Published online Jun 7, 2015. doi: 10.3748/wjg.v21.i21.6451
Peer-review started: January 14, 2015
First decision: March 10, 2015
Revised: March 15, 2015
Accepted: April 28, 2015
Article in press: April 28, 2015
Published online: June 7, 2015
Processing time: 148 Days and 13.3 Hours
Colonoscopy techniques combining or replacing air insufflation with water infusion are becoming increasingly popular. They were originally designed to reduce colonic spasms, facilitate cecal intubation, and lower patient discomfort and the need for sedation. These maneuvers straighten the rectosigmoid colon and enable the colonoscope to be inserted deeply without causing looping of the colon. Water-immersion colonoscopy minimizes colonic distension and improves visibility by introducing a small amount of water. In addition, since pain during colonoscopy indicates risk of bowel perforation and sedation masks this important warning, this method has the potential to be the favored insertion technique because it promotes patient safety without sedation. Recently, this water-immersion method has not only been used for colonoscope insertion, but has also been applied to therapy for sigmoid volvulus, removal of lesions, lower gastrointestinal bleeding, and therapeutic diagnosis of abnormal bowel morphology and irritable bowel syndrome. Although a larger sample size and prospective head-to-head-designed studies will be needed, this review focuses on the usefulness of water-immersion colonoscopy for diagnostic and therapeutic applications.
Core tip: Water-immersion colonoscopy minimizes colonic distension, reducing patient discomfort and the need for sedation. Due to these characteristic advantages, this method has been applied to treatment in diverse ways, not just as an insertion technique during colonoscopy. Its ease and safety are favorable for detorsion for sigmoid volvulus and treatment of lower gastrointestinal bleeding in the early postoperative period. Underwater endoscopic mucosal resection increases the proportion of completely resected lesions, and reduces recurrence, posttreatment bleeding, and perforation. Water-immersion colonoscopy is also useful for estimating the colon morphology based on changes in the water surface and the rotated direction of the colon.
- Citation: Sugimoto S, Mizukami T. Diagnostic and therapeutic applications of water-immersion colonoscopy. World J Gastroenterol 2015; 21(21): 6451-6459
- URL: https://www.wjgnet.com/1007-9327/full/v21/i21/6451.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i21.6451
Colonoscopy is performed both diagnostically and therapeutically, and considered the gold standard for the examination and removal of lesions in the colorectum[1,2]. Although it may be not true of specialists, the reported cecal intubation rate in unsedated colonoscopy using air insufflation (AI) is about 80%, while the rate in sedated colonoscopy is greater than 90%[3]. Loop formation, distension, and elongation of the colon, particularly at the sigmoid colon, are all causes of pain for patients[4], especially when procedures are performed without sedation. Pain associated with pushing through loops reduces the cecal intubation rate in unsedated patients. Therefore, in the United States[5] and in some Asian and Western European countries[6,7], conscious sedation or deep sedation is almost universally utilized during colonoscopy[3]. By right, deciding on the appropriate approach requires an assessment of the patient’s sedation needs and risks prior to the colonoscopy. It requires scrupulous attention to whether the patient has an increased risk of difficult airway management or increased cardiopulmonary complications of colonoscopy such as co-morbidities or being elderly, or obese. In addition, pain during colonoscopy indicates risk of perforation, but sedation masks this important warning[3]. From a safety point-of-view, unsedated colonoscopy seems to be more feasible if it is well tolerated by patients. Recently, the feasibility of unsedated colonoscopy has become well established[3] due to advances in gastrointestinal endoscopy, but it is often difficult to persuade endoscopists in countries where sedation is almost universally utilized of the merit of unsedated colonoscopy; they might even believe that this issue is of marginal clinical importance.
Colonoscopy techniques combining or replacing AI with water infusion were originally designed to reduce colonic spasms, facilitate cecal intubation, and lower patient discomfort and the need for sedation[8-10]. Indeed, the water infusion method has shown promise in minimizing discomfort and the need for sedation[10-16]. When water infusion in lieu of AI is used without sedation, the cecal intubation rate is enhanced to more than 90%[11-16]. While water infusion is becoming increasingly popular, it is not yet widely available, and its inherent utility currently suffers from criticisms such as “Preferable results may not be achieved when performed by less experienced endoscopists” and “The prolonged insertion time due to the time-consuming suction and exchange of water is a waste of time”. Yet, these are misapprehensions: colonoscopy with water infusion can be easily performed by even less experienced endoscopists[3,10,17] and is very useful not only for the insertion of the colonoscope but also as a diagnostic and therapeutic tool. Recently, this method has been applied to therapy for sigmoid volvulus, the removal of lesions, lower gastrointestinal bleeding, and therapeutic diagnosis of abnormal bowel morphology and irritable bowel syndrome. This review focuses on the unique merits of water infusion and its therapeutic applications.
Falchuk et al[8] first described water colonoscopy, i.e., the basic idea of water-immersion (WI) colonoscopy, for patients with severe diverticulosis in 1984. They filled the colon with 100-300 mL of water in lieu of AI to distend the lumen. The water opened and straightened this portion of the sigmoid colon, making it possible to distinguish clearly the real from the apparent lumen. The water was subsequently removed by suction. This technique was then modified by other groups seeking to facilitate cecal intubation, reduce colonic spasms, lower patient discomfort, and decrease the need for sedation[9,18,19]. To sum up, this water method requires the infusion of water in lieu of AI to distend the lumen during the insertion of the colonoscope.
