Published online Jun 28, 2015. doi: 10.3748/wjg.v21.i24.7604
Peer-review started: December 19, 2014
First decision: January 22, 2015
Revised: February 12, 2015
Accepted: March 30, 2015
Article in press: March 31, 2015
Published online: June 28, 2015
Processing time: 192 Days and 16.7 Hours
Pancreatic tumors, with peri-pancreatic main vascular invasion, especially the superior mesenteric vein (SMV) or the portal vein, are very common. In some cases, vascular resection and reconstruction are required for complete resection of pancreatic tumors. However, the optimum surgical method for venous management is controversial. Resection of the SMV without reconstruction during surgery for pancreatic tumors is rarely reported. Here we present the case of a 58-year-old woman with a giant pancreatic mucinous cystadenoma adhering to the SMV, who underwent an en bloc tumor resection, including the main trunk of the SMV and the spleen. No venous reconstruction was performed during surgery. No ischemic changes occurred in the bowel. The presence of several well-developed collateral vessels was shown by 3-dimensional computed tomography examination. The patient had an uneventful postoperative period and was discharged. This case indicated that the main trunk of the SMV can be resected without venous reconstruction if adequate collateralization has formed.
Core tip: Pancreatic tumors, with peri-pancreatic main vascular invasion, especially the superior mesenteric vein (SMV) or the portal vein, are very common. In some cases, vascular resection and reconstruction are required for complete resection of pancreatic tumors. Resection of the SMV without reconstruction during surgery for pancreatic tumors is rarely reported. This report presents the case of a 58-year-old woman with a giant pancreatic mucinous cystadenoma adhering to the SMV, who underwent an en bloc tumor resection, including the main trunk of the SMV and the spleen. No vascular reconstruction was performed after resection of the main trunk of the SMV.
- Citation: Chen YT, Jiang QL, Zhu Z, Wang S, Zhao XM, Lan ZM, Che X, Zhang JW, Cui L, Tang XL, Wang CF. Resection of the main trunk of the superior mesenteric vein without reconstruction during surgery for giant pancreatic mucinous cystadenoma: A case report. World J Gastroenterol 2015; 21(24): 7604-7607
- URL: https://www.wjgnet.com/1007-9327/full/v21/i24/7604.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i24.7604
Tumor clearance during pancreatectomy can be facilitated by resection of the vessels involved, especially the superior mesenteric vein (SMV) or the portal vein (PV). To date, there is still controversy regarding management of the SMV segments either by ligation or repair during surgery[1]. Multiple reports have compared the outcome of simple ligation of the SMV to venous reconstruction. If the SMV is simply ligated, the collateral vessels will maintain sufficient blood flow through the portosystemic collaterals and inferior mesenteric vein. Until recently, all the reports on SMV ligation have referred to the distal end of this vessel. To the best of our knowledge, there is no report on the clinical course and consequences following resection of the main trunk of the SMV without reconstruction. Here we report a case of giant pancreatic mucinous cystadenoma with resection of the main trunk of the SMV without reconstruction and the postoperative course, as well as the radiographic findings following SMV resection.
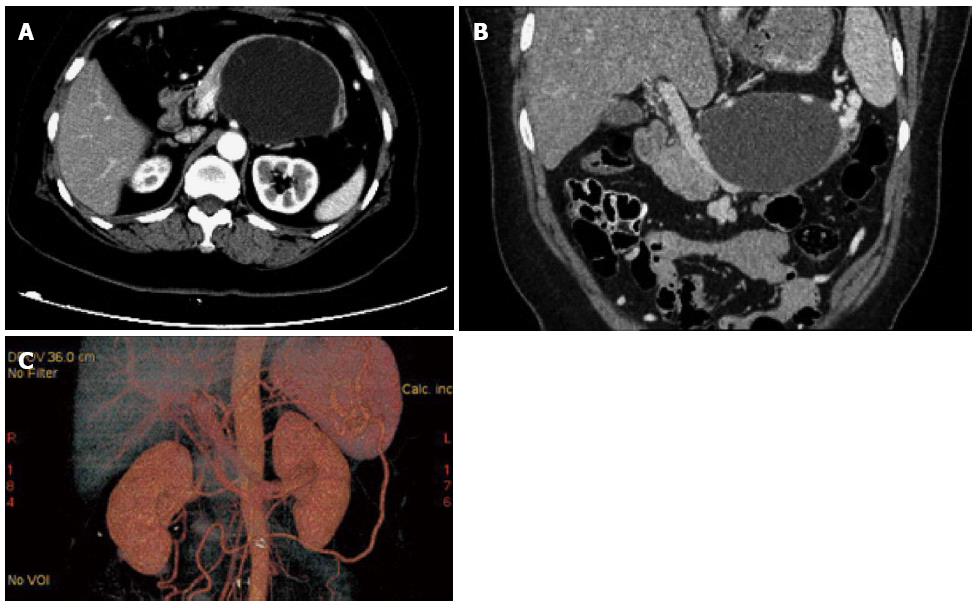
A 58-year-old woman was seen as an outpatient at our Gastropancreatic Unit in July 2012. She had not experienced abdominal pain and was admitted to our unit due to ultrasonographic detection of a cyst 8.3 cm in diameter located in the body-tail of the pancreas two weeks previously. On admission, physical examination revealed no major abnormalities and laboratory investigations were unremarkable. Tumor markers (CA 19-9, CEA, CA 125) were normal. Abdominal contrast-enhanced computed tomography was carried out and indicated a cystic tumor in the body-tail of the pancreas 9.5 cm in diameter (Figure 1A). Coronal multiplanar reformation (MPR) showed that the lesion was adhered to and constricted the main trunk of the SMV (Figure 1B). A preoperative 3-dimensional computed tomography (CT) scan showed the presence of several well-developed collateral vessels (Figure 1C).
