Published online Sep 7, 2015. doi: 10.3748/wjg.v21.i33.9817
Peer-review started: April 4, 2015
First decision: May 18, 2015
Revised: June 3, 2015
Accepted: July 8, 2015
Article in press: July 8, 2015
Published online: September 7, 2015
Processing time: 156 Days and 10 Hours
An appendiceal neurofibroma (ANF) is a rare neoplasm associated with neurofibromatosis type 1(NF-1), an inheritable neurocutaneous disorder that involves multiple systems including the intraabdominal organs. Appendiceal diverticulitis occasionally ruptures in the absence of intense abdominal pain, which can lead to serious consequences. Recent reports highlight the association between appendiceal diverticulum and appendiceal neoplasms; however, there is still little information on the association between appendiceal diverticulitis and ANF in NF-1. A 51-year-old Japanese male with NF-1 was referred to the division of surgery for mild right lower quadrant pain. It was suspected he had perforated acute appendicitis with periappendiceal abscess based on clinical manifestations and findings of computed tomography. An emergency appendectomy was conducted. The pathological examination revealed diffusely proliferated tumor cells of a neurofibroma, coexistent with multiple appendiceal diverticulums, leading to the diagnosis of perforated appendiceal diverticulitis associated with ANF. Although he developed a remnant abscess, he recovered with the conservative treatments of antibiotics and drainage. This case suggests that appendiceal diverticulitis might be a complication of appendiceal involvement of NF-1, and that it occasionally ruptures in the absence of intense abdominal pain. Clinicians should recognize that NF-1 can cause various abdominal manifestations.
Core tip: An appendiceal neurofibroma (ANF) is a rare neoplasm associated with neurofibromatosis type 1 (NF-1), an inheritable neurocutaneous disorder that involves multiple systems including the intraabdominal organs. Appendiceal diverticulitis occasionally ruptures in the absence of intense abdominal pain, which can lead to serious consequences. There is still little information on the association between appendiceal diverticulitis and ANF in NF-1. This patient presented with NF-1 and developed an ANF, complicated with appendiceal diverticulitis, which highlights the possible association of appendiceal diverticulitis and ANF in NF-1. This case could be used to enhance clinicians’ awareness of abdominal manifestations in NF-1.
- Citation: Ozaki A, Tsukada M, Watanabe K, Tsubokura M, Kato S, Tanimoto T, Kami M, Ohira H, Kanazawa Y. Perforated appendiceal diverticulitis associated with appendiceal neurofibroma in neurofibromatosis type 1. World J Gastroenterol 2015; 21(33): 9817-9821
- URL: https://www.wjgnet.com/1007-9327/full/v21/i33/9817.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i33.9817
Neurofibromatosis type 1 (NF-1) is one of the most common inheritable diseases[1]. It is a neurocutaneous disorder that possesses a high risk of multiple tumor formation[2]. It can involve intraabdominal organs as well as the nervous system and the skin[1,2].
An appendiceal neurofibroma (ANF) is a rare neoplasm associated with NF-1[3-6]. It typically presents with an appendicitis-like abdominal pain[3,4,7]. Imaging study shows an enlarged and diffusely thickened appendix[4-6]. Surgical resection is the standard treatment[4-8].
Appendiceal diverticulitis occasionally ruptures in the absence of an intense abdominal pain, and some patients develop serious consequences such as secondary peritonitis and abdominal abscesses[9-11]. In addition, it is more likely to rupture compared with acute appendicitis[9-11]. While an association between appendiceal diverticulum and appendiceal neoplasms has recently been reported[12,13], little is known about the association between appendiceal diverticulitis and ANF in NF-1. This report focuses on a patient with NF-1 who developed an ANF, complicated by appendiceal diverticulitis.
A fifty-one-year old Japanese male with NF-1 presented with mild right lower quadrant pain that lasted one week. He was diagnosed with NF-1 due to café-au-lait spots and cutaneous neurofibromas at age of twenty-five, thereafter his skin lesions gradually worsened.
