Published online Jan 21, 2015. doi: 10.3748/wjg.v21.i3.1028
Peer-review started: April 30, 2014
First decision: June 10, 2014
Revised: July 3, 2014
Accepted: September 5, 2014
Article in press: September 5, 2014
Published online: January 21, 2015
Processing time: 269 Days and 4.1 Hours
Focal nodular hyperplasia (FNH) is a benign hepatic tumor characterized by hepatocyte hyperplasia and a central stellate scar. The association of FNH with other hepatic lesions, such as adenomas, hemangiomas and hepatocellular carcinoma, has been previously reported, but FNH associated with another hepatic tumor is rare in infants. Here we report a case of FNH coexistent with hepatoblastoma in a 36-d-old girl. Computed tomography (CT) imaging showed an ill-delineated, inhomogeneous enhanced mass with a central star-like scar in the right lobe of the liver. The tumor showed early mild enhancement at the arterial phase (from 40HU without contrast to 52HU at the arterial phase), intense enhancement at the portal phase (87.7HU) and 98.1HU in the 3-min delay scan. A central scar in the tumor presented as low density on non-contrast CT and slightly enhanced at delayed contrast-enhanced scanning. This infant underwent surgical resection of the tumor. Histopathology demonstrated typical FNH coexistent with a focal hepatoblastoma, which showed epithelioid tumor cells separated by proliferated fibrous tissue.
Core tip: Focal nodular hyperplasia (FNH) is infrequent in infants, and hepatoblastoma is the most common primary malignant liver tumor in infants. The case reported here was a 36-d-old girl suffering from FNH coexistent with hepatoblastoma. Computed tomography imaging showed an ill-delineated, inhomogeneous enhanced mass with a central star-like scar in the right lobe of the liver. The patient underwent surgical resection of the tumor, and histopathology demonstrated typical FNH coexistent with a focal hepatoblastoma.
- Citation: Gong Y, Chen L, Qiao ZW, Ma YY. Focal nodular hyperplasia coexistent with hepatoblastoma in a 36-d-old infant. World J Gastroenterol 2015; 21(3): 1028-1031
- URL: https://www.wjgnet.com/1007-9327/full/v21/i3/1028.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i3.1028
Focal nodular hyperplasia (FNH) is a benign liver tumor, often asymptomatic and discovered incidentally[1,2]. Although FNH can be found at any age, it is rare in children, and comprises only 2% of all pediatric liver tumors[3]. There have been various reports on the association between FNH and other hepatic lesions, such as hepatocellular adenomas[4], hemangiomas[5], hepatocellular carcinoma[6] and metastases[7]. We herein report a case of FNH associated with hepatoblastoma in a 36-d-old female infant. To the best of our knowledge, only one case of FNH complicated by hepatoblastoma has been reported in a 4-year-old boy after treatment of stage IV neuroblastoma[8].
A 36-d-old girl presented to the hospital with a history of jaundice. Physical examination revealed a palpable solid mass fixed on the right quarter of the abdomen approximately 7 cm × 8 cm × 8 cm in diameter. The baby was full-term and delivered normally without asphyxia. Her mother had a history of progesterone administration before and in the early stages of pregnancy.
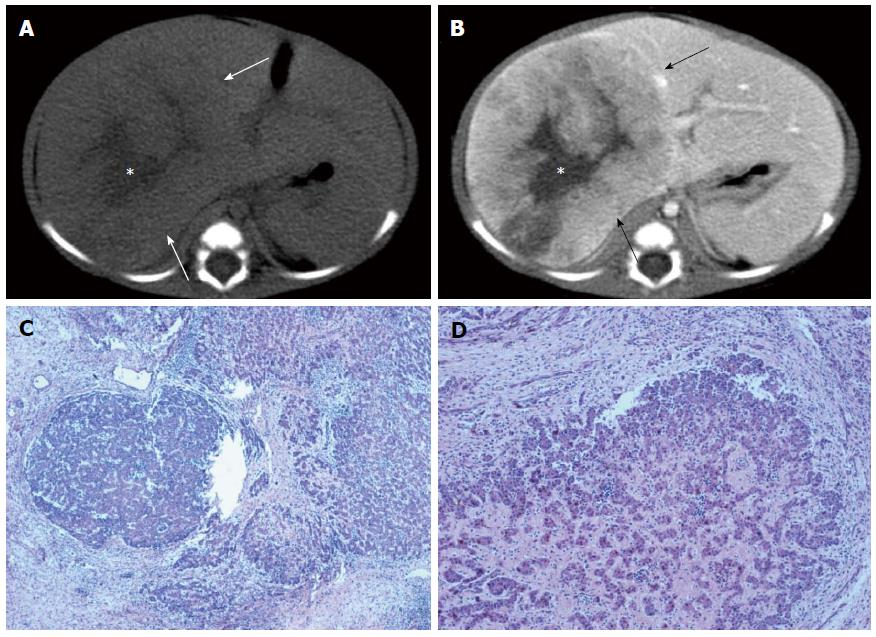
Sonography revealed a huge uneven hypo-echoic mass in the right lobe of the liver. Computed tomography (CT) imaging showed an ill-delineated, inhomogeneous enhanced mass with a central star-like scar in right lobe of the liver (Figure 1A, B). The tumor showed early mild enhancement at the arterial phase (from 40HU without contrast to 52HU at the arterial phase), intense enhancement at the portal phase (87.7HU) and 98.1HU in the 3-min delay scan, with slight enhancement of the central scar.
Laboratory evaluations included serum total bilirubin (TBIL) 93.1 μmol/L (normal 5.1-17.1 μmol/L), direct bilirubin (DBIL) 42.6 μmol/L (normal 0-6 μmol/L) and an alpha-fetoprotein (AFP) level of 74390 ng/mL (normal 0-77 ng/mL). Serum markers for both hepatitis B and hepatitis C virus were negative.
The infant underwent surgical resection of the tumor. The histopathology demonstrated FNH coexistent with hepatoblastoma (Figure 1C and D).
Up to 75% of pediatric liver tumors are malignant[9], and FNH constitutes 5% of benign liver tumors in children[10]. Although FNH is found at any age, even in newborn[11,12], it is rare in children, and two age peaks have been described, around 6 years and 18 years[10].
The pathogenesis of FNH is not well understood[2,13-15]. The most widely accepted theory is that FNH is the result of congenital or acquired vascular abnormalities[14,15]. Numerous studies have reported an increased incidence of FNH in long-term survivors of childhood malignancies or following hematopoietic stem cell transplantation[8,14-17]. It was thought that FNH was a complication of chemotherapy or radiation therapy in these patients[15].
The features of FNH on MRI and CT include homogeneity, arterial phase enhancement suggestive of hypervascularity, a lack of lesion capsule, and the presence of a central scar[15,18]. Ultrasound, CT, and especially MRI have proven effective at distinguishing FNH from other benign and malignant lesions in adults. In children, due to its infrequency and more variable imaging features, the accuracy of radiologic diagnosis of FNH is challenging. Atypical or variable radiologic features such as absence or non-enhancement of the central scar may be more common in children than adults[9]. Atypical features make it difficult to differentiate FNH from other benign or malignant lesions, including hepatic adenoma, hemangioma or infantile hemangioendothelioma, hepatoblastoma, and hepatocellular carcinoma.
Although there is no evidence in the literature of malignant degeneration of FNH, there are several reports of FNH occurring simultaneously with malignant neoplasms[6-9]. Gutweiler et al[8] described a case of hepatoblastoma concomitant with FNH after treatment of neuroblastoma in a 4-year-old boy. Similarly, Lautz et al[9] described a patient with hepatocellular carcinoma and concomitant FNH with a history of neuroblastoma. At present, most children with FNH should continue to undergo surgical resection due to symptoms, increasing size, or inability to confidently rule out malignancies[9].
A 36-d-old girl presented to the hospital with a history of jaundice.
Physical examination revealed a palpable solid mass fixed on the right quarter of the abdomen.
Hepatoblastoma, hemangioma or infantile hemangioendothelioma.
Serum level of total bilirubin was 93.1 umol/L, direct bilirubin was 42.6 μmol/L, and alpha-fetoprotein level was 74390 ng/mL.
Sonography and computed tomography (CT) imaging revealed a mass in the right lobe of the liver. The tumor showed early mild enhancement at the arterial phase, intense enhancement at the portal phase and slight enhancement of the central scar in the 3-min delay scan.
Histopathology demonstrated typical focal nodular hyperplasia (FNH) coexistent with a focal hepatoblastoma.
The infant underwent surgical resection of the tumor.
There are several reports of FNH occurring in children after treatment of malignant neoplasms. However, no cases of FNH and hepatoblastoma have been reported in infants.
Hepatoblastoma is more common in infants than FNH. The tumor in this infant showed a typical central scar on CT imaging, and histopathology confirmed FNH coexistent with a focal hepatoblastoma.