In Japan, Hamamoto et al[20] reported the first randomized controlled trial (RCT) associated with unsedated water colonoscopy performed by three trainees. In this RCT, the water method was used in which 500-1000 mL of water were instilled into the colon by an enema. Compared with using AI, the proportion of patients who complained of abdominal pain during the procedure was lower (water method 17.1% vs AI 33.3%, P < 0.01) and cecal intubation was faster (10.5 min vs 16.2 min, P < 0.01).
Mizukami et al[17], later modified the water method[10]. This version, called the “collapse-submergence method” or “water-navigation method” demonstrated novelty in its removal of the boundary line between intracolonic water and air and complete suctioning of residual luminal air to improve visibility. This kind of water method associated with complete removal of residual luminal air is widely used as a WI method at present. The WI method combined with a cap attached to the tip of the colonoscope allows an adequate distance between the instrument and the colonic wall to be maintained, thus keeping the luminal direction in view and improving insertion[10]. With this cap-assisted combination, the endoscopic view is maintained by the space inside the cap filled with a small amount of clear water. Water accumulates around the tip of the colonoscope, flows straight down into the descending colon, and straightens the rectosigmoid colon. This mechanism enables the colonoscope to be inserted through the sigmoid colon without causing looping of the colon. In an RCT performed by 10 endoscopists (including trainees), Asai et al[21] confirmed that WI increased the success rate of insertion through the sigmoid colon without loop formation using a magnetic endoscope imaging device. The success rate of insertion without loop formation was 37.5%, 40.0%, and 53.8% in the standard AI, cap-assisted AI, and cap-assisted WI groups, respectively. There were no significant differences among the groups with respect to cecal intubation rate, cecal intubation time, or number of polyps > 5 mm in diameter per patient. Importantly, there were no significant differences among the three groups in terms of cecal intubation time, including the time taken to infuse the water (approximately 30 s) and the short time required for water removal. Many other RCTs have been performed[22-31] and the WI method has been shown to reduce pain scores, need for sedation, and general patient distress[11-14].
Water-aided colonoscopy entails infusion of water in lieu of AI to distend the lumen during the insertion of the colonoscope. Leung et al[15] suggested that water-aided colonoscopy be broadly classified into two categories depending on the the timing of the removal of infused water: the WI method (water infusion with water removal predominantly during withdrawal)[22-31] and the water exchange (WE) method (water infusion with water removal predominantly during insertion)[32-37]. However, there is a lack of consensus among other groups on the clear distinction between WI and WE.
In daily medical practice, procedures are sometimes a mixture of the two techniques. WI includes suctioning residual luminal air using a small amount of water: even if endoscopists intend to perform WI, poor bowel preparation requires a degree of suction and then reinfusion of fresh water to see the lumen and continue the insertion. On the other hand, WE amounts to nearly the same thing as WI when the bowel is prepared properly because there is no need for the exchange of water. In principle, water infusion involves turning the insufflation gas off and filling the colon with water only during insertion[15]. However, WI colonoscopy can be usually performed together with air or carbon dioxide insufflation during insertion after passing through the sigmoid-descending junction. These undefinitive classifications remain issues of note, especially when performing RCTs or meta-analyses.
Compared with AI, recent studies show that both WI and WE reduce insertion pain in patients who are lightly sedated or unsedated[11-16]. WI, performed together with carbon dioxide insufflation during withdrawal, has added benefits for improving patient comfort[38,39]. If patients tolerate the procedure well without sedation, pain during colonoscopy can be a warning sign of impending complications, such as perforation[3]. WI also enhances cecal intubation in previously incomplete colonoscopies[40].
Systematic reviews indicate that the WI method has no impact on the adenoma detection rate (ADR)[11-14], an indicator of colonoscopy quality[41,42]. In contrast, some meta-analyses that separated RCTs using WI with those using WE have suggested that WE may be superior in increasing the ADR[15,16], but this difference was not statistically significant[36].
To further increase the ADR, indigo carmine and cap-assisted colonoscopy can be combined with the WE method. Leung et al[43] reported that indigo carmine (concentration: 0.008%) used in conjunction with the WE method enhances the ADR (WE 44% vs combined 62%, P = 0.03). It has already been reported that cap-assisted colonoscopy combined with WI has the potential to reduce patient discomfort and make colonoscope insertion easier[10,44]. In a later study, the potential improvement to ADR by cap-assisted colonoscopy was evaluated by Yen et al[45], who reported that the WE method combined with it resulted in a higher ADR compared to AI colonoscopy in consecutive patients (cap-assisted WE 75.0% vs AI 59.4%, P = 0.02), although this was a retrospective study. The impact of WE colonoscopy on ADR has become a new avenue of investigation.
One of the biggest disadvantages of WE compared to WI is the longer procedure time, because suctioning dirty water and replacing it with clean water can be time-consuming. However, there are complementary advantages. Hsieh et al[36] reported in a RCT that for their AI, WI, and WE groups, while the cecal intubation time averaged 6.3 min, 5.7 min, and 16.4 min, the painless insertion rate was 30.0%, 43.3%, 61.1%, respectively. The improved ADR with WE might also be explained by the improved bowel cleansing and the longer insertion time. Whether WE colonoscopy becomes one of the more preferred techniques in daily medical practice is controversial due to the prolonged insertion time caused by time-consuming suction and exchange of water. Although WE colonoscopy may improve the ADR, the benefit of water-aided colonoscopy that most practitioners mainly focus on is improved patient comfort. However, concerned readers should note that WE is not an essential component in the therapeutic applications of WI described below in this review.