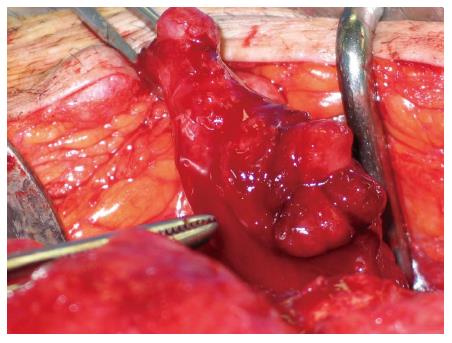
At the initial examination, he was afebrile, but there was localized rigidity with mild tenderness in the right lower quadrant. His white blood cell count was 13580/mL with 84% neutrophils. Serum levels of C-reactive protein were 7.26 mg/dL (normal value: < 0.3 mg/dL). An emergent abdominal computed tomography showed an inflamed and diffusely thickened appendix and abdominal abscess (Figure 1). Based on the clinical diagnosis of perforated acute appendicitis with periappendiceal abscess, an emergency laparotomy was conducted. A lower midline incision was performed to successfully drain the abdominal abscess. The appendix was thickened diffusely, perforated, and surrounded by a malodorous abscess (Figure 2). The appendix was successfully resected, and the abscess was drained. During the surgery, drainage tubes were placed in the rectovesical pouch and the abscess cavity, respectively. Drainage from the rectovesical pouch was serous, and the tube was removed six days after the surgery, when the amount of drainage decreased. However, even one week after the surgery, the drainage from the abscess cavity remained purulent, leading to the diagnosis of a remnant abscess. The patient received the conservative treatments of antibiotics and drainage, and the amount of the exudates via the tube gradually decreased. The tube was removed twenty-two days after the surgery. He was discharged twenty-three days after the surgery.
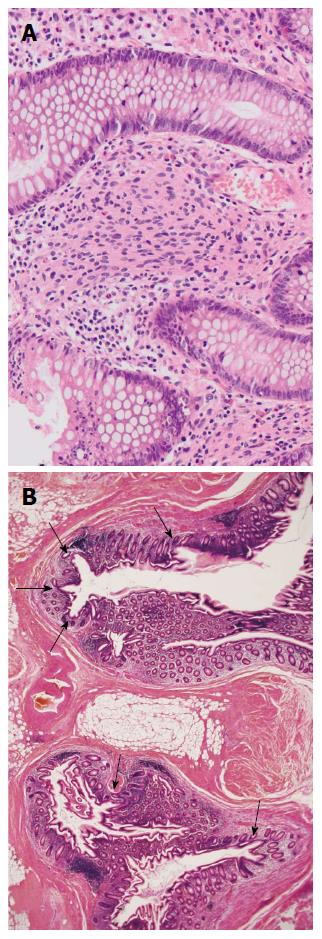
The resected appendix was thickened diffusely and stiffened. A pathological examination showed diffuse proliferation of the tumor cells of a neurofibroma (Figure 3A), coexisting with multiple diverticulums (Figure 3B). The majority of diverticulums were small in size, causing subtle epithelial herniation. The final diagnosis was perforated appendiceal diverticulitis associated with ANF.
This case suggests that appendiceal diverticulitis may be a complication of ANF in NF-1. We cannot deny the possibility of coincidental occurrence of the two diseases since little information is available concerning the association between appendiceal diverticulitis and ANF in NF-1. However, recent studies suggest that appendiceal diverticulum might be a complication of appendiceal neoplasms[12,13]. It is speculated that tumor cells proliferating in the appendiceal wall contribute to elevation of the intraluminal pressure by obstructing the appendicular root and/or by stiffening and thickening the appendiceal wall. This process is thought to lead to the development of appendiceal diverticulum and diverticulitis[12]. The present case was compatible with these reports, considering that the appendix including its root was diffusely thickened and stiffened as a result of diffuse proliferation of the tumor cells. Evidence of elevated intraluminal pressure was not apparent because the patient presented after the development of perforation. Furthermore, the status of NF-1 was progressive in the present case. A recent study has shown that gastrointestinal neurofibromas in NF-1, including an ANF, arise during midlife or after the development of skin lesions[1]. In the present case, the majority of appendiceal diverticulums were small in size, suggesting that they were in the early phase of development[13]. Thus, it is reasonable to assume that appendiceal diverticulums and ANF concurrently developed. These findings support the possible association between appendiceal diverticulitis and ANF in NF-1.
