Published online Jan 21, 2015. doi: 10.3748/wjg.v21.i3.997
Peer-review started: March 7, 2014
First decision: April 28, 2014
Revised: May 13, 2014
Accepted: October 15, 2014
Article in press: October 15, 2014
Published online: January 21, 2015
Processing time: 320 Days and 4.5 Hours
Abdominal surgery in cirrhotic patients with portal hypertension is associated with high incidence of disease and mortality. In these patients, oncological gastric procedures with lymph-nodes dissection show much higher complication rates than in normotensive portal vein patients. Thus, normalization of portal vein pressure may be a favorable determinant factor to reduce complications. We report a case of a patient with hepatitis C virus-related hepatic cirrhosis, esophageal varices, portal hypertension and gastric cancer. We demonstrated the efficacy of a preoperative trans-jugular porto-systemic shunt to perform oncological radical resection more safely. We retained preoperative the trans-jugular porto-systemic shunt in the patients with elevated portal pressure and gastric cancer to perform a gastrectomy more safely and to decrease morbidity and mortality of these cases.
Core tip: We suggest a preoperative trans-jugular porto-systemic shunt in patients with portal hypertension and gastric cancer to perform a safer gastrectomy. This procedure decreases intraoperational blood loss and postoperative morbidity. Moreover, the normalization of portal vein pressure permits the performance of an oncological nodes dissection. Finally, this technique may reduce perioperative mortality.
- Citation: Liverani A, Solinas L, Cesare TD, Velari L, Neri T, Cilurso F, Favi F, Bizzarri G. Preoperative trans-jugular porto-systemic shunt for oncological gastric surgery in a cirrhotic patient. World J Gastroenterol 2015; 21(3): 997-1000
- URL: https://www.wjgnet.com/1007-9327/full/v21/i3/997.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i3.997
Abdominal surgery in cirrhotic patients with portal hypertension is associated with high incidence of disease and mortality. In these patients, oncological gastric procedures with lymph-nodes dissection show a much higher rate of complications than in normotensive portal vein patients. Thus, normalization of portal vein pressure may be a favorable determinant factor to reduce complications.
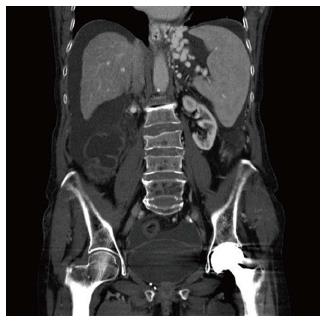
An 80-year-old female patient presented an endoscopic report of gastric neoplasia. Two months previously, she was subjected to an endoscopic oesophageal varices ligation because of variceal rupture (Figure 1). The Child-Pugh classification was B and portal pressure was up to 28 mmHg.
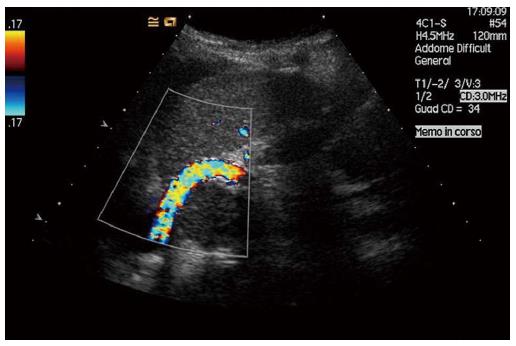
Preoperative oncological staging showed the absence of local or distant metastasis, and the patient was a candidate for radical resection. To reduce portal pressure and the risks of esophagogastric variceal rupture relapse, a preoperative transjugular intrahepatic portosystemic shunt (TIPSS) was proposed and successfully created. The right gastric vein was coiled. Normal portal pressure was reached, with values ranging from 12 to 15 mmHg.
Radiological procedure: the patient was placed a supine position in the angiographic suite. A rotation of the head to the left was required.
We used a spontaneous breathing general anesthesia for the radiological procedure, using a laryngeal mask, with a mixture of O2, N2O and isoflurane (1%-2%).
Puncture of the right internal jugular vein was performed with real-time sonography guidance using an 18-gauge needle.
