Published online Sep 7, 2015. doi: 10.3748/wjg.v21.i33.9758
Peer-review started: January 17, 2015
First decision: March 26, 2015
Revised: April 4, 2015
Accepted: April 28, 2015
Article in press: April 28, 2015
Published online: September 7, 2015
Processing time: 234 Days and 20.3 Hours
AIM: To evaluate the change in spectrum of gastric polyps in the Chinese population in the past ten years.
METHODS: A total of 157902 consecutive patients undergoing esophagogastroduodenoscopy (EGD) from 2004 to 2013 in a tertiary hospital were retrospectively reviewed using an EGD database. Endoscopic records of 4043 patients diagnosed with gastric polyps were recalled for analysis. Data including demographics, information on polyps such as location, pathological diagnosis, reflux esophagitis and Helicobacter pylori infection were obtained. We focused on epithelial polyps, especially hyperplastic polyps, fundic gland polyps and adenomas, and histological classification of specimens from biopsy and endoscopic polypectomy was performed by professional pathologists, based on the updated guidelines. To explore the age distribution of gastric polyps over time, we divided patients with polyps into four groups: A (aged < 30 years), B (aged 30-44 years), C (aged 45-59 years) and D (aged > 60 years). Differences in localization, age, and sex distribution of gastric polyps were analyzed by statistical software.
RESULTS: A total of 157902 EGD procedures were performed in ten years at our digestive endoscopy center, of which 4043 cases were diagnosed with gastric polyps confirmed by pathology. There were 2574 (63%) female and 1469 (37%) male patients with an average age of 54.7 years. The overall prevalence of gastric polyps was 2.6% (4043/157902). Our database demonstrated a rising prevalence of gastric polyps over the decade, increasing from 1.0% (80/8025) to 4.70% (828/17787) between 2004 and 2013. There has been a change in the spectrum of gastric polyps with the frequencies of FGPs increasing from 19% (15/80) to 77% (638/828) and hyperplastic polyps decreasing from 65% (52/80) to 15% (123/828). Moreover, data on 1921 polyps in 828 patients diagnosed with gastric polyps in 2013 showed that FGP was the most common type in the current polyp spectrum, making up 81.3% (1562/1921). Location and age distribution of gastric polyps have also altered. The prevalence of polyps located in the antrum decreased from 37.5% (30/80) to 9.30% (77/828), with an increasing prevalence of polyps in the corpus, from 45% (36/80) to 64.25% (532/828). The constituent ratio of older patients (aged > 60 years) in the polyp population decreased from 62.5% (50/80) to 32.13% (266/828), while that of patients aged 45-60 years showed an increased trend.
CONCLUSION: There was a shift change in the spectrum of gastric polyps in the Chinese population with altered location and age distribution in the past ten years.
Core tip: Recent studies have suggested that fundic gland polyps (FGPs) are the dominant type of gastric polyps rather than hyperplasic polyps. In the Chinese population, data on the spectrum of gastric polyps are limited, and the dynamic change in polyp spectrum has never been evaluated on a large scale. Hence, we retrospectively reviewed 4043 cases with gastric polyps from 157902 patients who underwent esophagogastroduodenoscopy in a tertiary hospital over a 10-year period. We observed a dynamic change in the spectrum of gastric polyps, which presented as a shift in which FGPs rather than hyperplastic polyps were the most common type, and the age, location and sex distribution of gastric polyps were also altered.
- Citation: Fan NN, Yang J, Sun G, Lu ZS, Ling Hu EQ, Wang XD, Yang YS. Changes in the spectrum of gastric polyps in the Chinese population. World J Gastroenterol 2015; 21(33): 9758-9764
- URL: https://www.wjgnet.com/1007-9327/full/v21/i33/9758.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i33.9758
Polyps are defined as protuberant lesions into the lumen originating in the epithelium or submucosa, which are characterized as sessile or pedunculated, sporadic, or part of a syndrome[1]. Gastric polyps are usual finding under endoscopic exam and most patients are asymptomatic. However, larger gastric polyps may result in some symptoms, such as bleeding, anemia, abdominal pain, and even gastric outlet obstruction[2-4]. Widespread use of endoscopic examinations contributes to improving the detected rate of gastric polyps. Endoscopic features of some polyps may be useful for diagnosis, yet not every polypoid lesion can be defined as a polyp unless histopathologically confirmed[5]. Based on histological features, gastric polyps are classified into two groups: neoplastic and non-neoplastic polyps with several subtypes[6]. Most gastric polyps are non-neoplastic, which is different to colorectal polyps.
