Published online May 7, 2015. doi: 10.3748/wjg.v21.i17.5281
Peer-review started: October 18, 2014
First decision: November 14, 2014
Revised: January 26, 2015
Accepted: March 19, 2015
Article in press: March 19, 2015
Published online: May 7, 2015
Processing time: 208 Days and 17.7 Hours
AIM: To compare closure methods, closure times and medical costs between two groups of patients who had post-endoscopic resection (ER) artificial ulcer floor closures.
METHODS: Nineteen patients with duodenal adenoma, early duodenal cancer, and subepithelial tumors that received ER between September 2009 and September 2014 at Kagawa University Hospital and Ehime Rosai Hospital, an affiliated hospital of Kagawa University, were included in the study. We retrospectively compared two groups of patients who received post-ER artificial ulcer floor closure: the conventional clip group vs the over-the-scope clip (OTSC) group. Delayed bleeding, procedure time of closure, delayed perforation, total number of conventional clips and OTSCs and medical costs were analyzed.
RESULTS: Although we observed delayed bleeding in three patients in the conventional clip group, we observed no delayed bleeding in the OTSC group (P = 0.049). We did not observe perforation in either group. The mean procedure times for ulcer closure were 33.26 ± 12.57 min and 9.71 ± 2.92 min, respectively (P = 0.0001). The resection diameters were 18.8 ± 1.30 mm and 22.9 ± 1.21 mm for the conventional clip group and the OTSC group, respectively, with significant difference (P = 0.039). As for medical costs, the costs of all conventional clips were USD $1257 and the costs of OTSCs were $7850 (P = 0.005). If the post-ER ulcer is under 20 mm in diameter, a conventional clip closure may be more suitable with regard to the prevention of delayed perforation and to medical costs.
CONCLUSION: If the post-ER ulcer is over 20 mm, the OTSC closure should be selected with regard to safety and reliable closure even if there are high medical costs.
Core tip: Duodenal postoperative exposure of the artificial ulcer floor to pancreatic juice and bile acid induces delayed perforation. There are, however, no reports on comparisons of closure methods, closure times and medical costs according to the different methods for closure of artificial ulcer floors. If the post-endoscopic resection (ER) ulcer is under 20 mm in diameter, the conventional clip closure might be more suitable with regard to the prevention of delayed perforation and to medical costs. If the post-ER ulcer is over 20 mm, the over-the-scope clip closure should be selected with regard to safety and reliable closure even if there are high medical costs.
- Citation: Mori H, Ayaki M, Kobara H, Fujihara S, Nishiyama N, Matsunaga T, Yachida T, Masaki T. Suitable closure for post-duodenal endoscopic resection taking medical costs into consideration. World J Gastroenterol 2015; 21(17): 5281-5286
- URL: https://www.wjgnet.com/1007-9327/full/v21/i17/5281.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i17.5281
Primary duodenal adenoma and cancer reportedly account for approximately 0.02%-0.04%[1] and 0.035%-0.12%[2,3] of all gastrointestinal neoplastic lesions, respectively, whereas the frequency of duodenal neuroendocrine tumors (e.g., carcinoid tumors) has been reported to be 0.5%[4-6]. In recent years, esophageal, gastric, and colorectal endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) have been gradually developed and are sometimes performed for duodenal tumors. Early duodenal cancers remaining inside of the mucosa with no lymph node metastasis are an indication for endoscopic resection (ER)[7]. However, because the duodenum is fixed on the retroperitoneum with two bending portions (the superior and lower duodenal angles), in many cases, it is difficult to secure the visual field for conducting endoscopy, to manipulate the endoscope, and to appropriately set the distance and angle of the knife with flexible endoscopes. In addition, it is difficult to obtain a mucosal bulge by local injection due to the presence of Brunner glands and a thin muscular layer. This procedure is associated with many operation-related complications, such as perforation. Because postoperative exposure of the artificial ulcer floor to pancreatic juice and bile acid induces delayed perforation, various closure methods for the ulcer floor have been reported[8]. However, there are currently no reports on comparisons of closure methods, closure times and medical costs according to different methods for closure of artificial ulcer floors after EMR or ESD. There have been many reports with regard to the usefulness of the over-the-scope clip (OTSC) system (Ovesco Endoscopy GmbH, Tüebingen, Germany) for perforation, bleeding and fistulas of the digestive tract. Thus, we compared the differences of two methods to close artificial ulcer floors using a conventional clip or OTSC after ER for duodenal tumors to prevent post-ER artificial ulcers from exposure to pancreatic juice and bile acid, which leads to delayed perforation.
Nineteen patients with duodenal adenoma, early duodenal cancer, and subepithelial tumors that received ER between September 2009 and September 2014 at Kagawa University Hospital and Ehime Rosai Hospital, an affiliated hospital of Kagawa University, were included in the study. The microvascular and surface patterns were examined preoperatively in all cases by magnifying narrow band imaging (NBI) using the highest magnification (approximately optical magnification × 80) for preoperative endoscopic diagnosis. In addition, a biopsy was conducted for histological diagnosis. The inclusion criteria were early duodenal cancer, adenomas with a diameter of < 20 mm or neuroendocrine tumors with a diameter of < 10 mm, and a World Health Organization (WHO) classification of up to Grade 1. The exclusion criterion was patients with suspected massive submucosal invasion detected by magnifying NBI and endosonography (EUS), in whom surgical resection was performed instead. These criteria are also recommended by the Japan Gastroenterological Society.
ER, especially ESD, was performed carefully to prevent perforation. Moreover, markings were made at the site close to the tumors after evaluating the periphery of the tumors in detail by magnifying NBI using a GIF TYPE H260Z (OLYMPUS Co., Tokyo, Japan) to minimize the postoperative ulcer floor as much as possible. Local injection with a liquid that was composed of > 50% concentrated hyaluronic acid was administered in all cases. When local injection resulted in an insufficient bulge, concentrated hyaluronic acid was used without dilution. A shallow incision was first made in the mucosa on the distal side, and the mucosa was subsequently detached from the proximal side after trimming the submucosa when possible. Because the duodenal muscular layer is very thin, the insufflation volume was adjusted so that the knife tip was parallel to the muscular layer when possible, and the electrification duration was shortened as much as possible. In addition, excessive countertraction on the muscular layer by the tip hood was avoided.
Because artificial ulcers after ER are exposed to pancreatic juice and bile acid, conventional clip closure, with or without a detainment snare, or closure with an OTSC was used for the post-ER artificial ulcer closure. Either conventional clipping or the OTSC system was selected as the closing method at the discretion of each operator (i.e., three endoscopists, each having treated > 100 cases of gastric ESD).
We retrospectively compared two groups of patients who received post-ER artificial ulcer floor closure: the conventional clip group vs the OTSC group. Delayed bleeding, procedure time of closure, delayed perforation, total number of conventional clips and OTSCs and medical costs were analyzed.
GIF TYPE Q260J and GIF TYPE H260Z (OLYMPUS. Co., Tokyo, Japan) endoscopes were used. A dual knife (KD-650L, OLYMPUS. Co., Tokyo, Japan) or IT knife 2 (KD-611L, OLYMPUS. Co., Tokyo, Japan) was used. A coagrasper (FD-410LR, OLYMPUS. Co., Tokyo, Japan) hemostatic forceps was used. The tip attachment employed was an Elastic Touch Attachment (TOP. Co., Tokyo, Japan). An ERBE VIO300D incisional device was used, and a UCR (OLYMPUS. Co., Tokyo, Japan) was used as the CO2 insufflation device.
All values are presented as the mean ± SD. Patient baselines statistics were analyzed using a Mann-Whitney U test. P values < 0.05 were considered statistically significant. All statistical analyses were performed using GraphPad Prism version 5 for Windows (Graph Pad Software, San Diego, CA, United States).
