Published online Aug 21, 2015. doi: 10.3748/wjg.v21.i31.9380
Peer-review started: January 21, 2015
First decision: March 10, 2015
Revised: March 20, 2015
Accepted: April 28, 2015
Article in press: April 28, 2015
Published online: August 21, 2015
Processing time: 211 Days and 20.2 Hours
AIM: To present a simple colonoscopy reporting system that can be checked easily the detection rate of colon polyps.
METHODS: A simple colonoscopy reporting system Kosin Gastroenterology (KG quality reporting system) was developed. The polyp detection rate (PDR), adenoma detection rate (ADR), serrated polyp detection rate (SDR), and advanced adenoma detection rate (AADR) are easily calculated to use this system.
RESULTS: In our gastroenterology center, the PDR, ADR, SDR, and AADR test results from each gastroenterologist were updated, every month. Between June 2014, when the program was started, and December 2014, the overall PDR and ADR in our center were 62.5% and 41.4%, respectively. And the overall SDR and AADR were 7.5% and 12.1%, respectively.
CONCLUSION: We envision that KG quality reporting system can be applied to develop a comprehensive system to check colon polyp detection rates in other gastroenterology centers.
Core tip: Detecting the rate of colon polyps, such as the adenoma detection rate is an important quality indicator during colonoscopy exams. However, reporting the detection rate in daily practice is not easy because manual reporting requires a lot of time and effort. To our knowledge, reporting systems for detecting the rate of colon polyps are rare. We developed a simple colonoscopy reporting system that can be checked easily the detection rate of colon polyps. We envision our system can be applied to develop an optimal system for assessing the detection rate of colon polyps in other gastroenterology centers.
- Citation: Kim JH, Choi YJ, Kwon HJ, Park SJ, Park MI, Moon W, Kim SE. Simple colonoscopy reporting system checking the detection rate of colon polyps. World J Gastroenterol 2015; 21(31): 9380-9386
- URL: https://www.wjgnet.com/1007-9327/full/v21/i31/9380.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i31.9380
Colorectal cancer is ranked as the third leading cause of cancer-related death in the world[1-3]. It is well known that most colorectal cancers arise from adenomatous polyps and patients with adenomatous polyps have greater risks of future development of advanced neoplasia[4-8]. A colonoscopy is a useful tool to detect and remove colorectal polyps. However, a number of polyps could be missed clinically during colonoscopic examination, which can increase the incidence of interval cancer[9-12]. A large tandem colonoscopy study that assessed variable detection of adenomas, demonstrated miss rates ranged from 17% to 48%[13]. To reduce the missing rate of colon polyps, several quality indicators including adenoma detection, bowel preparation, cecal intubation, withdrawal time, patient’s discomfort, and complications, such as perforation and postpolypectomy bleeding have been suggested, all of which aim to measure colonoscopists’ performance and to target quality improvement[14,15]. Of such indicators, the adenoma detection rate (ADR) is currently considered the most important quality indicator during colonoscopy[16-18]. According to data from the study by Boroff et al[19], the polyp detection rate (PDR) may be a valid surrogate marker of ADR in the proximal but not the distal colon. In daily practice however, reporting for the PDR and ADR is not easy, because manual reporting requires a lot of time and effort. Recently, van Doorn et al[20] developed a new colonoscopy reporting system that enables automatic quality assessment, and reported that 94% of colonoscopies that are performed overall were reported completely and that ADR was used as the measurement unit in 35.4% of the system reports. However, in practice it is not easy to introduce this system to other gastroenterology centers, because additional costs will be incurred as this system was developed in collaboration with the Olympus Corporation.
To our knowledge, reporting systems for detecting the rate of colon polyps are rare. Our gastroenterology center also had not checked the PDR and ADR until May 2014, because we thought that this process was complicated. The “KG (Kosin gastroenterology) quality reporting system” was produced because we wanted to identify an easier and more accessible way to check PDR and ADR on routine colonoscopic examination. We tried to develop a simple colonoscopy reporting system which can possibly check the PDR and ADR, as well as the serrated polyp detection rate (SDR) and advanced adenoma detection rate (AADR). In this study, we describe a simple colonoscopy reporting system that was applied in our gastroenterology center to check the PDR, ADR, SDR, and AADR.
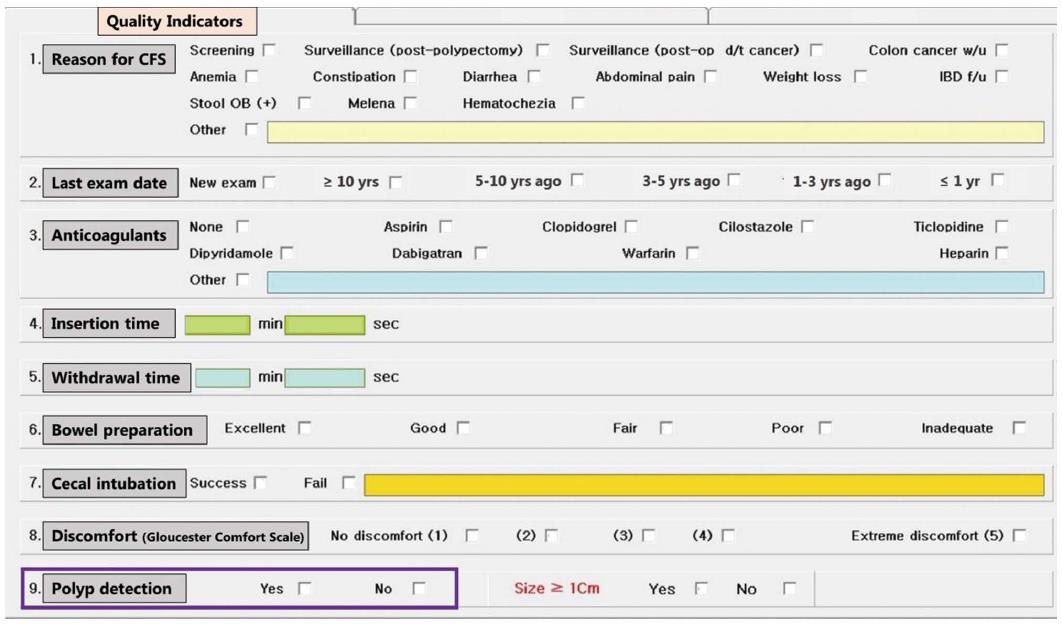
The “KG Quality reporting system” platform used our hospital’s computer program system. In previous colonoscopic input program systems that were used in our gastroenterology center, we manually entered some data including the insertion time, withdrawal time, bowel preparation, and cecal intubation. Based on the current literature and knowledge[15,20], we developed a colonoscopic input program system list that included established quality indicators, such as “reason for colonoscopy, insertion time, withdrawal time, bowel preparation, cecal intubation, patient’s discomfort status, and polyp detection (including whether polyp size are larger or smaller than 1 cm)”. Two indicators, including “last examination date and anticoagulants”, were also added (Figure 1). We used the Aronchick bowel preparation scale as the bowel preparation index, and the Gloucester Comfort Scale[21] as the patient’s discomfort scale index. All indicators could be entered with one click, except for insertion time and withdrawal time which are entered as the number of minutes and seconds. If one or more polyps were located during the colonoscopic examination, the gastroenterologist would check “yes” for the polyp detection indicator (violet colored box on Figure 1). The polyp size which is measure by using open biopsy forceps, could be indicated by selecting whether “Size ≥ 1 cm” or not.
