Published online Apr 28, 2015. doi: 10.3748/wjg.v21.i16.5056
Peer-review started: July 27, 2014
First decision: September 15, 2014
Revised: September 18, 2014
Accepted: December 14, 2014
Article in press: December 22, 2014
Published online: April 28, 2015
Processing time: 274 Days and 10.2 Hours
AIM: To examine the available evidence on safety, competency and cost-effectiveness of nursing staff providing gastrointestinal (GI) endoscopy services.
METHODS: The literature was searched for publications reporting nurse endoscopy using several databases and specific search terms. Studies were screened against eligibility criteria and for relevance. Initial searches yielded 74 eligible and relevant articles; 26 of these studies were primary research articles using original datasets relating to the ability of non-physician endoscopists. These publications included a total of 28883 procedures performed by non-physician endoscopists.
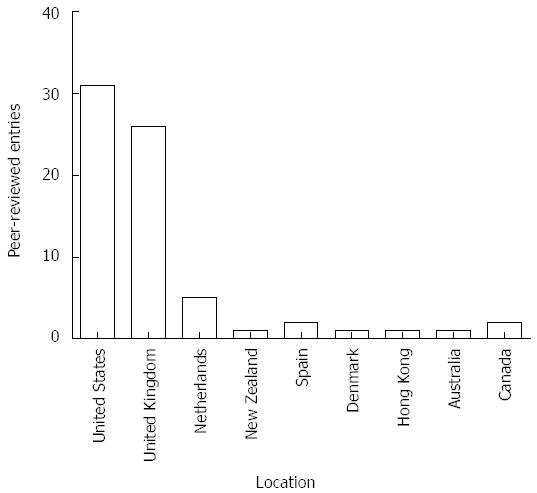
RESULTS: The number of publications in the field of non-specialist gastrointestinal endoscopy reached a peak between 1999 and 2001 and has decreased thereafter. 17/26 studies related to flexible sigmoidoscopies, 5 to upper GI endoscopy and 6 to colonoscopy. All studies were from metropolitan centres with nurses working under strict supervision and guidance by specialist gastroenterologists. Geographic distribution of publications showed the majority of research was conducted in the United States (43%), the United Kingdom (39%) and the Netherlands (7%). Most studies conclude that after appropriate training nurse endoscopists safely perform procedures. However, in relation to endoscopic competency, safety or patient satisfaction, all studies had major methodological limitations. Patients were often not randomized (21/26 studies) and not appropriately controlled. In relation to cost-efficiency, nurse endoscopists were less cost-effective per procedure at year 1 when compared to services provided by physicians, due largely to the increased need for subsequent endoscopies, specialist follow-up and primary care consultations.
CONCLUSION: Contrary to general beliefs, endoscopic services provided by nurse endoscopists are not more cost effective compared to standard service models and evidence suggests the opposite. Overall significant shortcomings and biases limit the validity and generalizability of studies that have explored safety and quality of services delivered by non-medical endoscopists.
Core tip: A systematic review was performed to examine the available evidence on safety, competency and cost-effectiveness of nursing staff providing gastrointestinal endoscopy services. Most studies conclude that after appropriate training nurse endoscopists safely perform procedures. Contrary to general beliefs, endoscopic services provided by nurse endoscopists are not more cost effective compared to standard service models due largely to the increased need for subsequent endoscopies, specialist follow-up and primary care consultations. The empirical evidence that supports non-physician endoscopists is limited to strictly supervised roles in larger metropolitan settings and mainly flexible sigmoidoscopy and upper endoscopy for asymptomatic or low complexity patients.
- Citation: Stephens M, Hourigan LF, Appleyard M, Ostapowicz G, Schoeman M, Desmond PV, Andrews JM, Bourke M, Hewitt D, Margolin DA, Holtmann GJ. Non-physician endoscopists: A systematic review. World J Gastroenterol 2015; 21(16): 5056-5071
- URL: https://www.wjgnet.com/1007-9327/full/v21/i16/5056.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i16.5056
Nurse endoscopy training and delivery of endoscopic services was first reported in the United States more than 35 years ago for flexible sigmoidoscopy (FS)[1]. Several studies soon emerged, confirming that nursing staff with appropriate training and supervision could adequately perform endoscopic procedures such as FS. Other studies have since established that nurse endoscopists can safely perform upper endoscopies and colonoscopies. In an era where safe, yet cost-effective, policies run at the forefront of stakeholders’ minds, the question of how nursing staff can undertake additional roles in the endoscopic suites is continually raised. After more than 35 years, it appears timely to review the available evidence surrounding the role of nurse endoscopists. To our knowledge, there have been no systematic reviews of the literature that have examined the full body of evidence surrounding uptake, safety, accuracy and most importantly, the cost-effectiveness of nurse endoscopists.
Competent endoscopy has both procedural (manual dexterity) and cognitive aspects. Procedural skills refer to the ability of endoscopists to insert/withdraw the endoscope, navigate the alimentary tract with acceptable views and perform further actions such as biopsy, polypectomy or other interventions. Procedural (technical) competence necessitates that these actions are executed in a timely manner that exposes the patient to acceptable risk of complications. Procedural or technical skill is generally measured by direct observation of the procedure[2] alongside several quality indicators such as overall procedural time, caecal intubation time, caecal intubation rate, polyp/adenoma detection rate, depth of insertion, adequacy of views on review of video footage, rate of complications and patient satisfaction.
On the other hand, cognitive (or non-technical) skill refers to the ability of endoscopists to perform more complex tasks beyond the procedure itself. These include: (1) recognizing and interpreting gross pathology; (2) interpreting the patient’s clinical picture in relation to endoscopic findings; (3) understanding the patient’s current clinical risk and how this could change with/without further endoscopic treatment; (4) knowledge of any viable alternatives to endoscopic procedures that could better serve the patient; (5) recommending treatments/further investigations appropriate to the severity of pathology seen; and finally; and (6) understanding the indications and contraindications for the proposed procedure.
These cognitive elements are important during the composition of the report and any follow-up by the endoscopists, as well as during the procedure itself. By their nature, the cognitive aspects of endoscopy do not lend themselves towards easy measurement, especially when comparing competence between study groups. Assessment of endoscopists’ reports by consultant gastroenterologists (gold standard) after review of video footage has been performed with some merit, but assessment is often subjective and limited to measuring sensitivity and specificity of detecting simple gross pathology[3,4].
Physician and surgical trainees in gastroenterology and surgical specialities undergo extensive training before providing independent endoscopic services. This training addresses both the procedural and cognitive aspects of endoscopy, with procedural competency being obtained more rapidly compared to cognitive competency, which requires years of comprehensive clinical training. Indeed, many studies have shown that a high level of procedural competency for FS is typically achieved after around 100-200 supervised procedures, with higher numbers needed for colonoscopy/upper endoscopy.
This applies regardless of whether the trainees are junior doctors, advanced trainees, fellows, or non-physician personnel[5-13]. It is unlikely however, that nurses and other non-physician endoscopists routinely acquire the same level of cognitive competency as physician endoscopists or other medically qualified and trained staff. This cognitive aspect, intrinsic to the procedure, requires the ability to make a well-reasoned decision within the context of the patient’s full clinical picture, to take responsibility for decisions made, to manage efficiently complications and to guide subsequent follow-up. This is a style of thinking which is fostered in physicians through years of training, yet generally not taught in nursing education, which tends to be more protocol based. On the other hand it might be argued that these cognitive skills are not required to perform a simple procedure, which requires a clearly defined but limited set of skills. However, from the perspective of the healthcare system as a whole, one needs to examine not only the actual procedure, but also all costs involved in its delivery, and this necessarily includes an evaluation of cost-effectiveness of the entire “episode of care”.
