Published online Aug 21, 2015. doi: 10.3748/wjg.v21.i31.9245
Peer-review started: January 27, 2015
First decision: April 14, 2015
Revised: April 21, 2015
Accepted: July 3, 2015
Article in press: July 3, 2015
Published online: August 21, 2015
Processing time: 205 Days and 22.9 Hours
Hemorrhoids is recognized as one of the most common medical conditions in general population. It is clinically characterized by painless rectal bleeding during defecation with or without prolapsing anal tissue. Generally, hemorrhoids can be divided into two types: internal hemorrhoid and external hemorrhoid. External hemorrhoid usually requires no specific treatment unless it becomes acutely thrombosed or causes patients discomfort. Meanwhile, low-graded internal hemorrhoids can be effectively treated with medication and non-operative measures (such as rubber band ligation and injection sclerotherapy). Surgery is indicated for high-graded internal hemorrhoids, or when non-operative approaches have failed, or complications have occurred. Although excisional hemorrhoidectomy remains the mainstay operation for advanced hemorrhoids and complicated hemorrhoids, several minimally invasive operations (including Ligasure hemorrhoidectomy, doppler-guided hemorrhoidal artery ligation and stapled hemorrhoidopexy) have been introduced into surgical practices in order to avoid post-hemorrhiodectomy pain. This article deals with some fundamental knowledge and current treatment of hemorrhoids in a view of a coloproctologist - which includes the management of hemorrhoids in complicated situations such as hemorrhoids in pregnancy, hemorrhoids in immunocompromised patients, hemorrhoids in patients with cirrhosis or portal hypertension, hemorrhoids in patients having antithrombotic agents, and acutely thrombosed or strangulated hemorrhoids. Future perspectives in the treatment of hemorrhoids are also discussed.
Core tip: Hemorrhoids is a very common anorectal disease defined as the symptomatic enlargement and/or distal displacement of anal cushions. Apart from abnormally dilated vascular channel and destructive changes in supporting tissue within anal cushions, there is emerging evidence that hemorrhoids is associated with hyperperfusion state of anorectal region and some degree of tissue inflammation. This article comprehensively and thoroughly reviews the pathophysiology, clinical diagnosis, and current treatment of hemorrhoids - which includes dietary and lifestyle modification, pharmacological approach, office-based procedures and operations for hemorrhoids (such as hemorrhoidectomy and other non-excisional surgery). The management of hemorrhoids in complicated situations is also addressed.
- Citation: Lohsiriwat V. Treatment of hemorrhoids: A coloproctologist’s view. World J Gastroenterol 2015; 21(31): 9245-9252
- URL: https://www.wjgnet.com/1007-9327/full/v21/i31/9245.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i31.9245
Hemorrhoids is a very common anorectal disease defined as the symptomatic enlargement and/or distal displacement of anal cushions[1,2], which are prominences of anal mucosa formed by loose connective tissue, smooth muscle, arterial and venous vessels[3]. The true prevalence of hemorrhoids is unknown; however, recent evidence has suggested an increasing prevalence of hemorrhoids over time. In 1990, an epidemiologic study of hemorrhoids in the United State revealed a prevalence rate of 4.4%, whereas some reports in the 21st century from South Korea and Austria yielded a prevalence of hemorrhoids in adult population of 14.4%[4] and 38.9%[5], respectively. It has been estimated that 25% of British people and 75% of American citizens will experience hemorrhoids at some time in their lives[6,7], especially in pregnant women and elderly adults.
People with hemorrhoids, and those wrongly thought to have hemorrhoids, had a tendency to use self-medication rather than to seek proper medical attention[8]. According to the Google’s annual roundup in 2012 (Google Zeitgeist), hemorrhoids was the top trending heath issue in the United State, ahead of gastroesophageal reflux disease and sexually transmitted disease. Unfortunately, the quality of information about hemorrhoids treatment on the internet was greatly variable and almost 50% of websites were of poor quality[9]. Clinicians should therefore advise and treat patients with hemorrhoids with evidence-based medicine and the standard of care. Practically, most patients with low-graded hemorrhoids can be effectively treated with non-operative measures by either primary care physician, gastroenterologist or general surgeon in an outpatient setting. Surgery is indicated for high-graded hemorrhoids, or when non-operative approaches have failed, or complications have occurred[2]. This article deals with some fundamental knowledge and current treatment of uncomplicated and complicated hemorrhoids in a view of a coloproctologist.