The mean age of the patients (13 men and 6 women) was 62.5 years. Table 1 shows the characteristics of the patients in both groups (i.e., conventional clip group vs OTSC group). The lesion sites were in the second portion and bulb in 10 cases and 2 cases in the conventional clip group, respectively and in 5 cases and 2 cases in the OTSC group, respectively. There were 8 cases and 4 cases in the conventional clip group that received EMR or ESD, respectively, and 4 cases and 3 cases in the OTSC group received EMR of ESD, respectively. There were no significant differences in baseline characteristic for both groups.
| Conventional clip group, n | Over-the-scope clip group, n | P value1 | |
| Patients | 12 | 7 | |
| Age (yr), mean ± SD | 62.5 ± 15.8 | 64.3 ± 13.7 | 0.20 |
| Sex, M/F | 8/4 | 5/2 | 0.42 |
| Location of lesions | |||
| 2nd portion | 10 | 5 | 0.31 |
| Bulb | 2 | 2 | 0.40 |
| Resection method (mean ± SD, min) | |||
| EMR | 8 (15.7 ± 3.68) | 4 (14.6 ± 4.57) | 0.52 (0.68) |
| ESD | 4 (45.7 ± 12.51) | 3 (55.7 ± 16.35) | 0.43 (0.43) |
Table 2 shows the results for the two groups. The lesion diameters obtained by pathologic examination were 12.5 ± 1.60 mm for the conventional clip group and 13.3 ± 1.74 mm for the OTSC group, with no significant difference (P = 0.14). The resection diameters were 18.8 ± 1.30 mm and 22.9 ± 1.21 mm for the conventional clip group and the OTSC group, respectively, with significant difference (P = 0.039).
| Conventional clip (n = 12) | Over-the-scope clip (n = 7) | P value1 | |
| Lesion diameter (mm), mean ± SD | 12.5 ± 1.60 | 13.3 ± 1.74 | 0.140 |
| Resection diameter (mm), mean ± SD | 18.8 ± 1.30 | 22.9 ± 1.21 | 0.039 |
| Delayed bleeding (POD 1-7) | 3 | 0 | 0.049 |
| Treatment measure for delayed bleeding | hemostatic forceps | - | - |
| Delayed perforation (POD 1-7) | 0 | 0 | - |
| Procedure time of ulcer closure (min), mean ± SD | 33.26 ± 12.57 | 9.71 ± 2.92 | 0.0001 |
| Clips, mean | 9.8 | 1.25 | 0.015 |
| Total clips | 121 | 10 | 0.002 |
| Cost of one clip (¥/$/€)2 | 975/9.56/7.01 | 80000/785/576 | 0.008 |
| Cost of all clips (¥/$/€)2 | 117975/1257/847 | 800000/7850/5760 | 0.005 |
| Pathological diagnosis | |||
| Adenoma | 7 | 4 | 0.410 |
| Tubular adenocarcinoma | 4 | 2 | 0.390 |
| Leiomyoma | 1 | 0 | 0.810 |
| Carcinoid | 0 | 1 | 0.810 |
Although we observed delayed bleeding until day 7 after ER in 3 patients in the conventional clip group, we observed no delayed bleeding in the OTSC group (P = 0.049). We controlled the bleeding using hemostatic forceps, and we observed no subsequent bleeding. We did not observe perforation in either group. The mean procedure time for ulcer closure was 33.26 ± 12.57 min in the conventional clip group and 9.71 ± 2.92 min in the OTSC group, which showed a significant difference (P = 0.0001; Table 2).
As for medical costs, one clip costs ¥975, USD $9.56, or €7.01, and complete closure of an artificial ulcer required an average of 9.8 clips in the conventional clip group; one OTSC costs ¥80000, $US 785, or €576, and complete closure of an artificial ulcer required an average of 1.25 OTSCs in the OTSC group (P = 0.008; Table 2). The total of 121 conventional clips were used in the conventional clip group, and 10 OTSCs were used in the OTSC group. Therefore, the costs of all conventional clips were ¥117975, $1257, and €847, and the costs of all OTSCs were ¥800000, $7850, €5760, resulting a significant difference (P = 0.005; Table 2). In the histopathological examinations, we observed no significant differences between the groups in the proportions of adenoma, tubular adenocarcinomas, leiomyoma and carcinoids.
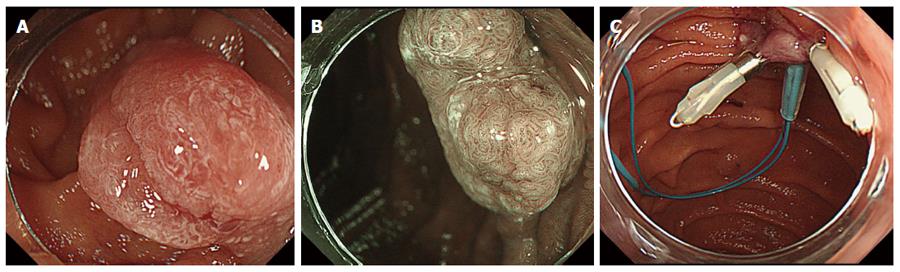
Figure 1 shows representative white light magnified endoscopic images with an irregular microsurface pattern (Figure 1A), and magnifying NBI images with an irregular microvascular pattern (Figure 1B), and an ulcer floor closure with a detainment snare and conventional clips (Figure 1C).
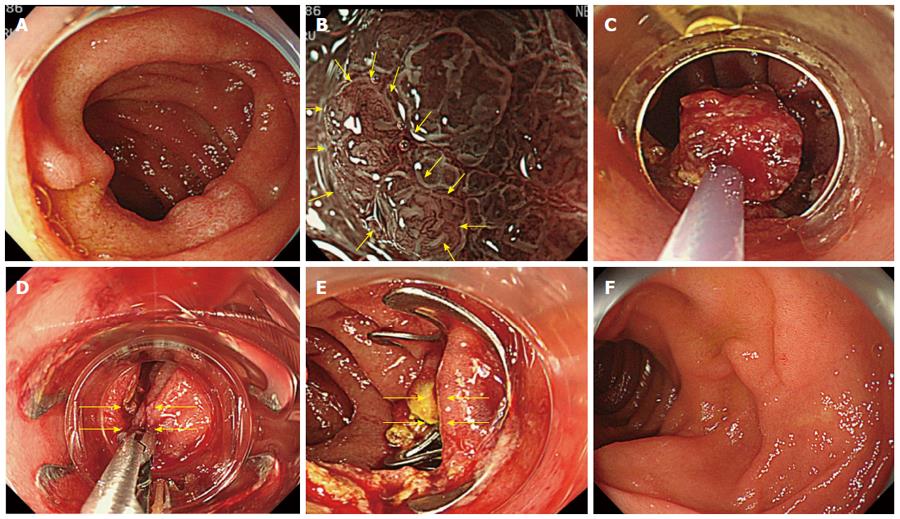
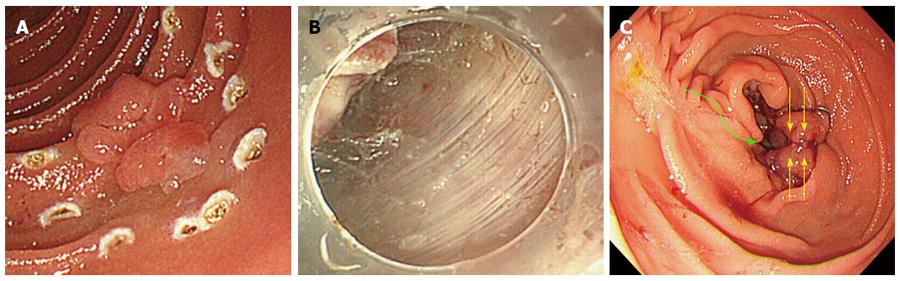
Figures 2 and 3 show representative white light endoscopic images (Figures 2A and 3A), magnifying NBI images (Figure 2B), resection by EMR (Figure 2C), resection by ESD (Figure 3B), and post-ER artificial ulcer closure by OTSC (Figures 2D, E and 3C). The OTSC was not visible on the ulcer floor, which had recovered within the mucosa with chorioepithelium 6 mo later without stricture (Figure 2F).