This systematic review aims to assess the current evidence to support the provision of diagnostic or therapeutic endoscopic services by trained non-physicians including nurses, and the evidence regarding cost-effective delivery of services that meet patient needs. We specifically aim to assess: (1) the evidence that non-physician endoscopists can acquire the required procedural and cognitive skills to deliver endoscopic services; (2) the cost-benefit analysis of procedures performed by nurses and other non-physicians as compared to medical and surgical specialists, and (3) characterize the service models that have been used so far.
We devised the following Boolean search terms: nurse and endoscopist (“nurse and performed” or “delivered”) or “nurse practitioner” and (“endoscopy” or “colonoscopy” or “flexible sigmoidoscopy” or “esophagogastroduodenoscopy”); (“non-medical” or “non-physician” or “non-medical” or “non-physician” or “physician assistant”) and “endoscopy”. We searched each of the following electronic databases using each of the above search terms individually: Cochrane Library; MEDLINE; CINAHL; Google Scholar. The most recent search was performed January 2014.
To be deemed eligible and relevant for inclusion in the review, studies/articles must have described or referred to non-medical personnel (i.e., nurses, physicians assistants, technicians, non-medical personnel or those not practicing as a doctor) being the primary proceduralists for any form of gastrointestinal endoscopy. Non-medical personnel needed to be included in the review as there is discrepancy in the terminology in literature. Studies that were solely focused on capsule endoscopy or nurses assisting in placing percutaneous endoscopic gastrostomy tubes were excluded from the systematic search part of the review. Studies were excluded if they were not published in a peer-reviewed journal. All languages and age ranges were included. There were no date limits.
For all eligible studies, any entries that were identified as “comments” on other articles were removed from any analyses. The remaining articles were stratified into “primary research measuring endoscopists’ performance” or “other”. For each primary research study, the following information was extracted: author names and year of publication, country of origin, total number of procedures performed by nurses/non-medical endoscopists, degree of supervision of endoscopists, clinical setting, whether there was true randomization of patients, number and type of proceduralists, potential biases, outcome parameters used by the study and important outcomes. If studies referred to other pieces of research or articles that were not discovered by the systematic search, but were eligible and relevant, they were also included in the review.
The number of publications (primary research or otherwise) by year, publications by country and total non-physician procedures reported were assessed. The data were extracted from the identified primary research articles independently by two of the authors (MS and GH). These data were compared and discrepancies assessed and agreement reached when required. The review of the data also included an assessment of the overall quality of the studies. For this assessment, key criteria such as randomization, concealment of randomization, the risk of selective reporting and other relevant indicators of bias[14] and study quality were assessed with the results tabulated in keeping with the Cochrane Collaboration’s Risk of Bias Assessment. A meta-analysis of the data was not possible due to the heterogeneity of the studies. Where original data were re-reported in second or third publications, only the original data were included.
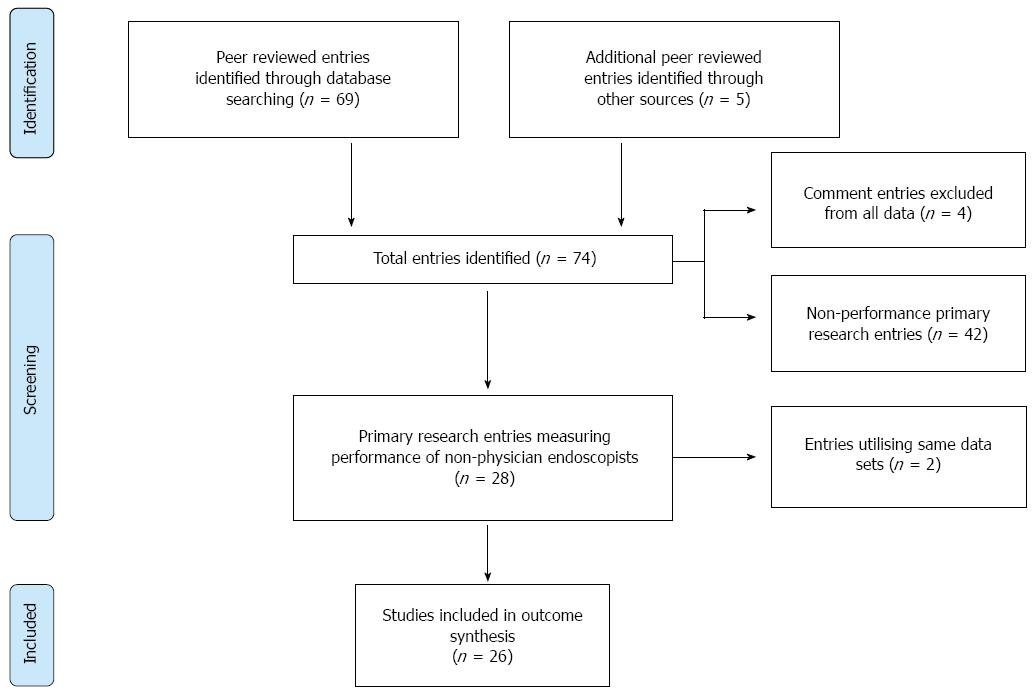
The literature search identified 74 publications, of which 4 were identified as “comments” and removed from any further analysis. Publications were dated between March 1977 and September 2013. In these 70 studies, a total of 28883 non-physician endoscopies had been documented. Twenty eight (40%) were identified as primary research measuring endoscopists’ performance with definable outcome parameters. Two studies re-reported original data and excluded leaving 26 studies suitable for further analysis (Figure 1 and Table 1). Of these primary research studies there were 17476 documented non-physician endoscopies (n = 17476).
| Publication | Setting | Non-physician proce-dures | Supervision | True randomization of patients? | Procedurists | Potential biases | Outcome parameters | Modality | Outcome |
| Rosevelt et al[8], 1984 | Metropolitan Tertiary Centre, United States | 825 | Yes | No | 1 NE | Patient selection biasEndoscopist selection biasLevel of assistance not documented | Polyp detection rateComplications | FS | Polyp detection rate of 8.7%No complications |
| Schroy et al[4], 1988 | Metropolitan Tertiary Centre, United States | 100 | Yes | No | 1 NE | Patient selection biasEndoscopist selection biasLevel of assistance not documentedConcordance criteria not given | Polyp detection rateConcordance of findings with expert opinion | FS | Polyp detection rate of 36%Video review showed k = 0.72 concordance with GCNurse sensitivity = 75%, specificity = 94% |
| DiSario et al[15], 1993 | Metropolitan Tertiary Centre, United States | 80 | Yes | Yes | 5 NEs5 GRs | Endoscopist selection biasLevel of assistance not documented1 NE excluded due to incompetency after trainingComparison of outcome groups for missed lesions not calculated | Insertion depthIdentification of anatomyComplicationsProcedure timeMissed lesions | FS | Polyp detection rate of 24%Insertion depth, complications and procedure time similar between groupsNEs missed more lesions and missed more anatomy |
| Maule[7], 1994 | Metropolitan Tertiary Centre, United States | 1881 | Yes | No | 4 NEs2 GCs | Endoscopist selection biasComplicated patient referred away from NEsLevel of assistance not documented | Insertion depthComplicationsPolyp detection ratePatient satisfaction | FS | GCs had significantly deeper insertion depthsSimilar polyp detection rateSimilar patient satisfaction |
| Moshakis et al[16], 1996 | Metropolitan Tertiary Centre, United Kingdom | 50 | Yes | No | 1 NE1 GC | Endoscopist selection biasPatient selection biasNE was compared to GC who performed trainingLevel of assistance not documentedMethod of quality scoring not given | Insertion depth“Quality and accuracy” | FS | Insertion depth, quality and accuracy were similar between comparison groups |
| Duthie et al[6], 1998 | Metropolitan Tertiary Centre, United Kingdom | 205 | Not specified | No | 1 NE | Endoscopist selection biasPatient selection biasCriteria for “successful procedure” not given | Successful procedure when compared to various other imaging modalities | FS | 93% of procedures considered “successful” |
| Schoenfeld, Cash et al[17], 1999 | Metropolitan Tertiary Centre, United States | 114 | Yes | No | 1 NE3 GFs3 Surgical Consultants | Endoscopist selection biasPatient selection biasLevel of assistance not documented | Depth of insertionProcedure timePolyp detection ratePatient satisfactionComplications | FS | Surgeons had less depth of insertion than NEs or GFsNEs had longer procedures than GFs or surgeonsPolyp detection rate similarNo complications |
| Schoenfeld, Lipscomb et al[10], 1999 | Metropolitan Tertiary Centre, United States | 151 | Yes | Yes | 3 NEs4 GCs | Endoscopist selection biasPatient selection biasLevel of assistance not documentedHigh threshold for detecting difference in polyp detection rate | Polyp detection rateDepth of insertionComplications | FS | Polyp detection rates similar between groups (43%-45%)GCs had much greater depth of insertionNo complications |
| Wallace et al[9], 1999 | Metropolitan Tertiary Centre, United States | 2323 | Yes | No | 1 NE2 PAs15 GCs | Endoscopist selection biasPatient selection biasLevel of assistance not documented | Depth of insertionPolyp detection rateComplications | FS | GCs had significantly greater depths of insertion compared with NE+PAsPolyp detection rate similar between groups (23%-27%)No complications |
| Schoen et al[26], 2000 | Metropolitan Tertiary Centre, United States | 660 | Not specified | No | 1 PE1 GC1 MC | Endoscopist selection biasPatient selection biasLevel of assistance not documented | Patient satisfaction | FS | Similar patient satisfaction between groups |
| Shapero et al[27], 2001 | Metropolitan Tertiary Centre, Canada | 488 | No | No | 2 NEs | Endoscopist selection biasPatient selection bias Level of assistance not documented | Polyp detection rateComplicationsDepth of insertionProcedure time | FS | Average depth of insertion 52.9 cm8.4 min average procedure timePolyp detection rate of 15.4% |
| Jain et al[28], 2002 | Metropolitan Tertiary Centre, United States | 5000 | No | No | Not specifiedNo physicians | Unknown endoscopistsPatient selection biasLevel of assistance not documentedNo comparison | Polyp detection rateNo complications | FS | No major complications polyp detection rate of 13.3% |
| Meenan et al[29], 2003 | Metropolitan Tertiary Centre, United Kingdom | 25 | Yes | No | 1 NE4 GFs | Endoscopist selection biasPatient selection biasLevel of assistance not documentedViews by NE were limited to the esophagus | Adequacy of views obtain by radial ultrasound by endoscopy | EGD | NEs had consistently lower quality scores |
| Smale et al[30], 2003 | Metropolitan Tertiary Centre, United Kingdom | 1487 | Yes | No | 2 NEs15 mixed medical/surgical physicians | Endoscopist selection biasPatient selection biasLevel of assistance not documentedComplicated patients excludedRetrospective and prospective | Differences in sedationPatient satisfaction | EGD | No difference between groups for sedation or patient satisfactionSubjectively, nurses reporter fewer studies as normal |
| Wildi et al[22], 2003 | Metropolitan Tertiary Centre, United States | 40 | Yes | No | 1 NE1GC | Endoscopist selection biasPatient selection biasLevel of assistance not documentedMethod of assessment not given | Concordance of findings with GC | EGD | NE had sensitivity of 75% and specificity of 98% with GC as gold standard |
| Nielsen et al[12], 2005 | Metropolitan Tertiary Centre, Denmark | 69 | Yes | No | 2 NEsUnknown number of physicians | Endoscopist selection biasPatient selection biasLevel of assistance not documented | Patient satisfaction | FS | Nurses had better patient satisfaction than physicians |
| Meining et al[3], 2007 | Metropolitan Tertiary Centre, United Kingdom | 190 | Yes | Yes | 2 NEs1 GC2 GRs1 Physician not specified1 MC | Endoscopist selection biasPatient selection biasLevel of assistance not documentedSubjectivey, nurses tended to focus on the entire examination whilst physicians focused on the reason for referral | Adequacy of views for entire procedureDuration of procedureUse of sedation | EGD | Nurses had twice the amount of adequate views however took twice as long on average.Nurses used sedation more frequently |
| Williams et al[19], 2006 Williams et al[21], 2009 | Nation-wide Metropolitan Tertiary Centres, United Kingdom | 957 | Yes | Yes | 30 NEs67 physicians (not specified) | Significantly higher numbers of patients changed schedule from physician to nurse (due | Patient satisfactionAdequacy of viewsDepth of insertionEndoscopic procedures performedDuration of examinationComplications | EGD | Patient satisfaction favoured nursesNo difference for depth of insertionNurses took biopsies for histology in upper endoscopy and FS more frequently than physicians.There were more normal histology findings for nurses |
| Richardson et al[20], 2009 | Need for assistanceNeed for subsequent follow up and investigationCost-benefit analysis | Nurses were more likely to report sedation and procedural details whilst physicians were more likely to report diagnosis and suggested treatment.Nurses took biopsies for H. pylori more frequentlyNo major differences in final diagnoses frequency between 2 groups.No serious complicationsSimilar need for assistance.Nurses had greater follow-up cost per procedure whilst physicians had greater labor costs per procedure.Physicians had greater overall costs per procedure but greater patient improvement.Physicians were 87% more likely to be cost-effective than nurse endoscopists. | |||||||
| Koornstra et al[11], 2009 | Metropolitan Tertiary Centre, Netherlands | 300 | Yes | No | 2 NEs1 GF1 GC | Endoscopist selection biasPatient selection biasLevel of assistance not documented | Caecal intubation rateCaecal intubation timeComplicationsPatient satisfaction | Col | Similar caecal intubation rates/times (80%-90%) between GF and NEs but much lower/longer than GC after 150 procedures.Patient satisfaction similar between GF and NEs, less than for GC.Similar complication rate. |
| Maslekar, Hughes et al[31], 2010 | Metropolitan Tertiary Centre, United Kingdom | 308 | Not specified | No | 1 NE1 PA/TSeveral physicians not specified | Endoscopist selection biasPatient selection biasLevel of assistance not documentedNE and PA/Ts had less colonoscopies more FS | ComplicationsPatient satisfaction | Col and FS | No difference between all 3 groups |
| Maslekar, Waudby et al[32], 2010 | Metropolitan Tertiary Centre, United Kingdom | 26 | Yes | No | 1 Surgical Registrar1 PA/T | Endoscopist selection biasPatient selection biasLevel of assistance not documentedPatients needing resection excluded | Accuracy of endoscopists to gauge position in colon | FS | PA/T accuracy of 70% with Registrars accuracy of 80%, not statistically significant. |
| Shum et al[18], 2010 | Metropolitan Tertiary Centre, HK | 119 | Yes | No | 1 NE | No comparison group | Mean procedure timeDepth of insertionComplications | FS | 9.4 min average procedure time53.5 cm average depth of insertionNo major complications |
| Limoges-Gonzalez et al[44], 2011 | Metropolitan Endoscopy Centre, United States | 50 | Yes | Yes | 1 NE2 GCs | Endoscopist selection biasLevel of assistance not documented | Adenoma detection rateCaecal intubation rateCaecal intubation timePatient satisfactionSedation useComplications | Col | Adenoma detection rate higher in NE (42%) than GCs (17%)All other parameters similar across both groups |
| de Jonge et al[33], 2012 | Multi-metropolitan tertiary centre, Netherlands | 162 | Not specified | No (retrospective) | 6 NEs113 Staff not specified including GCs, GFs, surgeons, MCs | Data was retrospective review of reports | Overall caecal intubation rateAdenoma detection rate | Col | NEs and GFs and GCs found more adenomas and had greater caecal intubation rates (94%) than nongastroenterology staff, especially surgical |
| van Putten et al[34], 2012 | Multi-metropolitan tertiary centre, Netherlands | 1000 | Yes | No | 10 NEs | Endoscopist selection biasPatient selection bias | Unassisted caecal intubation rateWithdrawal timeAdenoma detection rateAssistance requirementsPatient satisfactionComplications | Col | Unassisted caecal intubation rate of 94%23% of colonoscopies required assistance from GCWithdrawal time of 10 minAdenoma detection rate of 23%1 perforation and 1 onset of atrial fibrillation95% of patients satisfied with procedure |
| Massl et al[5], 2013 | Multi-metropolitan tertiary centre, Netherlands | 866 | Yes | No | 7 NEs8 GFs | Endoscopist selection biasNEs had significantly lower ASA scores on patientsLevel of assistance not reported | Unassisted caecal intubation rateCaecal intubation timeComplicationsPolyp detection rate | Col | Unassisted caecal intubation rate was significantly lower 77% for NE than GFs (88%).Polyp detection rate (45%), complications, withdrawal and intubation times were similar between groups.Crude cost-analysis showed a saving of €7.61 per colonoscopy where 1 GC supervises 3 NEs. Did not account for higher need for repeat colonoscopies due to incomplete procedures |
The key quality indicators of the studies are summarized in Table 2. There was a widespread lack of randomization or blinding of concealment. In addition some of these open, uncontrolled and unblinded studies[5-7,10,12,15-18] appear to represent descriptive “verifications” of training programs that were developed. Overall the quality of these studies was very limited.
| Publication | Sequence generation | Allocation concealment | Blinding of participants, personnel and outcome assessors | Incomplete outcome data | Selective outcome reporting | Other sources of bias | Study hypothesis and power calculation |
| Rosevelt[8], 1984 | No randomization | No | No | Not specified | Likely, report was intended to describe a successful training program | No hypothesis, no statistics | |
| Schroy et al[4], 1988 | No randomization, review of videotape | No | No | Not specified | Report of an established service model. Review of videotapes Quality assurance | No statistics | |
| DiSario[15], 1993 | Computer generated randomization | Not specified | No | Not specified | Aim was to demonstrate that “.registered nurses could be trained to perform the flexible sigmoidoscopy in a similar to resident physicians’ | Not powered to demonstrate equivalence, no formal power calculations | |
| Maule[7], 1994 | No randomization | Not specified | No | Not specified | The study was done to confirm that training of nurse endoscopists is feasible. | Hypothesis defined (no difference), no power calculation for equivalence study, oucome parameters not specified a priori | |
| Moshakis et al[16], 1996 | No randomization, no comparator | Not specified | No | Not specified | Report describes the successful training of one (1) nurse endoscopist | No hypotheses, no statistical analysis | |
| Duthie et al[6], 1998 | No randomization | No | No | Not specified | Evaluation of a training program that was developed and implemented by the authors (self-fulfilling prophecy) | Not evident | No hypothesis, no power calculation |
| Schoenfeld et al[17], 1999 | No randomization, patients allocated to the ‘first available provider’ | No | No | Not specified | No evidence | Not evident | Several outcome parameters specified, but no hypothesis tested, no power calculation for equivalence. |
| Schoenfeld et al[10], 1999 | Randomization of veterans referred for flexible sigmoidoscopy. Computer generated randomization | No | unknown | Not specified | Justifies the implemented clinical service model. | Several outcome parameters listed, but no specific hypothesis, power calculation provided (to identify differences, but not targeting equivalence) | |
| Wallace et al[9], 1999 | No randomization, nurse-coordinator assigned eligible patients to a physician or non-physician endoscopists based upon ‘daily staffing assignments and patient time preference’ | No | Unknown | Not specified | Justifies the implemented clinical service model. | No hypothesis stated, no power calculation | |
| Schoen et al[26], 2000 | No randomization | No | No | Not specified | Study targeted to demonstrate the good tolerability of flexible sigmoidoscopy | Gender distribution of patients was not equivalent across examiners, and the nurse practitioner did not have trainees working with her. | No hypothesis stated, no proper power calculation |
| Shapero et al[27], 2001 | No randomization, allocation not clear | No | No | Not specified | Data justify the implemented clinical practice | Data are generated in the setting of CRC screening with flexible sigmoidoscopy, highly selective cohort. | Not done |
| Jain et al[28], 2002 | No randomization | No | No | Not specified | Justification of implemented clinical practice | CRC screening utilizing flexible sigmoidoscopy, selective cohort | Not done |
| Meenan et al[29], 2003 | No randomization | No | No | Not specified | Assessement of training progress | Not done | |
| Smale et al[30], 2003 | No randomization, part one retrospective analysis of endoscopy data base, second part prospective data collection | No | No | Not specified | Review and justification of clinical practice | Not done | |
| Wildi et al[22], 2003 | No randomization | No | No | Not specified | Sequential procedures Nurse endoscopist followed by physyician, potential effect of sequence. | Not done | |
| Nielsen et al[12], 2005 | No randomization | No | No | Not specified | Quality assurance of existing training program | Not done | |
| Meining et al[3], 2007 | No details in relation to the randomization process are provided. Patients unequally allocated to endoscopist or nurse | No | No | Reported but uneven numbers of ‘Randomization failures (33 vs 0). Considerable number of patients excluded (only 367 out of 641 reported) | Review and justification of clinical practice | Primary outcome parameter was stated as “appropriate diagnosis”, this outcome parameter was not reported. | Not done |
| Williams et al[19], 2006 Williams et al[21], 2009 Richardson et al[20], 2009 | Randomization of patients to nurse or physician endoscopy | No | No | Properly reported | Primary outcome parameter not related to endoscopic. Measured with Gastrointestinal Symptoms Rating scale up to one year after procedure | Only patients suitable to be serviced by nurse endoscopists included. Numerically more patients from the nurse cohort were lost of follow-up without specified reasons (286 vs 269). A trend for more patients with weight loss in the physicians cohort, more patients in the physicians’’ cohort had previously barium enema (suggesting more chronic or relapsing symptoms) | Authors make reference to required sample sizes. Total number of patients completed was below the required sample size |
| Koornstra et al[11], 2009 | It is stated that patients were randomly allocated, no information is given on allocation. Proportion of inpatients lower in the nurse group. No evidence for ethic approval or consent of patients. Training of nurse and medical staff was not identical | No | No | No information provided | Multiple endpoints reported | The authors developed a training program and with their data they aimed to confirm that their training program delivered (self-fulfilling prophecy). | Not powered to verify equivalence |
| Maslekar et al[31], 2010 | Patients were allocated by administrative staff into the nurse or medical specialist group. | No | No | Incomplete response data cited as reason for exlusion (48/561 excluded), no intention to treat analysis | Study justifies an implemented service model that aims to address shortage of medical specialists | The instrument was unlikely to detect group differences. Variable mixture of flexible sigmoidoiscopy and colonoscopy across groups | No power calculation |
| Maslekar et al[32], 2010 | No randomization | No information given | No | Not reported | Justifies implemented service and training model | For flexible sigmoidoscopies the validity of the endoscopists impression of maximal extension was tested. A priori unlikely to identify difference. | No power calculation |
| Shum et al[18], 2010 | No randomizatiom, no comparator | No | No | No information provided | Justifies the implemented training model | No | |
| Limoges-Gonzalez et al[44], 2011 | It is stated that patients were randomly allocated, no information is given on allocation. | No | No | No information provided | Justifies the implemented service model | Postprocedure questionnaire was administered after (at least) 30 min of recovery. Drug effects likely to blunt potential differences | No power calculation |
| de Jonge et al[33], 2012 | Routine quality data were used, no randomization. | No | No | No information provided | Data were partly retrospective data, partly prospective data, no justification given. | ? | No power calculation |