Since the majority of published RCTs using water infusion at present were performed by endoscopists highly experienced with this method, there appears to be a misunderstanding that this method is difficult for less experienced endoscopists. Actually, WI colonoscopy is the preferred method for trainees, and colonoscopy with water infusion was easily performed by trainees in some published RCTs[20-23,26]. In our experience, trainees can perform painless unsedated colonoscopy from the outset after training with a colon model[10,17], even if they have no experience in colonoscopy or esophagogastroduodenoscopy.
Loop formation and the distension and elongation of the colon, particularly at the sigmoid colon, are often the cause of pain in patients[4]. WI resolves passing though the sigmoid-descending junction without loop formation, which is often a technical challenge for trainees[17], and prevents excessive AI. WI also minimizes discomfort and the need for sedation, which can mask pain, a warning sign of impending complication[3]. Thus, WI is useful for trainee education, and the ease and safety of this method renders it useful for therapeutic applications.
Colonic volvulus is one of the most common causes of acute large bowel obstruction. The long, redundant, sigmoid colon, with an elongated mesentery, is prone to twisting on itself; it is the most common location of colonic volvulus (60% of cases)[46]. Sigmoid volvulus (SV) has a high associated mortality rate in cases of obstruction and ischemic changes. SV occurs more frequently in elderly patients, particularly those with psychiatric issues or dementia, or senile patients in nursing homes[47].
The therapeutic management of SV remains controversial and can be classified into nonsurgical and surgical treatment. However, nonsurgical treatment such as endoscopic detorsion is generally considered appropriate, to minimize invasive treatment[48,49]. After endoscopic detorsion, an elective resection of the sigmoid colon is recommended in cases where the risks associated with elective surgery are less than those associated with recurrence[50]. The controversy surrounding the indications for elective surgery is based on the high surgical risk for patients of advanced age, or with multiple comorbidities[51-53]. Since mortality rates are significantly lower in patients without ischemic change, early diagnosis and endoscopic treatment are of primary concern.
It is important that endoscopic detorsion should only be attempted in patients not contraindicated for endoscopic therapy: such excluded patients include those with hemodynamic instability peritonitis, intestinal ischemia, or perforation[54]. Meticulous attention should be taken to minimize the introduction of air due to the risk of perforation in an already dilated colon proximal to the obstruction. During the insertion phase of colonoscopy, WI instead of traditional AI has been proposed in order to reduce pain[10]. Once perforation occurs during treatment, a large amount of intestinal fluid, including stool, leaks into the abdominal cavity, creating a high risk of peritonitis. In these perforation cases, emergency surgery should be done immediately and the peritonitis risk is the same with traditional AI colonoscopy. Therefore, reducing the risk of perforation is paramount. WI colonoscopy minimizes colonic distension and improves visibility by introducing a small amount of water[10]. Since excessive AI increases the risk of perforation, the risk of perforation may be particularly high when the trainees perform endoscopic detorsion. In addition, since pain during colonoscopy is indicative of possible bowel perforation and sedation masks this important warning[3], a painless, unsedated colonoscope insertion technique during endoscopic detorsion is essential for patient safety[52].
Sugimoto et al[54-56] reported the prognosis of 21 SV patients who underwent 71 endoscopic detorsion procedures using WI colonoscopy without sedation. The procedures were carried out by 14 colonoscopists, including 9 trainees. Because the WI was cap-assisted, aspiration of all air made it possible to maintain a clear endoscopic view even without bowel preparation. Endoscopic detorsion was successfully completed in all cases without complications. Although the recurrence rate of endoscopic detorsion with WI was relatively high (56% per patient and 75% per procedure), resection of the sigmoid colon was avoidable in most cases[54]. However, this was not a comparative study but a retrospective collection of descriptive clinical results, and so the results cannot be said to prove that WI colonoscopy is better than AI colonoscopy. Around the same time, Tan et al[57] reported two cases of SV using a similar method and described the possibility of greatly reduced perforation risk. It is also difficult to make a definitive conclusion from this report because of the small number of patients. A larger sample size and a prospective head-to-head-designed study are needed to confirm the effectiveness of this method. Nonetheless, these clinical results suggest that WI colonoscopy for the management of SV should be considered a therapeutic option for avoiding high-risk surgery in high-risk and elderly patients.
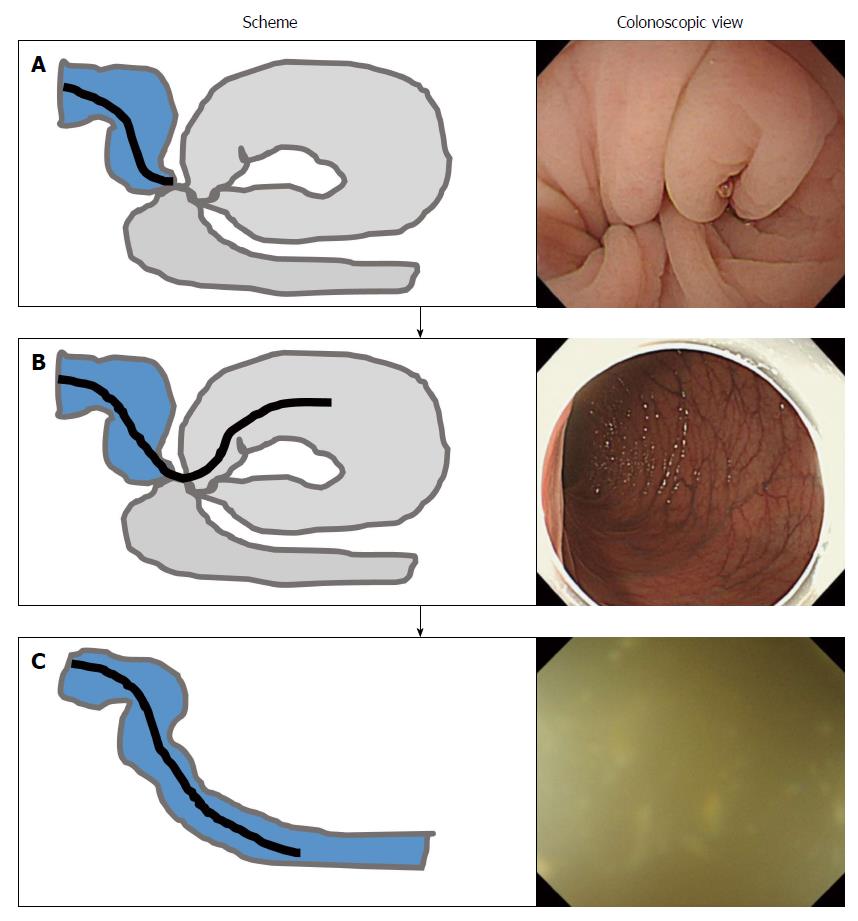
To accord with the torsion of the sigmoid colon, the colonoscope is inserted with a twisting motion. At the point of the obstruction, the colonoscope passes through the twisted colonic segment without AI (Figure 1A). If this operation is successful, the distended proximal segment appears (Figure 1B) and the endoscopic suction decompresses the lumen, often resulting in spontaneous detorsioning. Successful detorsion can be confirmed without the need for fluoroscopic guidance as when soft, aqueous stool flows out from the oral side (Figure 1C)[54,55]. In addition, unsedated procedures can be safely performed by careful checking of a patient’s symptoms; these symptoms often resolve when the detorsion is successful[54]. The ease and safety of WI colonoscopy is beneficial, especially for trainees. For these reasons, WI has been applied to endoscopic treatment, rather than just an insertion method.
Generally, after reaching the cecum, the residual water is suctioned and air insufflated, distending the colon to facilitate inspection and removal of lesions including polypectomy, endoscopic mucosal resection (EMR), and endoscopic submucosal dissection (ESD) each of which are usually performed upon scope withdrawal. However, AI can cause colonic spasms and contractions. Colonic spasms around larger lesions in an air-filled colon often interfere with lesion removal. The procedure is sometimes difficult, especially in the sigmoid colon, which is often dependent and will not retain insufflated air. To solve this problem, carbon dioxide, which is more rapidly absorbed than air, is commonly used[38,39]. On the other hand, water infusion has been recently used for the removal of lesions. While AI makes the angulations in the sigmoid more acute, water infusion straightens the sigmoid in patients in the left lateral decubitus position[10].
Binmoeller et al[58] described underwater EMR (UEMR) of large colon polyps using the WI method. Filling the sigmoid with clear water provides luminal distention and allows easy underwater polyp visualization. UEMR is applied to the removal of lesions of varying sizes, forms, and locations[59-64]. UEMR is useful in difficult polypectomy cases and has potential as a salvage intervention when endoscopic treatment with AI is unsuccessful[59-61]. For example, UEMR eliminates the need for submucosal injection and is useful for salvage treatment of recurrent adenomas with fibrosis after piecemeal EMR[60]. Compared with conventional EMR, UEMR increases the proportion of complete resection of medium- to large-sized lesions, and reduces the proportion of recurrences, posttreatment bleeding, transmural burns, and perforation[58-64]. Since water does not affect the conductivity of the tissue during polypectomy, cold as well as hot snare polypectomy can be safely executed in a water-filled lumen. Water acts as a heat sink and prevents direct contact of the polyp tip with the nearby colonic wall; thus, UEMR can minimize the risk of contralateral mucosal burns during polypectomy[62].
UEMR is a relatively simple and safe method for the removal of large colorectal lesions and is simple for endoscopists with extensive experience in conventional EMR or ESD to master[63]. On the other hand, the major limitation of UEMR is that it does not work well under conditions of poor bowel preparation, as the residual stool tends to obscure the endoscopic view. In such cases, residual stool must be removed with clean water by WE. Large, prospective controlled studies from multiple institutions are needed.
Colonoscopy is generally not recommended in the early postoperative period after colorectal anastomosis, as this leads to a high risk of anastomosis leakage due to excessive AI or inadvertent pressure from the endoscope. Since WI minimizes colonic distension relative to AI[10], WI colonoscopy may reduce the risk of anastomosis leakage. This concept of using WI colonoscopy is similar to that of endoscopic detorsion for SV[54]. Frossard et al[65] and Gor et al[66] have reported that WI colonoscopy renders the location of the anastomosis and the source of active bleeding identifiable with minimum colonic distension in patients that have undergone colorectal anastomosis, thus allowing the safe placement of clips on the active vessels to stop the bleeding. In a water-filled lumen, the blood from the bleeding site streams into the water, making it easy to pinpoint the site of bleeding for treatment. However, large prospective studies are needed to determine the feasibility of WI colonoscopy for locating and staunching postoperative gastrointestinal bleeding, as the reports mentioned above involved only three patients.
While colonoscopy can be performed without pain in most cases, some patients do experience it. Most of these patients have abnormal colon morphology and the pain is caused when the colonoscope is passing the flexures, which are hairpin bends in the colon[4,67]. Mizukami et al[68] reported that the use of the PCF-PQ260 colonoscope (Olympus Co., Tokyo, Japan), which is designed with passive-bending and high-force transmission[69-71], combined with the WI method, significantly shortens cecal intubation time and reduces pain thanks to its minimal turning radius in these difficult cases. Abnormal colon morphology such as mesocolon descendens and sigmoid colon malrotation was frequently observed in such cases. Although there are marked geographic variations, with high incidences in Japan and low incidences in Western countries, abnormal colon morphology is common in irritable bowel syndrome (IBS) patients, and seems to cause disorders related to defecation[72-74]. Significant association between IBS and physical activity[75] or past surgical history[76] suggests that bowel morphology is a potentially influential factor on gastrointestinal symptoms.
WI colonoscopy is useful not only for minimizing discomfort but also for estimating colon morphology. Colon morphology can be roughly determined based on changes in the water surface and the rotated direction of the colon. The accuracy of this determination can be confirmed by computed tomographic colonography or barium enema soon after the colonoscopy. After evaluation of colon morphology, patients with abnormal colon morphology can be treated by exercise, massage, and administering saline laxatives[72-74]. WI colonoscopy is a useful diagnostic tool that can lead to better treatments for defecation disorders due to abnormal colon morphology. As this idea is only of theoretical interest at present, interpreting WI colonoscopy findings in terms of colon morphology is still only learnable through experience, and just a few experienced endoscopists understand this role that the evaluation method can serve. The studied results are available in a meeting abstract[72] and in Japanese-only articles[73,74], books, and TV shows. Developing objective criteria and methods to evaluate colon morphology and assessing the appropriateness of WI are needed.
In summary, WI colonoscopy is useful not only for the insertion phase of colonoscopy but also as a tool with diverse diagnostic and therapeutic applications. Especially in difficult cases, the WI method can act as a salvage intervention when endoscopic treatment with AI is unsuccessful. The ease and safety of WI colonoscopy is also beneficial and is advantageous to therapeutic applications. To promote the use of WI in colonoscopy and other situations and to address typical criticisms of this technique, further large prospective studies are needed to straighten out misunderstandings related to the WI method. It is hoped that use of WI colonoscopy and its therapeutic applications will become increasingly widespread.
P- Reviewer: Jiang SL, Trevisani J S- Editor: Yu J L- Editor: A E- Editor: Wang CH
| 1. | Edwards BK, Ward E, Kohler BA, Eheman C, Zauber AG, Anderson RN, Jemal A, Schymura MJ, Lansdorp-Vogelaar I, Seeff LC. Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010;116:544-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1390] [Cited by in RCA: 1505] [Article Influence: 100.3] [Reference Citation Analysis (1)] |
| 2. | Nishihara R, Wu K, Lochhead P, Morikawa T, Liao X, Qian ZR, Inamura K, Kim SA, Kuchiba A, Yamauchi M. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med. 2013;369:1095-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 968] [Cited by in RCA: 1158] [Article Influence: 96.5] [Reference Citation Analysis (0)] |
| 3. | Leung FW, Aljebreen AM, Brocchi E, Chang EB, Liao WC, Mizukami T, Schapiro M, Triantafyllou K. Sedation-risk-free colonoscopy for minimizing the burden of colorectal cancer screening. World J Gastrointest Endosc. 2010;2:81-89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 21] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Shah SG, Brooker JC, Thapar C, Williams CB, Saunders BP. Patient pain during colonoscopy: an analysis using real-time magnetic endoscope imaging. Endoscopy. 2002;34:435-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 100] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Rex DK, Khalfan HK. Sedation and the technical performance of colonoscopy. Gastrointest Endosc Clin N Am. 2005;15:661-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 67] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Bowles CJ, Leicester R, Romaya C, Swarbrick E, Williams CB, Epstein O. A prospective study of colonoscopy practice in the UK today: are we adequately prepared for national colorectal cancer screening tomorrow? Gut. 2004;53:277-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 410] [Cited by in RCA: 421] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 7. | Ladas SD, Satake Y, Mostafa I, Morse J. Sedation practices for gastrointestinal endoscopy in Europe, North America, Asia, Africa and Australia. Digestion. 2010;82:74-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 8. | Falchuk ZM, Griffin PH. A technique to facilitate colonoscopy in areas of severe diverticular disease. N Engl J Med. 1984;310:598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 49] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Baumann UA. Water intubation of the sigmoid colon: water instillation speeds up left-sided colonoscopy. Endoscopy. 1999;31:314-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Mizukami T, Yokoyama A, Imaeda H. Collapse-submergence method: simple colonoscopic technique combining water infusion with complete air removal from the rectosigmoid colon. Dig Endosc. 2007;19:43-48. [RCA] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Rabenstein T, Radaelli F, Zolk O. Warm water infusion colonoscopy: a review and meta-analysis. Endoscopy. 2012;44:940-951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Jun WU, Bing HU. Comparative effectiveness of water infusion vs air insufflation in colonoscopy: a meta-analysis. Colorectal Dis. 2013;15:404-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Lin S, Zhu W, Xiao K, Su P, Liu Y, Chen P, Bai Y. Water intubation method can reduce patients’ pain and sedation rate in colonoscopy: a meta-analysis. Dig Endosc. 2013;25:231-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Hu D, Xu Y, Sun Y, Zhu Q. Water infusion versus air insufflation for colonoscopy: a meta-analysis of randomized controlled trials. Tech Coloproctol. 2013;17:487-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Leung FW, Amato A, Ell C, Friedland S, Harker JO, Hsieh YH, Leung JW, Mann SK, Paggi S, Pohl J. Water-aided colonoscopy: a systematic review. Gastrointest Endosc. 2012;76:657-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 91] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 16. | Leung FW, Hu B, Wu J. Comparative effectiveness of water immersion and water exchange versus air insufflation for colonoscopy. J Interv Gastroenterol. 2013;3:100-103. |
| 17. | Mizukami T, Hibi T. How I teach my trainees “Water Navigation Colonoscopy”. Am J Clin Med. 2010;7:144-146. |
| 18. | Sakai Y. Colon examination and diagnosis with colonoscopy. Gastroenterol Endosc. 1988;30 Suppl 1:2925-2927 (in Japanese). [DOI] [Full Text] |
| 19. | Sekioka T, Kosuga T, Endou K Iizuka O, Omatsu M, Fujie J, Tsuji M, Nakai O, Masuda M, Hirata K, Ichiji H. A new insertion technique of the colonoscopy: The submarine method. Gastroenterol Endosc. 1990;32:1461-1468 (in Japanese with English abstract). [DOI] [Full Text] |
| 20. | Hamamoto N, Nakanishi Y, Morimoto N, Inoue H, Tatukawa M, Nakata S, Kawai Y, Kurihara N, Ookuchi S, Shizuku T. A new water instillation method for colonoscopy without sedation as performed by endoscopists-in-training. Gastrointest Endosc. 2002;56:825-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Asai S, Fujimoto N, Tanoue K, Akamine E, Nakao E, Hashimoto K, Ichinona T, Nambara M, Sassa S, Yanagi H. Water immersion colonoscopy facilitates straight passage of the colonoscope through the sigmoid colon without loop formation: randomized controlled trial. Dig Endosc. 2015;27:345-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Leung CW, Kaltenbach T, Soetikno R, Wu KK, Leung FW, Friedland S. Water immersion versus standard colonoscopy insertion technique: randomized trial shows promise for minimal sedation. Endoscopy. 2010;42:557-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 84] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 23. | Park SC, Keum B, Kim ES, Jung ES, Lee SD, Park S, Seo YS, Kim YS, Jeen YT, Chun HJ. Usefulness of warm water and oil assistance in colonoscopy by trainees. Dig Dis Sci. 2010;55:2940-2944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 24. | Brocchi E, Pezzilli R, Tomassetti P, Campana D, Morselli-Labate AM, Corinaldesi R. Warm water or oil-assisted colonoscopy: toward simpler examinations? Am J Gastroenterol. 2008;103:581-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 49] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 25. | Radaelli F, Paggi S, Amato A, Terruzzi V. Warm water infusion versus air insufflation for unsedated colonoscopy: a randomized, controlled trial. Gastrointest Endosc. 2010;72:701-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 66] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 26. | Ransibrahmanakul K, Leung JW, Mann SK, Siao-Salera R, Lim BS, Hasyagar C, Yen D, Nastaskin I, Leung FW. Comparative effectiveness of water vs air methods in minimal sedation colonoscopy performed by supervised trainees in the US - a RCT. Am J Clin Med. 2010;7:113-118. |
| 27. | Hsieh YH, Lin HJ, Tseng KC. Limited water infusion decreases pain during minimally sedated colonoscopy. World J Gastroenterol. 2011;17:2236-2240. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 28] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 28. | Hsieh YH, Tseng KC, Hsieh JJ, Tseng CW, Hung TH, Leung FW. Feasibility of colonoscopy with water infusion in minimally sedated patients in an Asian Community Setting. J Interv Gastroenterol. 2011;1:185-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 29. | Pohl J, Messer I, Behrens A, Kaiser G, Mayer G, Ell C. Water infusion for cecal intubation increases patient tolerance, but does not improve intubation of unsedated colonoscopies. Clin Gastroenterol Hepatol. 2011;9:1039-1043.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 30. | Falt P, Liberda M, Smajstrla V, Kliment M, Bártková A, Tvrdík J, Fojtík P, Urban O. Combination of water immersion and carbon dioxide insufflation for minimal sedation colonoscopy: a prospective, randomized, single-center trial. Eur J Gastroenterol Hepatol. 2012;24:971-977. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 31. | Amato A, Radaelli F, Paggi S, Baccarin A, Spinzi G, Terruzzi V. Carbon dioxide insufflation or warm-water infusion versus standard air insufflation for unsedated colonoscopy: a randomized controlled trial. Dis Colon Rectum. 2013;56:511-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 32. | Leung JW, Mann SK, Siao-Salera R, Ransibrahmanakul K, Lim B, Cabrera H, Canete W, Barredo P, Gutierrez R, Leung FW. A randomized, controlled comparison of warm water infusion in lieu of air insufflation versus air insufflation for aiding colonoscopy insertion in sedated patients undergoing colorectal cancer screening and surveillance. Gastrointest Endosc. 2009;70:505-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 76] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 33. | Leung FW, Harker JO, Jackson G, Okamoto KE, Behbahani OM, Jamgotchian NJ, Aharonian HS, Guth PH, Mann SK, Leung JW. A proof-of-principle, prospective, randomized, controlled trial demonstrating improved outcomes in scheduled unsedated colonoscopy by the water method. Gastrointest Endosc. 2010;72:693-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 115] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 34. | Leung J, Mann S, Siao-Salera R, Ransibrahmanakul K, Lim B, Canete W, Samson L, Gutierrez R, Leung FW. A randomized, controlled trial to confirm the beneficial effects of the water method on U.S. veterans undergoing colonoscopy with the option of on-demand sedation. Gastrointest Endosc. 2011;73:103-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 74] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 35. | Cadoni S, Gallittu P, Sanna S, Fanari V, Porcedda ML, Erriu M, Leung FW. A two-center randomized controlled trial of water-aided colonoscopy versus air insufflation colonoscopy. Endoscopy. 2014;46:212-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 36. | Hsieh YH, Koo M, Leung FW. A patient-blinded randomized, controlled trial comparing air insufflation, water immersion, and water exchange during minimally sedated colonoscopy. Am J Gastroenterol. 2014;109:1390-1400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 83] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 37. | Garborg K, Kaminski MF, Lindenburger W, Wiig H, Hasund A, Wronska E, Bie RB, Kleist B, Løvdal L, Holme Ø. Water exchange versus carbon dioxide insufflation in unsedated colonoscopy: a multicenter randomized controlled trial. Endoscopy. 2015;47:192-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 38. | Saito Y, Uraoka T, Matsuda T, Emura F, Ikehara H, Mashimo Y, Kikuchi T, Kozu T, Saito D. A pilot study to assess the safety and efficacy of carbon dioxide insufflation during colorectal endoscopic submucosal dissection with the patient under conscious sedation. Gastrointest Endosc. 2007;65:537-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 152] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 39. | Sajid MS, Caswell J, Bhatti M, Sains P, Baig M, Miles W. Carbon dioxide insufflation versus conventional air insufflation for colonoscopy: a systematic review and meta-analysis of published randomized controlled trials. Colorectal Dis. 2014;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 40. | Vemulapalli KC, Rex DK. Water immersion simplifies cecal intubation in patients with redundant colons and previous incomplete colonoscopies. Gastrointest Endosc. 2012;76:812-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 41. | Kaminski MF, Regula J, Kraszewska E, Polkowski M, Wojciechowska U, Didkowska J, Zwierko M, Rupinski M, Nowacki MP, Butruk E. Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med. 2010;362:1795-1803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1287] [Cited by in RCA: 1468] [Article Influence: 97.9] [Reference Citation Analysis (0)] |
| 42. | Corley DA, Jensen CD, Marks AR, Zhao WK, Lee JK, Doubeni CA, Zauber AG, de Boer J, Fireman BH, Schottinger JE. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med. 2014;370:1298-1306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1251] [Cited by in RCA: 1561] [Article Influence: 141.9] [Reference Citation Analysis (0)] |
| 43. | Leung J, Mann S, Siao-Salera R, Ngo C, McCreery R, Canete W, Leung F. Indigocarmine added to the water exchange method enhances adenoma detection - a RCT. J Interv Gastroenterol. 2012;2:106-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 44. | Falt P, Šmajstrla V, Fojtík P, Liberda M, Kliment M, Tvrdík J, Urban O. Cap-assisted water immersion for minimal sedation colonoscopy: prospective, randomized, single-center trial. Dig Endosc. 2013;25:434-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 45. | Yen AW, Leung JW, Leung FW. A novel method with significant impact on adenoma detection: combined water-exchange and cap-assisted colonoscopy. Gastrointest Endosc. 2013;77:944-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 46. | Lal SK, Morgenstern R, Vinjirayer EP, Matin A. Sigmoid volvulus an update. Gastrointest Endosc Clin N Am. 2006;16:175-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 62] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 47. | Larkin JO, Thekiso TB, Waldron R, Barry K, Eustace PW. Recurrent sigmoid volvulus - early resection may obviate later emergency surgery and reduce morbidity and mortality. Ann R Coll Surg Engl. 2009;91:205-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 48. | Kuzu MA, Aşlar AK, Soran A, Polat A, Topcu O, Hengirmen S. Emergent resection for acute sigmoid volvulus: results of 106 consecutive cases. Dis Colon Rectum. 2002;45:1085-1090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 39] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 49. | Chung YF, Eu KW, Nyam DC, Leong AF, Ho YH, Seow-Choen F. Minimizing recurrence after sigmoid volvulus. Br J Surg. 1999;86:231-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 51] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 50. | Tan KK, Chong CS, Sim R. Management of acute sigmoid volvulus: an institution’s experience over 9 years. World J Surg. 2010;34:1943-1948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 51. | Raveenthiran V, Madiba TE, Atamanalp SS, De U. Volvulus of the sigmoid colon. Colorectal Dis. 2010;12:e1-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 73] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 52. | Safioleas M, Chatziconstantinou C, Felekouras E, Stamatakos M, Papaconstantinou I, Smirnis A, Safioleas P, Kostakis A. Clinical considerations and therapeutic strategy for sigmoid volvulus in the elderly: a study of 33 cases. World J Gastroenterol. 2007;13:921-924. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 59] [Cited by in RCA: 55] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 53. | Ballantyne GH. Sigmoid volvulus: high mortality in county hospital patients. Dis Colon Rectum. 1981;24:515-520. [PubMed] |
| 54. | Sugimoto S, Hosoe N, Mizukami T, Tsunoda Y, Ito T, Imamura S, Tamura T, Nagakubo S, Morohoshi Y, Koike Y. Effectiveness and clinical results of endoscopic management of sigmoid volvulus using unsedated water-immersion colonoscopy. Dig Endosc. 2014;26:564-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 55. | Sugimoto S, Mizukami T, Ito T, Tsunoda Y, Imamura S, Tamura T, Nagakubo S, Morohoshi Y, Koike Y, Fujita Y. Endoscopic detorsion for sigmoid volvulus using unsedated water-immersion colonoscopy. Endoscopy. 2013;45 Suppl 2 UCTN:E263-E264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 56. | Sugimoto S, Mizukami T, Morohoshi Y, Komatsu H. Sigmoid volvulus associated with Chilaiditi’s syndrome. Intern Med. 2013;52:515-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 57. | Tan C, Kunkel D, Ocampo LH, Sanmiguel CP, Karsan S, Cohen H, Leung FW. A novel application of the water exchange method in the treatment of sigmoid volvulus: a report of two cases. J Interv Gastroenterol. 2013;3:28-30. |
| 58. | Binmoeller KF, Weilert F, Shah J, Bhat Y, Kane S. “Underwater” EMR without submucosal injection for large sessile colorectal polyps (with video). Gastrointest Endosc. 2012;75:1086-1091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 275] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 59. | Anderson JM, Goel GA, Cohen H, Leung FW. Water infusion distention during colonoscopy is a safe alternative technique to facilitate polypectomy in a “difficult location”. J Interv Gastroenterol. 2013;3:137-140. |
| 60. | Friedland S, Leung F. Underwater endoscopic mucosal resection as a salvage treatment after unsuccessful standard endoscopic mucosal resection in the colon. J Interv Gastroenterol. 2013;3:93-95. |
| 61. | Kim HG, Thosani N, Banerjee S, Chen A, Friedland S. Underwater endoscopic mucosal resection for recurrences after previous piecemeal resection of colorectal polyps (with video). Gastrointest Endosc. 2014;80:1094-1102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 89] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 62. | Ocampo LH, Kunkel DC, Yen A, Tan CR, Leung JW, Leung FW. Underwater hot and cold snare polypectomy can be safely executed during water exchange colonoscopy. J Interv Gastroenterol. 2013;3:104-106. |
| 63. | Wang AY, Flynn MM, Patrie JT, Cox DG, Bleibel W, Mann JA, Sauer BG, Shami VM. Underwater endoscopic mucosal resection of colorectal neoplasia is easily learned, efficacious, and safe. Surg Endosc. 2014;28:1348-1354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 64. | Uedo N, Nemeth A, Johansson GW, Toth E, Thorlacius H. Underwater endoscopic mucosal resection of large colorectal lesions. Endoscopy. 2015;47:172-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 65. | Frossard JL, Gervaz P, Huber O. Water-immersion sigmoidoscopy to treat acute GI bleeding in the perioperative period after surgical colorectal anastomosis. Gastrointest Endosc. 2010;71:167-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 66. | Gor N, Patil A. Endoscopic management of postoperative ileocolonic anastomotic bleeding by using water submersion. Gastrointest Endosc. 2011;74:721-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 67. | Luo M, Shan H, Zhou K. CT virtual colonoscopy in patients with incomplete conventional colonoscopy. Chin Med J (Engl). 2002;115:1023-1026. [PubMed] |
| 68. | Mizukami T, Ogata H, Hibi T. “Passive-bending colonoscope” significantly improves cecal intubation in difficult cases. World J Gastroenterol. 2012;18:4454-4456. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 69. | Sato K, Shigiyama F, Ito S, Kitagawa T, Tominaga K, Suzuki T, Maetani I. Colonoscopy using a small-caliber colonoscope with passive-bending after incomplete colonoscopy due to sharp angulation or pain. Surg Endosc. 2013;27:4171-4176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 70. | Hoff G, Bretthauer M, Huppertz-Hauss G, Sauar J, Paulsen J, Dahler S, Kjellevold Ø. Evaluation of a novel colonoscope designed for easier passage through flexures: a randomized study. Endoscopy. 2005;37:1123-1126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 71. | Saito Y, Kimura H. Responsive insertion technology. Dig Endosc. 2011;23 Suppl 1:164-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 72. | Mizukami T, Suzuki H, Hibi T. Classification and treatment of irritable bowel syndrome (IBS) based on colonoscopy abnormal bowel motility type and abnormal bowel morphology type. Gastroenterology. 2010;138 Suppl 1:S233 (meeting abstract). [DOI] [Full Text] |
| 73. | Mizukami T, Horiuchi Y, Mori N, Matsuo Y, Nagakubo S, Morohoshi Y, Hara Y, Komatsu H, Suzuki H, Hibi T. Endoscopic evaluation of colonic movement after the administration of a spasmolytic drug to irritable bowel syndrome patients: application to diagnosis and therapy. J Psychosom Digest Dis. 2009;16:91-97 (in Japanese). |
| 74. | Mizukami T, Suzuki H, Hibi T. Colonoscopic examination on Irritable Bowel Syndrome (IBS) patients: Abnormal bowel motility type and abnormal bowel morphology type. J Psychosom Digest Dis. 2010;17:33-39 (in Japanese). |
| 75. | Johannesson E, Simrén M, Strid H, Bajor A, Sadik R. Physical activity improves symptoms in irritable bowel syndrome: a randomized controlled trial. Am J Gastroenterol. 2011;106:915-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 216] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 76. | Longstreth GF, Yao JF. Irritable bowel syndrome and surgery: a multivariable analysis. Gastroenterology. 2004;126:1665-1673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 155] [Article Influence: 7.4] [Reference Citation Analysis (0)] |