Published online Aug 14, 2015. doi: 10.3748/wjg.v21.i30.9228
Peer-review started: January 31, 2015
First decision: March 10, 2015
Revised: March 29, 2015
Accepted: May 2, 2015
Article in press: May 4, 2015
Published online: August 14, 2015
Processing time: 198 Days and 20.8 Hours
Pancreatic hemangiomas are a rare type of cystic tumor, with very few cases reported in the literature. Herein, we present the case of a 28-year-old woman who was admitted to our hospital for abdominal pain. A physical examination failed to reveal any abnormalities that could explain her symptoms. A contrast-enhanced computed tomography showed a multilocular cyst with moderately enhanced septa and fluid-fluid levels in the body and tail of the pancreas. A serous cystadenoma or pseudocyst of the pancreas was initially suspected, and the patient underwent a subtotal pancreatectomy and splenectomy. The pathologic diagnosis was a pancreatic hemangioma. This is the second case of pancreatic hemangioma with fluid-fluid levels reported in the literature. Upon imaging, the presentation of this tumor can resemble serous or mucinous cystadenomas, pseudocysts of the pancreas, and side-branch type intraductal papillary mucinous neoplasms. This report reviews the clinical symptoms, radiologic features, pathologic characteristics, differential diagnoses, and treatment of this rare lesion type.
Core tip: Pancreatic hemangioma is a rare benign tumor that is even more rare in adults. We report a case of pancreatic hemangioma in a 28-year-old woman. The tumor appeared as a multilocular cyst with septa and fluid-fluid levels in the body and tail of the pancreas. The septa were only moderately enhanced. This is the second reported case of fluid-fluid level in pancreatic hemangioma. Treatment of the pancreatic hemangioma in this case involved resection of the body and tail of the pancreas and concurrent splenectomy.
- Citation: Lu T, Yang C. Rare case of adult pancreatic hemangioma and review of the literature. World J Gastroenterol 2015; 21(30): 9228-9232
- URL: https://www.wjgnet.com/1007-9327/full/v21/i30/9228.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i30.9228
Visceral hemangiomas are common benign tumors that are typically found in the liver, spleen, and gastrointestinal tract. Pancreatic hemangiomas are very rare cystic lesions that are more common in childhood, with only a few cases in adults reported in the English language literature[1-13]. These lesions show strong contrast enhancement in arterial phase computed tomography (CT) scans. Herein, we report a rare case of an adult pancreatic hemangioma that presented as a multilocular cyst with septa and fluid-fluid levels and only moderate enhancement of the septa.
A 28-year-old woman was referred to our hospital for upper abdominal pain. Her medical history included gestational diabetes and a caesarean section. A physical examination failed to reveal any abnormality that would explain her symptoms. Blood test findings, including a complete blood count and liver function tests, were within normal ranges. Alpha-fetoprotein and carcinoembryonic antigen levels were also within normal ranges, however the tumor marker CA19-9 was slightly elevated at 35.42 U/mL.
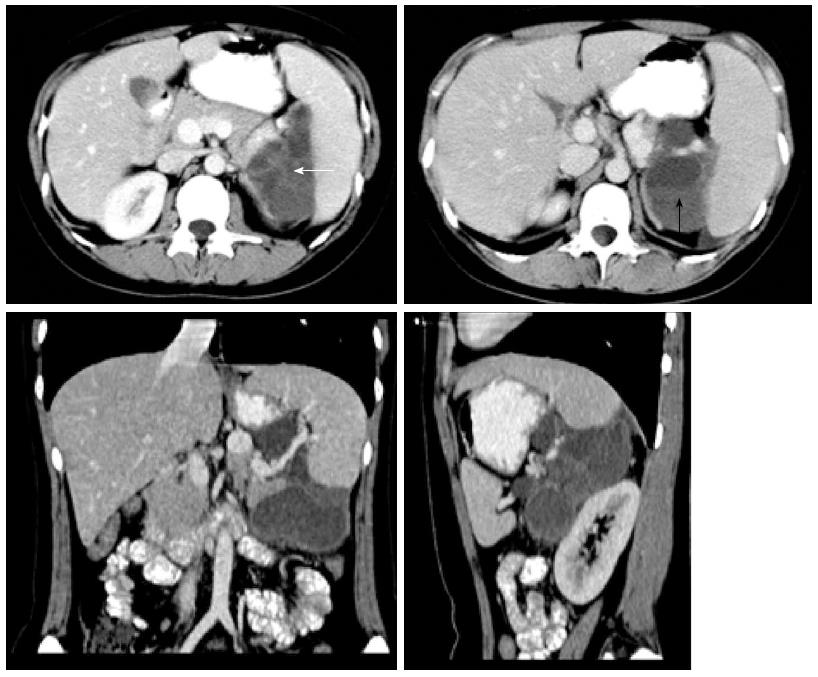
Contrast-enhanced CT of the abdomen showed a multilocular cyst with septa and fluid-fluid levels measuring 5.5 cm × 6.5 cm × 8.8 cm in the body and tail of the pancreas (Figure 1). The septa were moderately enhanced after injection of contrast agent. The tumor compressed the spleen forward and the left kidney backward. The left prerenal fascia was thickened. The findings indicated a cystic lesion with a possible solid component such as cystadenoma or pseudocyst of the pancreas with intracystic hemorrhage.
The patient underwent a subtotal pancreatectomy. During the laparotomy, a multilocular mass of approximately 8 cm × 10 cm was palpated at the body and tail of the pancreas. The tumor was tightly adhered to the splenic hilum; therefore, a splenectomy was performed, as preservation of the spleen was difficult. Gross pathologic examination revealed a reddish tumor composed of multilocular cysts containing intracystic hemorrhaged blood and formation of surrounding granulation tissue. The spleen was normal. The mass was diagnosed upon pathology as a pancreatic hemangioma. The postoperative course was uneventful and the patient was healthy without any signs of recurrence after the surgery; follow-up was for 2 years and 4 mo.
Vascular tumors of the pancreas, including lymphangioma, hemangioma, hemolymphangioma, hemangiopericytoma, hemangioblastoma and hemangiosarcoma, are rare cystic tumors that account for 0.1% of all pancreatic tumors[14]. Among the least common of these, pancreatic hemangiomas undergo three phases in children: proliferating phase, involuting phase, and involuted phase. When observed in adulthood, however, this tumor type can present as a fibrofatty residuum. Adult pancreatic hemangiomas appear as cysts lined by a single uniform layer of endothelial cells that may be immunoreactive for the endothelial markers CD31, CD34, and factor VIII-related antigen.
To our knowledge, only 13 other cases of pancreatic hemangioma have been reported in the literature (Table 1). These tumors are more commonly found in female patients (12/14; 85.71%), with an average age of presentation at 50.64 years (range: 23-79 years). The most common presenting symptom was abdominal or epigastric pain (8/14; 57.14%), though hematemesis, malaise, nausea, thrombocytopenia, dizziness, and palpitations were also noted. The tumors ranged in size from 3 cm to 20 cm, and were most frequently located in the pancreatic head (7/14; 50.00%), followed by body/tail (5/14; 35.71%), neck (1/14; 7.14%), and the whole pancreas (1/14; 7.14%).
| Case | Year | Ref. | Age/sex | Symptoms | Diagnostic imaging | Location | Size, cm | Treatment | IHC positivity |
| 1 | 1939 | Ranström[1] | 61/F | Found incidentally at autopsy | N/A | Head | 7 × 7 | N/A | N/A |
| 2 | 1961 | Ringoir et al[2] | 71/F | Hemetemesis, melena | Abdominal plain film, iv cholangiography | Head | 15 | Retrocolic gastroenterostomy, vagotomy | N/A |
| 3 | 1972 | Colardyn et al[3] | 42/M | AP, back pain | Abdominal plain film angiography | Body/tail | N/A | Fat-free diet, anticholinergics | N/A |
| 4 | 1985 | Mangin et al[4] | 62/F | Malaise, nausea, thrombocytopenia | US, ERCP, non-contrast CT | Head/body/tail | 20 × 7 | Laparotomy, observation | N/A |
| 5 | 1991 | Kobayashi et al[5] | 30/M | Abdominal distention | US, CT, MRI, angiography | Head | 20 | PD | N/A |
| 6 | 1991 | Dageförde et al[6] | 79/F | AP | US, ERCP, angiography | Body/tail junction | 6 × 3 | Observation | N/A |
| 7 | 2003 | Chang et al[7] | 70/F | EP | CT, angiography | Body/tail junction | 4.0 × 3.2 | Subtotal P | F8 |
| 8 | 2006 | Plank et al[8] | 36/M | AP | CT, MRI, intraoperative US | Head | 3 | Laparotomy | N/A |
| 9 | 2008 | Mundinger et al[9] | 45/F | EP radiating to back | CT, MRI | Head | 6.2 × 5.3 | Pylous-preserving PD | CD31, CD34 |
| 10 | 2011 | Weidenfeld et al[10] | 73/F | AP radiating to the left back | CT | Uncinate process | 5 × 4 × 3 | PD | CD31, CD34, F8 |
| 11 | 2011 | Lee et al[11] | 49/F | Dizziness, palpitation | US, CT, EUS | Neck | 5 | Central P, pancreatogastrostomy | CD34 |
| 12 | 2013 | Lu et al[12] | 23/F | Found during health examination | US, CT, MRI | Head | 5 × 4 × 3 | Subtotal P | N/A |
| 13 | 2014 | Naito et al[13] | 40/F | AP | CT, MRI | Body/tail | 10 | P | N/A |
| 14 | 2015 | Present case | 28/F | EP | CT | Body/tail | 10 × 8 | Subtotal P, splenectomy | N/A |
The majority of reported cases of pancreatic hemangioma were identified by CT (10/14; 71.43%) or ultrasonography (6/14; 42.86%), with magnetic resonance imaging (MRI) utilized in some of the more recent cases (5/14; 35.71%). By ultrasonography, the tumor appears as a hyperechogenic mass with slow or no blood flow, which is distinct from the abundant blood supply of malignant neoplasms. By CT and MRI, the tumor appears as a well-defined cystic mass, usually alveolar or multilocular, without dilation of the main pancreatic duct. Although hemangiomas are thought to show strong enhancement in the arterial phase of contrast-enhanced CT images, this phenomenon was not detected in most of the reported cases, including the present case. This may have been due to the fact that blood flow through cavernous vascular areas of cystic pancreatic tumors is slowed by neovascularization and arteriovenous shunting[5]. Additionally, the arterial phase signal intensity is influenced by the ratio of cystic to solid tumor tissue, which impacts the relative degree of vascularity[9]. As a result, a diagnosis of pancreatic hemangioma should not be ruled out solely based on poor arterial phase enhancement on contrast-enhanced CT. With MRI, pancreatic hemangiomas show low signal intensity on unenhanced T1-weighted images, and moderate to high signal intensity on T2-weighted images. In contrast, these lesions show only moderate gadolinium-enhancement with washout on delayed phase images, and no uptake of mangafodipir, with better delineation of the mass[8].
There are several differential diagnoses to consider for pancreatic hemangioma. Pseudocysts are also rarely enhanced upon imaging, but follow a history of pancreatitis. Serous cystadenomas appear as multicystic or lobular cystic lesions with septation, typically with central calcification within the fibrous stroma. Mucinous cystadenomas have a smooth shape, with or without septations, and peripheral eggshell calcification. Side-branch type intraductal papillary mucinous neoplasms appear as a pleomorphic cystic mass with communication between the lesion and the main pancreatic duct[12]. In the present case, the CT was a multilocular cystic mass with septa and thickening of the left prerenal fascia with no signs of adjacent structure infiltration or destruction of the pancreatic or common bile ducts. Thus, we initially considered a benign lesion, such as a serous cystadenoma or pseudocyst of the pancreas. However, after surgery, the tumor was confirmed to be hemangioma with surrounding inflammation, which may explain the thickening of the left prerenal fascia. The fluid-fluid level observed in our case is a very rare manifestation. Only one other case reported in the literature by Lu et al[12] described a pancreatic hemangioma with fluid-fluid levels, supposing it to be intracystic hemorrhage.
Treatments of pancreatic hemangioma vary, though a conservative therapy is recommended due to their benign nature. In children, the lesions tend to regress, thus follow-up with no treatment is advocated. Pancreatic hemangiomas in adults have been treated with surgical resection because of the risk of bleeding, as well as the fact that it can be difficult to differentiate them from epithelial tumors of the pancreas. Tumors located in the body and tail of the pancreas have been treated by resection of these areas with preservation of the spleen or by local resection. Local resection is also a suitable option for tumors in the head of the pancreas, rather than pancreaticoduodenectomy, as there is no increase in operative risks and complications and more pancreatic tissue is preserved. In the case presented here, the tumor was located in the body and tail of the pancreas; however, the characteristics of the lesion were not clear prior to surgery. Intraoperatively, the tumor was tightly adhered to the splenic hilum. Thus, a splenectomy was performed along with the resection of the body and tail of pancreas.
In conclusion, pancreatic hemangiomas are rare benign tumors that are distinct from other visceral hemangiomas. Pancreatic hemangioma should be considered as a differential diagnosis in cases of a multilocular cystic pancreatic mass without obvious enhancement and with fluid-fluid levels that may result from intracystic hemorrhage. In addition, these tumors lack malignant signs such as infiltration of adjacent structures and obstruction of the pancreatic and common bile ducts.
A 28-year-old woman with a history of gestational diabetes and caesarean section presented with abdominal pain.
Her physical examination failed to reveal any abnormalities to explain her symptoms.
Pseudocyst or serous cystadenoma.
Elevated CA19-9 (35.42 U/mL).
Contrast-enhanced computed tomography (CT) of the abdomen showed a multilocular cyst with septa and fluid-fluid levels measuring 5.5 cm × 6.5 cm × 8.8 cm in the body and tail of the pancreas.
The mass was diagnosed as a pancreatic hemangioma.
Subtotal pancreatectomy and splenectomy was performed.
Only 13 cases of pancreatic hemangioma have previously been reported in the literature.
Pancreatic hemangiomas are rare benign vascular tumors of the pancreas.
Pancreatic hemangioma should be considered as a differential diagnosis in cases of a multilocular cystic pancreatic mass without obvious enhancement and with fluid-fluid levels that may result from intracystic hemorrhage.
The authors describe one rare case of adult pancreatic hemangioma. CT of the tumor showed a multilocular cyst with septa and fluid-fluid levels. The article highlights the imaging and differential diagnoses of the disease.
P- Reviewer: Lorber A S- Editor: Qi Y L- Editor: A E- Editor: Zhang DN
| 1. | Ranström V. Haemangioma caverosum pancreatic. Zentralblatt für allgemeine pathologie und pathologische. 1939;73:33-35. |
| 2. | Ringoir S, Derom F, Colle R, Mortier G. Hemangioma of the pancreas. Report of a case. Gastroenterology. 1961;41:43-45. [PubMed] |
| 3. | Colardyn F, Elewaut A, Van de Velde E, Barbier F. Hemangioma of the pancreas. Tijdschr Gastroenterol. 1972;15:260-267. [PubMed] |
| 5. | Kobayashi H, Itoh T, Murata R, Tanabe M. Pancreatic cavernous hemangioma: CT, MRI, US, and angiography characteristics. Gastrointest Radiol. 1991;16:307-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Dageförde J, Gmelin E, Otte M. [Hemangioma of the pancreas]. Rofo. 1991;154:332-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Chang WT, Lee KT, Yang SF. Cavernous hemangioma of the pancreas: report of a case. Pancreas. 2003;26:310-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Plank C, Niederle B, Ba-Ssalamah A, Schimaa W. Pancreatic hemangioma: imaging features with contrast-enhanced CT and gadolinium- and mangafodipir- enhanced MRI. Eur J Radiol Ext. 2006;57:59-62. [RCA] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Mundinger GS, Gust S, Micchelli ST, Fishman EK, Hruban RH, Wolfgang CL. Adult pancreatic hemangioma: case report and literature review. Gastroenterol Res Pract. 2009;2009:839730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Weidenfeld J, Zakai BB, Faermann R, Barshack I, Aviel-Ronen S. Hemangioma of pancreas: a rare tumor of adulthood. Isr Med Assoc J. 2011;13:512-514. [PubMed] |
| 11. | Lee J, Raman K, Sachithanandan S. Pancreatic hemangioma mimicking a malignant pancreatic cyst. Gastrointest Endosc. 2011;73:174-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Lu ZH, Wu M. Unusual features in an adult pancreatic hemangioma: CT and MRI demonstration. Korean J Radiol. 2013;14:781-785. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Naito Y, Nishida N, Nakamura Y, Torii Y, Yoshikai H, Kawano H, Akiyama T, Sakai T, Taniwaki S, Tanaka M. Adult pancreatic hemangioma: A case report. Oncol Lett. 2014;8:642-644. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Le Borgne J, de Calan L, Partensky C. Cystadenomas and cystadenocarcinomas of the pancreas: a multiinstitutional retrospective study of 398 cases. French Surgical Association. Ann Surg. 1999;230:152-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 317] [Article Influence: 12.2] [Reference Citation Analysis (0)] |