| van Putten et al[34], 2012 | Allocation of patients by secretatial staff, no randomization | No | Not reported | Not specified | Justifies and implemented service model | Significant differences in comorbidities (more severe in the Gastroenterologists group), differences in source of referral. Outcome assessment limited to immediate salary comparisons not total costs including pathology and follow-up. | No power calculation |
| Massl et al[5], 2013 | It is stated that patients allocated by administrative staff, endoscopists assigned to lists randomly based on availability | No | No | 79/2025 procedures not included due to drop out of 1 nurse endoscopist for unspecified reasons | Justifies the implemented service model | Patients younger than 18 years or referred for therapeutic procedures were excluded from the nurse endoscopist group only. Drop out of nurse endoscopist not justified. | Power calculation done.Appropriate numbers achieved. |
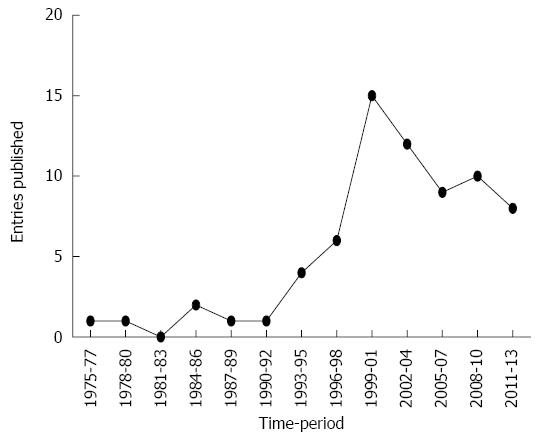
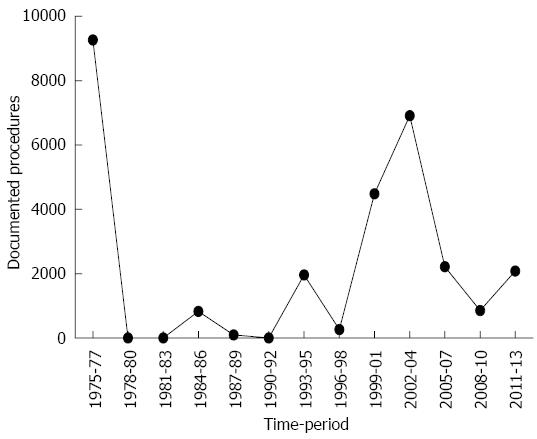
Publication activity was quantified using all 70 published papers and did not include “comment” publications. Publication activity graphed by 3-year periods (Figure 2) demonstrates a rapid increase in publications between 1990 and 2001, peaking at 15 articles for the 3-year period 1999 to 2001. Over the past 9 years, the rate has slowly decreased with fewer than 10 publications in the last 3 years. This decline is mirrored by a decline in documented procedures performed by non-physician endoscopists (Figure 3). Of note, 96% (2030/2080) of documented procedures, and 75% (3/4) of original datasets in the last 3 years have come from one (Dutch) research group. The overall geographic distribution of publication activity is demonstrated in Figure 4.
Twenty eight articles were identified in literature that measured the performance of non-physician endoscopists (Table 1). Of these, Williams et al[19], Richardson et al[20] and Williams et al[21] used the same datasets leaving 26 studies suitable for analysis. Seventeen out of 26 original datasets related to FSs (n = 12218), 5 to upper GI endoscopy (n = 2150) and 6 studies to colonoscopy (n = 2559). Several datasets related to 2 types of procedures. 19% of all datasets were from randomized patients (n = 1428); 64% of the original datasets were created utilizing ≤ 2 non-physician endoscopists (n = 5056). Eighty seven of the 91 (96%) non-physician endoscopists were nurse endoscopists. All studies were from centres in metropolitan regions with nurses working under strict supervision and guidance of gastroenterologists. It is important to note that all studies were conducted at tertiary hospitals or university centres in metropolitan locations. There are no data on unsupervised practice outside these closely monitored and well-defined settings.
Studies varied with regard to measures of procedural competence and outcome, however most used polyp/adenoma detection rate (FS and colonoscopy), insertion depth (FS), complications, patient satisfaction, procedure time and caecal intubation time/rate (colonoscopy). Studies attempting to measure cognitive competence were limited to Schroy et al[4]; Moshakis et al[16] and Wildi et al[22]. Williams et al[19] assessed post-procedural reports but not for content, only for the presence of specific details included on the report.
The available data do not allow a direct comparison or meta-analysis of the procedural performance of medical specialist and nurse endoscopists since the assessments were not standardized. In addition, substantial methodological limitations reduce the validity of results. For example, in studies comparing nurse and medical or surgical endoscopists, patients were seldom randomly allocated. However, based upon the data presented it appears reasonable to conclude that after appropriate training nurse endoscopists (and other non-medical staff) can perform specific endoscopic procedures under appropriate supervision by a medical or surgical specialist and within well-defined settings.
Genuine cost-benefit analyses of non-physician endoscopists are scarce in the literature, although many articles claim non-physician endoscopists having a high likelihood of providing a cheaper per-procedure service. A crude cost-benefit analysis by Massl et al[5] suggested that a total saving of €7.61 (about USD10.39) per procedure could be achieved with a model of 1 senior gastroenterologist supervising 3 active nurse endoscopists. However these costs did not account for the total episode of care including follow-up procedures, follow-up consultations, histology and other factors. This is important given the likelihood that a procedure performed by a nurse endoscopist will require further follow-up for disease management. Indeed, a cost-benefit analysis from the United Kingdom took most of these factors into consideration in a national randomized National Health Service (NHS) based dataset[19-21] where 30 experienced nurse endoscopists performed both upper endoscopies and FS, but not colonoscopy (957 non-physician procedures). While physicians were more expensive per hour (£1.82/min vs£0.53/min), nurse endoscopists had significantly increased need for subsequent endoscopy, specialist follow-up and primary care follow-up at 1 year following their procedures. This lead to higher overall costs being calculated as £53 per procedure in the non-physician group. They also found that patients who underwent a physician procedure had on average a greater gain of 0.0153 quality adjusted life years, based on responses from patient surveys. Their final conclusion was that at a price of £30,000 per QALY, the accepted NHS value, physicians were 87% more likely to be cost-effective 1 year after upper endoscopy or FS compared to nurse endoscopists.
The role of the nurse endoscopist initially arose to meet the burgeoning demand for endoscopies in the face of a severe shortage of physician endoscopists, first in the United States and later in the United Kingdom. To this day, the demand for endoscopic procedures continues to rise, due largely to the demographic changes associated with an ageing population[23,24] and the widespread introduction of colorectal cancer screening programs[25]. Additionally, it has been suggested that non-physician endoscopists could contribute to the much-needed provision of endoscopic services in the underserved rural and remote locations. Thus this systematic review was conducted to assess the available evidence supporting the role of nurse endoscopists.
Our analysis suggests that under supervision by medical specialists non-physician endoscopists can perform GI endoscopy to a satisfactory standard; however this model of care does not seem to be cost efficient when compared with traditional physician service models. In addition, the studies have significant shortcomings and biases that limit their validity and generalizability. Most studies that addressed patient satisfaction and other endoscopic procedural (technical) competencies (for example, completion of procedure) were hampered by significant limitations such as lack of randomization, biased patient recruitment and allocation[4-9,11,12,16-18,22,26-34] and other methodological problems. With regard to potential general relevance of the available data, it must be noted that all studies were conducted in metropolitan centres. There are no data supporting safety and appropriateness of endoscopic services provided by non-medical endoscopists without close supervision outside of metropolitan centres. Thus, suggestions of improving endoscopic service provision at remote or rural sites by employing nurse endoscopists are unsubstantiated by any published data.
In this systematic review on non-physician endoscopy we ultimately identified 26 original datasets that were suitable for analysis. Of note, most studies were conducted prior to 2001 with a subsequent decline in total publication activity (Figure 2). Further, 96% of documented procedures performed by non-physician endoscopists in the past 3 years originated from two Dutch metropolitan tertiary centres. This apparent global decline in interest is supported by various surveys that show uptake of non-physician models is poorer than expected in the United States and United Kingdom, despite an increase in demand for endoscopies. Pathmakanthan et al[35] found that 42% of responding United Kingdom hospitals employed nurse endoscopists, and 90% of these were limited to esophagogastroduodenoscopies (EGDs) and FSs. However, the response rate to this survey was modest with 176 respondents from 292 (60%) surveyed hospitals. As a consequence, the results are likely to be subject to bias.
In the United States, Sharma et al[36] found that non-physician endoscopists performed 3.1% of EGDs, 2.2% of colonoscopies and 4% of FSs. Given that their response rate was only 2%, the true rate is likely to be much lower than this figure. The reason for the relatively limited uptake of nurse endoscopists remains unclear. However, considering that the nurse endoscopist’s role was initially developed in the United States yet they perform only a small fraction of all endoscopies, it would appear that there are major flaws with the application of this service model. While reimbursement regulations may be the reason why nurse endoscopists are not contributing more substantially to service delivery, it appears that inferior cost-efficiency of nurse endoscopies is the reason for this minimal impact on service delivery.
From the data in Table 1, it is reasonable to conclude that there is evidence to support nurse endoscopists, and to a lesser extent, other non-physician endoscopists, in performing these procedures. However, there are clearly limitations. Nurses frequently had statistically significant shorter depths of insertion[7-10] but without effects on polyp or adenoma detection rates. Patient satisfaction, procedure times and complication rates were comparable when performed by physicians compared to non-physicians. It should be noted however, that complication rates of endoscopic procedures are low and are mostly related to interventions such as polypectomy. A recent large French study utilising a sample of approximately 100000 colonoscopies reported between 4.5 and 9.7 perforations per 10000 colonoscopies[37]. Complications rates for sigmoidoscopies are substantially lower[38,39]. With less than 18000 documented non-physician endoscopies with safety data available and the majority of published studies focusing on low risk sigmoidoscopies, firm conclusions in relation to safety of endoscopic procedures done by nurse endoscopists cannot be made.
With regards to colorectal cancer prevention, colonoscopy is now the best endoscopic modality[40-43]. With regards to studies focussed on colonoscopies, there are two major Dutch studies. van Putten et al[34] found that nurse endoscopists could eventually reach an unassisted caecal intubation rate of 94%, however 23% of procedures still required a physician’s assistance, 10 nurse endoscopists had an adenoma detection rate of 23%. There was 1 perforation from the 1000 procedures. The second Dutch study (Massl et al[5]) found that newly trained nurse endoscopists had a significantly lower caecal intubation rate compared to newly trained gastroenterology fellows (77% vs 88%, P < 0.05), yet procedure times and complication rates were similar. The smaller Dutch study found that nurse endoscopists and gastroenterology fellows/consultants had a similar overall caecal intubation rate, although levels of assistance were not documented[33]. The only recent non-Dutch study came from a University-based endoscopy clinic in the United States[44]. Their sole nurse endoscopist had an adenoma detection rate of 42%, vs 17% for 2 gastroenterology consultants. These findings were not replicated in any other colonoscopy or flexible colonoscopy study, which all demonstrated similar adenoma/polyp detection rates between non-physicians and physicians. Given the small number of patients and low number of proceduralists, this study is likely an outlier from the norm. Certainly, large trials in the United States have shown that adenoma detection rates in University-based endoscopy clinics can vary between 15.7% and 46.2%[45].
Providing endoscopic services is more than mastering the technical skills required to safely advance the scope. Lesion recognition in the context of the full clinical picture and decision making with regard to the overall management of the patient are critical components of patient care. There are no good data to support the performance of non-physician endoscopists with regard to these cognitive aspects of endoscopic procedures. If the detection of gross pathology could be perceived as a measure of cognitive competence, a study by Schroy et al[4] showed that nurse endoscopists performing sigmoidoscopies had a poor sensitivity (75%) while specificity (94%) was acceptable when compared with a consultant gastroenterologist’s findings as the gold standard. Further evidence is required before non-physician endoscopists can be considered as being “competent” in endoscopy. Recognising relevant lesions and making clinical decisions in the context of the patient’s full clinical picture is critical to deliver efficient and meaningful services.
Cost-benefit analyses are a way to assess the efficiency of services and genuine analyses on non-physician endoscopists are scarce in the literature. A crude cost-benefit analysis by Massl et al[5] suggests that a total saving of €7.61 per procedure could be achieved with a service model of three nurse endoscopists supervised by a gastroenterologist. However this did not account for differences in the costs of disease management including, follow-up procedures, follow-up consultations, expenditure for consumables and pathology. Indeed, nurse endoscopists take more biopsies than physicians (34.7% vs 26.5%, P < 0.007), with no additional detection of pathology[19]. Unsurprisingly, nurses had far greater levels of normal histology results than physicians (P < 0.0001)[19].
The sole genuine cost-benefit analysis in literature was a randomized study in the United Kingdom[19-21]. This study involved 30 nurse endoscopists performing both EGD and FS. Although the physicians’ salaries were higher (£1.82/min vs£0.53/min), patients examined by nurse endoscopists had an increased need for subsequent endoscopies, specialist follow-up and primary care follow-up after the procedure. Thus the study concluded that at a price of £30000 per QALY, the accepted National Health Service value, physicians were more likely to be cost-effective one year after the procedure. This cost-benefit analysis did not take into account expenditure and loss of consultant time in training and supervising nurses, the increase in follow-up non-endoscopic investigations or increased expenditure for the required follow-up of biopsies. Based on the conservative estimates from the study, and the above mentioned additional unaccounted costs of nurse endoscopists, physician endoscopists appear to be more cost-effective than nurse endoscopists. While there is anecdotal evidence from individual sites that some nurse endoscopists may work well in defined settings, the available data from larger studies does not support the assumption that the nurse endoscopy model is a more cost efficient service model.
While the salary of a nurse endoscopist might be lower as compared to a fully qualified specialist, it could be expected that services provided by nurse endoscopists are more cost efficient. However, the data point to the opposite. It is evident from the published data that the provision of endoscopic services is a multi-step process that includes a complex combination of patient-centred technical and non-technical cognitive skills. So far the assessment of endoscopic services delivered by nursing or other non-physician staff appears to be focussed on the technical aspects of procedures, rather than clinical gain of the procedures. This focus on technical/procedural aspects is appropriate to ensure safe service delivery. However, the implementation of nurse endoscopists to improve the delivery of endoscopy services is not cost-effective when compared with services delivered by specialists. This is most likely due to the cognitive aspects of service delivery. The comprehensive training of medical specialists appears to result in more cost effective service delivery.
When the model of nurse endoscopists was initially introduced in the United States and the United Kingdom the primary aim was to address the shortage of medical or surgical endoscopists. In most countries this is currently not the key problem; inappropriate funding, lack of infrastructure or issues of productivity and quality are the capacity limiting factors. Based upon the available evidence it is highly unlikely that the introduction or the increased use of nurse or other non-medical endoscopists will improve access to quality endoscopic services and improve the cost efficiency of delivery of endoscopic services.
Based upon the available anecdotal evidence and the data it appears that nurse endoscopists might be suitable to address shortages of workforce if they are imbedded into larger teams of specialists in metropolitan centres focusing on the delivery of less complex procedures such as follow-up surveillance procedures. However, before this is accepted as the appropriate setting for nurse endoscopists, the implications for training and overall productivity of services need to be properly explored, particularly in relation to colonoscopy and video capsule endoscopy where there are only limited reports on the use of non-physician endoscopists performing these procedures[46-50].
More data are obviously required. Besides the need to assess and improve the ability of nurse endoscopists to effectively contribute to the service delivery, it is necessary to explore all potential avenues that are suitable to provide cost efficient quality services to patients. This may include novel models of multi-professional teamwork, better integrated and focussed training of other professional groups such as General Practitioners for non-metropolitan (rural) settings to provide core endoscopic services to populations that are currently not properly serviced by specialists.
Most studies assessing training and performance of non-physician endoscopists have substantial methodological limitations. Studies were often uncontrolled, without random patient allocation and open to bias (selection and reporting bias). In all studies, nurse and other non-physician endoscopists worked only within a multidisciplinary team with strict supervision from a qualified physician or surgeon endoscopist.
With regard to cognitive competences in relation to the delivery of endoscopic services, nurses appear to perform less well than medical endoscopists. This emphasizes the need to work in teams with close supervision. In relation to cost-efficiency, nurse and non-physician endoscopists are probably less cost-effective than medical endoscopists. This is related to the increased need of follow-ups and reflects the cognitive component. More research is needed in this area.
All available data are from large and metropolitan centres. There is no evidence to suggest that the delivery of endoscopic services outside large metropolitan centres with several procedure rooms running in parallel benefits service delivery or is a safe option.
While nurse endoscopists may increase the capacity of endoscopic services when imbedded into larger endoscopic units, this does not appear to be a cost-efficient option as compared to traditional service models.
Nurse endoscopy training and delivery of endoscopic services was first reported in the United States more than 35 years ago for flexible sigmoidoscopy (FS). Several studies soon emerged, confirming that nursing staff with appropriate training and supervision could adequately perform endoscopic procedures such as FS. Other studies have since established that nurse endoscopists can safely perform upper endoscopies and colonoscopies. In an era where safe, yet cost-effective, policies run at the forefront of stakeholders’ minds, the question of how nursing staff can undertake additional roles in the endoscopic suites is continually raised.
There have been no systematic reviews of the literature that have examined the full body of evidence surrounding uptake, safety, accuracy and most importantly, the cost-effectiveness of nurse endoscopists.
Contrary to general beliefs, endoscopic services provided by nurse endoscopists are not more cost effective compared to standard service models and evidence suggests the opposite. Overall significant shortcomings and biases limit the validity and generalizability of studies that have explored safety and quality of services delivered by non-medical endoscopists.
The paper is very interesting with significant results in the field of evidence on safety, competency and cost-effectiveness of nursing staff providing gastrointestinal endoscopy services. The tables are too broad and difficult to clear. Authors need to reduce and make more informative.
P- Reviewer: Stanojevic GZ S- Editor: Yu J L- Editor: A E- Editor: Zhang DN
| 1. | Spencer RJ, Ready RL. Utilization of nurse endoscopists for sigmoidoscopic examinations. Dis Colon Rectum. 1977;20:94-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Haycock A, Koch AD, Familiari P, van Delft F, Dekker E, Petruzziello L, Haringsma J, Thomas-Gibson S. Training and transfer of colonoscopy skills: a multinational, randomized, blinded, controlled trial of simulator versus bedside training. Gastrointest Endosc. 2010;71:298-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 84] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 3. | Meining A, Semmler V, Kassem AM, Sander R, Frankenberger U, Burzin M, Reichenberger J, Bajbouj M, Prinz C, Schmid RM. The effect of sedation on the quality of upper gastrointestinal endoscopy: an investigator-blinded, randomized study comparing propofol with midazolam. Endoscopy. 2007;39:345-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 66] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 4. | Schroy PC, Wiggins T, Winawer SJ, Diaz B, Lightdale CJ. Video endoscopy by nurse practitioners: a model for colorectal cancer screening. Gastrointest Endosc. 1988;34:390-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Massl R, van Putten PG, Steyerberg EW, van Tilburg AJ, Lai JY, de Ridder RJ, Brouwer JT, Verburg RJ, Alderliesten J, Schoon EJ. Comparing quality, safety, and costs of colonoscopies performed by nurse vs physician trainees. Clin Gastroenterol Hepatol. 2014;12:470-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Duthie GS, Drew PJ, Hughes MA, Farouk R, Hodson R, Wedgwood KR, Monson JR. A UK training programme for nurse practitioner flexible sigmoidoscopy and a prospective evaluation of the practice of the first UK trained nurse flexible sigmoidoscopist. Gut. 1998;43:711-714. [PubMed] |
| 7. | Maule WF. Screening for colorectal cancer by nurse endoscopists. N Engl J Med. 1994;330:183-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 142] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Rosevelt J, Frankl H. Colorectal cancer screening by nurse practitioner using 60-cm flexible fiberoptic sigmoidoscope. Dig Dis Sci. 1984;29:161-163. [PubMed] |
| 9. | Wallace MB, Kemp JA, Meyer F, Horton K, Reffel A, Christiansen CL, Farraye FA. Screening for colorectal cancer with flexible sigmoidoscopy by nonphysician endoscopists. Am J Med. 1999;107:214-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Schoenfeld P, Lipscomb S, Crook J, Dominguez J, Butler J, Holmes L, Cruess D, Rex D. Accuracy of polyp detection by gastroenterologists and nurse endoscopists during flexible sigmoidoscopy: a randomized trial. Gastroenterology. 1999;117:312-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 95] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 11. | Koornstra JJ, Corporaal S, Giezen-Beintema WM, de Vries SE, van Dullemen HM. Colonoscopy training for nurse endoscopists: a feasibility study. Gastrointest Endosc. 2009;69:688-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Nielsen KT, Langer S, Neumann R, Krarup N. [The nurse as endoscopist]. Ugeskr Laeger. 2005;167:3494-3496. [PubMed] |
| 13. | Cass OW, Freeman ML, Peine CJ, Zera RT, Onstad GR. Objective evaluation of endoscopy skills during training. Ann Intern Med. 1993;118:40-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 161] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18487] [Cited by in RCA: 24807] [Article Influence: 1771.9] [Reference Citation Analysis (3)] |
| 15. | DiSario JA, Sanowski RA. Sigmoidoscopy training for nurses and resident physicians. Gastrointest Endosc. 1993;39:29-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 60] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Moshakis V, Ruban R, Wood G. Role of the nurse endoscopist in colorectal practice. Br J Surg. 1996;83:1399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Schoenfeld PS, Cash B, Kita J, Piorkowski M, Cruess D, Ransohoff D. Effectiveness and patient satisfaction with screening flexible sigmoidoscopy performed by registered nurses. Gastrointest Endosc. 1999;49:158-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 66] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Shum NF, Lui YL, Choi HK, Lau SC, Ho JW. A comprehensive training programme for nurse endoscopist performing flexible sigmoidoscopy in Hong Kong. J Clin Nurs. 2010;19:1891-1896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | Williams J, Russell I, Durai D, Cheung WY, Farrin A, Bloor K, Coulton S, Richardson G. What are the clinical outcome and cost-effectiveness of endoscopy undertaken by nurses when compared with doctors? A Multi-Institution Nurse Endoscopy Trial (MINuET). Health Technol Assess. 2006;10:iii-iv, ix-x, 1-195. [PubMed] |
| 20. | Richardson G, Bloor K, Williams J, Russell I, Durai D, Cheung WY, Farrin A, Coulton S. Cost effectiveness of nurse delivered endoscopy: findings from randomised multi-institution nurse endoscopy trial (MINuET). BMJ. 2009;338:b270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Williams J, Russell I, Durai D, Cheung WY, Farrin A, Bloor K, Coulton S, Richardson G. Effectiveness of nurse delivered endoscopy: findings from randomised multi-institution nurse endoscopy trial (MINuET). BMJ. 2009;338:b231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 22. | Wildi SM, Wallace MB, Glenn TF, Mokhashi MS, Kim CY, Hawes RH. Accuracy of esophagoscopy performed by a non-physician endoscopist with a 4-mm diameter battery-powered endoscope. Gastrointest Endosc. 2003;57:305-310. [PubMed] |
| 23. | Macafee DA, Waller M, Whynes DK, Moss S, Scholefield JH. Population screening for colorectal cancer: the implications of an ageing population. Br J Cancer. 2008;99:1991-2000. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 24. | Nowossadeck E, Haberland J, Kraywinkel K. [The future incidence of colorectal and lung cancers: results of the calculation of different scenarios for the year 2020]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2014;57:103-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Benson VS, Patnick J, Davies AK, Nadel MR, Smith RA, Atkin WS. Colorectal cancer screening: a comparison of 35 initiatives in 17 countries. Int J Cancer. 2008;122:1357-1367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 177] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 26. | Schoen RE, Weissfeld JL, Bowen NJ, Switzer G, Baum A. Patient satisfaction with screening flexible sigmoidoscopy. Arch Intern Med. 2000;160:1790-1796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 65] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 27. | Shapero TF, Alexander PE, Hoover J, Burgis E, Schabas R. Colorectal cancer screening: video-reviewed flexible sigmoidoscopy by nurse endoscopists--a Canadian community-based perspective. Can J Gastroenterol. 2001;15:441-445. [PubMed] |
| 28. | Jain A, Falzarano J, Jain A, Decker R, Okubo G, Fujiwara D. Outcome of 5,000 flexible sigmoidoscopies done by nurse endoscopists for colorectal screening in asymptomatic patients. Hawaii Med J. 2002;61:118-120. [PubMed] |
| 29. | Meenan J, Anderson S, Tsang S, Reffitt D, Prasad P, Doig L. Training in radial EUS: what is the best approach and is there a role for the nurse endoscopist? Endoscopy. 2003;35:1020-1023. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 30. | Smale S, Bjarnason I, Forgacs I, Prasad P, Mukhood M, Wong M, Ng A, Mulcahy HE. Upper gastrointestinal endoscopy performed by nurses: scope for the future? Gut. 2003;52:1090-1094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 31. | Maslekar S, Hughes M, Gardiner A, Monson JR, Duthie GS. Patient satisfaction with lower gastrointestinal endoscopy: doctors, nurse and nonmedical endoscopists. Colorectal Dis. 2010;12:1033-1038. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 32. | Maslekar S, Waudby P, Avery G, Monson JR, Duthie GS. Quality assurance in flexible sigmoidoscopy: medical and nonmedical endoscopists. Surg Endosc. 2010;24:89-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 33. | de Jonge V, Sint Nicolaas J, Cahen DL, Moolenaar W, Ouwendijk RJ, Tang TJ, van Tilburg AJ, Kuipers EJ, van Leerdam ME. Quality evaluation of colonoscopy reporting and colonoscopy performance in daily clinical practice. Gastrointest Endosc. 2012;75:98-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 82] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 34. | van Putten PG, Ter Borg F, Adang RP, Koornstra JJ, Romberg-Camps MJ, Timmer R, Poen AC, Kuipers EJ, Van Leerdam ME. Nurse endoscopists perform colonoscopies according to the international standard and with high patient satisfaction. Endoscopy. 2012;44:1127-1132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 35. | Pathmakanthan S, Murray I, Smith K, Heeley R, Donnelly M. Nurse endoscopists in United Kingdom health care: a survey of prevalence, skills and attitudes. J Adv Nurs. 2001;36:705-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 36. | Sharma VK, Coppola AG, Raufman JP. A survey of credentialing practices of gastrointestinal endoscopy centers in the United States. J Clin Gastroenterol. 2005;39:501-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 37. | Blotière PO, Weill A, Ricordeau P, Alla F, Allemand H. Perforations and haemorrhages after colonoscopy in 2010: a study based on comprehensive French health insurance data (SNIIRAM). Clin Res Hepatol Gastroenterol. 2014;38:112-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (1)] |
| 38. | Lohsiriwat V. Colonoscopic perforation: incidence, risk factors, management and outcome. World J Gastroenterol. 2010;16:425-430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 173] [Cited by in RCA: 158] [Article Influence: 10.5] [Reference Citation Analysis (4)] |
| 39. | Gatto NM, Frucht H, Sundararajan V, Jacobson JS, Grann VR, Neugut AI. Risk of perforation after colonoscopy and sigmoidoscopy: a population-based study. J Natl Cancer Inst. 2003;95:230-236. [PubMed] |
| 40. | Nishihara R, Wu K, Lochhead P, Morikawa T, Liao X, Qian ZR, Inamura K, Kim SA, Kuchiba A, Yamauchi M. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med. 2013;369:1095-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 968] [Cited by in RCA: 1156] [Article Influence: 96.3] [Reference Citation Analysis (0)] |
| 41. | Atkin WS, Edwards R, Kralj-Hans I, Wooldrage K, Hart AR, Northover JM, Parkin DM, Wardle J, Duffy SW, Cuzick J. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet. 2010;375:1624-1633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1242] [Cited by in RCA: 1136] [Article Influence: 75.7] [Reference Citation Analysis (0)] |
| 42. | Wang YR, Cangemi JR, Loftus EV, Picco MF. Risk of colorectal cancer after colonoscopy compared with flexible sigmoidoscopy or no lower endoscopy among older patients in the United States, 1998-2005. Mayo Clin Proc. 2013;88:464-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 43. | Segnan N, Armaroli P, Bonelli L, Risio M, Sciallero S, Zappa M, Andreoni B, Arrigoni A, Bisanti L, Casella C. Once-only sigmoidoscopy in colorectal cancer screening: follow-up findings of the Italian Randomized Controlled Trial--SCORE. J Natl Cancer Inst. 2011;103:1310-1322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 428] [Cited by in RCA: 451] [Article Influence: 32.2] [Reference Citation Analysis (0)] |
| 44. | Limoges-Gonzalez M, Mann NS, Al-Juburi A, Tseng D, Inadomi J, Rossaro L. Comparisons of screening colonoscopy performed by a nurse practitioner and gastroenterologists: a single-center randomized controlled trial. Gastroenterol Nurs. 2011;34:210-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 45. | Kahi CJ, Vemulapalli KC, Johnson CS, Rex DK. Improving measurement of the adenoma detection rate and adenoma per colonoscopy quality metric: the Indiana University experience. Gastrointest Endosc. 2014;79:448-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 46. | Lieberman DA, Ghormley JM. Physician assistants in gastroenterology: should they perform endoscopy? Am J Gastroenterol. 1992;87:940-943. [PubMed] |
| 47. | Vance M. The nurse colonoscopist--training and quality assurance. Gastrointest Endosc Clin N Am. 2005;15:829-837. [PubMed] |
| 48. | Sidhu R, Sanders DS, Kapur K, Marshall L, Hurlstone DP, McAlindon ME. Capsule endoscopy: is there a role for nurses as physician extenders? Gastroenterol Nurs. 2007;30:45-48. [PubMed] |
| 49. | Levinthal GN, Burke CA, Santisi JM. The accuracy of an endoscopy nurse in interpreting capsule endoscopy. Am J Gastroenterol. 2003;98:2669-2671. [PubMed] |
| 50. | Niv Y, Niv G. Capsule endoscopy examination--preliminary review by a nurse. Dig Dis Sci. 2005;50:2121-2124. [PubMed] |