Published online Jan 14, 2015. doi: 10.3748/wjg.v21.i2.688
Peer-review started: June 5, 2014
First decision: July 9, 2014
Revised: September 4, 2014
Accepted: September 30, 2014
Article in press: September 30, 2014
Published online: January 14, 2015
Processing time: 227 Days and 21.4 Hours
Intussusception is rarely reported in adult patients with acute leukemia. We report a case of intussusception in a 29-year-old woman with acute myeloid leukemia (AML). She developed right lower quadrant pain, fever, and vomiting on day 16 of induction chemotherapy. Physical examination showed tenderness and guarding at the right lower quadrant of the abdomen. Abdominal computed tomography (CT) showed distension of the cecum and ascending colon, which were filled with loops of small bowel, and herniation of the ileocecal valve into the cecum. We proceeded to laparotomy and revealed ileocecal intussusception with the ileocecal valve as the leading point. The terminal ileum was thickened and invaginated into the cecum, which showed gangrenous changes. Right hemicolectomy was performed and microscopic examination of the colonic tissue showed infiltration of leukemic cells. The patient recovered after the operation and was subsequently able to continue treatment for AML. This case demonstrates that the diagnosis of intussusception is difficult because the presenting symptoms can be non-specific, but abdominal CT can be informative for preoperative diagnosis. Resection of the involved bowel is recommended when malignancy is suspected or confirmed. Intussusception should be considered in any leukemia patients presenting with acute abdomen. A high index of clinical suspicion is important for early diagnosis.
Core tip: Gastrointestinal complications are common in patients with acute leukemia, but intussusception is rarely reported in adult leukemia patients. Previous reports have mainly been in children with leukemia. We report a case of intussusception in an adult after chemotherapy for acute myeloid leukemia (AML). A 29-year-old woman with AML presented with fever, vomiting and right lower quadrant pain. Abdominal computed tomography showed features of intussusception. Resection of the involved bowel was performed and the patient recovered from the operation. A high index of clinical suspicion is important for early diagnosis.
- Citation: Law MF, Wong CK, Pang CY, Chan HN, Lai HK, Ha CY, Ng C, Yeung YM, Yip SF. Rare case of intussusception in an adult with acute myeloid leukemia. World J Gastroenterol 2015; 21(2): 688-693
- URL: https://www.wjgnet.com/1007-9327/full/v21/i2/688.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i2.688
Gastrointestinal complications are common in patients with acute leukemia. They can be due to leukemic invasion of the bowel, an altered immune state, or the toxicity of chemotherapy[1]. Intussusception is the telescoping of one segment of the gastrointestinal tract into an adjacent one, and it is more common in children than in adults[2,3]. It is rarely reported in adult patients with acute leukemia and there is only one other case report of intussusception in an adult patient with AML, confirmed by bone marrow examination[4].
We report a case of intussusception in an adult with acute myeloid leukemia (AML). Although this complication is rare in adults, it should be considered as a differential diagnosis in patients with acute leukemia presenting with abdominal pain.
A 29-year-old woman was diagnosed with AML, confirmed by bone marrow examination, which showed AML with maturation (WHO classification) and poor-risk cytogenetics. She was given induction chemotherapy with daunorubicin 60 mg/m2 daily for 3 d and cytarabine 100 mg/m2 daily for 7 d. On day 16 of induction treatment, she developed right lower quadrant pain, fever, and vomiting. There was no history of prior surgery. Physical examination showed tenderness and guarding at the right lower quadrant of the abdomen, but no palpable abdominal mass. Bowel sounds were normal.
Blood tests showed that the patient’s white cell count was 0.3 × 109/L (normal: 4.0 × 109-9.7 × 109/L), hemoglobin 7.0 g/dL (normal: 11.9-15.1 g/dL), and platelet count 15 × 109/L (normal: 150 × 109-384 × 109/L). Liver and renal function tests were normal, and testing for HIV antibody was negative. Blood cultures were taken and the patient was given an intravenous injection of empirical broad-spectrum antibiotic.