Improvement in the ESD technique and the development of safe devices have allowed conventional resections by EMR and en bloc resections by ESD of duodenal neoplastic lesions. However, intraoperative perforation has been reported to occur with very high frequency compared with that in esophageal, gastric, and colorectal ESDs, indicating a high degree of difficulty in duodenal ESD[9-11]. Moreover, the incidence of delayed perforation has been reported to be as high as 6%-7%. For the prevention of delayed perforation, it is necessary to close and reef the ulcer floor because artificial ulcer floors are exposed to digestive juices, such as pancreatic juice and bile acid, after resection[12]. The placement of endoscopic nasobiliary drainage (ENBD) and endoscopic nasopancreatic drainage (ENPD) and the administration of pancreatic enzyme inhibitors have been reported to be effective[13]. However, it is difficult to postoperatively insert ENBD or ENPD in every case due to the high risk of detachment of the thin myenteric parts because of overstressing the artificial ulcer floor after ESD. In addition, insertion before ESD is also likely to be difficult because of the drainage tube, which acts as an additional obstacle to endoscopic manipulation during ESD.
In a report by Ono et al at the Conference of Japan Gastroenterological Endosocpy Society on a multicenter questionnaire survey conducted in 13 facilities in Japan, the intraoperative and delayed perforation rates were 9.3% and 3.1%, respectively, resulting in a 12% total perforation rate. Intraoperative perforation occurred in 3.9% and 24% of EMR and ESD cases, respectively, whereas delayed perforation occurred in 1.2% and 6% of EMR and ESD cases, respectively.
In terms of delayed bleeding and procedure times, the conventional clip closure was significantly inferior to the OTSC closure. With close follow-up observation, delayed bleeding is certainly controllable with a hemostatic forceps, and the procedure time of the conventional clip is within a tolerable time. Therefore, both methods are suitable for post-ER prophylactic treatment.
With regard to delayed perforation, because the conventional clip closure and the OTSC closure showed no significant difference, both methods are suitable for post-ER closure. When closing 20-mm or larger artificial ulcer floors with normal clips and a detainment snare, a gap is generated between the clips, leading to exposure to digestive juices. The OTSC system is considered very effective and safe for the closure of artificial ulcer floors because single reefing strongly closes the floor in the system. However, there is a notable disadvantage with the OTSC closure. The costs of all OTSCs were 6- to 7-times more expensive than that of conventional clips. In terms of medical costs, this difference cannot be ignored.
In conclusion, if the post-ER ulcer is under 20 mm in diameter, the conventional clip closure might be more suitable with regard to the prevention of delayed perforation and to medical costs. However, if the post-ER ulcer is over 20 mm in diameter, the OTSC closure should be selected with regard to safety and reliable closure even if there are high medical costs.
We would like to thank Dr. Makoto Oryu for technical and editorial assistance.
Duodenal postoperative exposure of the artificial ulcer floor to pancreatic juice and bile acid induces delayed perforation. Because the indication for endoscopic resection (ER) for duodenal tumors has been controversial, in recent years, ER has been performed gradually. As postoperative exposure of the artificial ulcer floor to pancreatic juice and bile acid induces delayed perforation, there are currently no reports on comparisons of closure methods, closure times and medical costs.
There are no reports on comparisons of closure methods, closure times and medical costs according to the different methods for closure of artificial ulcer floors of post-Endoscopic resection.
There have been many reports with regard to the usefulness of the over-the-scope clip (OTSC) system for perforation, bleeding and fistulas of the digestive tract. Thus, the authors compared the differences of two methods to close artificial ulcer floors using a conventional clip or OTSC after ER for duodenal tumors to prevent post-ER artificial ulcers from exposure to pancreatic juice and bile acid, which leads to delayed perforation.
If the post-ER ulcer is over 20 mm, the OTSC closure should be selected with regard to safety and reliable closure even if there are high medical costs.
