Published online Apr 21, 2015. doi: 10.3748/wjg.v21.i15.4765
Peer-review started: September 10, 2014
First decision: October 14, 2014
Revised: October 29, 2014
Accepted: November 11, 2014
Article in press: November 11, 2014
Published online: April 21, 2015
Processing time: 222 Days and 24 Hours
Cholecystocolic fistula secondary to gallbladder carcinoma is extremely rare and has been reported in very few studies. Most cholecystocolic fistulae are late complications of gallstone disease, but can also develop following carcinoma of the gallbladder when the necrotic tumor penetrates into the adjacent colon. Although no currently available imaging technique has shown great accuracy in recognizing cholecystocolic fistula, abdominopelvic computed tomography may show fistulous communication and anatomical details. Herein we report an unusual case of cholecystocolic fistula caused by gallbladder carcinoma, which was preoperatively misdiagnosed as hepatic flexure colon carcinoma.
Core tip: Cholecystocolic fistula is rare and difficult to diagnose preoperatively. In our report, we preoperatively misdiagnosed our patient as having hepatic flexure colon cancer with adhesion to the gallbladder. The patient was diagnosed with gallbladder carcinoma intraoperatively along with a cholecystocolic fistula secondary to invasion of the colon by the mass. A postoperative review of the preoperative abdominopelvic computed tomography (CT) also resulted in the identification of the cholecystocolic fistula. Abdominopelvic CT may be helpful in the preoperative diagnosis of this condition.
- Citation: Ha GW, Lee MR, Kim JH. Cholecystocolic fistula caused by gallbladder carcinoma: Preoperatively misdiagnosed as hepatic colon carcinoma. World J Gastroenterol 2015; 21(15): 4765-4769
- URL: https://www.wjgnet.com/1007-9327/full/v21/i15/4765.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i15.4765
Cholecystocolic fistula (CCF) secondary to gallbladder carcinoma is extremely rare and has been reported in very few studies[1,2]. Although most CCFs are late complications of gallstone disease, they may develop following carcinoma of the gallbladder when the necrotic tumor penetrates into the adjacent colon. CCF is the second most common type of cholecystoenteric fistula (10%-20%) after cholecystoduodenal fistula (75%)[3-5]. Although no currently available imaging technique has shown great accuracy in recognizing CCF, abdominopelvic computed tomography (CT) may show fistulous communication and anatomical details.
We report an unusual case of CCF caused by gallbladder carcinoma, which was preoperatively misdiagnosed as hepatic flexure colon carcinoma.
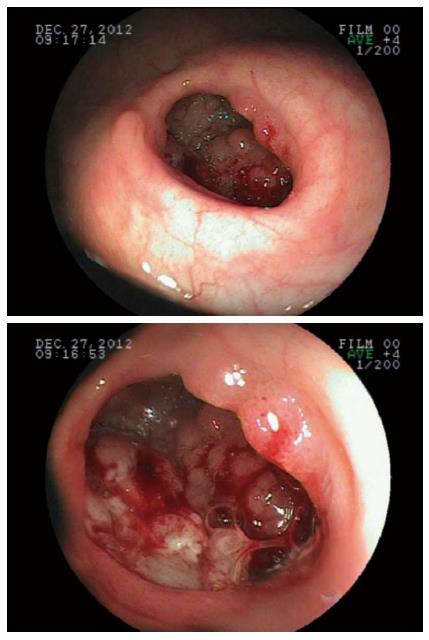
A 62-year-old woman who underwent a colonoscopy during regular health screening at a primary hospital and was found to have an apparent hepatic flexure colon cancer visited the department of colorectal surgery of our hospital for treatment. Colonoscopy had shown a diverticulum with an embedded, laterally spreading tumor-like lesion at the hepatic flexure colon (Figure 1). Colonoscopic biopsy showed a well differentiated adenocarcinoma likely arising from a tubulo-villous adenoma. The patient had no specific symptoms and physical examination showed no specific findings in her abdomen. Her prior medical history included diabetes mellitus and hypertension. Laboratory tests and a plain radiograph of the abdomen were unremarkable.
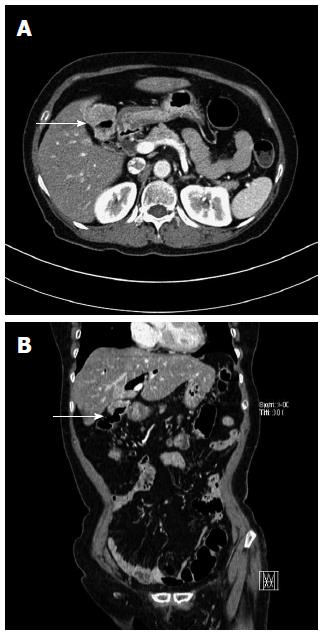
The patient underwent an abdominopelvic CT with IV contrast to evaluate the clinical stage of the tumor. CT showed a mass, along with thickening of the wall, of the hepatic flexure colon adherent to the gallbladder. Thickening of the gallbladder walls was also observed, along with a gallstone, diffuse intrahepatic biliary duct dilatation and pneumobilia, but without a definitive obstructive lesion. The rest of the abdomen was unremarkable.
Based on colonoscopic and radiologic findings, the patient was preoperatively diagnosed with a hepatic flexure colon cancer.
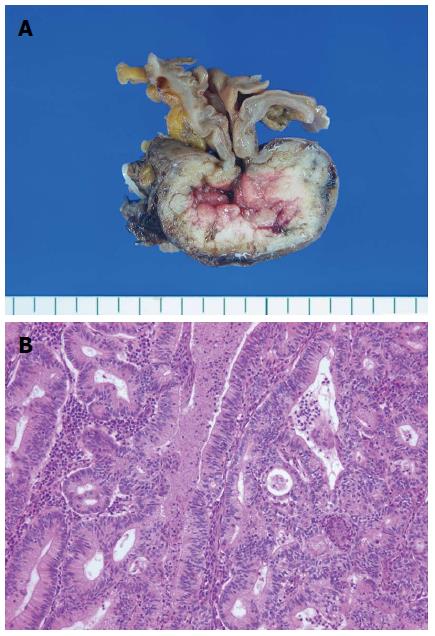
Laparoscopic exploration revealed a malignant appearing mass with inflammatory changes throughout the entire body of the gallbladder. The gallbladder was hard to palpation, with the lesion invading the adjacent part of the hepatic flexure colon. Thickening of the hepatic flexure colon wall was also observed, along with continuity of the colonic and gallbladder lumen. The patient was diagnosed with gallbladder carcinoma intraoperatively along with a cholecystocolic fistula secondary to invasion of the colon by the mass. However, there was no visible mass in the hepatic flexure colon and no gross evidence of direct invasion of the liver (Figure 2). Surgery included a right hemicolectomy along with resection of the regional lymph nodes and cholecystectomy, all performed laparoscopically. Seven days after the surgery, the patient was discharged without any complications.
Histopathological examination of the resected specimen showed a gallbladder adenocarcinoma with direct invasion of the colon but no regional lymph node metastases in 10 adjacent lymph nodes. A polypoid tumor about 4 cm in size was located in the body of the gallbladder (Figure 3). The resection margins of the cystic duct and colon were negative for malignancy. According to the AJCC classification, the gallbladder adenocarcinoma could be pathologically staged as IIIA (pT3N0).
A postoperative review of the preoperative abdominopelvic CT scan resulted in the identification of the cholecystocolic fistula. The gallbladder wall was contiguous with the wall of the hepatic flexure; the gallbladder showed an air-filled appearance, and the margin between the liver and the gallbladder was well defined (Figure 4).
Following surgery, the patient was treated with oral chemotherapy (Tegafur-uracil) for 19 mo, with no evidence of further development of the tumor or metastases.
CCF is a late and uncommon complication of long-lasting inflammatory processes of the gallbladder caused by gallstones, occurring in about 0.1% of patients with biliary disease[3-5]. CCF may also occur in patients with abdominal trauma, Crohn’s disease and malignancies of the biliary tract, colon and head of the pancreas[6]. Most patients with CCF are elderly and there is a female preponderance (2-4:1)[5,7]. The low incidence of CCF in patients with gallstone disease may be due to early diagnosis and standard surgical treatment of cholelithiasis.