It is to be noted that the appendix ruptured in the absence of an intense abdominal pain. This finding is compatible with previous reports on appendiceal diverticulitis[9-11], while exact pathogenesis remains to be clarified. Appendiceal diverticulitis frequently presents with a mild right lower quadrant pain and more indolent clinical courses, compared with acute appendicitis[9,10]. However, it can easily rupture because the development of appendiceal diverticulum induces the epithelial herniation through the muscularis propria, which causes the thinning of appendiceal wall[10,11,14]. This case shows that perforation of the appendiceal diverticulum can cause a massive abdominal abscess. It is important to make an early diagnosis, and to initiate appropriate treatments promptly to avoid severe sequelae such as secondary peritonitis when patients with NF-1 develop appendiceal diverticulitis[9-11]. Visualization of the appendiceal diverticulum using abdominal ultrasonography might be useful in the preoperative diagnosis of appendiceal diverticulitis[11,15,16].
NF-1 can cause various abdominal manifestations. Abdominal neurofibromas can arise from the esophagus to the anorectum, and also in the associated peritoneal and mesenteric soft tissues[1]. Other than neurofibromas, gastrointestinal stromal tumors and neuroendocrine tumors may occur[17]. An early diagnosis is important, considering the risk of malignancy and complications, such as hemorrhage, obstruction, and perforation[17,18]. However, a recent report indicates abdominal manifestations of NF-1 rarely come into the mind of clinicians due to a lack of knowledge about their frequency and wide clinicopathological spectrum[1]. Awareness of abdominal manifestations holds great importance in the management of NF-1, as it has been shown that a considerable number of patients with NF-1 develop abdominal tumors[17].
In conclusion, this case suggests that appendiceal diverticulitis might be a complication of appendiceal involvement of NF-1, and that it occasionally ruptures even in the absence of intense abdominal pain. Clinicians should recognize that NF-1 can cause various abdominal manifestations.
A fifty-one-year old Japanese male with neurofibromatosis type 1 presented with mild right lower quadrant pain that lasted one week.
The patient was afebrile, but there was localized rigidity with mild tenderness in the right lower quadrant.
Based on the pathological findings, the diagnosis of appendiceal diverticulitis and appendiceal neurofibroma was made, although the clinical diagnosis was perforated acute appendicitis with periappendiceal abscess.
The patient had elevated hematological values for white blood cell count (13580/mL) with 84% neutrophils, and C-reactive protein (7.26 mg/dL).
An emergent abdominal computed tomography showed an inflamed and diffusely thickened appendix and abdominal abscess.
The pathological examination revealed diffusely proliferated tumor cells of a neurofibroma, coexistent with multiple appendiceal diverticulums.
An emergency appendectomy and the following conservative treatments of antibiotics and drainage were conducted.
An appendiceal neurofibroma is a rare neoplasm associated with neurofibromatosis type 1. Appendiceal diverticulitis occasionally ruptures in the absence of intense abdominal pain. Although recent reports highlight the association between appendiceal diverticulum and appendiceal neoplasms, there is still little information on the association between appendiceal diverticulitis and appendiceal neurofibroma in neurofibromatosis type 1.
An appendiceal neurofibroma is a rare neoplasm associated with neurofibromatosis type 1.
This case suggests that appendiceal diverticulitis might be a complication of appendiceal involvement of neurofibromatosis type 1, and that it occasionally ruptures in the absence of intense abdominal pain.
This report highlights the possible association of appendiceal diverticulitis and appendiceal neurofibroma in neurofibromatosis type 1. This case could be used to enhance clinicians’ awareness of abdominal manifestations in neurofibromatosis type 1, while whether this case is just rare in clinical settings or if this case represents other patients remains to be elucidated.
P- Reviewer: Glockzin G, Mayir B, Piccinni G, Ryu DH S- Editor: Ma YJ L- Editor: A E- Editor: Ma S
| 1. | Agaimy A, Vassos N, Croner RS. Gastrointestinal manifestations of neurofibromatosis type 1 (Recklinghausen’s disease): clinicopathological spectrum with pathogenetic considerations. Int J Clin Exp Pathol. 2012;5:852-862. [PubMed] |
| 2. | Ferner RE. Neurofibromatosis 1 and neurofibromatosis 2: a twenty first century perspective. Lancet Neurol. 2007;6:340-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 311] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 3. | Agaimy A, Märkl B, Kitz J, Wünsch PH, Arnholdt H, Füzesi L, Hartmann A, Chetty R. Peripheral nerve sheath tumors of the gastrointestinal tract: a multicenter study of 58 patients including NF1-associated gastric schwannoma and unusual morphologic variants. Virchows Arch. 2010;456:411-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 70] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 4. | Samuel I, Jakate S, Ramsey MM, Saclarides TJ. Abdominal mass in a 19-year-old with neurofibromatosis. Postgrad Med J. 1997;73:325-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Guo L, He K, Xu X, Li G, Li Z, Xia Y, Teng X, Teng L. Giant appendiceal neurofibroma in von Recklinghausen’s disease: A case report and literature review. Oncol Lett. 2014;8:1957-1960. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Lockhart ME, Smith JK, Canon CL, Morgan DE, Heslin MJ. Appendiceal ganglioneuromas and pheochromocytoma in neurofibromatosis type 1. AJR Am J Roentgenol. 2000;175:132-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Merck C, Kindblom LG. Neurofibromatosis of the appendix in von Recklinghausen’s disease. A report of a case. Acta Pathol Microbiol Scand A. 1975;83:623-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Rosenberg E, Sheiner E, Holcberg G. Neurofibromatosis type 1 and masses of the appendix: a case report. J Reprod Med. 2006;51:578-580. [PubMed] |
| 9. | Lobo-Machín I, Delgado-Plasencia L, Hernández-González I, Brito-García A, Burillo-Putze G, Bravo-Gutiérrez A, Martínez-Riera A, Medina-Arana V. Appendiceal diverticulitis and acute appendicitis: differences and similarities. Rev Esp Enferm Dig. 2014;106:452-458. [PubMed] |
| 11. | Yamana I, Kawamoto S, Inada K, Nagao S, Yoshida T, Yamashita Y. Clinical characteristics of 12 cases of appendiceal diverticulitis: a comparison with 378 cases of acute appendicitis. Surg Today. 2012;42:363-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Dupre MP, Jadavji I, Matshes E, Urbanski SJ. Diverticular disease of the vermiform appendix: a diagnostic clue to underlying appendiceal neoplasm. Hum Pathol. 2008;39:1823-1826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 13. | Kallenbach K, Hjorth SV, Engel U, Schlesinger NH, Holck S. Significance of acquired diverticular disease of the vermiform appendix: a marker of regional neoplasms? J Clin Pathol. 2012;65:638-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Rabinovitch J, Arlen M, Barnett T, Cuello R, Rabinovitch P. Diverticulosis and Diverticulitis of the Vermiform Appendix. Ann Surg. 1962;155:434-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Iki K, Echigo M, Nogami A, Iwamoto S, Takeo T, Tsunoda T, Eto T. Preoperative diagnosis of acute appendiceal diverticulitis by ultrasonography. Surgery. 2001;130:87-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Kubota T, Omori T, Yamamoto J, Nagai M, Tamaki S, Sasaki K. Sonographic findings of acute appendiceal diverticulitis. World J Gastroenterol. 2006;12:4104-4105. [PubMed] |