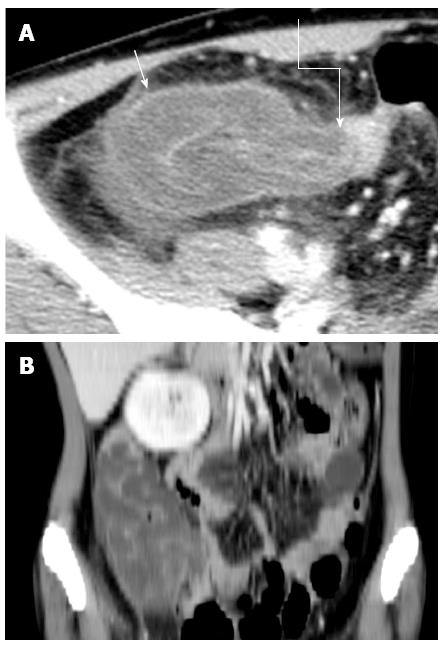
Abdominal computed tomography (CT) showed that the cecum and ascending colon appeared distended and filled with loops of small bowel (Figure 1). The ileocecal valve was herniated into the cecum. The wall of the ascending colon and cecum appeared thickened, and adjacent stranding was noted around the cecum, likely due to inflammation. The transverse colon appeared collapsed and the proximal small bowel was dilated with increased air-fluid level. Intussusception was suspected and emergency surgery was performed.
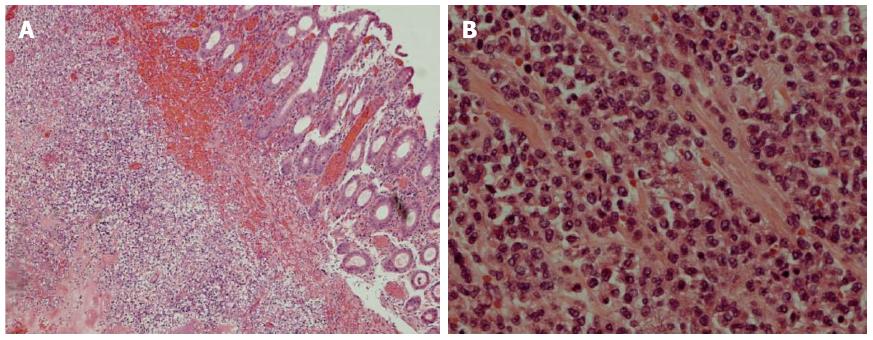
Laparotomy revealed ileocecal intussusception with the ileocecal valve as the leading point. The terminal ileum was thickened and invaginated into the cecum, which showed gangrenous changes. Right hemicolectomy was performed and a 5-cm long segment of ileum and a 5-cm long segment of ascending colon were examined. Macroscopic examination showed a mass 2 cm from the ileocecal junction. The mass had a whitish/brownish cut surface and was firm in consistency. The mucosal surface of the cecum and colon appeared edematous. Microscopic examination of the mass and colonic tissue showed that the submucosal and muscle layers were extensively infiltrated by leukemic cells. The cells were medium sized with irregular nuclear membranes and scanty cytoplasm (Figure 2). The cells were immunoreactive to myeloperoxidase, which is a myeloid marker.
The patient developed a wound infection after the operation. She was treated with a course of antibiotics and the wound infection improved. The patient was subsequently able to continue treatment of AML.
Intussusception is the telescoping of a proximal segment of the gastrointestinal tract within the lumen of the adjacent segment[2]. This condition is uncommon in adults and the diagnosis is usually made at laparotomy[3]. Most cases of adult intussusception involve the small or large bowel, but it sometimes occurs in the stomach or a surgically created stoma[3,5]. Intussusception may occur at sites of benign or malignant lesions, or may be idiopathic[6].
Intussusception is rarely reported in adult patients with acute leukemia, and previous reports have almost exclusively been in pediatric leukemia patients[7-15]. We identified only one other case report of intussusception in an adult patient with AML, who presented with small bowel obstruction[4]. Table 1 shows the features of previously reported cases of intussusception in acute leukemia in the literature and our present case. Adults with acute leukemia who develop intussusception present with abdominal pain or features of intestinal obstruction, whereas in pediatric patients, the clinical features are usually abdominal pain, vomiting, diarrhea and sometimes fecal blood.
| Number | Age/sex | Underlying leukemia | Clinical features | Imaging findings | Treatment | Clinical outcome | Ref. |
| 1 | 5-yr/F | ALL | Abdominal pain, abdominal distension and constipation | X-ray showed fluid levels in bowel | Gastric suction, antibiotic therapy and supportive measures | Patient died. Autopsy showed most of the intussuscepted small bowel was gangrenous. An intramural hematoma was the leading point of the intussusceptum | Feldman et al[7] |
| 2 | 7-yr/M | ALL | Abdominal distension | Not available | No surgical intervention | Patient died and intussusception was diagnosed at autopsy | Dudgeon et al[8] |
| 3 | 4-yr/M | ALL | Abdominal pain, fever, vomiting and a right lower quadrant abdominal mass | Abdominal X-ray demonstrated small intestinal obstruction | At laparotomy, necrotic ileum and cecum were resected. A primary ileocolic anastomosis was performed. | Patient died with perforation of ileocolic anastomosis with peritonitis | Dudgeon et al[8] |
| 4 | 14-yr/M | ALL | Vomiting, intermittent abdominal pain | Barium enema demonstrated an intussusception in descending colon reduced to ileocecal valve | Laparotomy showed a necrotic ileo-ileal intussusception. An ileal resection with primary anastomosis was performed. | Patient died with perforation of ileocolic anastomosis with peritonitis | Dudgeon et al[8] |
| 5 | 11-yr/M | AML | Abdominal pain, vomiting and diarrhea | Abdominal X-ray showed air-fluid levels | Supportive treatment | Patient died of intussusception | Karakousis et al[9] |
| 6 | 4-yr/F | ALL | Abdominal pain and vomiting | Not available | Resection of the involved bowel | Patient died of intussusception | Karakousis et al[9] |
| 7 | 7-yr/F | ALL | Fever and colicky abdominal pain | X-ray showed dilated loops of small bowel | Surgical reduction of intussusception | Recovered from operation and continued treatment of acute leukemia | Micallef-Eynaud et al[10] |
| 8 | 13-yr/F | ALL | Abdominal distension, abdominal pain, vomiting, symptoms of bowel obstruction | Barium enema showed small bowel intussusception | Surgical excision of the involved bowel | Recovered from operation and continued treatment of acute leukemia | Seckl et al[11] |
| 9 | 7-mo/M | ALL | Abdominal distension, small bowel obstruction | CT scan showed small bowel obstruction | Surgical reduction of intussusception with resection of leading edge | Recovered from operation and continued chemotherapy for leukemia | Manglani et al[12] |
| 10 | 8-mo/ F | ALL | Vomiting, blood and mucus in stool | Abdominal X-ray showed increased gas shadows in small intestine | Reduction of ileocolic intussusception | Recovered from operation and continued treatment of acute leukemia | Kumari et al[13] |
| 11 | 3-yr/M | ALL | Abdominal pain, diarrhea, ileus | US showed thickened bowel loops with target lesion | Reduction of ileocolic intussusception | Patient died due to Escherischia coli septicemia | Gavan et al[14] |
| 12 | 7-yr/F | ALL | Fever and colicky abdominal pain | X-ray showed a soft tissue mass in right iliac fossa. US revealed target lesion | Reduction of intussusception | Recovered from operation and continued treatment of acute leukemia | Arestis et al[15] |
| 13 | 7-yr/F | ALL | Fever, diarrhea and colicky abdominal pain | US showed a target-shaped soft tissue mass in descending colon | Right hemicolectomy was performed | Recovered from operation and continued treatment of acute leukemia | Arestis et al[15] |
| 14 | 25-yr/M | AML | Epigastric pain and vomiting, intestinal obstruction | Not available, but laparotomy was performed and a segment of thickened ileum which had led to ileo-ileal intussusception was found | Ileo-ileal intussusception was resected to relieve obstruction | Patient died of leukemia | Kini et al[4] |
| 15 | 29-yr/F | AML | Right lower quadrant pain, fever, vomiting | CT scan showed that the cecum and ascending colon appeared distended and filled with loops of small bowel, and ileocecal valve was herniated into the cecum | Right hemicolectomy was performed | Recovered from operation and continued treatment of acute leukemia | Present case |
| 16 | 66-yr/M | CLL | Left lower abdominal pain | US showed a large round mass in the right mid- abdomen that had alternating hypoechoic and hyperechoic rings surrounding an echogenic center (doughnut sign) | There was no surgical intervention | Patient died of leukemia | Shim et al[25] |
A metastatic intestinal mass may act as the leading point of the intussusception[8]. Leukemia can produce a tumor mass by leukemic infiltration and hyperplasia of a polypoid nature or by intramural extravasation of blood with the formation of hematomas[7]. An intramural hematoma can be the leading point of each intussusceptum. Patients with acute leukemia usually have thrombocytopenia at presentation or after chemotherapy and are prone to hematoma formation.
