Published online Jan 21, 2015. doi: 10.3748/wjg.v21.i3.1040
Peer-review started: June 8, 2014
First decision: June 27, 2014
Revised: August 14, 2014
Accepted: September 18, 2014
Article in press: September 19, 2014
Published online: January 21, 2015
Processing time: 227 Days and 5 Hours
Paratyphoid fever can be complicated by massive lower gastrointestinal bleeding with ileocolonic ulcerations, which are commonly localized using colonoscopy. The most common manifestations include multiple, variable-sized, round or oval-shaped, punched-out ulcers. Occasionally, massive lower gastrointestinal bleeding can occur from erosion of blood vessels. We present a rare case of severe lower gastrointestinal bleeding due to paratyphoid A fever that was successfully controlled with hemoclippings. A 30-year-old man experienced high fever and hematochezia whose blood culture showed Salmonella paratyphi A. A complete colonoscopy was successfully performed up to the level of the terminal ileum, which showed multiple, shallow, ulcerated lesions over the entire terminal ileum. A bleeding vessel was seen in one of the ulcers, with overlaying blood clots. Endoscopic hemostasis was successfully performed with four pieces of endoclip and without immediate complication. This report highlights the use of colonoscopy and endoscopic therapy with endoclips for lower gastrointestinal bleeding, which should be considered before surgery.
Core tip: We present a case of severe lower gastrointestinal bleeding due to paratyphoid A fever that was well-controlled by hemoclippings. Although this type of complication is rare with paratyphoid A fever, clinicians should be cognizant of the possibility for intestinal bleeding from the ulcers in the ileum and proximal colon, which can appear as multiple, variable-sized, round or oval-shaped, punched-out ulcers. Colonoscopy and endoscopic therapy with endoclips should be considered before surgery.
- Citation: Wang H, Dong XL, Yu XM, Chung KS, Gao JP. Successful endoscopic hemoclipping of massive lower gastrointestinal bleeding from paratyphoid A fever. World J Gastroenterol 2015; 21(3): 1040-1043
- URL: https://www.wjgnet.com/1007-9327/full/v21/i3/1040.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i3.1040
Paratyphoid fever can be complicated by ileocolonic ulcerations and massive lower gastrointestinal bleeding (LGIB). The infectious organisms causing the condition localize to the Peyer’s patches of the terminal ileum. Hyperplasia and necrosis in these areas can result in multiple, variable-sized, round or oval-shaped, punched-out ulcers. Conservative therapy is commonly used for treating paratyphoid fever and gastrointestinal infections that are complicated by a minor episode of LGIB. However, a life-threatening hemorrhage can occur in 3%-10% of patients[1], which is associated with a high mortality unless specifically treated[2]. Although antimicrobial therapy is usually the mainstay treatment[3], surgical involvement is sometimes necessary[4]. Occasionally, a massive LGIB can occur from erosion of blood vessels. Colonoscopy has recently been advocated for localizing the site of bleeding among patients with typhoid fever, and favorable results have been found with endoscopic hemostasis without immediate complications[5,6]. However, diagnostic methodologies and treatment strategies for LGIB in patients with typhoid fever have not yet been established[4,7]. Here we present a rare case of severe LGIB due to paratyphoid A fever that was successfully controlled by endoscopic therapy with endoclips.
A 30-year-old man was admitted to our hospital with a six-day history of fever, poor appetite, and abdominal discomfort. He had no history of recent travel. The vital signs were normal except for a body temperature of 39.8 °C. The physical examination was unremarkable except for tenderness in the right lower quadrant. Abnormal laboratory values were as follows: alanine aminotransferase, 57 U/L; aspartate aminotransferase, 82 U/L; and white cell count, 3.64 × 109/L. Stool tests showed the presence of occult blood. A blood culture identified Salmonella paratyphi A that was sensitive to levofloxacin, and intravenous treatment was thus administered.
On the second day of hospitalization, the patient experienced hematochezia and dizziness. Hemoglobin levels dropped from 12.2 to 7.3 g/dL, and the patient was transfused with two units of packed red blood cells to maintain hemodynamic stability.
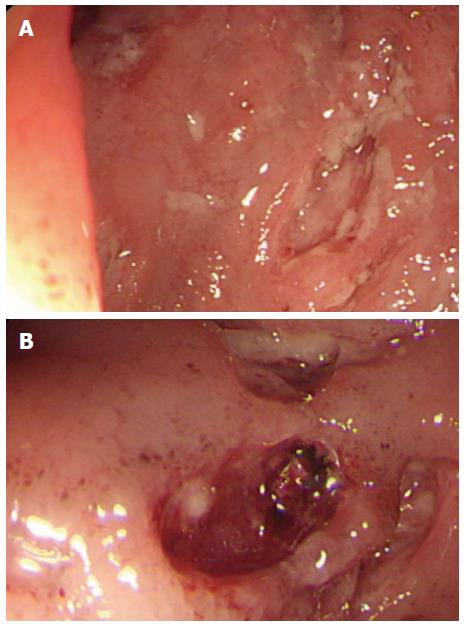
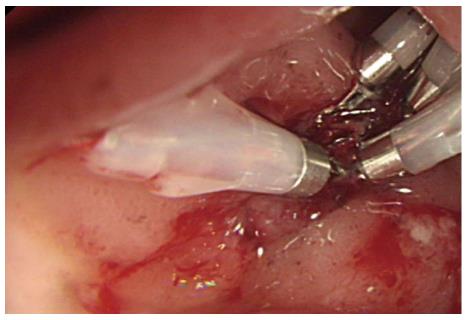
A complete colonoscopy was successfully performed up to the level of the terminal ileum. Multiple, shallow, ulcerated lesions were observed over the entire terminal ileum, and there was a bleeding vessel visible with overlaying blood clots in one of the ulcers (Figure 1). Four pieces of endoclip were successfully placed without complication (Figure 2), and the patient immediately became hemodynamically stable.
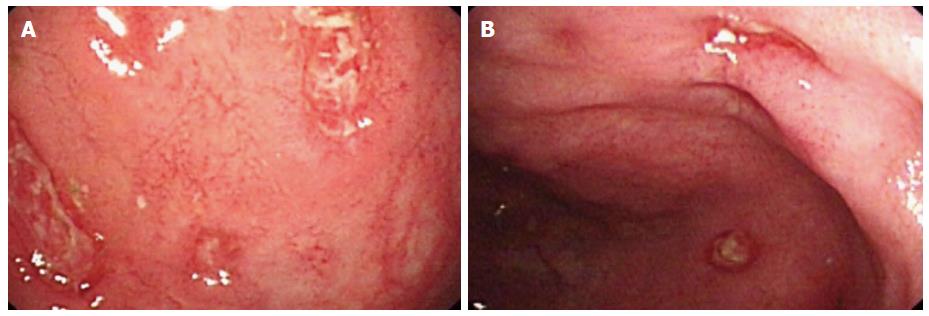
A ten-day course of levofloxacin (400 mg/d) was continued. The patient became afebrile and did not have subsequent bleeding. A colonoscopy was repeated after 12 d showing isolated ulcerations and normal intervening mucosa in the terminal ileum and cecum (Figure 3). The patient made a rapid recovery and was discharged after a total of 12 d in good health with a hemoglobin level of 9.7 g/dL. A colonoscopy was again performed 30 d after discharge, which showed complete resolution of the inflammation.
There are few articles concerning the management of typhoid or paratyphoid fever in patients with LGIB. Surgical intervention based on a selective angiography is the first choice of management[2]. When treating the patient in the present case, bleeding was stopped with hemoclippings, as it was not known during the colonoscopy that this was a case of paratyphoid A fever. Endoclips are effective for active vascular bleeding, non-bleeding visible vessels and adherent clots[8]. Yoshida et al[9] reported the control of massive colonic bleeding with hemoclippings in patients with ulcerative colitis. Hemoclippings have an advantage over epinephrine injections for preventing recurrent bleeding[10], without adding the risk of thermal injury over electrocoagulation[11].
To our knowledge, this is the first case of endoscopic hemoclipping hemostasis against massive LGIB in a patient with paratyphoid A fever. We advocate the use of hemoclipping with colonoscopy and endoscopic therapy in cases of LGIB with paratyphoid fever before radiologic or surgical intervention, particularly in patients that are hemodynamically compromised. In summary, clinicians should consider paratyphoid A fever among the other causes in patients with intestinal bleeding from ulcers in the ileum and proximal colon.
A 30-year-old man with massive lower gastrointestinal bleeding from paratyphoid A fever was successfully treated with endoscopic hemoclipping.
The patient was diagnosed with massive lower gastrointestinal bleeding from paratyphoid A fever.
Differential diagnoses were inflammatory bowel disease and intestinal tuberculosis.
The patient was diagnosed with paratyphoid A fever by blood culture and the following blood test results were obtained: alanine aminotransferase, 57 U/L; aspartate aminotransferase, 82 U/L; white cell count 3.64 × 109/L; hemoglobin level dropped from 12.2 to 7.3 g/dL.
A complete colonoscopy up to the level the terminal ileum revealed multiple shallow ulcer lesions and a bleeding vessel with overlaying blood clots in one of the ulcers in the terminal ileum.
The patient was treated with levofloxacin and endoscopic therapy in the form of endoclips.
Massive lower gastrointestinal bleeding from paratyphoid A fever is rare, with few cases of successful treatment using endoscopic hemoclipping reported in the literature.
Clinicians must be alert to typhoid fever in patients with intestinal bleeding from ulcers in the ileum and proximal colon and colonoscopy and endoscopic therapy in the form of endoclips should be considered before surgery.
The authors report an interesting case involving massive lower gastrointestinal bleeding from paratyphoid A fever that was successfully treated with endoscopic hemoclipping. The treatment option described in the article may be helpful for readers who have patients suffering the same condition.
P- Reviewer: Ciacci C S- Editor: Qi Y L- Editor: A E- Editor: Wang CH
| 1. | Gläser A. [Pathology and clinical aspects of bone neoplasms]. Zentralbl Chir. 1976;101:321-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 100] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Rubin CM, Fairhurst JJ. Life-threatening haemorrhage from typhoid fever. Br J Radiol. 1988;61:415-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Mandal BK. Modern treatment of typhoid fever. J Infect. 1991;22:1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Zuckerman MJ, Meza AD, Ho H, Menzies IS, Dudrey EF. Lower gastrointestinal bleed in a patient with typhoid fever. Am J Gastroenterol. 2000;95:843-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Kang JY. Endoscopic diagnosis of ileal ulceration in typhoid fever. Gastrointest Endosc. 1988;34:442-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Lee JH, Kim JJ, Jung JH, Lee SY, Bae MH, Kim YH, Son HJ, Rhee PL, Rhee JC. Colonoscopic manifestations of typhoid fever with lower gastrointestinal bleeding. Dig Liver Dis. 2004;36:141-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Sharma V, Prashar BS, Kanga AK, Thakur S. Typhoid fever--an update. Indian J Med Sci. 1998;52:163-165. [PubMed] |
| 8. | Saltzman JR, Strate LL, Di Sena V, Huang C, Merrifield B, Ookubo R, Carr-Locke DL. Prospective trial of endoscopic clips versus combination therapy in upper GI bleeding (PROTECCT--UGI bleeding). Am J Gastroenterol. 2005;100:1503-1508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Yoshida Y, Kawaguchi A, Mataki N, Matsuzaki K, Hokari R, Iwai A, Nagao S, Itoh K, Miura S. Endoscopic treatment of massive lower GI hemorrhage in two patients with ulcerative colitis. Gastrointest Endosc. 2001;54:779-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Odom KD. Recovering the ESWL patient. J Post Anesth Nurs. 1988;3:14-16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Chuttani R, Barkun A, Carpenter S, Chotiprasidhi P, Ginsberg GG, Hussain N, Liu J, Silverman W, Taitelbaum G, Petersen B. Endoscopic clip application devices. Gastrointest Endosc. 2006;63:746-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 70] [Article Influence: 3.7] [Reference Citation Analysis (0)] |