FNH coexistent with a focal hepatoblastoma is rare in infants. The dynamic CT images in this infant are helpful to diagnose FNH in the liver, but it is challenging to confirm a coexistent focal hepatoblastoma.
P- Reviewer: Chen Y, Otte JB, Tang KF S- Editor: Ma YJ L- Editor: A E- Editor: Zhang DN
| 1. | Finch MD, Crosbie JL, Currie E, Garden OJ. An 8-year experience of hepatic resection: indications and outcome. Br J Surg. 1998;85:315-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 30] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Nguyen BN, Fléjou JF, Terris B, Belghiti J, Degott C. Focal nodular hyperplasia of the liver: a comprehensive pathologic study of 305 lesions and recognition of new histologic forms. Am J Surg Pathol. 1999;23:1441-1454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 271] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 3. | Reymond D, Plaschkes J, Lüthy AR, Leibundgut K, Hirt A, Wagner HP. Focal nodular hyperplasia of the liver in children: review of follow-up and outcome. J Pediatr Surg. 1995;30:1590-1593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 57] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Nagorney DM. Benign hepatic tumors: focal nodular hyperplasia and hepatocellular adenoma. World J Surg. 1995;19:13-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 94] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Toshikuni N, Kawaguchi K, Miki H, Kihara Y, Sawayama T, Yamasaki S, Takano S, Minato T. Focal nodular hyperplasia coexistent with hemangioma and multiple cysts of the liver. J Gastroenterol. 2001;36:206-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Zhang SH, Cong WM, Wu MC. Focal nodular hyperplasia with concomitant hepatocellular carcinoma: a case report and clonal analysis. J Clin Pathol. 2004;57:556-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Nisar PJ, Zaitoun AM, Damera A, Hodi Z, Tierney GM, Beckingham IJ. Metastatic rectal adenocarcinoma to the liver associated with focal nodular hyperplasia. J Clin Pathol. 2002;55:967-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Gutweiler JR, Yu DC, Kim HB, Kozakewich HP, Marcus KJ, Shamberger RC, Weldon CB. Hepatoblastoma presenting with focal nodular hyperplasia after treatment of neuroblastoma. J Pediatr Surg. 2008;43:2297-2300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Lautz T, Tantemsapya N, Dzakovic A, Superina R. Focal nodular hyperplasia in children: clinical features and current management practice. J Pediatr Surg. 2010;45:1797-1803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Jha P, Chawla SC, Tavri S, Patel C, Gooding C, Daldrup-Link H. Pediatric liver tumors--a pictorial review. Eur Radiol. 2009;19:209-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | De Luca G, Zamparelli M, Fadda C, Martone A. Focal nodular hyperplasia of the liver in infancy: a case report. J Pediatr Surg. 2006;41:456-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Kang J, Choi HJ, Yu E, Hwang I, Kim YM, Cha HJ. A case report of fetal telangiectatic focal nodular hyperplasia. Pediatr Dev Pathol. 2007;10:416-417. [PubMed] [DOI] [Full Text] |
| 13. | Ndimbie OK, Goodman ZD, Chase RL, Ma CK, Lee MW. Hemangiomas with localized nodular proliferation of the liver. A suggestion on the pathogenesis of focal nodular hyperplasia. Am J Surg Pathol. 1990;14:142-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 31] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Kumagai H, Masuda T, Oikawa H, Endo K, Endo M, Takano T. Focal nodular hyperplasia of the liver: direct evidence of circulatory disturbances. J Gastroenterol Hepatol. 2000;15:1344-1347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Towbin AJ, Luo GG, Yin H, Mo JQ. Focal nodular hyperplasia in children, adolescents, and young adults. Pediatr Radiol. 2011;41:341-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 16. | Bouyn CI, Leclere J, Raimondo G, Le Pointe HD, Couanet D, Valteau-Couanet D, Hartmann O. Hepatic focal nodular hyperplasia in children previously treated for a solid tumor. Incidence, risk factors, and outcome. Cancer. 2003;97:3107-3113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 83] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 17. | Joyner BL, Levin TL, Goyal RK, Newman B. Focal nodular hyperplasia of the liver: a sequela of tumor therapy. Pediatr Radiol. 2005;35:1234-1239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 41] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Cheon JE, Kim WS, Kim IO, Jang JJ, Seo JK, Yeon KM. Radiological features of focal nodular hyperplasia of the liver in children. Pediatr Radiol. 1998;28:878-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |