Published online Aug 21, 2015. doi: 10.3748/wjg.v21.i31.9437
Peer-review started: May 12, 2014
First decision: June 10, 2014
Revised: July 8, 2014
Accepted: August 28, 2014
Article in press: August 28, 2014
Published online: August 21, 2015
Processing time: 466 Days and 4.9 Hours
Primary adenocarcinoma of the small intestine occurs in over 50% of cases in the duodenum. However, its location in the third and fourth duodenal portions occurs rarely and is a diagnostic challenge. The aim of this work is to report an adenocarcinoma of the third and fourth duodenal portions, emphasizing its diagnostic difficulty and the value of video capsule endoscopy. A man, 40 years old, with no medical history, with abdominal discomfort and progressive fatigue, presented four months ago with one episode of moderate melena. The physical examination was normal, except for mucosal pallor. Blood tests were consistent with microcytic, hypochromic iron deficiency anemia with 7.8 g/dL hemoglobin. The upper and lower endoscopy were normal. Additional work-up with video capsule endoscopy showed a polypoid lesion involving the third and fourth portions of the duodenum. Biopsy showed a moderately differentiated adenocarcinoma. Abdominal computed tomography showed a wall thickening from the third duodenal portion to the proximal jejunum, without distant metastasis. The patient underwent segmental resection (distal duodenum and proximal jejunum) with duodenojejunostomy. The surgical specimen histology confirmed the biopsy diagnosis, with transmural infiltration, without nodal involvement. Conclusion: Adenocarcinoma of the third and fourth portions of the duodenum is difficult to diagnose and capsule endoscopy is of great value.
Core tip: Third and/or fourth duodenal portion adenocarcinoma is a rare disease, associated with a vague clinical picture and a diagnostic challenge. Capsule endoscopy has shown a higher accuracy compared to conventional endoscopic methods. This case reports the occurrence of adenocarcinoma of the third and fourth duodenal portions and the value of capsule endoscopy to minimize the diagnostic difficulty.
- Citation: Paquissi FC, Lima AHFBP, Lopes MFDNV, Diaz FV. Adenocarcinoma of the third and fourth portions of the duodenum: The capsule endoscopy value. World J Gastroenterol 2015; 21(31): 9437-9441
- URL: https://www.wjgnet.com/1007-9327/full/v21/i31/9437.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i31.9437
The small intestine is approximately 75% of the length and 90% of the mucosal surface of the gastrointestinal tract but represents only 2% to 5% of all primary malignant gastrointestinal tumors. Tumors in the small intestine are about 13 to 18 times less common than colon cancer, despite its exposure to a variety of endogenous and exogenous harmful substances[1,2]. Histologically, there are four subtypes of malignant tumors of the small intestine: adenocarcinomas (around 40%); neuroendocrine tumors (35% to 40%); lymphomas (15%) and sarcomas (11% to 13%)[3,4]. When distributed by segments, adenocarcinomas are more common in the duodenum and proximal jejunum, neuroendocrine tumors and lymphomas are more common in the distal portions, while sarcomas have diffuse distribution[3,5].
Duodenal adenocarcinoma represents approximately 0.5% of all malignant gastrointestinal tumors and the most studied of them are those located in the first and second (most periampullary) portions[6,7]. The location of this tumor in the third and/or fourth duodenal portion is rare, presents with non-specific symptoms and is of difficult diagnosis using conventional endoscopic methods[8]. In this paper is presented an adenocarcinoma of the third and fourth portions of the duodenum, with review of the literature, emphasizing the difficulties and the value of video capsule endoscopy for diagnosis.
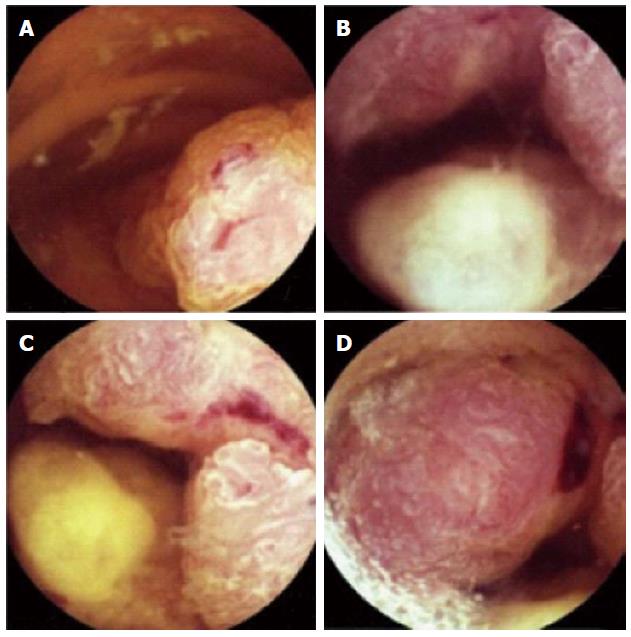
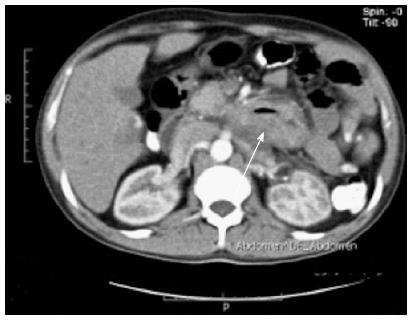
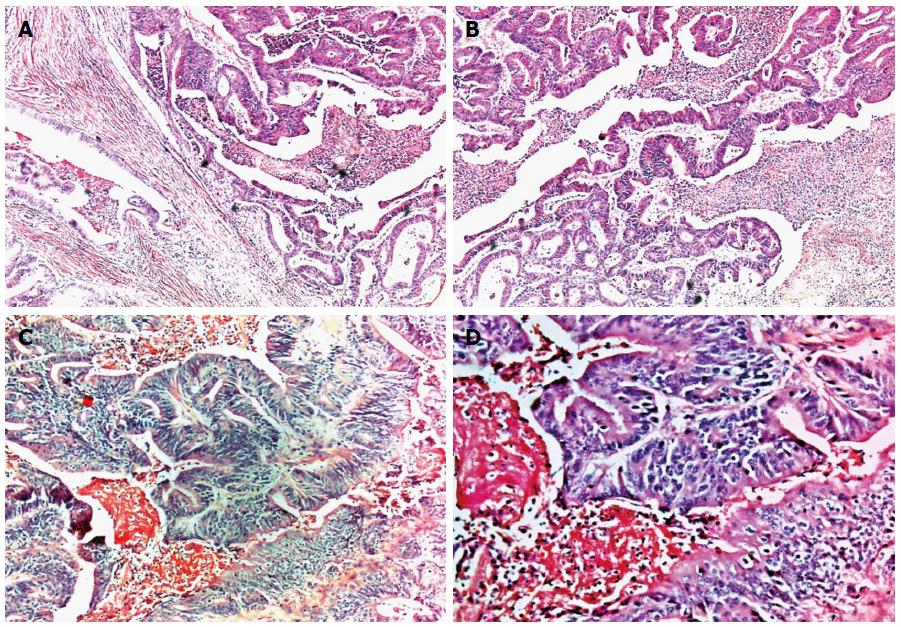
A man, 40 years old, with no medical history, presented with epigastric and mesogastric discomfort and progressive fatigue, with four months of evolution; and reported an episode of melena in moderate quantity. Physical examination was normal except for mucosal pallor. The laboratory findings were consistent with microcytic, hypochromic iron deficiency anemia with 3.49 × 106/mm3 RBC, 7.8 g/dL hemoglobin, 27.5% hematocrit, 79 fL MCV, 22.5 pg MCH, 28.4 g/dL MCHC, 22.6% RDW, 915000/mm3 platelets, and 13 ng/mL serum ferritin. Urine analysis, serum liver function test (LFT), hemolysis markers, and serum electrolytes were unremarkable. Upper gastrointestinal endoscopy (until the 2nd duodenal portion) and colonoscopy were normal. Further investigation, using video capsule endoscopy, in the outpatient setting, showed polypoid lesions involving the third and fourth portions of the duodenum (Figure 1). The biopsy showed a moderately differentiated adenocarcinoma. Abdominal CT showed a wall thickening involving the third and fourth portions of the duodenum and proximal jejunum, with no clear cleavage lines with adjacent structures without evidence of nodal and distant metastasis (Figure 2). The patient underwent a segmental resection of the duodenum (third and fourth portions) and proximal jejunum, with duodenojejunostomy. The pathological examination of the surgical specimen confirmed a moderately differentiated adenocarcinoma infiltrating the wall of the organ without lymph node metastasis (Figure 3). The patient underwent a follow-up by oncology.
This case represents a rare location of primary duodenal adenocarcinoma[8] in a younger patient compared to the average peak incidence of duodenal adenocarcinoma shown in literature (seventh decade of life), with a slight predominance for males[9]. The patient was younger, and there was no known condition associated with early occurrence, such as inflammatory bowel disease[10], familial adenomatous polyposis, or hereditary nonpolyposis colorectal cancer, in which cancer presents earlier (median 39 years)[11] in his personal and/or family medical history .
The clinical picture of adenocarcinoma in the third and fourth portions occurs with rather non-specific symptoms. Unlike periampullary tumors, whose main clinical picture is jaundice and other clinical aspects from the obstruction of the hepatobiliary-pancreatic system[7], in third and fourth portion tumors there are non-specific symptoms such as vague abdominal pain, weight loss, anemia symptoms, but no frank bleeding, and more rarely, bowel obstruction dominates the clinical picture[12,13]. In this case, the duration of symptoms before diagnosis was 4 mo, that is within the average literature range (from 1.4 to 8 mo)[7] One study showed worse 2-year survival rate associated with 4 mo or longer duration[14].
In routine work-up, both upper and lower endoscopy were normal. This situation is a substratum for missing tumors in the third and/or fourth portions, and is often worsened by the low index of clinical suspicion, which usually delays the diagnosis, resulting in advanced disease at diagnosis and decreasing the rate of potentially curative resections[7,15]. After nondiagnostic conventional endoscopic tests, in the setting of iron deficiency anemia, it is worth having a high index of suspicion for tumors beyond the second portion and to carry on the work-up using a method of greater accuracy for these tumors, the endoscopic capsule[8,16].
Capsule endoscopy is a non-invasive procedure that uses a wireless endoscopic device that allows imaging of the gastrointestinal tract. In this case, it was a valuable tool that allowed complete small bowel exploration in the ambulatory setting. The main indications for its use are the evaluation of obscure gastrointestinal bleeding, and Crohn’s disease[17,18]. Its sensitivity and specificity for diagnosing a small bowel tumor is 88.9% to 95% and 75% to 95% respectively, in the setting of obscure gastrointestinal bleeding[16,19]. Tumors are found in about 3% to 9% of patients undergoing this procedure for evaluation of obscure gastrointestinal bleeding, and 50% to 60% were malignant[18]. Video capsule endoscopy has also been used for the evaluation of patients with certain disorders that increase the risk of tumors of the small intestine, such as familial adenomatous polyposis[18].
Treatment of primary duodenal adenocarcinoma depends on the location and staging. In this case, a segmental resection of the duodenum (3rd and 4th portions) and the proximal jejunum (20 cm from duodenojejunal flexure), with primary duodenojejunostomy was performed. This approach was preferred to more extensive resection, because it provides equivalent survival rates to extensive resections (since it is possible to achieve negative margins), with the benefit of lower morbidity than that associated with pancreaticoduodenectomy[20] and even better survival, as was shown in one study[21]. Currently, extensive pancreaticoduodenectomy applies more to tumors of the proximal duodenum (1st and 2nd portions)[22].
The pathological examination of the surgical specimen confirmed a moderately differentiated adenocarcinoma, which is the most common histological grade[3,23], that infiltrates the three layers of the wall, without invasion of adjacent organs or metastasis to the lymph nodes, and surgical margins were negative for tumor cells. Therefore, it was a stadium II tumor (T3 N0 M0), that is the most frequent stage for adenocarcinoma in this site[12,24]. Despite negative margins and no lymph node involvement, the combination of 3 variables present in this case - tumor extension, histological grade and transmural invasion - are associated with poor prognosis[6].
With regard to the adjuvant treatment, there is no established protocol for small bowel adenocarcinomas, due to the lack of randomized trials[25]; and the few available data from retrospective studies have shown no statistically significant overall survival benefit[26]. As with treatment, there is no established follow-up protocol for patients with resected adenocarcinoma of the small intestine. In this case, the patient continued follow-up by oncologist.
Malignant tumors of the small intestine, although rare, should be part of the differential diagnosis in the investigation of obscure gastrointestinal bleeding and the high index of suspicion and appropriate use of endoscopic capsule are of great value.
A 40-year-old male presenting with abdominal discomfort and progressive fatigue due to severe anemia by continuous bleeding from third and fourth portions duodenal cancer.
Small intestine examination with video capsule endoscopy revealed a multilobular tumor, ulcerated with low-flow bleeding lesion in the third and fourth duodenal portions.
Upper gastrointestinal endoscopy (until the 2nd duodenal portion) and colonoscopy were performed to rule out stomach and colon bleeding respectively.
Blood tests demonstrated RBC 3.49 × 106/mm3; hemoglobin 7.8 g/dL; MCH 79 fL and serum ferritin 13 ng/mL. Metabolic panel and liver function tests were within normal limits.
Abdominal computed tomography demonstrated a wall thickening involving third and fourth duodenal portions and proximal jejunum, without evidence of nodal and distant metastasis.
The histopathological examination of the surgical specimen demonstrated a three layer infiltrating adenocarcinoma, without lymph node invasion, with free surgical margins.
Segmental resection of the duodenum (3rd and 4th portions) and proximal jejunum (20 cm from duodenojejunal flexure) was performed, with primary duodenojejunostomy.
Malignant tumors of the third and fourth duodenal portions are a diagnostic challenge using conventional endoscopic tests; a high index of suspicion and appropriate use of the endoscopic capsule is of great value for early diagnosis.
The authors reported primary adenocarcinoma of the 3rd/4th portions of the duodenum in a 40-year-old man. Blood tests revealed microcytic, hypochromic iron deficiency anemia. Upper gastrointestinal endoscopy and colonoscopy were normal, but the polypoid lesions with low-flow bleeding were observed by video capsule endoscopy.
P- Reviewer: Charoenphandhu N S- Editor: Ma YJ L- Editor: O’Neill M E- Editor: Liu XM
| 1. | Aparicio T, Zaanan A, Svrcek M, Laurent-Puig P, Carrere N, Manfredi S, Locher C, Afchain P. Small bowel adenocarcinoma: epidemiology, risk factors, diagnosis and treatment. Dig Liver Dis. 2014;46:97-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 218] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 2. | Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8406] [Cited by in RCA: 8971] [Article Influence: 690.1] [Reference Citation Analysis (0)] |
| 3. | Dabaja BS, Suki D, Pro B, Bonnen M, Ajani J. Adenocarcinoma of the small bowel: presentation, prognostic factors, and outcome of 217 patients. Cancer. 2004;101:518-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 357] [Cited by in RCA: 350] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 4. | Bilimoria KY, Bentrem DJ, Wayne JD, Ko CY, Bennett CL, Talamonti MS. Small bowel cancer in the United States: changes in epidemiology, treatment, and survival over the last 20 years. Ann Surg. 2009;249:63-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 440] [Cited by in RCA: 467] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 5. | Pan SY, Morrison H. Epidemiology of cancer of the small intestine. World J Gastrointest Oncol. 2011;3:33-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 111] [Cited by in RCA: 144] [Article Influence: 10.3] [Reference Citation Analysis (1)] |
| 6. | Ryder NM, Ko CY, Hines OJ, Gloor B, Reber HA. Primary duodenal adenocarcinoma: a 40-year experience. Arch Surg. 2000;135:1070-1074; discussion 1074-1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 67] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Solej M, D’Amico S, Brondino G, Ferronato M, Nano M. Primary duodenal adenocarcinoma. Tumori. 2008;94:779-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Eliakim R, Fischer D, Suissa A, Yassin K, Katz D, Guttman N, Migdal M. Wireless capsule video endoscopy is a superior diagnostic tool in comparison to barium follow-through and computerized tomography in patients with suspected Crohn’s disease. Eur J Gastroenterol Hepatol. 2003;15:363-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | Kim MJ, Choi SB, Han HJ, Park PJ, Kim WB, Song TJ, Suh SO, Choi SY. Clinicopathological analysis and survival outcome of duodenal adenocarcinoma. Kaohsiung J Med Sci. 2014;30:254-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Xie J, Itzkowitz SH. Cancer in inflammatory bowel disease. World J Gastroenterol. 2008;14:378-389. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 215] [Cited by in RCA: 225] [Article Influence: 13.2] [Reference Citation Analysis (1)] |
| 11. | Björk J, Akerbrant H, Iselius L, Bergman A, Engwall Y, Wahlström J, Martinsson T, Nordling M, Hultcrantz R. Periampullary adenomas and adenocarcinomas in familial adenomatous polyposis: cumulative risks and APC gene mutations. Gastroenterology. 2001;121:1127-1135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 159] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 12. | Tocchi A, Mazzoni G, Puma F, Miccini M, Cassini D, Bettelli E, Tagliacozzo S. Adenocarcinoma of the third and fourth portions of the duodenum: results of surgical treatment. Arch Surg. 2003;138:80-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 69] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 13. | Bang CS, Yoon JH, Choi SH, Eom JH, Lee YS, Lee YH, Han SH. Primary Adenocarcinoma of Duodenum Located in Third Portion Cured by Wedge Resection. Korean J Helicobacter Up Gastrointest Res. 2013;13:263-266. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Delcore R, Thomas JH, Forster J, Hermreck AS. Improving resectability and survival in patients with primary duodenal carcinoma. Am J Surg. 1993;166:626-630; discussion 630-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 45] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Stell D, Mayer D, Mirza D, Buckels J. Delayed diagnosis and lower resection rate of adenocarcinoma of the distal duodenum. Dig Surg. 2004;21:434-438; discussion 438-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Hartmann D, Schmidt H, Bolz G, Schilling D, Kinzel F, Eickhoff A, Huschner W, Möller K, Jakobs R, Reitzig P. A prospective two-center study comparing wireless capsule endoscopy with intraoperative enteroscopy in patients with obscure GI bleeding. Gastrointest Endosc. 2005;61:826-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 201] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 17. | Ladas SD, Triantafyllou K, Spada C, Riccioni ME, Rey JF, Niv Y, Delvaux M, de Franchis R, Costamagna G. European Society of Gastrointestinal Endoscopy (ESGE): recommendations (2009) on clinical use of video capsule endoscopy to investigate small-bowel, esophageal and colonic diseases. Endoscopy. 2010;42:220-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 172] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 18. | Eliakim R. Video capsule endoscopy of the small bowel. Curr Opin Gastroenterol. 2010;26:129-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Pennazio M, Santucci R, Rondonotti E, Abbiati C, Beccari G, Rossini FP, De Franchis R. Outcome of patients with obscure gastrointestinal bleeding after capsule endoscopy: report of 100 consecutive cases. Gastroenterology. 2004;126:643-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 637] [Cited by in RCA: 604] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 20. | Bakaeen FG, Murr MM, Sarr MG, Thompson GB, Farnell MB, Nagorney DM, Farley DR, van Heerden JA, Wiersema LM, Schleck CD. What prognostic factors are important in duodenal adenocarcinoma? Arch Surg. 2000;135:635-641; discussion 641-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 160] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 21. | Kaklamanos IG, Bathe OF, Franceschi D, Camarda C, Levi J, Livingstone AS. Extent of resection in the management of duodenal adenocarcinoma. Am J Surg. 2000;179:37-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 90] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 22. | Halfdanarson TR, McWilliams RR, Donohue JH, Quevedo JF. A single-institution experience with 491 cases of small bowel adenocarcinoma. Am J Surg. 2010;199:797-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 148] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 23. | Hung FC, Kuo CM, Chuah SK, Kuo CH, Chen YS, Lu SN, Chang Chien CS. Clinical analysis of primary duodenal adenocarcinoma: an 11-year experience. J Gastroenterol Hepatol. 2007;22:724-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 24. | Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. American Joint Committee on Cancer (AJCC) Cancer staging manual. 7th ed. New York: Springer-Verlag 2010; 718. |
| 25. | Singhal N, Singhal D. Adjuvant chemotherapy for small intestine adenocarcinoma. Cochrane Database Syst Rev. 2007;CD005202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Overman MJ, Kopetz S, Lin E, Abbruzzese JL, Wolff RA. Is there a role for adjuvant therapy in resected adenocarcinoma of the small intestine. Acta Oncol. 2010;49:474-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 63] [Article Influence: 4.2] [Reference Citation Analysis (0)] |