Enlarged lymph nodes may also provide a leading point for intussusception in acute leukemia, because lymph node enlargement is common in patients with acute leukemia, particularly the lymphoblastic type[8]. Intussusception may also develop during induction chemotherapy from a leading point formed by leukemic filtrate, edema or necrosis[12].
The presenting symptoms of intussusception are non-specific in adult patients, but are generally chronic and consistent with partial obstruction[16]. Abdominal pain is the most common presenting symptom, followed by vomiting and bleeding from the rectum[6]. Patients may also present with an abdominal mass or intestinal obstruction[2,16].
Preoperative diagnosis of intussusception is difficult. Plain abdominal films may demonstrate features of intestinal obstruction and reveal the site of the obstruction[17]. Ultrasonography may show “pseudo-kidney” or “hay-fork” signs in the longitudinal view and “doughnut” or “target” signs in the transverse view[18]. The diagnostic accuracy of ultrasonography is dependent on the experience of the radiologist, and may be affected by obesity or the presence of massive air in the distended bowel loops.
Abdominal CT is the most useful investigation for making a preoperative diagnosis, especially in patients with non-specific abdominal pain, and it can help to assess the site and nature of the mass and the relationship to surrounding tissues. CT findings indicative of intussusception may include an apparent mass lesion, a crescent-like, eccentric, low-attenuation fatty mass or a rim of contrast material encircling the intussusceptum[19,20].
Adult intussusception requires surgical intervention[16]. However, there is still controversy regarding the extent of bowel resection, and whether reduction of the intussuscepted lesion should be attempted at operation. The potential risks of preliminary reduction of an intussuscepted bowel include perforation and seeding of tumor cells or microorganisms into the intra-abdominal cavity, venous tumor dissemination, and anastomotic complications of the edematous bowel tissue[21]. Therefore, it is recommended that resection is performed without attempting reduction when there are features of inflammation or ischemia of the bowel, or when malignancy is suspected or confirmed[21]. Our patient had ileocecal intussusception with underlying leukemia, and leukemic infiltration was suspected, so resection of the involved bowel was performed.
There have been several reports of successful surgical outcomes using the laparoscopic approach for adult intussusception[22-24]. The outcome of laparoscopic surgery is affected by the location and extent of the intussusception at diagnosis, the underlying cause, and the laparoscopic expertise of the surgeons.
In conclusion, intussusception is a rare complication in adult patients with acute leukemia. Diagnosis can be difficult because the presenting symptoms are often non-specific, but abdominal CT can be informative in making a preoperative diagnosis. Resection of the involved bowel is recommended. Intussusception should be considered in any leukemia patients presenting with acute abdomen. A high index of clinical suspicion is important for early diagnosis.
A 29-year-old woman with acute myeloid leukemia (AML) presented with abdominal pain, fever and vomiting, and was finally diagnosed with intussusception.
The clinical presentations of adult intussusception are non-specific and our patient presented with abdominal pain, fever and vomiting.
Other causes of acute abdomen such as intra-abdominal abscess and acute appendicitis were considered and these diagnoses were excluded by imaging.
Laboratory testing may not have been applicable in this case. The white cell count was not reliable because the patient received chemotherapy causing pancytopenia.
Contrast computed tomography showed the terminal ileum invaginating into the cecum. The wall of the cecum and ascending colon were thickened and edematous.
Biopsy of the resected specimen showed leukemic infiltration of the bowel.
Most cases of adult intussusception require surgical resection because the majority of cases are secondary to a pathological condition. The patient was treated with surgical resection of intussusception.
There is another case report of intussusception in an adult with AML who presented with epigastric pain, vomiting, and intestinal obstruction; surgery revealed ileo-ileal intussusception.
Intussusception is rarely reported in adult patient with acute leukemia in the literature and it is the uncommon term present in this case report.
Intussusception should be considered in adult patients with acute leukemia presenting with abdominal pain or intestinal obstruction.
The authors reported an interesting case of intussusception in an adult with acute myeloid leukemia occurred during induction chemotherapy. It is important to notice clinical suspicion of this entity, while this complication is rare.
