, there have been no reports in which a patient has suffered from both primary and cutaneous metastatic lesions. Herein, we present a very rare case in which high grade NF-NET with cutaneous metastasis as the first manifestation was subjected to surgical resection.
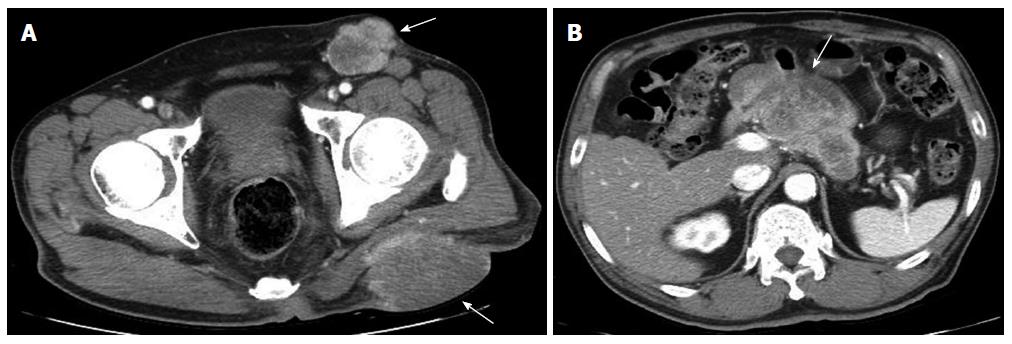
A 60-year-old male visited our outpatient clinic with a mass on his left hip. He had diabetes and alcoholic hepatitis. On physical examination, a large mass measuring 10 cm in diameter was observed on his hip and an approximate 5 cm left inguinal lymph node was palpable (Figure 1).
Serum tumor markers, including CEA and CA 19-9, were within normal limits, whereas serum amylase (227 IU/L, normal range 43-116 IU/L), lipase (378 IU/L, normal range 7-60), fasting blood sugar (144 mg/dL, normal range, 70-100 mg/dL), and liver function test levels [including aspartate aminotransferase (178 IU/L, normal range, 7-38 IU/L), alanine aminotransferase (225 IU/L; normal range, 4-43 IU/L), and serum alkaline phosphatase (370 IU/L, normal range, 103-335 IU/L)] were all above normal ranges.
An abdominal computerized tomography (CT) scan demonstrated not only a left hip mass and an enlarged left inguinal lymph node, but also a huge heterogeneous enhancing mass on the body of the pancreas (Figure 2). On a PET scan, additional metastases were not found.
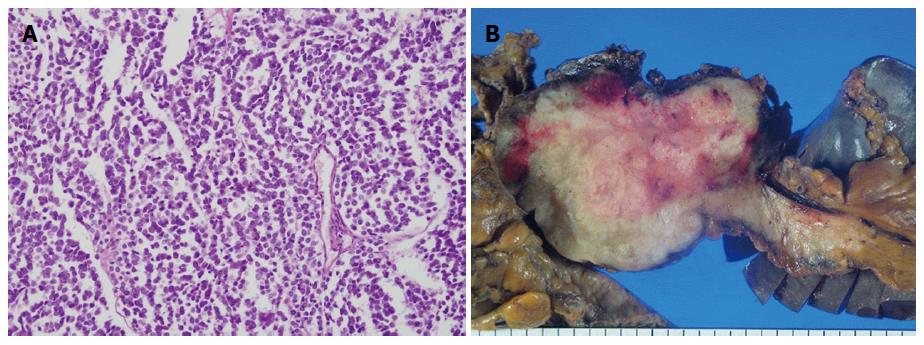
We planned a staged surgery and performed a hip and inguinal mass excision on December 19, 2014. The histopathological report revealed a metastatic small cell neuroendocrine carcinoma with a maximal diameter of 10.5 cm on the buttock mass and a 7 cm growth on an inguinal lymph node. The mitotic index was over 50 mitoses per 50 HPF and the Ki-67 index measured at 50%. On January 21, 2015, we performed a total pancreatectomy and a total gastrectomy, with the findings revealing a tumor of the body of the pancreas about 9 cm × 6 cm in diameter involving the left gastric artery, splenic artery, and splenic vein. The histopathological report was the same as that of a metastatic lesion. Additionally, the tumor had spread to 8 of the 32 lymph nodes (Figure 3).
On the 7th post-operative day, the patient developed a high fever and leukocytosis. We administered an abdominal CT scan, which revealed infected fluid collection in the lesser sac and a 4.7 cm-sized recurring mass which was detected at the operative bed of the left hip (Figure 4). After infection of the abdominal cavity was treated by antibiotics, we removed the left hip recurring mass on February 3, 2015. The histopathology was the same as in the previous report; with a maximum diameter of 7.5 cm. The patient was discharged without other complications on February 9, 2015. He is currently receiving chemotherapy based on etoposide and cisplatin treatment.
Cutaneous metastasis of pancreatic cancer is rare, with only 63 reported cases in the literature. Among these, adenocarcinoma was predominant (84.1%; 53/63) and the median survival of patients was 5 mo[8]. In the case of neuroendocrine tumors, 35 cases with cutaneous or subcutaneous metastases have been reported in the literature. Of these, cutaneous metastasis of PNET comprised only 2 cases[9]. One case developed into an umbilical metastasis 2 years after distal pancreatectomy for an islet cell tumor. The survival outcome of the 1st patient was not described[10]. The other patient had a scalp metastasis of a well-differentiated PNET and died 36 mo after a skin biopsy[9]. To our knowledge, our case is the third report of a cutaneous metastasis of PNET and the first of cutaneous metastasis of pancreatic neuroendocrine carcinoma (NEC).
It might be questionable as to whether surgical resection is beneficial in our patient. Based on SEER data, the prognostic factors of NF-PNETs were: resection of the primary tumor, low tumor grade, absence of distant metastases, and a younger age. In patients with distant metastases, the survival outcome of patients where both the primary and metastatic lesions were removed has been statistically better than in patients either undergoing resection of primary or metastatic sites or not undergoing resection. High grade tumors yield very dismal outcomes. The median survival time of low, intermediate, and high grade tumors are 5 years, 4.4 years, and 7 mo, respectively (P < 0.001)[1]. These tumor grade results were investigated regardless of primary and/or metastatic lesion resection. According to the European Neuroendocrine Tumor Society (ENETS) consensus guidelines, grade 3 metastatic NEC has an overall poor prognosis, regardless of whether or not they present with liver metastases[7]. ENETS suggested that resection of metastases of grade 3 NEC is generally not recommended, but may be considered in individual cases with isolated resectable metastases. It was also suggested that debulking resections with the removal of about 90% of the tumor volume can be exceptionally justified in a palliative situation[7].
Our case had a high grade of NF-PNET with distant and nodal metastases. As described, our case had recurrence within 1 mo. It took 46 d for the size of the recurrent mass to reach a 7.5 cm maximum size. The tumor grew very fast. Currently, the patient has survived for 4 mo after the 1st operation and has received 2 cycles of chemotherapy. A recent abdominal CT scan revealed an enlargement of the paraaortic lymph nodes (data not shown). Though he has undergone aggressive surgery, he has suffered from a Grade II complication of the Clavien-Dindo classification[11]. Some authors have reported that aggressive surgery could be done with acceptable morbidity and mortality rates for patients with advanced neuroendocrine tumors[12,13]. Hence, if it could be done safely, it seemed reasonable for this case of high-grade NF-PNET to be treated by aggressive surgical resection, despite the dismal prognosis.
In summary, we report the case of a patient who had a high grade NF-PNET with cutaneous metastasis and underwent surgical resection of both primary and metastatic tumors.
A 60-year-old man presented with a mass on his left hip.
On physical examination, a mass measuring 10 cm in diameter was observed on the patient’s hip and an approximately 5 cm left inguinal lymph node was palpable.
Differential diagnosis included pancreatic adenocarcinoma with cutaneous metastasis.
Serum CA 19-9 were within normal limits, whereas serum amylase (227 IU/L), lipase (378 IU/L), fasting blood sugar (144 mg/dL), and a liver function test levels [including aspartate aminotransferase (178 IU/L), alanine aminotransferase (225 IU/L), and serum alkaline phosphatase (370 IU/L)] were all above normal ranges.
An abdominal computerized tomography scan demonstrated not only a left hip mass and an enlarged left inguinal lymph node, but also a huge heterogeneous enhancing mass on the body of the pancreas.
The histopathological report revealed a metastatic small cell neuroendocrine carcinoma with 50% of the Ki-67 index.
The patient underwent staged surgery consisting of hip and inguinal masses excision, followed by a total pancreatectomy and a total gastrectomy.