At celiotomy, a giant cystic tumor was detected in the pancreatic body-tail. As the tumor was adhered to the main trunk of the SMV, the proximal and distal portions of the involved vein were clamped and en bloc tumor resection with the involved vein and spleen was performed. Unexpectedly, 50 min after SMV resection, no ischemic, edematous or necrosis changes were observed in the bowel. Thus, venous reconstruction was not performed after resection of the main trunk of the SMV.
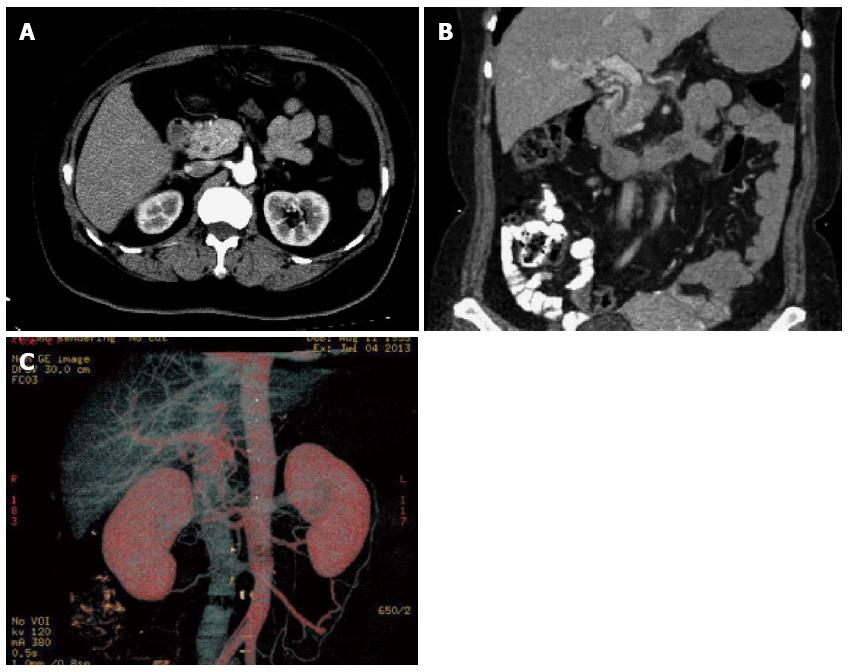
On postoperative day (POD) 5, the patient was allowed to drink water. On POD 7, the patient started a regular diet and consumed meals as guided. The patient had no abdominal complaints after surgery. In addition, there were no post-operative complications such as intra-abdominal bleeding or pancreatic fistula. On POD 14, no abnormal signs were observed on CT scanning, except in relation to the collateral vessels (Figure 2A-C). The patient was discharged on POD 20.
The final histopathological analysis revealed that the specimen consisted of a distal portion of the pancreas and the mass with the main trunk of the SMV, measuring 10.5 cm × 8.3 cm × 6.1 cm. Histology of the cyst wall showed mucinous cystadenoma of the pancreas. A negative margin was obtained. The patient was evaluated by CT scan within 4 wk after surgery and every 6 mo thereafter. The patient is currently being followed, with > 18 mo since surgery.
Cystic tumors of the pancreas are rare and comprise 10%-15% of pancreatic cystic masses[2]. In selected cases, giant cystic tumors may constrict the main vasculature around the pancreas, especially the SMV or PV. For the intact resection of tumors, resection of venous involvement and reconstruction are required. In 1951, Moore first reported the resection and reanastomosis of the SMV during radical pancreatoduodenectomy[3]. A subsequent study by Kim showed that most of the vein segments during pancreatic surgery can be reconstructed with end-to-end anastomosis or wedge resection with venoplasty. A great saphenous vein graft can be considered if the tension-free anastomosis or venoplasty without stenosis is doubtful[4]. Recent data from the trauma literature suggest that SMV ligation can occasionally be performed without catastrophic results due to abundant mesenteric venous collaterals[1], for some cases with thrombosis of the venous collaterals; SMV ligation was not well tolerated. A big challenge after SMV ligation is bowel complications, including ischemic and edema. If the vessel is ligated, a significant amount of bowel edema and venous engorgement may result. Significant impairment of venous return through the portal venous system may result in the development of systemic hypotension/splanchnic hypertension syndrome, which may lead to venous thrombosis, bowel ischemia, and necrosis[5]. Thus, Hans suggested that an SMV bypass would be a safe choice to reduce bowel edema. Do you need to include a reference for the work by Hans?
In the present case, no post-operative complications occurred after surgery. To the best of our knowledge, this is the first report of resection of the main trunk of the SMV without venous reconstruction, in which the clinical course and sequential changes in radiographic findings were documented. Katz and colleagues suggested that the ileal or jejunal branches of the SMV should be ligated at the time of elective surgery for pancreatic tumor; and bowel ischemia may be prevented by venous collateralization as long as the pancreatic head is left in situ and not resected[6]. Similarly, such collateralization may already be present if a degree of chronic venous obstruction is evident on preoperative imaging, and is further enhanced when the inferior mesenteric vein (IMV) enters the splenic vein or the SMV proximal (cephalad) to the site of SMV obstruction[7]. In our patient, it was suggested that the main trunk of the SMV may be resected without venous reconstruction if adequate collateralization was already present. Thus, careful preoperative radiographic examinations of collateralization and intraoperative observation of bowel ischemia are required in these cases.
In conclusion, we report the first case of SMV main trunk resection without reconstruction during surgery for a giant pancreatic mucinous cystadenoma in which the clinical course and sequential changes were documented. In the presence of adequate collateralization, the main trunk of the SMV can be resected without venous reconstruction in selected cases. A large scale analysis of this technique is required.
A 58-year-old woman with a giant pancreatic mucinous cystadenoma underwent an en bloc tumor resection, including the main trunk of the superior mesenteric vein (SMV) without reconstruction.
Cystic pancreatic lesion located in the body-tail of the pancreas adhering to and constricting the main trunk of the SMV.
Pancreatic adenocarcinoma, chronic pancreatitis, pancreatic neuroendocrine tumor.
Serum tumor markers such as carcinoma antigen (CA) 19-9, CA-125 and CEA were normal.
Contrast-enhanced computed tomography indicated a cystic tumor in the body-tail of the pancreas 9.5 cm in diameter.
Histology of the cyst wall showed mucinous cystadenoma of the pancreas.
The patient underwent an en bloc tumor resection of the giant mucinous cystadenoma with the involved vein and spleen.
The optimum surgical method for venous management in patients with pancreatic mucinous cystadenoma is controversial.
For selected cases, in the presence of adequate collateralization, the main trunk of the SMV can be resected without venous reconstruction.
Up to date, there is still a controversy on how to manage the SMV segments during the operation, to ligate or to repair? This report showed the first case of SMV main trunk resection without reconstruction during the surgery in which the clinical course and sequential changes were documented.
P- Reviewer: Malieckal A, Majewski M S- Editor: Qi Y L- Editor: Webster JR E- Editor: Liu XM
| 1. | Asensio JA, Petrone P, Garcia-Nuñez L, Healy M, Martin M, Kuncir E. Superior mesenteric venous injuries: to ligate or to repair remains the question. J Trauma. 2007;62:668-675; discussion 675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Hodgkinson DJ, ReMine WH, Weiland LH. Pancreatic cystadenoma. A clinicopathologic study of 45 cases. Arch Surg. 1978;113:512-519. [PubMed] |
| 3. | Moore GE, Sako Y, Thomas LB. Radical pancreatoduodenectomy with resection and reanastomosis of the superior mesenteric vein. Surgery. 1951;30:550-553. [PubMed] |
| 4. | Kim SM, Min SK, Park D, Min SI, Jang JY, Kim SW, Ha J, Kim SJ. Reconstruction of portal vein and superior mesenteric vein after extensive resection for pancreatic cancer. J Korean Surg Soc. 2013;84:346-352. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Asensio JA, Forno W, Roldán G, Petrone P, Rojo E, Ceballos J, Wang C, Costaglioli B, Romero J, Tillou A. Visceral vascular injuries. Surg Clin North Am. 2002;82:1-20, xix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 70] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Katz MH, Fleming JB, Pisters PW, Lee JE, Evans DB. Anatomy of the superior mesenteric vein with special reference to the surgical management of first-order branch involvement at pancreaticoduodenectomy. Ann Surg. 2008;248:1098-1102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Yamada Y, Mori H, Kiyosue H, Matsumoto S, Hori Y, Maeda T. CT assessment of the inferior peripancreatic veins: clinical significance. AJR Am J Roentgenol. 2000;174:677-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 55] [Article Influence: 2.2] [Reference Citation Analysis (0)] |