A 0.035 degree angle Hydrophilic Coated Guidewires (Terumo Glidewire®, Tokyo, Japan) was inserted into the jugular vein, down to the inferior vena cava (IVC).
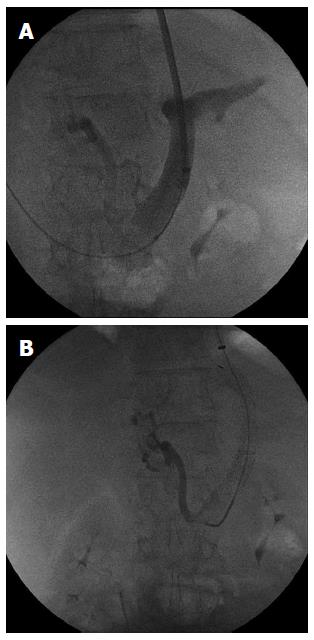
A 12-F introducer sheath was positioned in the right atrium and then into the IVC to measure the pressure. The hepatic vein was then catheterized directly using the curved metallic cannula of the TIPSS set (AngioDynamics®; Queensberry, NY, United States) and the guidewire (Terumo Glidewire®). The blood flow through the vein was sufficient to visualize the structure of the hepatic vein. Percutaneous puncture of portal vein was performed by placing a small introducer to permit portography (Figure 2).
The right hepatic vein was catheterized and the portal vein puncture was performed through the wall of the hepatic vein 1-3 cm from its origin. The catheter was turned anteriorly and advanced into the liver parenchyma for 4-5 cm. It was then slowly moved back and at the same time it was aspirated with a syringe. The correct puncture was checked via portography and a guidewire was introduced into the mesenteric vein.
Pressure was measured to evaluate the portosystemic differential pressure. A venogram was used to define the measure of the intrahepatic tract using a marked pigtail catheter.
Afterwards, an Amplatz Super Stiff™ Guidewire (Boston Scientific; Natick, MA, United States) was inserted into the splenic or mesenteric vein, and the intrahepatic tract was dilated using an 8 mm low-profile balloon (Wanda™, Boston Scientific; Natick, MA, United States).
The GORE® VIATORR® stent graft comprises a self-expanding nitinol endoprosthesis with a high radial strength and is covered with an ultrathin expanded polytetrafluoroethylene tube.
The 12-F introducer sheath was positioned into the portal system for 3 cm and moved back to have release of the uncovered tract within the portal vein. Once the endoprosthesis was positioned, the whole device was carefully removed until a resistance was felt, thus showing that the proximal tract of the device was positioned at the junction of the portal vein with the intrahepatic tract. The introducer was advanced largely upstream of the beginning of the endoprosthesis and, while positioning the system in place, the coated portion of the VIATORR® (60-20-10 mm, Figure 3) was released.
The endoprosthesis was then expanded, with the low-profile balloon catheter used previously. After complete deployment of the Viatorr, blood flow through the shunt was measured to check its function, and the mean atrial and portal pressures were evaluated to ascertain the hemodynamic significance of the procedure (PSG < 12 mmHg).
In conclusion, the right gastric vein, which fueled the massive variceal was embolized with coils. One month later, the patient was readmitted to the Surgical Department and a D-2 distal gastrectomy with a B2 gastrojejunal anastomosis was performed.
No intraoperative complications were observed and no transfusions were requested during the procedure. No postoperative bleeding or hepatic dysfunctions occurred, and the postoperative course was uneventful, except for delayed gastric stump empting with hospital discharge in 14 d.
A cirrhotic patient with portal hypertension as a candidate for an extrahepatic abdominal major procedure is a surgical challenge, especially if variceal bleeding is present. In these cases, morbidity and mortality is higher, ranging from 10% to 60%[1]. Gastric surgery in patients with portal hypertension is associated with mortality in excess of 10% and a morbidity rate of 25%[2].
The two major factors that contribute to higher operative mortality are propensity for bleeding and ascites, which increase the risk of infection. Less frequently hepatic insufficiency, hepato-renal syndrome or sepsis are determinants for postoperative complications, and often determine a fatal multiorgan failure[3].
Thus, it would seem important to achieve the best and most relevant preoperative control all correctable factors, such as ascites control, correction of coagulopathies, malnutrition and protein catabolism, amelioration of Child’s class or, finally, reduction of portal pressure.
In fact, a preoperative procedure to reduce or normalize portal pressure seems to decrease surgical risks, with lower incidence of complications and death[4-6].
At present, TIPSS is the preferred noninvasive procedure for treating portal hypertension and variceal bleeding[7-9]; however, its use preoperatively before extrahepatic abdominal surgery is rarely described (Figure 4).
In our patient, recent recurrent variceal bleeding had been referred and an oncological gastric procedure was mandatory.
We retained the preoperative TIPSS in the patients with elevated portal pressure and gastric cancer to perform a gastrectomy more safely, and to decrease the morbidity and mortality of these cases.
The patient had esophageal varices bleeding twice that were treated by endoscopy. In the last month the patient suffered dysphagia, epigastric pain and weight loss.
Gastroscopy showed an endoluminal hemorrhagic pyloric lesion of the stomach.
Histopathological examination after endoscopic biopsy showed gastric carcinoma.
Anemia, low dosage of albumin and coagulopathy.
A total body computed tomography scan showed the gastric lesion, esophageal varices, hepatic cirrhosis and ascites.
Trans-jugular porto-systemic shunt (TIPSS) and gastric resection was performed in two steps.
This case showed that preoperative TIPSS before gastric surgery reduced perioperative morbidity and mortality.
TIPSS is a useful and safe radiological procedure to treat portal vein hypertension. Cirrhotic patients undergoing oncological gastric surgery can be submitted to TIPSS 40-60 d before surgery. This procedure decreases intraoperative bleeding, morbidity and mortality.
P- Reviewer: Anand BS S- Editor: Gou SX L- Editor: Stewart G E- Editor: Zhang DN
| 1. | Guglielmi A, Girlanda R, Lombardo F, de Manzoni G, Frameglia M, Pelosi G, Baldin M. TIPS allowing for an endoscopic mucosal resection of early gastric cancer in a cirrhotic patient with severe hypertensive gastropathy: report of a case. Surg Today. 1999;29:902-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Catalano G, Urbani L, De Simone P, Morelli L, Coletti L, Cioni R, Matocci G, Mosca F, Filipponi F. Expanding indications for TIPSS: portal decompression before elective oncologic gastric surgery in cirrhotic patients. J Clin Gastroenterol. 2005;39:921-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Minicozzi A, Veraldi GF, Borzellino G. Minimally invasive treatment of portal hypertension, abdominal aortic aneurysm, and colon cancer: a case report. Surg Laparosc Endosc Percutan Tech. 2010;20:281-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Norton SA, Vickers J, Callaway MP, Alderson D. The role of preoperative TIPSS to facilitate curative gastric surgery. Cardiovasc Intervent Radiol. 2003;26:398-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Gil A, Martínez-Regueira F, Hernández-Lizoain JL, Pardo F, Olea JM, Bastarrika G, Cienfuegos JA, Bilbao JI. The role of transjugular intrahepatic portosystemic shunt prior to abdominal tumoral surgery in cirrhotic patients with portal hypertension. Eur J Surg Oncol. 2004;30:46-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 53] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Rumstadt B, Schilling D. The preoperative placement of transjugular intrahepatic portosystemic shunt for treatment of a patient with portal hypertension and gastric cancer. Hepatogastroenterology. 2008;55:303-304. [PubMed] |
| 7. | von Renteln D, Riecken B, Muehleisen H, Caca K. Transjugular intrahepatic portosystemic shunt and endoscopic submucosal dissection for treatment of early gastric cancer in a cirrhotic patient. Endoscopy. 2008;40 Suppl 2:E32-E33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Han SG, Han KJ, Cho HG, Gham CW, Choi CH, Hwang SY, Song SY. A case of successful treatment of stomal variceal bleeding with transjugular intrahepatic portosystemic shunt and coil embolization. J Korean Med Sci. 2007;22:583-587. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Palikhe M, Xue H, Jha RK, Li YC, Yuan J, Wang J, Zhang M. Changes in portal hemodynamics after TIPS in liver cirrhosis and portal hypertension. Scand J Gastroenterol. 2013;48:570-576. [PubMed] |