The over-the-scope clip system is used for perforation, bleeding and fistulas of the digestive tract.
This report compares the closure methods, i.e., conventional clip vs OTSC, following ER for duodenal tumors. Based on the results obtained with 19 patients, the authors concluded that if post-ER ulcer is under 20 mm diameter, a conventional closure may be more suitable. However, with ulcer > 20 mm, the OTSC closure should be selected. The manuscript is informative, well written, and supported by the tables and pictures. Hence, in my opinion, it deserves priority publishing.
P- Reviewer: Slomiany BL S- Editor: Yu J L- Editor: A E- Editor: Ma S
| 1. | Morrison WA, Donath D. Tumors of the Small Intestine. Cal West Med. 1941;55:235-237. [PubMed] |
| 2. | Burgerman A, Baggenstoss AH, Cain JC. [Primary malignant neoplasms of the duodenum, exclusing the papilla of vater; a clinicopathologic study of 31 cases]. Gastroenterology. 1956;30:421-431. [PubMed] |
| 3. | Hung FC, Kuo CM, Chuah SK, Kuo CH, Chen YS, Lu SN, Chang Chien CS. Clinical analysis of primary duodenal adenocarcinoma: an 11-year experience. J Gastroenterol Hepatol. 2007;22:724-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Mullen JT, Wang H, Yao JC, Lee JH, Perrier ND, Pisters PW, Lee JE, Evans DB. Carcinoid tumors of the duodenum. Surgery. 2005;138:971-97; discussion 977-978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 78] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 5. | Soga J. Carcinoids and their variant endocrinomas. An analysis of 11842 reported cases. J Exp Clin Cancer Res. 2003;22:517-530. [PubMed] |
| 6. | Modlin IM, Kidd M, Latich I, Zikusoka MN, Shapiro MD. Current status of gastrointestinal carcinoids. Gastroenterology. 2005;128:1717-1751. [PubMed] |
| 7. | Alexander S, Bourke MJ, Williams SJ, Bailey A, Co J. EMR of large, sessile, sporadic nonampullary duodenal adenomas: technical aspects and long-term outcome (with videos). Gastrointest Endosc. 2009;69:66-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 120] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 8. | Mori H, Shintaro F, Kobara H, Nishiyama N, Rafiq K, Kobayashi M, Nakatsu T, Miichi N, Suzuki Y, Masaki T. Successful closing of duodenal ulcer after endoscopic submucosal dissection with over-the-scope clip to prevent delayed perforation. Dig Endosc. 2013;25:459-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Yamamoto H, Miura Y. Duodenal ESD: conquering difficulties. Gastrointest Endosc Clin N Am. 2014;24:235-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Inoue T, Uedo N, Yamashina T, Yamamoto S, Hanaoka N, Takeuchi Y, Higashino K, Ishihara R, Iishi H, Tatsuta M. Delayed perforation: a hazardous complication of endoscopic resection for non-ampullary duodenal neoplasm. Dig Endosc. 2014;26:220-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 135] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 11. | Jung JH, Choi KD, Ahn JY, Lee JH, Jung HY, Choi KS, Lee GH, Song HJ, Kim DH, Kim MY. Endoscopic submucosal dissection for sessile, nonampullary duodenal adenomas. Endoscopy. 2013;45:133-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 103] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 12. | Nishiyama N, Mori H, Kobara H, Rafiq K, Fujihara S, Kobayashi M, Oryu M, Masaki T. Efficacy and safety of over-the-scope clip: including complications after endoscopic submucosal dissection. World J Gastroenterol. 2013;19:2752-2760. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 101] [Cited by in RCA: 106] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 13. | Fedorov ED, Plakhov RV, Mikhaleva LM, Ivanova EV, Galkova ZV, Buntseva OA. [The results of endoscopic mucosal resection and submucosal layer endoscopic dissection in patients with superficial epithelial neoplasms of stomach and duodenum]. Eksp Klin Gastroenterol. 2011;65-72. [PubMed] |