The exact pathophysiology of hemorrhoids is poorly understood. Currently, hemorrhoids is the pathologic term describing symptomatic and abnormally downward displacement of normal anal cushions[2]. As a result of destructive changes in the supporting connective tissue and abnormal blood circulation within anal cushions, the sliding anal cushions embrace abnormal dilation and distortion of hemorrhoid plexus. A recent study of morphology and hemodynamic of arterial supply to the anal canal revealed a hyperperfusion state of hemorrhoidal plexus in patients with hemorrhoids[10], suggesting the dysregulation of vascular tone within hemorrhoid tissue[1,2]. Moreover, it was evident that hemorrhoidal tissue contained some inflammatory cells[11] and newly-formed microvessels[12]. For circumferential prolapsing hemorrhoids, these might be related to an internal rectal prolapse[13]. In conclusion, although the true pathophysiology of hemorrhoid development is unknown, it is likely to be multifactorial[2] - including sliding anal cushion, hyperperfusion of hemorrhoid plexus, vascular abnormality, tissue inflammation and internal rectal prolapse (rectal redundancy). The different philosophies of hemorrhoid development may lead to different approaches to the treatment of hemorrhoids[2].
Several risk factors have been claimed to be the etiologies of hemorrhoid development including aging, obesity, abdominal obesity, depressive mood and pregnancy[4]. Meanwhile, some conditions related to increased intraabdominal pressure, such as constipation and prolonged straining, are widely believed to cause hemorrhoids as a result of compromised venous drainage of hemorrhoid plexus[14]. Some types of food and lifestyle, including low fiber diet, spicy foods and alcohol intake, was reported to link with the development of hemorrhoids and the aggravation of acute hemorrhoid symptoms[15].
The most common presentation of hemorrhoids is painless rectal bleeding during defecation with or without prolapsing anal tissue. The blood is normally not mixed in stool but instead coated on the outer surface of stool, or it is seen during cleansing after bowel movement. The blood is typically bright red since hemorrhoid plexus has direct arteriovenous communication[10]. Patients with complicated hemorrhoids such as acutely thrombosed external hemorrhoids and strangulated internal hemorrhoids may present with anal pain and lump at the anal verge. It is uncommon that patients with uncomplicated hemorrhoid manifest any anal pain. In fact, severe anal pain in patient with hemorrhoids is more likely due to anal fissure and anorectal abscess[2].
A precise history and thorough physical examination, including digital rectal examination and anoscopy, are imperative for the diagnosis of hemorrhoids. Unless bright red blood is clearly seen from hemorrhoids, any patients with rectal bleeding should be scheduled for flexible sigmoidoscopy or colonoscopy, especially those being at risk of colorectal cancer[1,2].
Hemorrhoids are generally classified by their location; internal (originates above the dentate line and covered by anal mucosa), external (originates below the dentate line and covered by anoderm) and mixed type. Internal hemorrhoids are further graded based on their appearance and degree of prolapse: (1) Grade I: non-prolapsing hemorrhoids; (2) Grade II: prolapsing hemorrhoids on straining but reduce spontaneously; (3) Grade III: prolapsing hemorrhoids requiring manual reduction; and (4) Grade IV: non-reducible prolapsing hemorrhoids which include acutely thrombosed, incarcerated hemorrhoids[16].
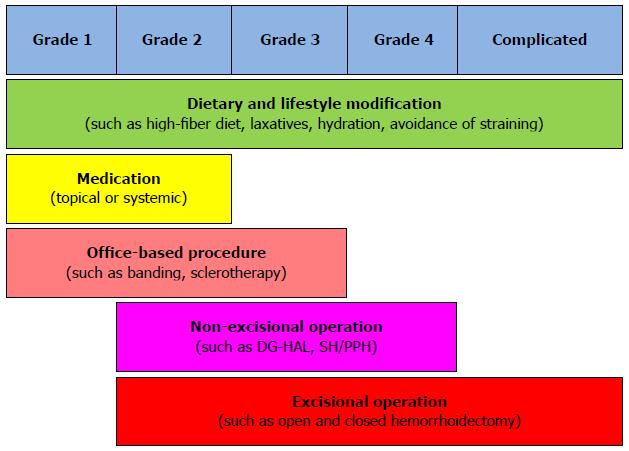
Treatment options mainly depend on the type and severity of hemorrhoids, patient’s preference and the expertise of physicians. Low-graded internal hemorrhoids are effectively treated with dietary and lifestyle modification, medical treatment and/or office-based procedures such as rubber band ligation and sclerotherapy (Figure 1). An operation is usually indicated in low-graded hemorrhoids refractory to non-surgical treatment, high-graded hemorrhoids, and strangulated hemorrhoids[2]. Meanwhile, external hemorrhoid requires no specific treatment unless it becomes acutely thrombosed or causes patient discomfort.
A meta-analysis of 7 clinical trials comprising of 378 patients with hemorrhoids showed that fiber supplement had a consistent benefit of relieving symptom and minimizing risk of bleeding by approximately 50%[17]. Although there is relatively little information of the efficacy of dietary and lifestyle modification on the treatment of hemorrhoids, many physicians include advice on dietary and lifestyle modification as a part of conservative treatment of hemorrhoids and as a preventive measure. The advice usually includes increasing the intake of dietary fiber and oral fluid, having regular exercise, refraining from straining and reading on the toilet, and avoiding drug causing constipation or diarrhea.
The main goal of medical treatment is to control acute symptoms of hemorrhoids rather than to cure the underlying hemorrhoids. There are several modern drugs and traditional medicine used which are available in a variety of format including pill, suppository, cream and wipes. However, the published literature lacks strong evidence supporting the true efficacy of topical treatment for symptomatic hemorrhoids. For an oral preparation, flavonoids are the most common phlebotonic agent used for treating hemorrhoids[18]. It is apparent that flavonoids could increase vascular tone, reduce venous capacity, decrease capillary permeability, facilitate lymphatic drainage and has anti-inflammatory effects[2]. A large meta-analysis of phlebotonics for hemorrhoids in 2012 showed that phlebotonics had significant beneficial effects on bleeding, pruritus, discharge and overall symptom improvement. Phlebotonics also alleviated post-hemorrhoidectomy symptoms[19].
Many office-based procedures (such as rubber band ligation, injection sclerotherapy, infrared coagulation, cryotherapy, radiofrequency ablation and laser therapy) are effectively performed for grade I- II hemorrhoids and some cases of grade III hemorrhoids with or without local anesthesia. Among several office-based procedures, rubber band ligation (RBL) appeared to have the lowest incidence of recurrent symptom and the need for retreatment[20]. RBL is also the most popular non-surgical intervention for hemorrhoids performed by surgeons[21]. It is a relatively safe and painless procedure with minimal complication. However, RBL is contraindicated in patient with anticoagulants or bleeding disorder, and those with concurrent anorectal sepsis. With a technical note, the proper position of rubber band should be at the base of hemorrhoid bundle or over the bleeding site, but not too close to the dentate line. Vacuum suction ligator may offer clearer visualisation of hemorrhoids and more precise placement of banding when compared to a traditional forcep ligator[22]. Multiple sites and serial sessions of banding may be required for large internal hemorrhoids.
Surgical intervention is usually required in low-graded hemorrhoids refractory to non-surgical treatment, high-graded symptomatic hemorrhoids, and hemorrhoids with complication such as strangulation and thrombosis. An operation for hemorrhoids may be performed if patient has other concomitant anorectal conditions requiring surgery, or due to patient’s preference.
An ideal operation for hemorrhoids should remove internal and external component of hemorrhoids completely, have minimal postoperative pain and complication, demonstrate less recurrence, and are easy to learn and perform. The procedure could be cheap and cost-effective too. Unfortunately, none of the currently available operation achieves all the ideal conditions. So far, excisional hemorrhoidectomy is the mainstay operation for grade III-IV hemorrhoids and complicated hemorrhoids. Of note, closed (Ferguson) hemorrhoidectomy and open (Milligan-Morgan) hemorrhoidectomy were equally effective and safe[23,24], but the Ferguson method was superior to the Milligan-Morgan method in term of long time patient satisfaction and continence[25]. Nevertheless, both techniques may lead to severe postoperative pain[26]. In order to minimize or avoid post-hemorrhoidectomy pain, more recent approaches including Ligasure hemorrhoidectomy, doppler-guided hemorrhoidal artery ligation and stapled hemorrhoidopexy have been adopted into the surgical treatment of hemorrhoids. In addition, perioperative care for hemorrhoids has been significantly improved[1,27].
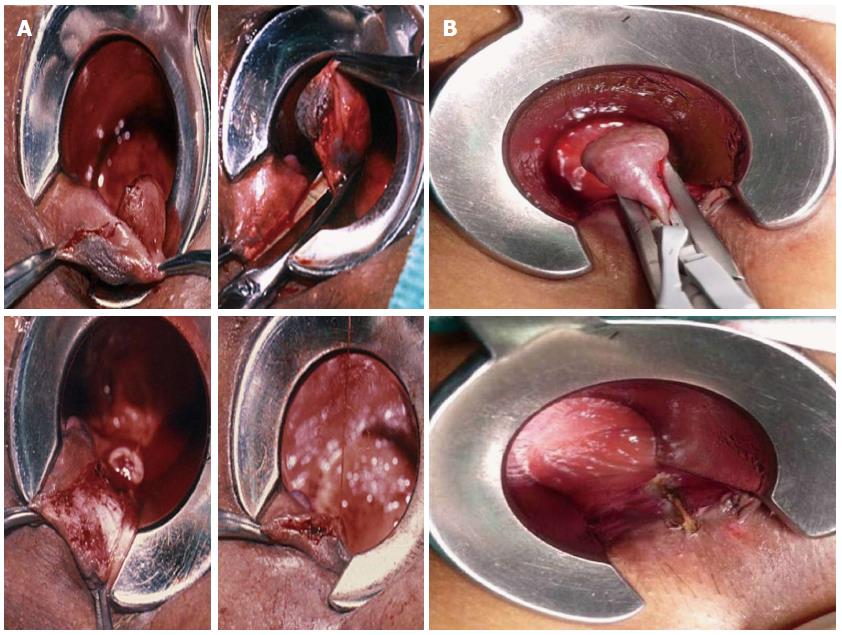
Surgical excision of hemorrhoids can be done by a variety of instrument such as a scalpel, scissors (Figure 2A), a cautery device, and more recently LigasureTM - a vessel sealing device (Figure 2B). A recent Cochrane Review demonstrates that Ligasure hemorrhoidectomy resulted in shorter operative time, less postoperative pain, and shorter convalescence period when compared to conventional hemorrhoidectomy[28]. Meanwhile, there was no significant difference in postoperative complications and long-term outcomes between the two techniques. Excisional hemorrhoidectomy can be performed safely in a day-case basis under the perianal infiltration of local anesthetics[29], or regional anesthesia, or general anesthesia. It is evident that some medications could decrease post-hemorrhoidectomy pain such as perioperative analgesia with oral non-steroidal anti-inflammatory drugs[30] and gabapentin[31], topical administration of sucralfate[32] or metronidazole[33], and postoperative administration of phlebotonic drugs[19].
Non-excisional operation for hemorrhoids includes doppler-guided hemorrhoidal artery ligation (DG-HAL) or known as transanal hemorrhoidal dearterialization (THD), and plication of hemorrhoids (or known as ligation anopexy or mucopexy). DG-HAL has been introduced into a surgical practice to cut off the blood supply to hemorrhoids without the need of hemorrhoid removal. It involves the surgical ligation of terminal branches of superior hemorrhoidal artery causing shrinkage of hemorrhoid bundles. Plication of hemorrhoids is often performed with DG-HAL to control the prolapse more effectively. However, the recurrence rate following DG-HAL was up to 60% for grade IV hemorrhoids. DG-HAL is therefore considered as one of the effective operations only for grade II-III hemorrhoids with a one-year recurrence rate of 10% for prolapse and 10% for bleeding[34]. Notably, DG-HAL is not a totally painless operation as approximately 20% of patients experienced postoperative pain especially during the defecation[34]. Meanwhile, a ligation anopexy or mucopexy was also demonstrated to be a good alternative to excisional hemorrhoidectomy for grade II-III hemorrhoids, with shorter operative time and lower postoperative pain[35]. Given the fact that there is the possibility of revascularization and recurrent prolapse, further studies on the long-term outcomes of non-excisional operations for hemorrhoids are needed.
Stapled hemorrhoidopexy, also known as a procedure for prolapse and hemorrhoids (PPH), is an alternative operation for treating advanced internal hemorrhoids. A circular staple device is used to excise a ring of redundant rectal mucosa just above hemorrhoid bundles - not hemorrhoids per se. By doing this, prolapsing hemorrhoids will be repositioning (hemorrhoidopexy) and shrinking (due to a partial interruption of blood supply to hemorrhoid plexus). A recent systematic review of 27 randomized controlled trials demonstrated that, compared with conventional hemorrhoidectomy, stapled hemorrhoidopexy had less pain, shorter operative time, and quicker patient’s recovery of patient, but a significantly higher rate of prolapse and reintervention for prolapse[36]. Interestingly, the latest meta-analysis comparing surgical outcomes between stapled hemorrhoidopexy and Ligasure hemorrhoidectomy in 2013 revealed that both surgical techniques were practically comparable - with a slightly favorable immediate postoperative results and technical advantages for Ligasure hemorrhoidectomy[37].
Given the fact that stapled hemorrhoidopexy did not offer any significant advantages over Ligasure hemorrhoidectomy[37] and it is a relatively expensive operation which may cause serious postoperative complications such as rectal stricture and rectal perforation[38] as well as severe chronic anal pain[39], stapled hemorrhoidopexy should be reserved for patients with circumferential prolapsing hemorrhoids and it must be performed by a well-trained surgeon[2].
Patients with acutely thrombosed or strangulated internal hemorrhoids usually present with severely painful and irreducible hemorrhoids. The incarcerated hemorrhoids may become necrotic and drain. This situation is quite difficult to treat particularly in a case of extensive strangulation or thrombosis (Figure 3A), or the presence of underlying circumferential prolapse of high-graded hemorrhoids. Manual reduction of the hemorrhoid masses, with or without intravenous analgesia or sedation, might help reducing pain and tissue congestion. Urgent hemorrhoidectomy is usually required in these circumstances. Unless the tissues are necrotic, mucosa and anoderm should be preserved as much as possible to prevent postoperative anal stricture. In expert hands, surgical outcomes of urgent hemorrhoidectomy were comparable to those of elective hemorrhoidectomy[40].
Acutely thrombosed external hemorrhoids often develop in patients with acute constipation, or those with a recent history of prolonged straining. A painful bluish-colored lump at the anal verge is a paramount finding (Figure 3B). The severity of pain is most intense within the first 24-48 h of onset. After that, the thrombosis will be gradually absorbed and patients will experience less pain. As a result, surgical removal of acute thrombus or excisional hemorrhoidectomy may be offered if patients experience severe pain especially within the first 48 h of onset. Otherwise, conservative measure will be exercised including pain control, warm sitz baths, and avoidance of constipation or straining. A resolving thrombosed external hemorrhoid could leave behind as a residual perianal skin tag -which may or may not require a subsequent excision.
Hemorrhoids are very common during pregnancy especially in the third trimester[41]. Acute crisis such as profound bleeding and irreducible prolapsing may be found in pregnant women with pre-existing hemorrhoids. Since hemorrhoids and its symptoms will gradually resolve after giving birth, the primary goal of treatment is to relief acute symptoms related to hemorrhoids - mostly by means of dietary and lifestyle modification. Kegel exercises, lying on left side, and avoidance of constipation could reduce the episode and severity of bleeding and prolapse. Fiber supplement, stool softener and mild laxatives are generally safe for pregnant women. Topical medication or oral phlebotonics may be used with special caution because the strong evidence of their safety and efficacy in pregnancy is lacking. In case of massive bleeding, anal packing could be a simple and useful maneuver. Hemorrhoidectomy is reserved in strangulated or extensively thrombosed hemorrhoids, and hemorrhoids with intractable bleeding.
In general any intervention or operation should be avoided, or performed with a careful consideration in immunocompromised patients because of an increases risk of anorectal sepsis and poor tissue healing in such cases[42]. A conservative measure is the mainstay for the treatment of hemorrhoids in this group of patients. If required, injection sclerotherapy appeared to be a better and safer alternative to banding and hemorrhoidectomy for treating bleeding hemorrhoids[43,44]. Antibiotic prophylaxis is always given before performing any intervention, even a minor office-based procedure, due to the possibility of bacteremia.
A clinician must differentiate bleeding hemorrhoids form bleeding anorectal varices because the latter can be managed by suture ligation along the course of varices, transjugular intrahepatic portosystemic shunt, or pharmacological treatment of portal hypertension[1]. Since a majority of bleeding hemorrhoids in such patients is not life threatening, conservative measure with the correction of any coagulopathy is a preferential initial approach. Of note, rubber band ligation is generally contraindicated in patients with advanced cirrhosis due to the risk of profound secondary bleeding following the procedure. Injection sclerotherapy is an effective and safe procedure for treating bleeding hemorrhoids in this situation. In a refractory case, suture ligation at the bleeder is advised. Hemorrhoidectomy is indicated when bleeding hemorrhoids are refractory to other approaches.
Anticoagulant or antiplatelet drugs may promote anorectal bleeding in patients with hemorrhoids and increase risk of bleeding after banding or surgery[45]. Unless the bleeding is persistent or profound, the discontinuity of antithrombotic drugs may be unnecessary because most of the bleeding episodes are self-limited and stop spontaneously. Conservative measure is therefore the mainstay treatment in these patients. Injection sclerotherapy is a preferential treatment for bleeding low-graded hemorrhoids refractory to medical treatment. Rubber band ligation is not recommended in patients with the current use of anticoagulant or antiplatelet drugs due to the risk of secondary bleeding. If banding or any form of surgery for hemorrhoids is scheduled, the cessation of anticoagulant or antiplatelet drugs about 5-7 d before and after the procedure is suggested[46].
To date, it is obvious that, apart from oral flavonoids-based phlebotonic drugs, currently available medication for hemorrhoids has no or limited beneficial effects on bleeding and prolapsing[19]. Since emerging evidence has suggested that perivascular inflammation, dysregulation of the vascular tone and vascular hyperplasia could play an important role in the development of hemorrhoids[2], the microcirculatory system of hemorrhoid tissue could be a potential and robust target for medical treatment. The combinations of vasoconstrictive and venoconstrictive agents, with or without anti-inflammatory drugs, might be a new pharmacological approach for hemorrhoids.
If an intervention, either office-based procedure or surgery - is indicated, evidence-based approaches must be exercised. Day-case operation or ambulatory surgery should be fully developed together with an effective program for peri-operative care[30]. Despite advances in office-based procedures and better surgical approaches, post-procedural pain and disease recurrence remain the most challenging problems in the treatment of hemorrhoids. Consequently, future researches and novel management of hemorrhoids may focus on how to minimize pain following a procedure and how to prevent recurrent hemorrhoids. Meanwhile, long-term results of newly or recently developed interventions are definitely required.
In conclusion, the better understanding of the pathophysiology of hemorrhoids would prompt the development of effective treatments for hemorrhoids. Preventive measures, by means of dietary and lifestyle modification, may be the best treatment of hemorrhoids. Once hemorrhoids develop, its treatment options mainly depend on the type and severity of hemorrhoids, patient’s preference and the expertise of physicians. Post-procedural pain and disease recurrence remain the most challenging problems in the treatment of hemorrhoids.
P- Reviewer: Li W, Peng JS, Rutegard J S- Editor: Yu J L- Editor: A E- Editor: Liu XM
| 1. | Lohsiriwat V. Approach to hemorrhoids. Curr Gastroenterol Rep. 2013;15:332. [PubMed] |
| 2. | Lohsiriwat V. Hemorrhoids: from basic pathophysiology to clinical management. World J Gastroenterol. 2012;18:2009-2017. [PubMed] |
| 3. | Thomson WH. The nature and cause of haemorrhoids. Proc R Soc Med. 1975;68:574-575. [PubMed] |
| 4. | Lee JH, Kim HE, Kang JH, Shin JY, Song YM. Factors associated with hemorrhoids in korean adults: korean national health and nutrition examination survey. Korean J Fam Med. 2014;35:227-236. [PubMed] |
| 5. | Riss S, Weiser FA, Schwameis K, Riss T, Mittlböck M, Steiner G, Stift A. The prevalence of hemorrhoids in adults. Int J Colorectal Dis. 2012;27:215-220. [PubMed] |
| 6. | Tucker H, George E, Barnett D, Longson C. NICE Technology Appraisal on Stapled Haemorrhoidopexy for the Treatment of Haemorrhoids. Ann R Coll Surg Engl. 2008;90:82-84. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (2)] |
| 8. | Rohde H, Christ H. [Haemorrhoids are too often assumed and treated. Survey of 548 patients with anal discomfort]. Dtsch Med Wochenschr. 2004;129:1965-1969. [PubMed] |
| 9. | Yeung TM, D’Souza ND. Quality analysis of patient information on surgical treatment of haemorrhoids on the internet. Ann R Coll Surg Engl. 2013;95:341-344. [PubMed] |
| 10. | Aigner F, Gruber H, Conrad F, Eder J, Wedel T, Zelger B, Engelhardt V, Lametschwandtner A, Wienert V, Böhler U. Revised morphology and hemodynamics of the anorectal vascular plexus: impact on the course of hemorrhoidal disease. Int J Colorectal Dis. 2009;24:105-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 70] [Article Influence: 4.4] [Reference Citation Analysis (1)] |
| 11. | Morgado PJ, Suárez JA, Gómez LG, Morgado PJ. Histoclinical basis for a new classification of hemorrhoidal disease. Dis Colon Rectum. 1988;31:474-480. [PubMed] |
| 12. | Chung YC, Hou YC, Pan AC. Endoglin (CD105) expression in the development of haemorrhoids. Eur J Clin Invest. 2004;34:107-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Corman ML, Gravié JF, Hager T, Loudon MA, Mascagni D, Nyström PO, Seow-Choen F, Abcarian H, Marcello P, Weiss E. Stapled haemorrhoidopexy: a consensus position paper by an international working party - indications, contra-indications and technique. Colorectal Dis. 2003;5:304-310. [PubMed] |
| 14. | Loder PB, Kamm MA, Nicholls RJ, Phillips RK. Haemorrhoids: pathology, pathophysiology and aetiology. Br J Surg. 1994;81:946-954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 199] [Article Influence: 6.4] [Reference Citation Analysis (5)] |
| 15. | Pigot F, Siproudhis L, Allaert FA. Risk factors associated with hemorrhoidal symptoms in specialized consultation. Gastroenterol Clin Biol. 2005;29:1270-1274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (2)] |
| 16. | Clinical Practice Committee, American Gastroenterological Association. American Gastroenterological Association medical position statement: Diagnosis and treatment of hemorrhoids. Gastroenterology. 2004;126:1461-1462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 17. | Alonso-Coello P, Mills E, Heels-Ansdell D, López-Yarto M, Zhou Q, Johanson JF, Guyatt G. Fiber for the treatment of hemorrhoids complications: a systematic review and meta-analysis. Am J Gastroenterol. 2006;101:181-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 78] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 18. | Misra MC. Drug treatment of haemorrhoids. Drugs. 2005;65:1481-1491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (4)] |
| 19. | Perera N, Liolitsa D, Iype S, Croxford A, Yassin M, Lang P, Ukaegbu O, van Issum C. Phlebotonics for haemorrhoids. Cochrane Database Syst Rev. 2012;8:CD004322. [PubMed] |
| 20. | MacRae HM, McLeod RS. Comparison of hemorrhoidal treatment modalities. A meta-analysis. Dis Colon Rectum. 1995;38:687-694. [PubMed] |
| 21. | Beattie GC, Wilson RG, Loudon MA. The contemporary management of haemorrhoids. Colorectal Dis. 2002;4:450-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Ramzisham AR, Sagap I, Nadeson S, Ali IM, Hasni MJ. Prospective randomized clinical trial on suction elastic band ligator versus forceps ligator in the treatment of haemorrhoids. Asian J Surg. 2005;28:241-245. [PubMed] |
| 23. | Ho YH, Buettner PG. Open compared with closed haemorrhoidectomy: meta-analysis of randomized controlled trials. Tech Coloproctol. 2007;11:135-143. [PubMed] |
| 24. | Arbman G, Krook H, Haapaniemi S. Closed vs. open hemorrhoidectomy--is there any difference? Dis Colon Rectum. 2000;43:31-34. [PubMed] |
| 25. | Jóhannsson HO, Påhlman L, Graf W. Randomized clinical trial of the effects on anal function of Milligan-Morgan versus Ferguson haemorrhoidectomy. Br J Surg. 2006;93:1208-1214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 26. | Yeo D, Tan KY. Hemorrhoidectomy - making sense of the surgical options. World J Gastroenterol. 2014;20:16976-16983. [PubMed] |
| 27. | Lohsiriwat V. Update on common anorectal diseases. Tech Coloproctol. 2014;18:87-88. [PubMed] |
| 28. | Nienhuijs S, de Hingh I. Conventional versus LigaSure hemorrhoidectomy for patients with symptomatic Hemorrhoids. Cochrane Database Syst Rev. 2009;CD006761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Lohsiriwat D, Lohsiriwat V. Outpatient hemorrhoidectomy under perianal anesthetics infiltration. J Med Assoc Thai. 2005;88:1821-1824. [PubMed] |
| 30. | Lohsiriwat V, Lohsiriwat D. Ambulatory anorectal surgery under perianal anesthetics infiltration: analysis of 222 cases. J Med Assoc Thai. 2007;90:278-281. [PubMed] |
| 31. | Poylin V, Quinn J, Messer K, Nagle D. Gabapentin significantly decreases posthemorrhoidectomy pain: a prospective study. Int J Colorectal Dis. 2014;29:1565-1569. [PubMed] |
| 32. | Gupta PJ, Heda PS, Kalaskar S, Tamaskar VP. Topical sucralfate decreases pain after hemorrhoidectomy and improves healing: a randomized, blinded, controlled study. Dis Colon Rectum. 2008;51:231-234. [PubMed] |
| 33. | Ala S, Saeedi M, Eshghi F, Mirzabeygi P. Topical metronidazole can reduce pain after surgery and pain on defecation in postoperative hemorrhoidectomy. Dis Colon Rectum. 2008;51:235-238. [PubMed] |
| 34. | Giordano P, Overton J, Madeddu F, Zaman S, Gravante G. Transanal hemorrhoidal dearterialization: a systematic review. Dis Colon Rectum. 2009;52:1665-1671. [PubMed] |
| 35. | Elshazly WG, Gazal AE, Madbouly K, Hussen A. Ligation anopexy versus hemorrhoidectomy in the treatment of second- and third-degree hemorrhoids. Tech Coloproctol. 2015;19:29-34. [PubMed] |
| 36. | Burch J, Epstein D, Sari AB, Weatherly H, Jayne D, Fox D, Woolacott N. Stapled haemorrhoidopexy for the treatment of haemorrhoids: a systematic review. Colorectal Dis. 2009;11:233-243; discussion 243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 57] [Article Influence: 3.6] [Reference Citation Analysis (1)] |
| 37. | Yang J, Cui PJ, Han HZ, Tong DN. Meta-analysis of stapled hemorrhoidopexy vs LigaSure hemorrhoidectomy. World J Gastroenterol. 2013;19:4799-4807. [PubMed] |
| 38. | Faucheron JL, Voirin D, Abba J. Rectal perforation with life-threatening peritonitis following stapled haemorrhoidopexy. Br J Surg. 2012;99:746-753. [PubMed] |
| 39. | Ielpo B, Venditti D, Balassone V, Favetta U, Buonomo O, Petrella G. Proctalgia as a late complication of stapled hemorrhoidectomy. Report of our case series. Int J Surg. 2010;8:648-652. [PubMed] |
| 40. | Pattana-arun J, Wesarachawit W, Tantiphlachiva K, Atithansakul P, Sahakitrungruang C, Rojanasakul A. A comparison of early postoperative results between urgent closed hemorrhoidectomy for prolapsed thrombosed hemorrhoids and elective closed hemorrhoidectomy. J Med Assoc Thai. 2009;92:1610-1615. [PubMed] |
| 41. | Gojnic M, Dugalic V, Papic M, Vidaković S, Milićević S, Pervulov M. The significance of detailed examination of hemorrhoids during pregnancy. Clin Exp Obstet Gynecol. 2005;32:183-184. [PubMed] |
| 42. | Morandi E, Merlini D, Salvaggio A, Foschi D, Trabucchi E. Prospective study of healing time after hemorrhoidectomy: influence of HIV infection, acquired immunodeficiency syndrome, and anal wound infection. Dis Colon Rectum. 1999;42:1140-1144. [PubMed] |
| 43. | Scaglia M, Delaini GG, Destefano I, Hultén L. Injection treatment of hemorrhoids in patients with acquired immunodeficiency syndrome. Dis Colon Rectum. 2001;44:401-404. [PubMed] |
| 44. | Buchmann P, Seefeld U. Rubber band ligation for piles can be disastrous in HIV-positive patients. Int J Colorectal Dis. 1989;4:57-58. [PubMed] |
| 45. | Nelson RS, Thorson AG. Risk of bleeding following hemorrhoidal banding in patients on antithrombotic therapy. Gastroenterol Clin Biol. 2009;33:463-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 46. | Mounsey AL, Halladay J, Sadiq TS. Hemorrhoids. Am Fam Physician. 2011;84:204-210. [PubMed] |