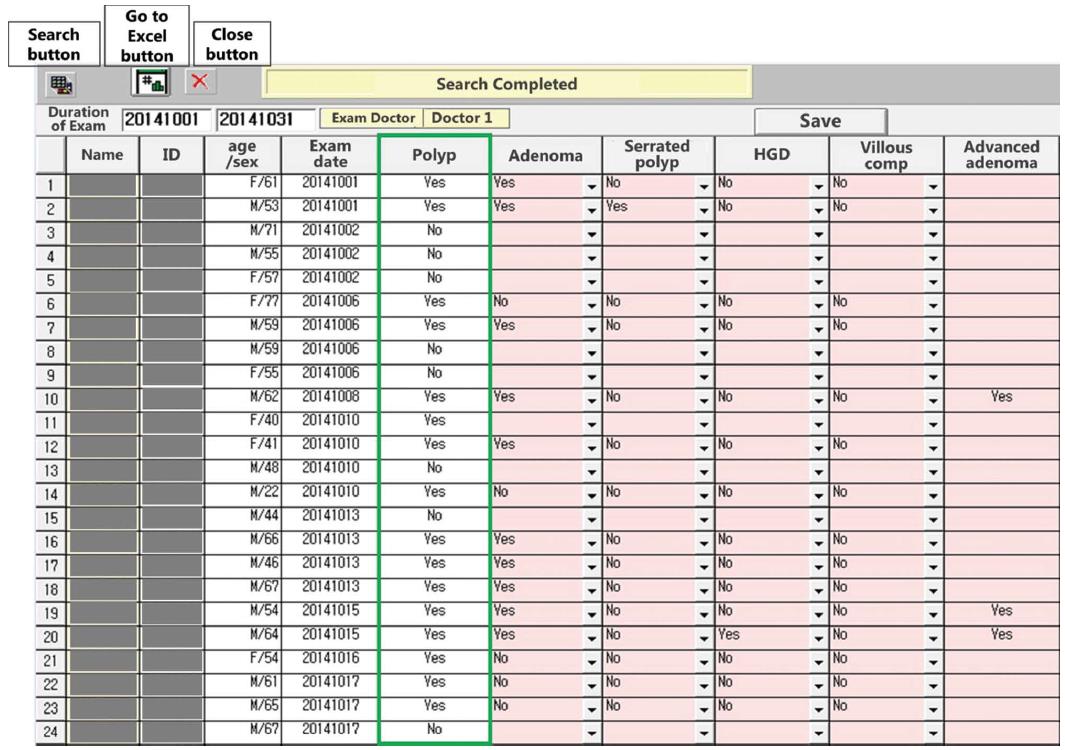
We made a patients’ list searchable so each gastroenterologist could find the examined patients. In this step, several items including “Polyp”, “Adenoma”, “Serrated polyp”, “HGD (high grade dysplasia)”, “Villous comp (component)”, and “Advanced adenoma” are presented on a new page (Figure 2). Serrated polyps are defined as hyperplastic polyps (HP) which excluded small lesions (< 10 mm) of HP limited to the rectum and sigmoid, sessile serrated adenoma/polyp (SSA/P), or traditional serrated adenoma (TSA)[22]. Advanced adenoma is defined as adenoma that was 1 cm or greater, or with HGD, or with villous component (tubulovillous or villous)[23,24]. The “Polyp” column (green colored box on Figure 2) is automatically presented as “Yes” or “No” which is linked with a click of “Yes” or “No” to the polyp detection indicator shown in Figure 1. For other items including “Adenoma”, “Serrated polyp”, “HGD”, “Villous comp”, and “Advanced adenoma”, we tried to link automatically with the pathological data, however, in practice, this approach was not easy. We modified this approach and adjusted the program so that data such as “Adenoma”, “Serrated polyp”, “HGD”, and “Villous comp” could be entered manually. Each gastroenterologist was asked to input this specific data. For example, if the histology of a resected polyp was adenoma, the examining gastroenterologist was asked to enter “Yes” in the “Adenoma” space. Similarly, if the histology of a resected polyp was serrated polyp, the examining gastroenterologist entered “Yes” in the ‘Serrated polyp’ space. In cases of adenoma with HGD or villous components, the gastroenterologist input “Yes” in the “HGD” or “Villous comp” spaces, respectively. If any one of the three components including “HGD”, “Villous comp” (shown in Figure 2), and “Size ≥ 1 cm (shown in Figure 1)” were entered as “Yes”, this information was automatically presented as “Yes” in the “Advanced adenoma” space. For cases with multiple resected polyps, additional work is needed to identify whether the resected polyp was an adenoma larger than 1 cm in size. Although this process could be tedious, entering one month of data only requires about 15 min. Additionally, this process can help to identify gastroenterologist’s own pathological data for resected polyps. These inputted data can be saved by selecting the “Save” button, and can be transferred to the Excel program (Microsoft Corporation, Washington, United States) (Figure 2).
Calculating PDR, ADR, SDR, and AADR is easily accomplished using the Microsoft Excel program. This process was performed by the investigator. PDR is calculated as the number of colonoscopies in which one or more polyps were detected, divided by the total number of colonoscopies performed by the colonoscopist. ADR is calculated as the number of colonoscopies in which one or more adenomas were detected, divided by the total number of colonoscopies performed by the colonoscopist. SDR is calculated as the number of colonoscopies in which one or more serrated polyps were identified, divided by the total number of colonoscopies performed by the colonoscopist. AADR is calculated as the number of colonoscopies in which one or more advanced adenomas were detected, divided by the total number of colonoscopies performed by the colonoscopist.
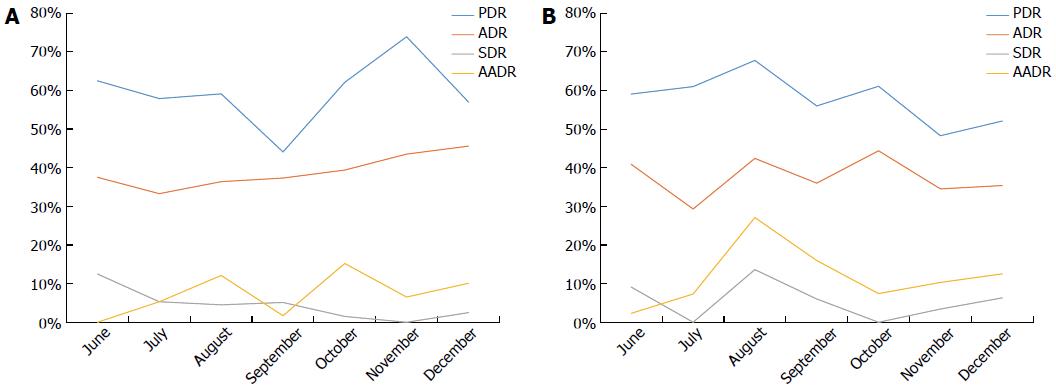
In our gastroenterology center there are three experts and eleven training fellows; a monthly average of 60 colonoscopic examinations are performed per gastroenterologist. By using our system, we calculated the PDR, ADR, SDR, and AADR of each gastroenterologist in our clinic. Based on these data, we analyzed the flow of data of each gastroenterologist, and estimated the overall PDR, ADR, SDR, and AADR of all gastroenterologists in our clinic. At the beginning of every month, the results of the last month, which consisted of tables and figures were updated and sent to all gastroenterologists in our clinic by e-mail. Between June 2014, when the program was started, and December 2014, the overall PDR of gastroenterologists in our clinic was 62.5% (66.0% in male patients, and 55.8% in female patients). The overall ADR was 41.4% (45.5% in male patients, and 36.3% in female patients), the overall SDR was 7.5% (7.7% in male patients, and 7.4% in female patients), and the overall AADR was 12.1% (13.6% in male patients, and 9.7% in female patients). These data are summarized in Table 1. The flow of each gastroenterologist’s monthly data was plotted with a broken line graph. Figure 3A and Figure 3B show examples for the flow of monthly data of two fellows.
| Month | 6 | 7 | 8 | 9 | 10 | 11 | 12 | Overall (male vs female) |
| PDR | 64.6% | 62.4% | 64.3% | 61.0% | 59.6% | 63.7% | 64.2% | 62.5% (66.0% vs 55.8%) |
| ADR | 40.4% | 36.1% | 44.3% | 38.2% | 40.7% | 41.0% | 47.2% | 41.4% (45.5% vs 36.3%) |
| SDR | 13.5% | 8.2% | 11.2% | 8.0% | 5.8% | 6.6% | 8.7% | 7.5% (7.7% vs 7.4%) |
| AADR | 6.8% | 13.5% | 16.0% | 11.2% | 13.3% | 11.2% | 12.8% | 12.1% (13.6% vs 9.7%) |
We worked to develop an easy system to check the PDR, ADR, SDR, and AADR during routine colonscopic examinations. The first step was to search the list of patients that were examined by each gastroenterologist. We allowed the examined patients’ list to be searchable by each gastroenterologist in our clinic, and we also made it possible to automatically link between the “Polyp” indicator (violet colored box on Figure 1) and the results of the “Polyp” column (green colored box on Figure 2). The second step was to input the “Adenoma”, “Serrated polyp”, “HGD”, and “Villous comp” data. This process was performed by each examining gastroenterologist. And then, PDR, ADR, SDR, and AADR were easily calculated as described in the “Methods” section.
Several quality indicators for colonoscopy are used in the KG quality reporting system (Figure 1). Of these indicators, ADR is the quality indicator with the strongest association to post-colonoscopy colorectal cancer or missed colorectal cancer. Among healthy asymptomatic patients that undergo screening colonoscopy, adenomas should detected in ≥ 25% of men and ≥ 15% women more than 50 years old[15]. In our gastroenterology center, the overall ADR was 41.4% (45.5% in male patients, and 36.3% in female patients) between June and December 2014. Serrated polyps are classified as HP which excluded small lesions (< 10 mm) of HP limited to the rectum and sigmoid, SSA/P, or TSA[22]. Both SSA/P and TSA are pre-cancerous lesions, and SSA/P located in the proximal colon is considered as a cause of interval cancer[25]. A recent article by these investigators showed that the SDR correlated with the ADR in their routine colonoscopic examinations[26]. In our gastroenterology center, the overall SDR was 7.5% (7.7% in male patients, and 7.4% in female patients) between June and December 2014. According to the current literature and knowledge, about one-third of all polyps larger than 10 mm in size have advanced histology, but diminutive polyps (≤ 5 mm in size) rarely have advanced pathology[27,28]. A polyp larger than 10 mm in size is categorized as advanced adenoma, which also includes adenoma with high-grade dysplasia (HGD), or with villous components (tubulovillous or villous)[23,24]. Recently, Greenspan et al[29] reported that the overall AADR was 7.97% for 14 colonoscopists who performed a total of 1944 colonoscopies. Additionally, Lee et al[30] showed that the overall AADR was 4.46% for 18 colonoscopists who performed a total of 561 colonoscopies. In our gastroenterology center, the overall AADR was 12.1% (13.6% in male patients, and 9.7% in female patients) between June and December 2014.
There are some limitations to the system we developed. First, the detection rate of colon polyps is not categorized by the reason for colonoscopy. Our data included patients with prior polypectomy as well as screening colonoscopy, so the detection rate of colon polyps in our gastroenterology center could be overestimated. In the next step, we will develop this system to categorize the detection rate of colon polyps by the reason for colonoscopy. Second, the input of pathologic data is performed manually in our system. Currently, each examining gastroenterologist enters the pathologic data of resected polyps, which it can cause manual data entry errors. The next step is to develop an automatic linkage between our system and pathologic data.
In addition to the practical application of our system which checks the detection rate of colon polyps, other possible associations between various quality indicators and the detection rate of colon polyps can be evaluated. The data acquired from our program can be used as a basis for performing colonoscopy research. Furthermore, identifying gastroenterologists’ own data for polyp detection rates can facilitate colonoscopic examination quality improvements. In the next step, we will develop our system to possible the statistical analysis for each quality indicator. Although the KG quality reporting system is still being developed, we hope that this system can be applied to develop an optimal system for assessing the detection rate of colon polyps in other gastroenterology centers.
Detecting the rate of colon polyps, such as the adenoma detection rate (ADR) is an important quality indicator during colonoscopy exams. However, reporting the detection rate in daily practice is not easy because manual reporting is time consuming and requires effort. To our knowledge, reporting systems for detecting the rate of colon polyps are rare.
This study presents a simple colonoscopy reporting system (KG quality reporting system) that can be checked easily the detection rate of colon polyps.
The KG quality reporting system is focused on the detection rate of colon polyps, such as polyp detection rate, ADR, serrated polyp detection rate, and advanced adenoma detection rate.
This system can be applied to develop an optimal system for assessing the detection rate of colon polyps in other gastroenterology centers.
Serrated polyps are defined as hyperplastic polyps which excluded small lesions (< 10 mm) of hyperplastic polyps limited to the rectum and sigmoid, sessile serrated adenoma/polyp, or traditional serrated adenoma. Advanced adenoma is defined as adenoma that was 1 cm or greater, or with high grade dysplasia, or with villous component (tubulovillous or villous).
This paper deals with a simple colonoscopy reporting system that can facilitate the automatic analysis of colonoscopy quality indicators. This system may be useful for performing colonoscopy research and improving the quality of colonoscopy.
P- Reviewer: Sakata Y, Trevisani L S- Editor: Ma YJ L- Editor: A E- Editor: Zhang DN
| 1. | Edwards BK, Ward E, Kohler BA, Eheman C, Zauber AG, Anderson RN, Jemal A, Schymura MJ, Lansdorp-Vogelaar I, Seeff LC. Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010;116:544-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1390] [Cited by in RCA: 1499] [Article Influence: 99.9] [Reference Citation Analysis (1)] |
| 2. | Ferlay J, Autier P, Boniol M, Heanue M, Colombet M, Boyle P. Estimates of the cancer incidence and mortality in Europe in 2006. Ann Oncol. 2007;18:581-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1761] [Cited by in RCA: 1707] [Article Influence: 94.8] [Reference Citation Analysis (0)] |
| 3. | Joseph DA, King JB, Miller JW, Richardson LC. Prevalence of colorectal cancer screening among adults--Behavioral Risk Factor Surveillance System, United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61 Suppl:51-56. [PubMed] |
| 4. | Cottet V, Jooste V, Fournel I, Bouvier AM, Faivre J, Bonithon-Kopp C. Long-term risk of colorectal cancer after adenoma removal: a population-based cohort study. Gut. 2012;61:1180-1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 181] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 5. | Loeve F, van Ballegooijen M, Boer R, Kuipers EJ, Habbema JD. Colorectal cancer risk in adenoma patients: a nation-wide study. Int J Cancer. 2004;111:147-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 74] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Robertson DJ, Greenberg ER, Beach M, Sandler RS, Ahnen D, Haile RW, Burke CA, Snover DC, Bresalier RS, McKeown-Eyssen G. Colorectal cancer in patients under close colonoscopic surveillance. Gastroenterology. 2005;129:34-41. [PubMed] |
| 7. | Yamaji Y, Mitsushima T, Ikuma H, Watabe H, Okamoto M, Kawabe T, Wada R, Doi H, Omata M. Incidence and recurrence rates of colorectal adenomas estimated by annually repeated colonoscopies on asymptomatic Japanese. Gut. 2004;53:568-572. [PubMed] |
| 8. | Muto T, Bussey HJ, Morson BC. The evolution of cancer of the colon and rectum. Cancer. 1975;36:2251-2270. [PubMed] |
| 9. | Ananthakrishnan AN, Chan AT. Missed polyps, missed opportunities. Gastrointest Endosc. 2011;74:262-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Corley DA, Jensen CD, Marks AR, Zhao WK, Lee JK, Doubeni CA, Zauber AG, de Boer J, Fireman BH, Schottinger JE. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med. 2014;370:1298-1306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1251] [Cited by in RCA: 1539] [Article Influence: 139.9] [Reference Citation Analysis (0)] |
| 11. | le Clercq CM, Winkens B, Bakker CM, Keulen ET, Beets GL, Masclee AA, Sanduleanu S. Metachronous colorectal cancers result from missed lesions and non-compliance with surveillance. Gastrointest Endosc. 2015;82:325-333.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 12. | Samadder NJ, Curtin K, Tuohy TM, Pappas L, Boucher K, Provenzale D, Rowe KG, Mineau GP, Smith K, Pimentel R. Characteristics of missed or interval colorectal cancer and patient survival: a population-based study. Gastroenterology. 2014;146:950-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 230] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 13. | Rex DK, Cutler CS, Lemmel GT, Rahmani EY, Clark DW, Helper DJ, Lehman GA, Mark DG. Colonoscopic miss rates of adenomas determined by back-to-back colonoscopies. Gastroenterology. 1997;112:24-28. [PubMed] |
| 14. | Kaminski MF, Regula J, Kraszewska E, Polkowski M, Wojciechowska U, Didkowska J, Zwierko M, Rupinski M, Nowacki MP, Butruk E. Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med. 2010;362:1795-1803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1287] [Cited by in RCA: 1451] [Article Influence: 96.7] [Reference Citation Analysis (0)] |
| 15. | Rex DK, Petrini JL, Baron TH, Chak A, Cohen J, Deal SE, Hoffman B, Jacobson BC, Mergener K, Petersen BT. Quality indicators for colonoscopy. Am J Gastroenterol. 2006;101:873-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 532] [Cited by in RCA: 559] [Article Influence: 29.4] [Reference Citation Analysis (0)] |
| 16. | Anderson JC, Butterly LF. Colonoscopy: quality indicators. Clin Transl Gastroenterol. 2015;6:e77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 17. | Leung FW. PDR or ADR as a quality indicator for colonoscopy. Am J Gastroenterol. 2013;108:1000-1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Rex DK, Kahi C, O’Brien M, Levin TR, Pohl H, Rastogi A, Burgart L, Imperiale T, Ladabaum U, Cohen J. The American Society for Gastrointestinal Endoscopy PIVI (Preservation and Incorporation of Valuable Endoscopic Innovations) on real-time endoscopic assessment of the histology of diminutive colorectal polyps. Gastrointest Endosc. 2011;73:419-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 406] [Cited by in RCA: 456] [Article Influence: 32.6] [Reference Citation Analysis (0)] |
| 19. | Boroff ES, Gurudu SR, Hentz JG, Leighton JA, Ramirez FC. Polyp and adenoma detection rates in the proximal and distal colon. Am J Gastroenterol. 2013;108:993-999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 85] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 20. | van Doorn SC, van Vliet J, Fockens P, Dekker E. A novel colonoscopy reporting system enabling quality assurance. Endoscopy. 2014;46:181-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 21. | National Health Service Bowel Cancer Screening Programme Endoscopy Quality Assurance Group. Quality assurance guidelines for colonoscopy publication no. 6. National Health Service;. 2011; Available from: http://www.cancerscreening.nhs.uk/bowel/publications/nhsbcsp06.pdf. |
| 22. | Rex DK, Ahnen DJ, Baron JA, Batts KP, Burke CA, Burt RW, Goldblum JR, Guillem JG, Kahi CJ, Kalady MF. Serrated lesions of the colorectum: review and recommendations from an expert panel. Am J Gastroenterol. 2012;107:1315-1329; quiz 1314, 1330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 825] [Cited by in RCA: 828] [Article Influence: 63.7] [Reference Citation Analysis (0)] |
| 23. | Martínez ME, Sampliner R, Marshall JR, Bhattacharyya AK, Reid ME, Alberts DS. Adenoma characteristics as risk factors for recurrence of advanced adenomas. Gastroenterology. 2001;120:1077-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 24. | Saini SD, Kim HM, Schoenfeld P. Incidence of advanced adenomas at surveillance colonoscopy in patients with a personal history of colon adenomas: a meta-analysis and systematic review. Gastrointest Endosc. 2006;64:614-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 141] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 25. | Arain MA, Sawhney M, Sheikh S, Anway R, Thyagarajan B, Bond JH, Shaukat A. CIMP status of interval colon cancers: another piece to the puzzle. Am J Gastroenterol. 2010;105:1189-1195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 289] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 26. | Kahi CJ, Li X, Eckert GJ, Rex DK. High colonoscopic prevalence of proximal colon serrated polyps in average-risk men and women. Gastrointest Endosc. 2012;75:515-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 129] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 27. | Lieberman D, Moravec M, Holub J, Michaels L, Eisen G. Polyp size and advanced histology in patients undergoing colonoscopy screening: implications for CT colonography. Gastroenterology. 2008;135:1100-1105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 355] [Cited by in RCA: 326] [Article Influence: 19.2] [Reference Citation Analysis (1)] |
| 28. | Pickhardt PJ. The natural history of colorectal polyps and masses: rediscovered truths from the barium enema era. AJR Am J Roentgenol. 2007;188:619-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 29. | Greenspan M, Rajan KB, Baig A, Beck T, Mobarhan S, Melson J. Advanced adenoma detection rate is independent of nonadvanced adenoma detection rate. Am J Gastroenterol. 2013;108:1286-1292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 30. | Lee SY, Kim NH, Chae HB, Han KJ, Lee TH, Jang CM, Yoo KM, Jung YS, Park JH, Kim HJ. [Correlation between adenoma detection rate and advanced adenoma detection rate]. Korean J Gastroenterol. 2014;64:18-23. [PubMed] |