P- Reviewer: Ashurst J, Namikawa T S- Editor: Qi Y L- Editor: Kerr C E- Editor: Wang CH
| 1. | Hunter TB, Bjelland JC. Gastrointestinal complications of leukemia and its treatment. AJR Am J Roentgenol. 1984;142:513-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 53] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, Vassiliou I, Theodosopoulos T. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009;15:407-411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 428] [Cited by in RCA: 507] [Article Influence: 31.7] [Reference Citation Analysis (2)] |
| 3. | Yalamarthi S, Smith RC. Adult intussusception: case reports and review of literature. Postgrad Med J. 2005;81:174-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 137] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 4. | Kini S, Amarapurkar A, Balasubramanian M. Small Intestinal Obstruction with Intussusception due to Acute Myeloid Leukemia: A Case Report. Case Rep Gastrointest Med. 2012;2012:425358. [PubMed] |
| 5. | Stubenbord WT, Thorbjarnarson B. Intussusception in adults. Ann Surg. 1970;172:306-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 104] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Reijnen HA, Joosten HJ, de Boer HH. Diagnosis and treatment of adult intussusception. Am J Surg. 1989;158:25-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 123] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Feldman BH, Schulaner FA. Intussusception as a cause of death in acute leukemia; report of a case. J Pediatr. 1963;63:463-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Dudgeon DL, Hays DM. Intussusception complicating the treatment of malignancy in childhood. Arch Surg. 1972;105:52-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Karakousis C, Holyoke ED, Douglass HO. Intussusception as a complication of malignant neoplasm. Arch Surg. 1974;109:515-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Micallef-Eynaud P, Eden OB. Intussusception in acute childhood lymphoblastic leukemia: an unusual complication. Pediatr Hematol Oncol. 1990;7:389-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Seckl MJ, Gregory MM, Watkins SM. Acute lymphoblastic leukaemia relapsing in bowel. Eur J Haematol. 1991;47:377-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Manglani MV, Rosenthal J, Rosenthal NF, Kidd P, Ettinger LJ. Intussusception in an infant with acute lymphoblastic leukemia: a case report and review of the literature. J Pediatr Hematol Oncol. 1998;20:467-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Kumari TP, Mohan SV, Shanavas A, Kumari PK. Intussusception at the onset of acute lymphoblastic leukemia in a child. Indian Pediatr. 1998;35:470-472. [PubMed] |
| 14. | Gavan DR, Hendry GM. Colonic complication of acute lymphoblastic leukaemia. Br J Radiol. 1994;67:449-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Arestis NJ, Mackinlay GA, Hendry GM. Intussusception in children with ALL receiving chemotherapy for acute lymphoblastic leukaemia. Pediatr Blood Cancer. 2005;45:838-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226:134-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 648] [Cited by in RCA: 666] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 17. | Cerro P, Magrini L, Porcari P, De Angelis O. Sonographic diagnosis of intussusceptions in adults. Abdom Imaging. 2000;25:45-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Boyle MJ, Arkell LJ, Williams JT. Ultrasonic diagnosis of adult intussusception. Am J Gastroenterol. 1993;88:617-618. [PubMed] |
| 19. | Gayer G, Apter S, Hofmann C, Nass S, Amitai M, Zissin R, Hertz M. Intussusception in adults: CT diagnosis. Clin Radiol. 1998;53:53-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 116] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 20. | Gayer G, Zissin R, Apter S, Papa M, Hertz M. Pictorial review: adult intussusception--a CT diagnosis. Br J Radiol. 2002;75:185-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 164] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 21. | Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 384] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 22. | Ishibashi Y, Yamamoto S, Yamada Y, Fujita S, Akasu T, Moriya Y. Laparoscopic resection for malignant lymphoma of the ileum causing ileocecal intussusception. Surg Laparosc Endosc Percutan Tech. 2007;17:444-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Akatsu T, Niihara M, Kojima K, Kitajima M, Kitagawa Y, Murai S. Adult colonic intussusception caused by cecum adenoma: successful treatment by emergency laparoscopy: report of a case. Surg Today. 2007;37:694-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Palanivelu C, Rangarajan M, Senthilkumar R, Madankumar MV. Minimal access surgery for adult intussusception with subacute intestinal obstruction: a single center’s decade-long experience. Surg Laparosc Endosc Percutan Tech. 2007;17:487-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | Shim CS, Kim JO, Cheon YK, Cho JY, Lee JS, Lee MS. A case of chronic lymphocytic leukemia-complicated colonic intussusception. Gastrointest Endosc. 2001;54:77-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |