Published online Jun 21, 2015. doi: 10.3748/wjg.v21.i23.7272
Peer-review started: January 6, 2015
First decision: March 10, 2015
Revised: March 24, 2015
Accepted: May 4, 2015
Article in press: May 4, 2015
Published online: June 21, 2015
Processing time: 165 Days and 20.4 Hours
AIM: To analyze the prevalence, length and predictors of hospitalization in the biological era in the population-based inception cohort from Veszprem province.
METHODS: Data of 331 incident Crohn’s disease (CD) patients diagnosed between January 1, 2000 and December 31, 2010 were analyzed (median age at diagnosis: 28; IQR: 21-40 years). Both in- and outpatient records were collected and comprehensively reviewed.
RESULTS: Probabilities of first CD-related hospitalization and re-hospitalization were 32.3%, 45.5%, 53.7% and 13.6%, 23.9%, 29.8%, respectively after one, three and five years of follow-up in Kaplan-Meier analysis. First-year hospitalizations were related to diagnostic procedures (37%), surgery or disease activity (27% and 21%). Non-inflammatory disease behavior at diagnosis (HR = 1.32, P = 0.001) and perianal disease (HR = 1.47, P = 0.04) were associated with time to first CD-related hospitalization, while disease behavior change (HR = 2.38, P = 0.002) and need for steroids (HR = 3.14, P = 0.003) were associated with time to first re-hospitalization in multivariate analyses. Early CD-related hospitalization (within the year of diagnosis) was independently associated with need for immunosuppressives (OR = 2.08, P = 0.001) and need for surgeries (OR = 7.25, P < 0.001) during the disease course.
CONCLUSION: Hospitalization and re-hospitalization rates are still high in this cohort, especially during the first-year after the diagnosis. Non-inflammatory disease behavior at diagnosis was identified as the pivotal predictive factor of both hospitalization and re-hospitalization.
Core tip: Recent data on hospitalization rates in Crohn’s disease (CD) are lacking from population-based studies. In the present study our aim was to analyze the prevalence, cause and predictors of hospitalization and re-hospitalization in the population-based inception cohort from Veszprem province. Relatively high rates of CD-related hospitalizations and re-hospitalizations were found in our cohort, especially during the first year after the diagnosis. Non-inflammatory disease behavior at diagnosis, behavior change in patients with initial B1 behavior, perianal disease and total AZA and anti-TNF exposure was associated with the time to first CD-related hospitalization. Early CD-related hospitalization was associated with non-inflammatory disease behavior, perianal or internal fistulizing disease, need for immunosuppressives and need for surgeries during the disease course.
- Citation: Golovics PA, Lakatos L, Mandel MD, Lovasz BD, Vegh Z, Kurti Z, Szita I, Kiss LS, Pandur T, Lakatos PL. Prevalence and predictors of hospitalization in Crohn’s disease in a prospective population-based inception cohort from 2000-2012. World J Gastroenterol 2015; 21(23): 7272-7280
- URL: https://www.wjgnet.com/1007-9327/full/v21/i23/7272.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i23.7272
Inflammatory bowel diseases (IBD) are chronic, progressive inflammatory diseases leading to disability. Crohn’s disease (CD) has a variable course; the majority of patients experience multiple relapses, while 25% experience chronic continuous symptoms and eventually developing complications necessitating hospitalization or surgery[1]. Crohn’s disease treated mostly in the outpatient setting; the need for hospitalization is regarded as an important outcome and a surrogate marker of disease severity. Both medical and surgical hospitalization events contribute significantly to the cost burden of the disease[2].
Relatively limited data are available on the hospitalization or re-hospitalization rates in IBD from in population-based cohorts. In a recent meta-analysis published in 2012, authors summarized the hospitalization and surgery rates published from population-based cohorts[3]. The majority of studies were published before the biological era and the concomitant paradigm shift in patient management including early stratification, tight monitoring, and tailored treatment strategy[4]. Reported hospitalization rates were high, ranging between 25% and 83% within five years of diagnosis, with the highest rate in the year following diagnosis. There was a significant geographic variation and a trend toward decreasing surgery rates. Surgery rates varied from 10% to 35% in the first year, and between 18%-59% and 29%-61% after 5 and 10 years, respectively. In addition, predictors for first hospitalization - including markers of complicated disease; location (upper GI, ileocolonic, small bowel), complicated disease behavior, age at onset, and gender - were hardly studied[5,6].
In recent years, a significant emphasis was placed on early patient stratification based upon the identification of predictive factors[7]. Phenotypic classification of Crohn’s disease plays an important role in determining treatment methodology, as it generally assists in predicting the likely clinical course[8,9]. The complex evaluation of clinical presentation, endoscopic findings, fecal, serological, and routine laboratory tests - as well as early treatment factors - is recommended. For example, in a landmark paper by Beaugerie et al[7], initial requirements for steroid use (OR = 3.1), an age below 40 years (OR = 2.1), and the presence of perianal disease (OR = 1.8) were associated with the development of disability. However, it is not clear if a need for early hospitalization should be regarded as an independent marker of later disease course or only a marker of disease severity.
Therefore, the aim of the present study was to prospectively analyze the prevalence, length, cause, and predictors of hospitalizations and re-hospitalizations in a population-based inception cohort from Veszprem province in the biological era, in patients diagnosed between January 1, 2000 and December 31, 2010, with follow-up until December 31, 2012. In addition, our aim was to study if early hospitalization was associated with the later disease course or treatment algorithm.
Three hundred thirty-one incident CD patients (M/F: 176/155, median age at diagnosis: 28 years; IQR 21-40 years, median follow-up: 6 years; IQR 2-9 years) diagnosed between January 1, 2000 and December 31, 2010 were included in this study. Both in- and outpatient records were collected from the Veszprem province database and comprehensively reviewed. The clinical characteristics of the patients are presented in Table 1.
| CD | n = 331 |
| Males | 176 (53.2) |
| Age at presentation (yr) | 28; IQR 21-40 |
| Follow-up (yr) | 6; IQR: 2-9 |
| Familial IBD | 59 (17.8) |
| Location | |
| L1 | 115 (34.7) |
| L2 | 105 (31.7) |
| L3 | 108 (32.6) |
| L4 only | 4 (0.9) |
| Behavior at diagnosis | |
| B1 | 182 (55.0) |
| B2 | 66 (19.9) |
| B3 | 83 (25.1) |
| Perianal disease | 59 (17.8) |
| Arthritis | 85 (25.7) |
| Ocular | 12 (3.6) |
| Cutaneous | 29 (8.8) |
| Steroid use | 194 (58.6) |
| Azathioprine use | 197 (59.5) |
| Biological use | 27 (8.2) |
| Smoking habits at diagnosis | |
| No | 147 (44.4) |
| Ex | 46 (13.9) |
| Yes | 138 (41.7) |
A more detailed description of our data collection method, case ascertainment, geographical and socioeconomic background of the province, and the Veszprem Province IBD Group was published in our previous epidemiological studies[10,11].
Diagnosis was based on the Lennard-Jones Criteria[12]. The disease phenotype (age at onset, duration, location, and behavior) was determined according to the Vienna and Montreal Classifications (perianal disease was from the beginning separately registered and cases diagnosed before 2005 were reclassified according to the Montreal system in 2005)[13]. Medical records, including data regarding the presence of major extraintestinal manifestations (EIM), previous frequency of flare-ups (frequent flare-up: > 1 clinical relapse/year[14]), previous surgical procedures (resections or perianal procedures), the presence of familial IBD, smoking habits, and perianal involvement, were determined by a thorough review of the patients’ medical charts, which had been collected in a uniform format. Medical therapy (steroid, immunosuppressive, or biological therapy) was registered with the starting date of the first prescription. Biological therapy was first approved (infliximab) in the inpatient setting in 1998, while adalimumab was registered in 2008. The reimbursement of biologicals has changed, and anti-TNFs are now approved for outpatient use.
All-cause and IBD-related hospitalization events (including medical-surgical complications) were registered throughout the disease course. Clinical, laboratory data, drug use, hospitalizations - including surgeries - were captured prospectively in all patients from the time of the diagnosis. In referral patients, disease phenotype, course, and hospitalization events were captured retrospectively at the time of the referral visit and prospectively thereafter.
Definitions: Major surgical events were defined as major esophageal, stomach, and duodenum resections, major intestinal and rectal resections, laparotomy, extensive gastrointestinal procedures, and gastrostomy, ileostomy and colostomy procedures, while minor surgeries were defined as perianal fistula drainage, fistulectomy, and abscess drainage. IBD-related hospitalizations included medical or surgical hospitalizations related to disease flare. Other events and patients hospitalized solely for diagnostic purposes (end not due to severe clinical activity) were excluded from the prediction analysis when we assessed the predictive potential of the importance of early hospitalizations. Disease behavior change was defined as a change from non-stricturing, non-penetrating (B1) to either stricturing (B2) or penetrating (B3) disease.
The central coordination and database management was completed at the 1st Department of Internal Medicine, Semmelweis University (by PLL). The study was approved by the Semmelweis University Regional and Institutional Committee of Science and Research Ethics and by the Csolnoky F. Province Hospital Institutional Committee of Science and Research Ethics and written informed consent was obtained from all patients prior to enrollment.
Variables were tested for normality by Shapiro Wilk’s W-test. The χ2-test and χ2-test with Yates correction, McNemar test, and logistic regression analysis were used to assess the association between categorical variables. Odds ratios (OR) were calculated. Variables with a P < 0.2 in univariate analysis were included in multivariate testing with anti-TNF type and gender added arbitrarily. Cox regression analysis was used for survival analysis. Results for continuous variables are expressed as median (interquartile range, IQR) unless otherwise stated. Peter L Lakatos performed all statistical analysis and statistical methods were reviewed by a biostatistician (Dr Peter Vargha, Semmelweis University). For statistical analysis, SPSS® 20.0 (SPSS Inc., Chicago, IL) was used. A P value < 0.05 was considered significant.
The clinical characteristics of the patients are summarized in Table 1. The ileal, colonic and ileocolonic localization rate was nearly equal; close to two-thirds of patients had inflammatory disease behavior, while the perianal involvement was 17.8%. During the median six-year follow-up, total steroid and AZA exposure was approximately 60%, and just fewer than 10% of patients were exposed to biologicals.
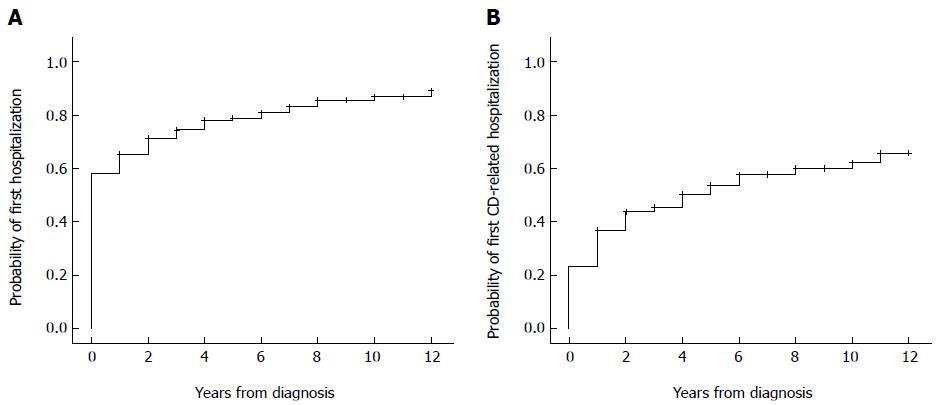
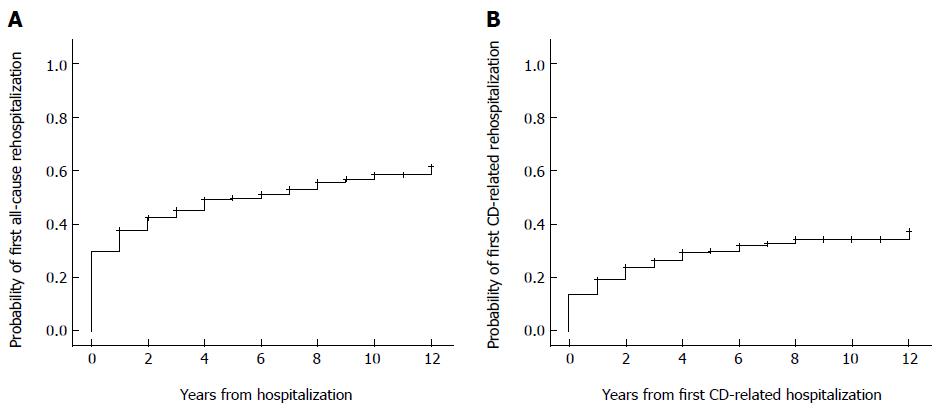
The probability of first all-cause and IBD-related hospitalization was 58%/32.3%, 74.4%/45.5% and 78.9%/53.7% after one, three, and five years of follow-up in a Kaplan-Meier analysis (Figure 1). The probability of hospitalization due to major surgery was 18.7%, 27.9% and 35.9% after one, three, and five years of follow-up. The probability of the first all-cause and IBD-related re-hospitalization was 29.6%/13.6%, 32.5%/23.9% and 49.7%/29.8% after one, three and five years (Figure 2).
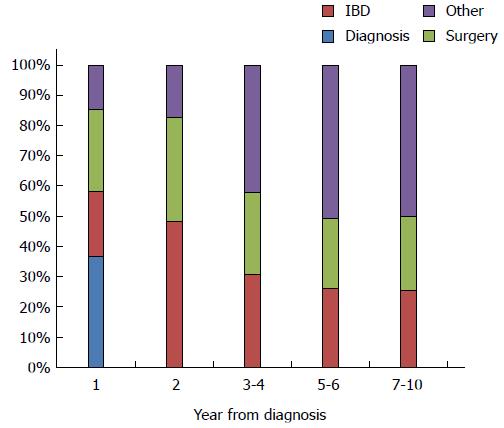
The main reasons for hospitalization in the first years were diagnostic procedures (37%), IBD-related surgery (27.2%), and disease activity (21.1%) (Figure 3). The relative frequency of surgery-related hospitalizations remained stable (23%-27% in years 1-10), while the proportion of non-IBD related hospital admissions increased after year three.
The mean duration of hospital admissions was 248 d per 100 patient-years follow-up for diagnostic procedures, 196, 300, 82, and 161 d per 100 patient-years follow-up for IBD-related medical, major-, and minor-surgical hospitalizations, and IBD-unrelated hospitalization events within one year of diagnosis. Corresponding rates were 33, 48, 13, and 21 d, and 58, 51, 5, and 57 d per 100 patient-years follow-up for CD-related medical, major-, minor-surgical hospitalizations, and IBD-unrelated events two and three to four years after the diagnosis.
Non-inflammatory disease behavior at diagnosis (PLogRank < 0.001, HR = 1.38, 95%CI: 1.18-1.61, P < 0.001), behavior change in patients with initial B1 behavior (PLogRank < 0.001, HR = 2.91, 95%CI: 1.84-4.61, P < 0.001), perianal disease (PLogRank < 0.001, HR = 1.80, 95%CI: 1.27-2.55, P = 0.001), total AZA and anti-TNF exposure (PLogRank = 0.038, HR = 1.36, 95%CI: 0.99-1.86, P = 0.059 and PLogRank = 0.017, HR = 1.69, 95%CI: 1.04-2.72, P = 0.033) but not gender, age at diagnosis, era of diagnosis (2000-2005 vs 2006-2010), smoking, and steroid exposure were significantly associated with time to first CD-related hospitalization (after excluding cases hospitalized for diagnosis) in a Kaplan-Meier and Cox-regression analysis. Non-inflammatory disease behavior at diagnosis (HR = 1.32, 95%CI: 1.11-1.55, P = 0.001), perianal disease (HR = 1.47, 95%CI: 1.02-2.12, P = 0.04) and disease behavior change (HR = 2.97, 95%CI: 1.78-4.96, P < 0.001) were associated with time to first CD-related hospitalization in multiple Cox-regression analysis.
Phenotype change from B1 (PLogRank < 0.001, HR = 2.93, 95%CI: 1.72-4.97, P < 0.001), arthritis (PLogRank = 0.02, HR = 1.58, 95%CI: 1.04-2.38, P = 0.03), need for steroids (PLogRank < 0.001, HR = 2.55, 95%CI: 1.60-4.07, P < 0.001) and total AZA and anti-TNF exposure (PLogRank < 0.001, HR = 2.45, 95%CI: 1.54-3.89, P < 0.001 and PLogRank = 0.03, HR = 1.83, 95%CI: 1.02-3.29, P = 0.041), but not gender, age at diagnosis, era of diagnosis (2000-2005 vs 2006-2010), or smoking were associated with time to first CD-related re-hospitalization in a Kaplan-Meier and Cox-regression analysis. Behavior change from B1 (HR = 2.38, 95%CI: 1.36-4.16, P = 0.002), and need for steroids (HR = 3.14, 95%CI: 1.46-6.74, P = 0.003) were associated with time to first CD-related hospitalization in multiple Cox-regression analyses.
Early IBD-related hospitalization was associated with age at onset according to the Montreal classification (P = 0.026), behavior (P < 0.001), non-inflammatory disease behavior at diagnosis (OR = 3.19, 95%CI: 1.95-5.22, P < 0.001), development of perianal (OR = 2.35, 95%CI: 1.19-4.64, P = 0.01) and/or internal fistulizing disease (OR = 3.82, 95%CI: 1.56-9.34, P = 0.002), presence of anemia (OR = 1.83, 95%CI: 1.15-2.86, P = 0.01), but not location, calendar year at diagnosis, presence of other EIMs, familial disease, smoking, or total steroid exposure.
In addition, early IBD-related hospitalization (after excluding the cases hospitalized for diagnostic purposes as well) was associated with disease behavior (P < 0.001), non-inflammatory disease behavior (OR = 5.04, 95%CI: 5.15-8.05, P < 0.001), perianal (OR = 2.06, 95%CI: 1.16-3.69, P = 0.013), or internal fistulizing disease (OR = 6.00, 95%CI: 2.69-13.7, P < 0.001) for need for immunosuppressives (OR = 2.08, 95%CI: 1.33-3.26, P = 0.001), and need for surgery or multiple surgeries (OR = 7.25, 95% CI: 4.34-12.1, P < 0.001) during the disease course, but not for age at onset or presence of anemia. In addition early IBD-related hospitalization was associated with disease location (P = 0.016) and smoking (P = 0.02) and with a trend towards more early hospitalizations in patients diagnosed in 2007-2012 (P = 0.06).
In a logistic regression model, the need for azathioprine was independently associated with early IBD-related hospitalization (P = 0.01, OR = 2.03), perianal disease (P =0.046, OR = 2.07), age at diagnosis (P = 0.002) and presence of arthritis (P < 0.001, OR = 2.96), but not with non-inflammatory behavior or era of diagnosis. (Table 2) In the same model, the need for early IBD-related hospitalization (P < 0.001, OR = 5.80), non-inflammatory behavior (P < 0.001, OR = 2.15), colonic location (P = 0.002, OR = 0.33) and, anaemia at presentation (P < 0.001, OR = 4.39), but not with smoking or perianal disease, were associated with the need for surgery (Table 2) The same associations were confirmed also in a time dependent Cox model, where the era of diagnosis was not associated with the need for surgery in this cohort (data not shown).
| Univariate analysis | Logistic regression | |
| Immunosuppressive use | ||
| Early IBD-related hospitalization | P = 0.001, OR = 2.08 | P = 0.01, OR = 2.03 |
| 95%CI: 1.33-3.26 | 95%CI: 1.18-3.49 | |
| Perianal disease | P = 0.01, OR = 2.28 | P = 0.046, OR = 2.07 |
| 95%CI: 1.21-4.30 | 95%CI: 1.01-4.22 | |
| Age at diagnosis1 | P < 0.001 | P = 0.002 |
| Location | P = 0.016 for location | NS |
| Smoking | P = 0.054 | P = 0.06 |
| Non-inflammatory behavior | P = 0.06 | NS |
| Arthritis | P = 0.03, OR = 1.76 | P < 0.001, OR = 2.96 |
| 95%CI: 1.05-2.98 | 95%CI: 1.63-5.39 | |
| Steroid use (any time) | P < 0.001, OR = 5.78 | - |
| 95%CI: 3.57-9.35 | ||
| Major IBD-related abdominal surgery | ||
| Early IBD-related hospitalization | P < 0.001, OR = 7.24 | P < 0.001, OR = 5.80 |
| 95%CI: 4.34-12.1 | 95%CI: 3.20-10.5 | |
| Non-inflammatory behavior | P < 0.001, OR = 5.38 | P < 0.001, OR = 2.15 |
| 95%CI: 3.30-8.76 | 95%CI: 1.56-2.94 | |
| Location | P < 0.0012 | P = 0.02 for location, |
| P = 0.002, OR = 0.33 | ||
| 95%CI: 0.16-0.67 for colonic location | ||
| Smoking | P = 0.17 | NS |
| Perianal disease | P = 0.19 | NS |
| Anaemia at presentation | P < 0.001, OR = 2.79 | P < 0.001, OR = 4.39 |
| 95%CI: 1.73-4.51 | 95%CI: 2.37-8.11 |
Hospitalization and re-hospitalization rates were relatively high in this population-based, inception cohort CD study from Eastern Europe. A significant proportion of patients were hospitalized for diagnostic workup. The mean duration of hospitalization was four- to fivefold higher in the first year after diagnosis compared to the subsequent years one to three years. Complicated disease behavior at diagnosis was identified as the key predictive factor for hospitalization and re-hospitalization. The need for early hospitalization was independently associated with the later disease course and clinically significant outcomes (need for immunosuppressives and surgery).
Relatively few data are available on hospitalization rates from population-based cohorts. In the early population-based studies between 1960 and 1985, the hospitalization rate was exceedingly high (e.g., in Denmark 83% of the CD patient hospitalized were admitted at least once within the first year after diagnosis, with admissions at a rate of about 20% per year over the next five years)[15]. In the same time period, the surgical rate was 35%, 8%, and 5% in the year of diagnosis, the second and third year following diagnosis, respectively. The cumulative risk was 61% within 10 years of diagnosis[16]. Of note, in a recent study by a Danish group, 66% of CD patients had at least one hospitalization event within seven years of diagnosis[17]. In contrast, in the early 2000s we found lower IBD-related hospitalization rates: 32.3% in the first year, 6.6%, and 4.1% annually in the second and third, and the fourth and fifth years after diagnosis. Interestingly, 56% of IBD-related hospitalization events were surgical hospitalizations within one year of diagnosis, while 40% to 48% of CD-related hospitalization events were surgical admissions in the subsequent nine years. Without question, re-hospitalization rates received inadequate study. The CD-related re-hospitalization rates in the present study were 13.6%, 23.9% and 29.8% within one, three and five years of diagnosis. Similarly, in the 1990s in a population-based study from Canada approximately 25% of subjects with CD were admitted annually, while only 4% were readmitted within one year and 56% was readmitted at least once. Nearly half of the hospitalizations were related to major surgery[18]. The annual age-adjusted hospitalization rate declined significantly from 29.2 to 26.9 per 100000 persons over the seven years of the study. Comparable rates were also reported from a more recent Canadian study between 1988 and 2008[19]. The cumulative IBD-related hospitalization rate was 26% and 36% after one and five years. In concordance with the present study, the highest hospitalization rates were within the first year of diagnosis and were no different according to the calendar year of diagnosis.
Lower ten-year cumulative hospitalization rates were also reported in the EC-IBD study[20]. The cumulative risk of hospitalization was 52.7% within ten years of diagnosis, with considerable geographical differences. Furthermore, hospitalization rates decreased after the first year of the diagnosis. Finally, even lower early hospitalization rates were reported in the very recent, population-based EpiCom study in patients diagnosed in 2010[21]. Cumulative CD-related hospitalization rates were 20% and 16% in western and eastern European centers, with 42% and 35% of events related to surgery, respectively.
Few data are available on the duration of hospitalization. In a study from Manitoba[6], the mean annual CD-related inpatient stay decreased from 17 to 11 days between 1991 and 2001. Fifty-two percent of CD patients were admitted and 40% readmitted within five years of diagnosis. Twenty-seven percent had a CD-related surgery with 15% readmitted for surgery. During the 15 years’ follow-up, 80% of admissions and 64% of surgeries were within five years of diagnosis. Concordantly, in the present study, the mean inpatient stay was 9.87 d in the year of the diagnosis, with rates in the subsequent three years decreasing significantly by 1.2-1.7 d annually. Of note, 46.7% of all CD-related hospitalizations occurred within one year of diagnosis, while 27.8%, 11.8%, and 13.7% of these events occurred between two to four, five to six, and seven to ten years after diagnosis. Comparable data were reported recently from Denmark, where hospitalization duration decreased from seven days per patient within one year of diagnosis to 0.9 d at year five[15].
The indication for hospitalization may be dependent on additional factors other than disease severity, including health insurance reimbursement policies and ethnic differences. For example, data from Kaiser Permanente Northern California (a health maintenance organization) suggested that hospitalization rates for Crohn’s disease decreased by 33% between 1998 and 2005[22]. The reasons for this rapid change are not clear.
As discussed above, major surgery represents 30%-50% of all CD-related hospitalization events. While data suggest a decrease in recent surgical rates[3] the majority of the studies report stable or only slightly fluctuating hospitalization rates after the 1970’s. Early studies reported higher surgery rates. In Stockholm, surgical rates were 30%, 50%, and 60% after 5, 10, and 15 years between 1955-1974 in a population-based study, while surgery rates were stable until 1989[23]. Similar to the present study and the data from Manitoba, in a more recent pre-biologic population-based cohort from Norway, (IBSEN) cumulative surgery rates in the 1990s were 14%, 27%, and 38% after one, five and ten years of diagnosis, respectively[24].
The indications for hospitalization may include diagnostic procedures, active disease requiring medical or surgical treatment, treatment related complications (side effects, infections), or unrelated causes. In a population-based study from Olmstead county[5] factors associated with first hospitalization included location (ileocolonic, small bowel, or upper gastrointestinal disease), and non-inflammatory behavior at baseline. In a further study from Canada, CD patients requiring hospitalization were more likely than UC cases to be female and younger[6]. Similarly, in the present study non-inflammatory disease behavior at diagnosis (HR = 1.32, P = 0.001), perianal disease (HR = 1.47, P = 0.04) were associated with time to first hospitalization while disease behavior change (HR = 2.38, P = 0.002) and need for steroids (HR = 3.14, P = 0.003) were associated with time to first re-hospitalization in multiple Cox-regression analyses. More data are available on predictors of surgery, including disease location, complicated disease behavior, perianal disease, smoking, medical strategy, and age at onset[3,25]. In addition, the association between arthritis and need for immunosuppressives reported in the present study warrants further investigations. However, a possible explanation is that extraintestinal manifestations may be regarded as markers of patients with systemic disease leading to more aggressive therapeutic strategy. Finally, the need for early hospitalization was identified as an independent marker of later disease course, and was associated with immunosuppressive use and surgery; this represents a major finding of this study.
The authors are aware of the possible limitations of the study. The indication for hospitalization is somewhat subjective and may be influenced by factors other than disease severity, such as insurance reimbursement or center protocols. In this study group, reimbursement policy and patient management did not change significantly in the during the study period. The main specialists delivering the majority of IBD care also remained the same. A further strength of the study is its population-based design, which enabled study of the full disease spectrum, including both mild and severe forms. We believe that this allows a more objective assessment of importance of possible predictors, which may not be possible in a solely referral-patient population. Thus data obtained in population-based setting are more objective in assess disease outcomes and enable generalizability of the findings to real-life IBD populations. Finally, an advantage of the present study was that we aimed to study the era after the approval introduction of biologicals. Thus, for the first time, we could investigate and report the change of hospitalization rates and indications of hospitalizations in the era of increasing biological use. Interestingly, only a relatively small proportion of CD patients were exposed to anti-TNFs. Nonetheless, our study provides an up-to-date view on the patterns and reasons for hospitalization in patients with Crohn’s disease. In addition, our data can contribute to the more accurate planning of health care access requirements of CD patients during the first 5-10 years of their disease.
In conclusion, hospitalization and re-hospitalization rates were still relatively high in this population-based cohort; almost half of disease-related hospitalizations occurred within one year of diagnosis. Subsequently, the average duration of hospitalization decreased significantly. Non-inflammatory disease behavior at diagnosis was identified as the pivotal predictive factor of hospitalization and re-hospitalization. Early hospitalization requirements were independently associated with clinical outcomes (need for immunosuppressives and surgery).
Hospitalizations are important outcome measures and major cost drivers in inflammatory bowel diseases. Recent clinical trials suggest that aggressive medical therapy leads to decreased hospitalization requirements. Recent data on hospitalization rates in Crohn’s disease (CD) from real life settings are lacking from population-based studies.
Limited data are available from population-based studies regarding health care utilization, including hospitalization requirements in CD from the era of biologicals.
Hospitalization and re-hospitalization rates are still high in this cohort. Non-inflammatory disease behavior at diagnosis was identified as the pivotal predictive factor of both hospitalization and re-hospitalization. Early hospitalization requirement was independently associated with clinically significant outcomes.
New data from this population-based cohort will help in predicting health care utilization requirements in CD patients in the current era which is important for both health care professionals and insurance companies. In addition, time-trends and predictors of hospitalizations were determined.
The main goal of the present study was to determine the inflammatory bowel diseases-related and all-cause first- and re-hospitalization rates during the first 5-years after the diagnosis stratified by disease duration and investigate the role of possible predictors.
The paper analyzes the factors influencing hospitalization rates in a subset of patients affected by CD. The paper is well written, inclusion/exclusion criteria and study protocol are appropriate; statistical analysis is proper and accurate.
P- Reviewer: Hokama A, Ierardi E, Wang K S- Editor: Qi Y L- Editor: A E- Editor: Liu XM
| 1. | Golovics PA, Mandel MD, Lovasz BD, Lakatos PL. Inflammatory bowel disease course in Crohn’s disease: is the natural history changing? World J Gastroenterol. 2014;20:3198-3207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (1)] |
| 2. | Burisch J, Jess T, Martinato M, Lakatos PL. The burden of inflammatory bowel disease in Europe. J Crohns Colitis. 2013;7:322-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 791] [Cited by in RCA: 739] [Article Influence: 61.6] [Reference Citation Analysis (0)] |
| 3. | Bernstein CN, Loftus EV, Ng SC, Lakatos PL, Moum B. Hospitalisations and surgery in Crohn’s disease. Gut. 2012;61:622-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 229] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 4. | Bouguen G, Levesque BG, Feagan BG, Kavanaugh A, Peyrin-Biroulet L, Colombel JF, Hanauer SB, Sandborn WJ. Treat to Target: A Proposed New Paradigm for the Management of Crohn’s Disease. Clin Gastroenterol Hepatol. 2015;13:1042-1050.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 209] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 5. | Peyrin-Biroulet L, Loftus EV, Harmsen WS. Emergency room visits and hospitalizations for Crohn’s disease in a populationbased cohort. Gastroenterology. 2010;138:S-532. |
| 6. | Longobardi T, Bernstein CN. Health care resource utilization in inflammatory bowel disease. Clin Gastroenterol Hepatol. 2006;4:731-743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 66] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Beaugerie L, Seksik P, Nion-Larmurier I, Gendre JP, Cosnes J. Predictors of Crohn’s disease. Gastroenterology. 2006;130:650-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 630] [Cited by in RCA: 639] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 8. | Tarrant KM, Barclay ML, Frampton CM, Gearry RB. Perianal disease predicts changes in Crohn’s disease phenotype-results of a population-based study of inflammatory bowel disease phenotype. Am J Gastroenterol. 2008;103:3082-3093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 185] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 9. | Lakatos PL, Czegledi Z, Szamosi T, Banai J, David G, Zsigmond F, Pandur T, Erdelyi Z, Gemela O, Papp J. Perianal disease, small bowel disease, smoking, prior steroid or early azathioprine/biological therapy are predictors of disease behavior change in patients with Crohn’s disease. World J Gastroenterol. 2009;15:3504-3510. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 92] [Cited by in RCA: 100] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 10. | Lakatos L, Mester G, Erdelyi Z, Balogh M, Szipocs I, Kamaras G, Lakatos PL. Striking elevation in incidence and prevalence of inflammatory bowel disease in a province of western Hungary between 1977-2001. World J Gastroenterol. 2004;10:404-409. [PubMed] |
| 11. | Lakatos L, Pandur T, David G, Balogh Z, Kuronya P, Tollas A, Lakatos PL. Association of extraintestinal manifestations of inflammatory bowel disease in a province of western Hungary with disease phenotype: results of a 25-year follow-up study. World J Gastroenterol. 2003;9:2300-2307. [PubMed] |
| 12. | Lennard-Jones JE. Classification of inflammatory bowel disease. Scand J Gastroenterol Suppl. 1989;170:2-6; discussion 16-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1396] [Cited by in RCA: 1445] [Article Influence: 40.1] [Reference Citation Analysis (0)] |
| 13. | Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR, Caprilli R, Colombel JF, Gasche C, Geboes K. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005;19 Suppl A:5A-36A. [PubMed] |
| 14. | Stange EF, Travis SP, Vermeire S, Beglinger C, Kupcinkas L, Geboes K, Barakauskiene A, Villanacci V, Von Herbay A, Warren BF. European evidence based consensus on the diagnosis and management of Crohn’s disease: definitions and diagnosis. Gut. 2006;55 Suppl 1:i1-i15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 402] [Cited by in RCA: 381] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 15. | Munkholm P, Langholz E, Davidsen M, Binder V. Disease activity courses in a regional cohort of Crohn’s disease patients. Scand J Gastroenterol. 1995;30:699-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 378] [Cited by in RCA: 345] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 16. | Munkholm P, Langholz E, Davidsen M, Binder V. Intestinal cancer risk and mortality in patients with Crohn’s disease. Gastroenterology. 1993;105:1716-1723. [PubMed] |
| 17. | Vester-Andersen MK, Vind I, Prosberg MV, Bengtsson BG, Blixt T, Munkholm P, Andersson M, Jess T, Bendtsen F. Hospitalisation, surgical and medical recurrence rates in inflammatory bowel disease 2003-2011-a Danish population-based cohort study. J Crohns Colitis. 2014;8:1675-1683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 18. | Bernstein CN, Nabalamba A. Hospitalization, surgery, and readmission rates of IBD in Canada: a population-based study. Am J Gastroenterol. 2006;101:110-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 110] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 19. | Nguyen GC, Nugent Z, Shaw S, Bernstein CN. Outcomes of patients with Crohn’s disease improved from 1988 to 2008 and were associated with increased specialist care. Gastroenterology. 2011;141:90-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 151] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 20. | Odes S, Vardi H, Friger M, Wolters F, Russel MG, Riis L, Munkholm P, Politi P, Tsianos E, Clofent J. Cost analysis and cost determinants in a European inflammatory bowel disease inception cohort with 10 years of follow-up evaluation. Gastroenterology. 2006;131:719-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 182] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 21. | Burisch J, Pedersen N, Cukovic-Cavka S, Turk N, Kaimakliotis I, Duricova D, Shonová O, Vind I, Avnstrøm S, Thorsgaard N. Initial disease course and treatment in an inflammatory bowel disease inception cohort in Europe: the ECCO-EpiCom cohort. Inflamm Bowel Dis. 2014;20:36-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 22. | Herrinton LJ, Liu L, Fireman B, Lewis JD, Allison JE, Flowers N, Hutfless S, Velayos FS, Abramson O, Altschuler A. Time trends in therapies and outcomes for adult inflammatory bowel disease, Northern California, 1998-2005. Gastroenterology. 2009;137:502-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 83] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 23. | Hellers G. Crohn’s disease in Stockholm county 1955-1974. A study of epidemiology, results of surgical treatment and long-term prognosis. Acta Chir Scand Suppl. 1979;490:1-84. [PubMed] |
| 24. | Solberg IC, Vatn MH, Høie O, Stray N, Sauar J, Jahnsen J, Moum B, Lygren I. Clinical course in Crohn’s disease: results of a Norwegian population-based ten-year follow-up study. Clin Gastroenterol Hepatol. 2007;5:1430-1438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 502] [Cited by in RCA: 526] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 25. | Lakatos PL, Golovics PA, David G, Pandur T, Erdelyi Z, Horvath A, Mester G, Balogh M, Szipocs I, Molnar C. Has there been a change in the natural history of Crohn’s disease? Surgical rates and medical management in a population-based inception cohort from Western Hungary between 1977-2009. Am J Gastroenterol. 2012;107:579-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 178] [Article Influence: 13.7] [Reference Citation Analysis (0)] |