Hyperplastic polyps (HPPs) used to be the most common polyps[7,8], with a relative prevalence of approximately 70%[1]. However, results from recent studies indicate that the prevalence of fundic gland polyps (FGPs) has increased greatly in recent decades. The reasons for this change remain unclear. Some previous studies have suggested several circumstances that may result in a spectrum change of gastric polyps[5], which include expanded indications for esophagogastroduodenoscopy (EGD), long-term use of proton pump inhibitors (PPIs), decreasing Helicobacter pylori (H. pylori) infection, and enhanced health consciousness in the general population. FGPs are reported as the most common type of polyps detected at EGD in the United States[9]. Although a similar spectrum of gastric polyps is also reported in the Northern Chinese population[10], few Chinese population-based data exist. Data on the spectrum and distribution patterns of gastric polyps in the Chinese patient population are limited, particularly for the dynamic observation of the spectrum of gastric polyps.
In view of this, we evaluated the spectrum of gastric polyps in the Chinese population by reviewing a 10-year consecutive EGD database. We also hypothesized that location, age and sex distribution of gastric polyps may have changed with the altered spectrum of polyps over the past 10 years.
This study was conducted at the Digestive Endoscopy Center of Chinese PLA General Hospital, which is a large hospital integrating medical services, education and research. All patients undergoing EGD in our center from January 1, 2004 to December 31, 2013 were analyzed retrospectively. All patients gave signed informed consent for EGD before the procedure. Specimens from biopsy and endoscopic polypectomy were interpreted by a professional group of pathologists. Gastric polyps of epithelial origin were included, while hamartomatous polyps, polyposis syndromes and non-mucosal intramural polyps were excluded. In particular, the study population excluded patients with esophageal, gastric or esophagogastric varices who underwent EGD, intended mainly for treatment with endoscopic cyanoacrylate injection, sclerotherapy or endoscopic variceal ligation, which is a characteristic endoscopy technique performed in our department.
Information on patients and polyps were obtained from endoscopy reports, which included age, sex, and location of gastric polyps, and histological diagnosis. Histological classification was carried out according to an updated classification suggested in the 2010 guidelines of the British Society of Gastroenterology (BSG)[11]. Gastric polyps of epithelial origin mainly include HPPs, FGPs, and adenomas. We focused on epithelial polyps, especially HPPs, FGPs and adenomas, which are classic gastric polyps. Infection with H. pylori was diagnosed by histology.
All statistical calculations were performed with SPSS version 15.0. Mean and standard deviation (SD) were used to describe continuous variables, while percentages were used for discrete variables. The significance of possible associations between discrete variables was assessed by the Pearson χ2 test.
We performed a total of 157902 EGD procedures over the 10-year review period. The study population comprised patients referred for various indications. Among these, 4043 (2.60%) cases were diagnosed with gastric polyps by pathology. The average age and sex distribution of patients with gastric polyps are shown in Table 1. There were 2574 (63%) female and 1469 (37%) male patients, with a mean age of 54.7 years (range: 8-92 years). Either FGP or HPP was significantly more frequent in women with a sex ratio of 1.39:1 and 1.32:1, respectively. However, only adenomas were predominant in men, with a male-to-female ratio of 3.69:1.0.
| GP | FGP | HPP | Adenomas | |
| Age (yr) | 54.7 ± 12.9 | 53.9 ± 12.6 | 55.2 ± 13.3 | 66.4 ± 10.1 |
| (mean ± SD) | ||||
| Gender (F/M) | 2574:1469 | 1190:857 | 580:439 | 16:59 |
| (1.75:1) | (1.39:1) | (1.32:1) | (1:3.69) | |
| Helicobacter pylori infection rate | 186/4043 | 82/2047 | 59/1019 | 1/75 |
| (4.60) | (4.0) | (5.79) | (1.33) | |
| Reflux esophagitis incidence | 356/4043 | 219/2047 | 39/1019 | - |
| (8.81) | (10.70) | (3.83) | ||
| Dysplasia | 68/4043 (1.68) | 3/2047 (0.15) | 14/2047 (0.68) | 45/75 (60) |
| HIN | 25/4043 (0.62) | - | - | 23/75 (31) |
The incidence of H. pylori infection in patients with gastric polyps diagnosed by pathology was 4.60% (186/4043). Among 1019 patients with HPPs, 59 (5.79%) patients were pathologically confirmed to have H. pylori infection, which was significantly more common than that in the FGP (4.0%) and adenoma (1.33%) groups (P = 0.005). 293 (10.70%) patients with FGPs were diagnosed with reflux esophagitis (RE), which was higher than those without FGPs, yet there was no difference in the various types of gastric polyps. Information on dysplasia in FGPs, HPPs and adenomas was recorded, in terms of the malignant potential of different types of polyps causing differing consequences for patients. Dysplasia occurred in various types of gastric polyps. Notably, dyspepsia was detected in 45 of 75 patients with adenomas, and high-grade intraepithelial neoplasia was confirmed in 23 cases, which was significantly higher than for other types of gastric polyps (60% vs 8.81%, P < 0.001; 60% vs 0.15%, P = 0.0000; 60% vs 0.68%, P = 0.0000).
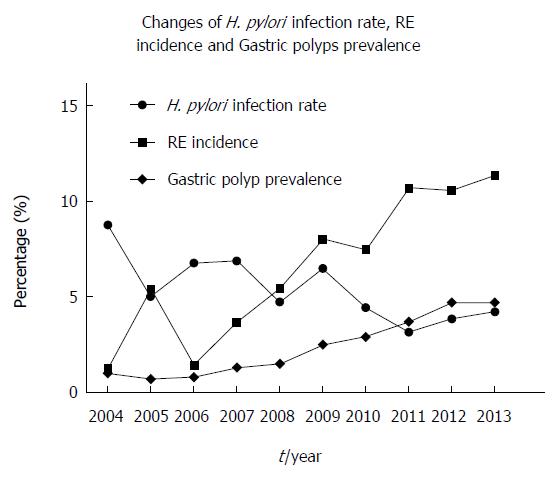
To explore the dynamic changes in age and sex distribution of gastric polyps, we also analyzed data on gastric polyp yield from EGD from 2004 to 2013 (Table 2). The average age of patients with polyps (54.7 years) was higher than the entire patient population (51.4 years). The average age of patients with gastric polyps showed a decreasing trend, from 59.6 years in 2004 to 54.7 years in 2013. A female predominance in the polyp population was present, with the highest sex ratio of 2.12:1.0. Moreover, the incidence of H. pylori in the polyp population decreased significantly from 8.75% (7/80) to 4.23% (35/828) (P = 0.2057), while the prevalence of reflux esophagitis rose from 1.25% (1/80) to 11.35% (94/828) (P = 0.0048).
| Year | Cases | Age (yr) | Gender (M/F) | Prevalence |
| (mean ± SD) | ||||
| 2004 | 80 | 59.6 ± 14.7 | 48:32 (1.5:1) | 80/8025 (1.0) |
| 2005 | 74 | 57.5 ± 11.4 | 34:40 (1:1.18) | 74/10739 (0.7) |
| 2006 | 140 | 55.6 ± 10.7 | 57:83 (1:1.46) | 140/13814 (0.8) |
| 2007 | 218 | 52.7 ± 11.3 | 93:125 (1:1.34) | 218/17372 (1.3) |
| 2008 | 275 | 53.3 ± 10.7 | 105:160 (1:1.52) | 275/17941 (1.5) |
| 2009 | 462 | 54.8 ± 13.1 | 171:291 (1:1.70) | 462/18364 (2.5) |
| 2010 | 496 | 54.7 ± 12.8 | 183:313 (1:1.71) | 496/17125 (2.9) |
| 2011 | 664 | 54.5 ± 12.5 | 223:441 (1:1.98) | 664/17893 (3.7) |
| 2012 | 806 | 54.8 ± 12.9 | 284:522 (1:1.83) | 806/18842 (4.7) |
| 2013 | 828 | 54.6 ± 12.1 | 271:575 (1:2.12) | 828/17787 (4.7) |
| Total | 4043 | 54.7 ± 12.9 | 1469:2574 (1:1.75) | 4043/157902 (2.6) |
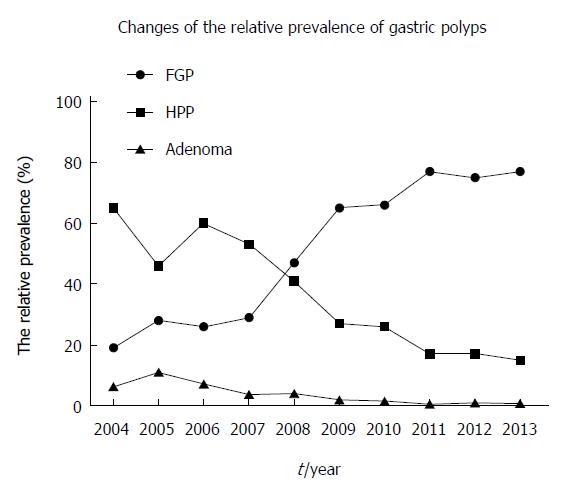
Among the 4043 cases with documented true polyps (both endoscopically and histologically identified), 2647 cases were diagnosed with FGPs, followed by HPPs (1019 cases), with adenomas detected only in 75 cases, and the remaining 302 cases were diagnosed with other types of gastric epithelial polyps, including polyps that could not be classified into definite types. The relative prevalence of FGPs, HPs and adenomas in this decade are described in Figure 1. The overall prevalence of FGPs, HPs and adenomas was 65% (2647/4043), 25% (1019/4043) and 1.9% (75/4043), respectively. There was an increase in the prevalence of gastric polyps on EGD in the past 10 years, which rose from 1.0% (80/8025) to 77% (638/828) (P = 0.0000) (Figure 2). FGP has become the most common type of gastric polyp rather than HPP. Figure 1 indicates that the relative frequencies of FGPs and HPs have also altered, increasing from 19% (15/80) to 77% (638/828) (P = 0.0000) for FGPs, and decreasing from 65% (52/80) to 15% (123/828) for HPPs (P = 0.0000). In order to re-evaluate the current spectrum of gastric polyps, we analyzed 1921 gastric polyps from 828 patients in 2013, of which 1561 were FGPs, 213 HPs, and 6 adenomas. FGP was confirmed as the most common type in the current polyp spectrum, comprising up to 81.30% (1562/1921).
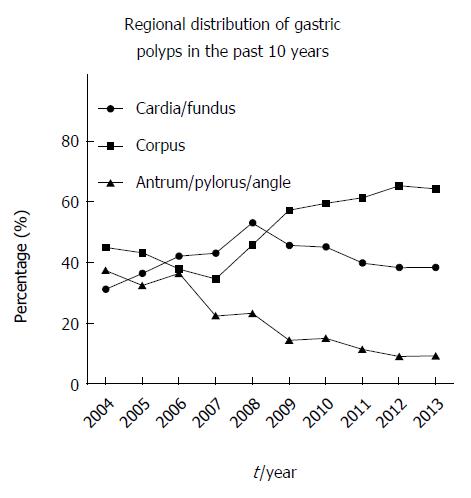
Moreover, we analyzed the regional distribution of gastric polyps over the past ten years. In our patient population, most gastric polyps were detected in the corpus and fundus (Figure 3). There was a progressive shift toward the corpus in the regional distribution of gastric polyps (45% vs 64.25%, P = 0.0007).
We divided patients with gastric polyps into four groups according to their age: Group A (aged < 30 years), Group B (aged 30-44 years), Group C (aged 45-59 years), and Group D (aged > 60 years). Overall, of 4043 cases, 1395 (34.5%) were aged > 60 years, with 17.29% and 44.99% in the younger age Groups B and C, respectively. Altered age distribution of gastric polyps was observed (Table 3). Patients aged 45-59 years comprised nearly half (44.99%) of the entire polyp population in 2013, while patients aged > 60 years were predominant in the polyp population before 2006 (41.43% vs 32.13%, P = 0.031). Gastric polyps were rarely detected in patients aged < 30 years, comprising only 3.22 % of patients with gastric polyps.
| Year | Group A | Group B | Group C | Group D |
| 2004 | 3/80 (3.8) | 10/80 (12.5) | 17/80 (21.25) | 50/80 (62.5) |
| 2005 | 1/74 (1.35) | 13/74 (17.57) | 24/74 (32.43) | 36/74 (48.65) |
| 2006 | 5/140 (3.57) | 22/140 (15.71) | 55/140 (39.29) | 58/140 (41.43) |
| 2007 | 12/218 (5.5) | 51/218 (23.4) | 88/218 (40.37) | 67/218 (30.73) |
| 2008 | 14/275 (5.09) | 54/275 (19.26) | 121/275 (44) | 86/275 (31.27) |
| 2009 | 13/462 (2.81) | 89/462 (18.75) | 195/462 (42.21) | 165/462 (35.71) |
| 2010 | 10/496 (2.02) | 93/496 (19.64) | 229/496 (46.17) | 164/496 (33.06) |
| 2011 | 22/664 (3.31) | 97/664 (14.61) | 329/664 (49.55) | 216/664 (32.53) |
| 2012 | 28/806 (3.47) | 131/806 (16.25) | 360/806 (44.67) | 287/806 (35.61) |
| 2013 | 22/828 (2.66) | 139/828 (16.69) | 401/828 (48.43) | 266/828 (32.13) |
| Total | 130/4043 (3.22) | 699/4043 (17.29) | 1819/4043(44.99) | 1395/4043 (34.5) |
We reviewed some of the characteristics of gastric polyps in 4043 patients recorded in an EGD database in a tertiary hospital over a 10-year period, which provided the first large-scale consecutive data on gastric polyps in the Chinese population in the past ten years. This is also the first report on the prevalence, location and sex distribution of gastric polyps in the Chinese population. The prevalence of gastric polyps on EGD ranges between 3.00% and 6.35%[5,12], which varies widely among published series, and correlates closely with the patient population[13]. In the present population, there was a gradual increase in the prevalence of gastric polyps in this decade, with the overall prevalence of 2.60% and 4.7% in 2013, respectively. Our data demonstrate the change in the spectrum of gastric polyps in China, with altered location and sex distribution. FGPs rather than HPPs are now the most common type of gastric polyps. Furthermore, there was an increasing age-specific prevalence of polyps in patients aged 45-59 years in this decade. We also confirmed a progressive shift towards the corpus in the regional distribution of gastric polyps. Gastric polyps occurred most frequently in the corpus of female patients aged 45-60 years, while adenomas were more frequent in the antrum of male patients aged > 60 years.
We compared our data with those from previous studies in China and other countries[1,5,10,14-17] (Table 4). The most significant difference in these studies of different populations was the relative proportion of FGPs. These differences may have been due to different populations, study design and methods, and time of study. Our data show a similar spectrum of polyps to that seen in a previous study in the Northern Chinese population[10] and in the USA[5]. In particular, the relative proportion of FGPs in the present study was consistent with that in the US study, which was up to 77% of gastric polyps. Our ten-year consecutive data on the relative proportion of FGPs suggest that FGPs have become the most predominant type since 2008. Moreover, the studies from the USA and China conducted after 2008 showed a similar spectrum of polyps. This phenomenon is believed not to be coincidental, and supports the notion that there has been a change in the spectrum of gastric polyps in western countries and China, and needs to be confirmed by more data from other countries.
| Ref. | Country | Pub. year | Years | Prevalence of polyps | No. of polyps | Median age (yr) | Gender(F/M) | FGP | HPP | Adenoma |
| Deppisch et al[7] | United States | 1989 | 10 | - | 121 | - | - | 17% | 75% | 8.6% |
| Stolte et al[12] | Germany | 1994 | 20 | - | 5515 | NR | NR | 47% | 28.3% | 9% |
| Sivelli et al[13] | Italy | 2002 | 6 | 164 | 61.4 | 01:01.5 | NR | 44.5% | 16.4% | |
| Gencosmanoglu et al[14] | Turkey | 2003 | 5 | - | 150 | 53 | 1.4:1 | 14% | 64% | 3% |
| Morais et al[1] | Brazil | 2007 | 5 | 153/26000 (0.59%) | 153 | 64 | 01:01.4 | 16.3% | 71.3% | 12.4% |
| Carmack et al[5] | United States | 2009 | 1 | 7877/121564 (6.35%) | 7877 | 56 | 1.4:1 | 77% | 17% | 0.7% |
| Cao et al[10] | China | 2000 | 1 | 68/6784 (1.0%) | 68 | 56.8 | 1.7:1 | 8.8% | 48.5% | 14.7% |
| Cao et al[10] | China | 2010 | 1 | 183/17337 (1.0%) | 183 | 55.9 | 2.0:1 | 66.1% | 20.8% | 4.9% |
| The present study | China | 2004-2013 | 10 | 183/157902 (2.60%) | 4043 | 54.7 | 1.75: 1 | 65% | 25% | 1.9% |
| The present study | China | 2013 | 1 | 828/17787 (4.7%) | 828 | 54.6 | 2.12:1 | 75% | 17% | 0.5% |
| Sonnenberg et al[17] | United States | 2015 | 1 | 71575 /927137 (7.72%) | 71575 | - | 2.03:1 | 79.9% | 18.6% | 0.92% |
In the present study, the polyp spectrum changed, with an increasing prevalence of FGPs. Several factors may explain this change. Although the relationship between PPI intake and FGP development remains controversial[18-22], a series of studies support the role of long-term PPI intake in the genesis of FGPs[21,23,24]. The increased incidence of gastroesophageal reflux disease and socioeconomic development in China has resulted in more individuals taking PPIs, and an increase in PPI-related FGPs. Our data indicated that there were significant differences in the incidence of reflux esophagitis under endoscopy in patients with FGPs compared with gastric polyps overall and those with HPPs. It is notable that the incidence of reflux esophagitis in patients with gastric polyps overall showed an increasing annual trend, which coincided with the increased detection rate of FGPs. This finding suggests a positive association between FGPs and reflux esophagitis, given that patients with reflux esophagitis tend to use PPIs for prolonged periods, while the latter (PPIs) has been associated with FGPs in a series of studies[24,25]. In the latest study performed in the USA, reflux disease was also reported to be significantly more common in patients with fundic gland polyps[17]. Thus, our data may indirectly support a possible correlation between PPIs and FGPs. However, we could not obtain information on the use of PPIs in this retrospective study, and our observations could not demonstrate a clear correlation between PPIs or reflux esophagitis and FGPs. Hence, further investigations are needed to determine the role of PPIs in the genesis of sporadic FGPs. The decrease in H. pylori infection may be another important factor, which is reported to be negatively associated with HPPs[26-29]. Most gastric HPPs disappear after eradication of H. pylori, therefore the decrease in infection may have led to a decrease in the prevalence of HPPs, which was confirmed in our study.
Few previous studies have addressed the prevalence of gastric polyps in different age groups. We demonstrated altered location and age distribution of gastric polyps over the past decade in the present study. Advances in digestive endoscopy techniques and enhanced health awareness have extended the indications for EGD. As a result, EGD has been performed in younger individuals, and gastric polyps have been detected at an early age. HPPs were most common in the antrum[30], while FGPs were most common in the fundus and upper corpus[31], thus the regional distribution of gastric polyps has changed with the spectrum. Our data demonstrate that adenomas are most common in elderly male patients, and have a high malignant potential with dysplasia occurring in 60% of cases, indicating that endoscopists should be aware of the presence of adenomas with high malignant potential in that population.
The present study was conducted in a tertiary hospital center over a long period of time, with large numbers of patients from different geographic areas in China, ensuring satisfactory representation of the entire nation in the results. However, this was a retrospective study and not a population-based screening study, therefore, when interpreting these data some factors should be taken into consideration. First, it was not a screening study based on an asymptomatic population undergoing EGD, and the study population comprised patients referred for various indications, and not all patients diagnosed with polyps or polypoid lesions by endoscopy accepted biopsy, thus the prevalence of polyps addressed in our study does not represent the true incidence in the entire population. Second, during the 10-year period, the guidelines for EGD and therapeutic trends have been updated. The biases of the population studied including socioeconomic, demographic and genetic characteristics should also be considered when comparing data from this study with previous studies. Lastly, H. pylori infection was diagnosed by pathology, which has a low sensitivity, resulting in a lower incidence of infection than the true situation.
In summary, the detection rate of gastric polyps in the Chinese population has gradually increased with widespread use of EGD in the recent decade. The spectrum of gastric polyps has changed, with FGPs rather than HPPs as the most common type of polyp. Widespread use of PPIs and decreased H. pylori infection may explain this change. Location and age distribution of gastric polyps have also been altered with the changed spectrum, where an increased number of polyps were detected in the corpus and a decreased proportion of patients aged > 60 years had polyps. These findings may allow us to explore the underlying factors associated with gastric polyps, and provide better endoscopic surveillance for the general population, especially in patients with gastric polyps.
Gastric polyps are the most common positive finding in gastroendoscopic procedures. The prevalence of gastric polyps varies widely among published studies, and correlates closely with the patient population. An altered spectrum of gastric polyps in the Western population has been reported, yet data from the Chinese population are limited.
Hyperplasic polyps were the most common type of gastric polyps. However, recent studies suggest a shift towards fundic gland polyps, which may be associated with several circumstances such as widespread use and expanded indications for endoscopic examinations, increased incidence of gastroesophageal reflux disease, and frequent intake of proton pump inhibitors.
The present study provides the first large-scale consecutive data on gastric polyps in the Chinese population over a 10-year period. It also provides information on the prevalence, location and sex distribution of gastric polyps in the Chinese population.
Evaluation of the dynamic change in the spectrum, location and age distribution of gastric polyps can help determine the underlying factors associated with gastric polyps, and provide better endoscopic surveillance for the general population, especially patients with gastric polyps.
Polyps are defined as protuberant lesions into the lumen originating in the epithelium or submucosa, which are characterized as sessile or pedunculated, sporadic, or part of a syndrome. Gastric polyps can be classified into various types, and hyperplastic polyps, fundic gland polyps and adenomas are common.
This is one of the largest series of the last years, providing a clear picture of epidemiology of gastric polyps in China, and underlines the correlation between type of polyps, location, age and associated pathologies. Moreover, a dynamic change in spectrum of gastric polyps is described. However, an obvious limitation is the retrospectivity of the present study, and further prospective studies should be encouraged.
P- Reviewer: Arolfo S, De Lisi S S- Editor: Yu J L- Editor: Webster JR E- Editor: Liu XM
| 1. | Morais DJ, Yamanaka A, Zeitune JM, Andreollo NA. Gastric polyps: a retrospective analysis of 26,000 digestive endoscopies. Arq Gastroenterol. 2007;44:14-17. [PubMed] |
| 2. | Nayudu SK, Niazi M, Balar B, Kumbum K. A rare complication of hyperplastic gastric polyp. Case Rep Gastrointest Med. 2013;2013:631975. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | He HY, Shen ZB, Fang Y, Sun YH, Qin XY. Bleeding and hyperpyrexia in an adult with gastric inflammatory fibroid polyp. Chin Med J (Engl). 2013;126:2594. [PubMed] |
| 4. | Vlacancich R, Sultan M, Al-Kawas F. Gastric outlet obstruction caused by prolapsed gastric polyp into the pyloric channel. Clin Gastroenterol Hepatol. 2014;12:A27-A28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Carmack SW, Genta RM, Schuler CM, Saboorian MH. The current spectrum of gastric polyps: a 1-year national study of over 120,000 patients. Am J Gastroenterol. 2009;104:1524-1532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 199] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 6. | Fock KM, Ang TL. Epidemiology of Helicobacter pylori infection and gastric cancer in Asia. J Gastroenterol Hepatol. 2010;25:479-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 216] [Article Influence: 14.4] [Reference Citation Analysis (1)] |
| 7. | Deppisch LM, Rona VT. Gastric epithelial polyps. A 10-year study. J Clin Gastroenterol. 1989;11:110-115. [PubMed] |
| 8. | Roseau G, Ducreux M, Molas G, Ponsot P, Amouyal P, Palazzo L, Amouyal G, Paolaggi JA. [Epithelial gastric polyps in a series of 13000 gastroscopies]. Presse Med. 1990;19:650-654. [PubMed] |
| 9. | Shaib YH, Rugge M, Graham DY, Genta RM. Management of gastric polyps: an endoscopy-based approach. Clin Gastroenterol Hepatol. 2013;11:1374-1384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 75] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 10. | Cao H, Wang B, Zhang Z, Zhang H, Qu R. Distribution trends of gastric polyps: an endoscopy database analysis of 24 121 northern Chinese patients. J Gastroenterol Hepatol. 2012;27:1175-1180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 56] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 11. | Goddard AF, Badreldin R, Pritchard DM, Walker MM, Warren B. The management of gastric polyps. Gut. 2010;59:1270-1276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 144] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 12. | Stolte M, Sticht T, Eidt S, Ebert D, Finkenzeller G. Frequency, location, and age and sex distribution of various types of gastric polyp. Endoscopy. 1994;26:659-665. [PubMed] |
| 13. | Sivelli R, Del Rio P, Bonati L, Sianesi M. [Gastric polyps: a clinical contribution]. Chir Ital. 2002;54:37-40. [PubMed] |
| 14. | Gencosmanoglu R, Sen-Oran E, Kurtkaya-Yapicier O, Avsar E, Sav A, Tozun N. Gastric polypoid lesions: analysis of 150 endoscopic polypectomy specimens from 91 patients. World J Gastroenterol. 2003;9:2236-2239. [PubMed] |
| 15. | Kelly PJ, Lauwers GY. Clinical guidelines: Consensus for the management of patients with gastric polyps. Nat Rev Gastroenterol Hepatol. 2011;8:7-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Islam RS, Patel NC, Lam-Himlin D, Nguyen CC. Gastric polyps: a review of clinical, endoscopic, and histopathologic features and management decisions. Gastroenterol Hepatol (N Y). 2013;9:640-651. [PubMed] |
| 17. | Sonnenberg A, Genta RM. Prevalence of benign gastric polyps in a large pathology database. Dig Liver Dis. 2015;47:164-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 18. | Matsuzaki J, Suzuki H, Minegishi Y, Sugai E, Tsugawa H, Yasui M, Hibi T. Acid suppression by proton pump inhibitors enhances aquaporin-4 and KCNQ1 expression in gastric fundic parietal cells in mouse. Dig Dis Sci. 2010;55:3339-3348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Thomson AB, Sauve MD, Kassam N, Kamitakahara H. Safety of the long-term use of proton pump inhibitors. World J Gastroenterol. 2010;16:2323-2330. [PubMed] |
| 20. | Fernández JL, Viola LA. Reply: Is there any association between proton pump inhibitors and fundic gland polyps? Rev Esp Enferm Dig. 2012;104:45-47; author reply 48. [PubMed] |
| 21. | Declich P, Belloni J, Tavani E, Omazzi B, Bortoli A, Devani M, Arena I, Bellone S, Saibeni S, Prada A. Fundic gland polyps and proton pump inhibitors: an obvious link, or an open question? Hum Pathol. 2014;45:1122-1123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Cao H, Qu R, Zhang Z, Kong X, Wang S, Jiang K, Wang B. Sporadic fundic gland polyps are not associated with proton pump inhibitors therapy but negatively correlate with Helicobacter pylori infection in China. Chin Med J (Engl). 2014;127:1239-1243. [PubMed] |
| 23. | el-Zimaity HM, Jackson FW, Graham DY. Fundic gland polyps developing during omeprazole therapy. Am J Gastroenterol. 1997;92:1858-1860. [PubMed] |
| 24. | Jalving M, Koornstra JJ, Wesseling J, Boezen HM, DE Jong S, Kleibeuker JH. Increased risk of fundic gland polyps during long-term proton pump inhibitor therapy. Aliment Pharmacol Ther. 2006;24:1341-1348. [PubMed] |
| 25. | Freeman HJ. Proton pump inhibitors and an emerging epidemic of gastric fundic gland polyposis. World J Gastroenterol. 2008;14:1318-1320. [PubMed] |
| 26. | Dirschmid K, Platz-Baudin C, Stolte M. Why is the hyperplastic polyp a marker for the precancerous condition of the gastric mucosa? Virchows Arch. 2006;448:80-84. [PubMed] |
| 27. | Ljubicić N, Banić M, Kujundzić M, Antić Z, Vrkljan M, Kovacević I, Hrabar D, Doko M, Zovak M, Mihatov S. The effect of eradicating Helicobacter pylori infection on the course of adenomatous and hyperplastic gastric polyps. Eur J Gastroenterol Hepatol. 1999;11:727-730. [PubMed] |
| 28. | Ohkusa T, Takashimizu I, Fujiki K, Suzuki S, Shimoi K, Horiuchi T, Sakurazawa T, Ariake K, Ishii K, Kumagai J. Disappearance of hyperplastic polyps in the stomach after eradication of Helicobacter pylori. A randomized, clinical trial. Ann Intern Med. 1998;129:712-715. [PubMed] |
| 29. | Tokunaga K, Tanaka A, Takahashi S. [Gastric hyperplastic polyps and H. pylori infection, their relationship and effects of eradication therapy]. Nihon Rinsho. 2013;71:1449-1452. [PubMed] |
| 30. | Stolte M. Hyperplastic polyps of the stomach: associations with histologic patterns of gastritis and gastric atrophy. Am J Surg Pathol. 2001;25:1342-1344. [PubMed] |
| 31. | Carmack SW, Genta RM, Graham DY, Lauwers GY. Management of gastric polyps: a pathology-based guide for gastroenterologists. Nat Rev Gastroenterol Hepatol. 2009;6:331-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 97] [Article Influence: 6.1] [Reference Citation Analysis (1)] |