A total of 2 cases of cutaneous metastasis of pancreatic neuroendocrine tumors (PNETs) have been reported in the literature. This is the third report of cutaneous metastasis of PNET and the first report of cutaneous metastasis of pancreatic neuroendocrine carcinoma.
Neuroendocrine tumors derived from the diffuse neuroendocrine system of the gastrointestinal tract and pancreas are fairly rare. They frequently have unpredictable and unusual biological behavior, and frequently present late after a delayed diagnosis.
This is the first known case report of grade 3 non-functioning PNET (NF-PNET) with cutaneous metastasis that was surgically removed. Although the patient quickly experienced recurrence, we think that if the lesions are almost totally removed, debulking resections can be justified.
NF-PNETs are rare and cutaneous metastases. This is interesting case with a described long-term patient outcome.
P- Reviewer: Chen YC S- Editor: Ma YJ L- Editor: Rutherford A E- Editor: Ma S
| 1. | Franko J, Feng W, Yip L, Genovese E, Moser AJ. Non-functional neuroendocrine carcinoma of the pancreas: incidence, tumor biology, and outcomes in 2,158 patients. J Gastrointest Surg. 2010;14:541-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 197] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 2. | Moo-Young TA, Prinz RA, Blumgart WRJH. Chapter 61 - Endocrine tumors of the pancreas: Clinical picture, diagnosis, and therapy. Blumgart’s Surgery of the Liver, Pancreas and Biliary Tract (Fifth Edition). Philadelphia: W.B. Saunders 2012; 934-944.e932. |
| 3. | Vagefi PA, Razo O, Deshpande V, McGrath DJ, Lauwers GY, Thayer SP, Warshaw AL, Fernández-Del Castillo C. Evolving patterns in the detection and outcomes of pancreatic neuroendocrine neoplasms: the Massachusetts General Hospital experience from 1977 to 2005. Arch Surg. 2007;142:347-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 165] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 4. | Hill JS, McPhee JT, McDade TP, Zhou Z, Sullivan ME, Whalen GF, Tseng JF. Pancreatic neuroendocrine tumors: the impact of surgical resection on survival. Cancer. 2009;115:741-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 234] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 5. | Dixon E, Pasieka JL. Functioning and nonfunctioning neuroendocrine tumors of the pancreas. Curr Opin Oncol. 2007;19:30-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Modlin IM, Oberg K, Chung DC, Jensen RT, de Herder WW, Thakker RV, Caplin M, Delle Fave G, Kaltsas GA, Krenning EP. Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol. 2008;9:61-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1268] [Cited by in RCA: 1183] [Article Influence: 69.6] [Reference Citation Analysis (0)] |
| 7. | Pavel M, Baudin E, Couvelard A, Krenning E, Öberg K, Steinmüller T, Anlauf M, Wiedenmann B, Salazar R; Barcelona Consensus Conference participants. ENETS Consensus Guidelines for the management of patients with liver and other distant metastases from neuroendocrine neoplasms of foregut, midgut, hindgut, and unknown primary. Neuroendocrinology. 2012;95:157-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 608] [Cited by in RCA: 595] [Article Influence: 45.8] [Reference Citation Analysis (0)] |
| 8. | Zhou HY, Wang XB, Gao F, Bu B, Zhang S, Wang Z. Cutaneous metastasis from pancreatic cancer: A case report and systematic review of the literature. Oncol Lett. 2014;8:2654-2660. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 9. | Jedrych J, Busam K, Klimstra DS, Pulitzer M. Cutaneous metastases as an initial manifestation of visceral well-differentiated neuroendocrine tumor: a report of four cases and a review of literature. J Cutan Pathol. 2014;41:113-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Zhang Y, Selvaggi SM. Metastatic islet cell carcinoma to the umbilicus: diagnosis by fine-needle aspiration. Diagn Cytopathol. 2003;29:91-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6210] [Cited by in RCA: 8637] [Article Influence: 539.8] [Reference Citation Analysis (0)] |
| 12. | Norton JA, Kivlen M, Li M, Schneider D, Chuter T, Jensen RT. Morbidity and mortality of aggressive resection in patients with advanced neuroendocrine tumors. Arch Surg. 2003;138:859-866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 152] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 13. | Phan GQ, Yeo CJ, Hruban RH, Lillemoe KD, Pitt HA, Cameron JL. Surgical experience with pancreatic and peripancreatic neuroendocrine tumors: review of 125 patients. J Gastrointest Surg. 1998;2:472-482. [PubMed] |