Diagnostic methods for CCF may include plain abdominal radiographs, barium enema, ERCP, ultrasound, abdominopelvic CT and/or diagnostic laparotomy[8,9]. However, preoperative diagnosis is rare (< 10%), in contrast to cholecystoenteric fistulas (43%)[4,5]. Its nonspecific symptoms may contribute to the low preoperative rate of CCF diagnosis[3,4]. Symptoms of CCF are usually nonspecific and may include diarrhea, melena and weight loss, resulting in a low rate of preoperative diagnosis, with most cases diagnosed intraoperatively. None of the imaging techniques currently used has been accurate in diagnosing CCF[10]. Thus, misdiagnosis may be frequent, and surgeons may have to switch from elective cholecystectomy to a more complex procedure that occasionally involves adhesiolysis and colonic resection.
The recent development of cross-sectional imaging on abdominopelvic CT has enhanced the ability to diagnose CCF. The presence of pneumobilia, ectopic gallstone, small bowel dilatation, nonvisualization of the gallbladder, or thick-walled atrophic gallbladder adherent to neighboring organs may indicate a cholecystoenteric fistula[11,12]. In most patients with CCF, the involvement of an inflammatory or neoplastic process appears localized to the superior aspect of the anterior hepatic flexure, and circumferential involvement of the lumen mimicking primary carcinoma of the colon may also occur[13,14]. These radiological presentations may be helpful in diagnosing CCF by abdominopelvic CT. Although abdominopelvic CT showed these findings in our patient, we preoperatively misdiagnosed our patient as having hepatic flexure colon cancer with adhesion to the gallbladder.
Although it is infrequent, gallbladder carcinoma may co-occur with CCF[15-18]. Studies of patients presenting with cholecystoenteric fistula have reported high rates of cancer associated with fistula (3%-14%)[5,19]. Thus, any uncertainty regarding the differential diagnosis between CCF and gallbladder carcinoma may be solved by performing immediate frozen sections, with a negative margin during tangential colonic resection always respected. That is, although the conventional surgical treatment of CCF caused by gallstones involves cholecystectomy and closure of the fistulous tract[20], surgical treatment of CCF in patients with gallbladder carcinoma involves radical cholecystectomy, including en bloc hepatic resection with lymphadenectomy, and resection of the involved colon. Our findings also indicate that a laparoscopic procedure is feasible and effective for the treatment of CCF secondary to gallbladder carcinoma, similar to findings in patients with CCF secondary to gallstones[3,4,20-22].
After the surgery, adjuvant chemotherapy or chemoradiation should be considered in patients with CCF secondary to advanced gallbladder carcinoma. Adjuvant chemotherapy regimens may include fluoropyrimidine, gemcitabine, and platinum compounds[23]. Single-agent fluoropyrimidine or gemcitabine is generally recommended in the adjuvant setting. Combination chemotherapy using gemcitabine and cisplatin is also considered as a therapeutic option. Our patient was treated with oral chemotherapy (Tegafur-uracil) for 19 mo, there was no evidence of recurrence or metastases.
In conclusion, CCF secondary to gallbladder carcinoma is extremely rare and difficult to diagnose preoperatively. Although CCF cannot be definitively diagnosed using current tools, abdominopelvic CT may be helpful in the preoperative diagnosis of this condition, with diagnosis assisted by the familiarity of the radiologist with the imaging appearance of this condition. The surgical treatment of CCF secondary to gallbladder carcinoma consists of radical cholecystectomy and resection of the involved colon, with laparoscopic procedures considered feasible and effective.
A 62-year-old woman who had an apparent hepatic flexure colon cancer with no specific symptoms visited the department of colorectal surgery of the hospital for treatment.
No specific findings in physical examination of her abdomen.
Hepatic flexure colon carcinoma, suspicious of direct invasion of the gallbladder.
All laboratory tests were within normal limits.
Computed tomography (CT) showed a mass, along with thickening of the wall, of the hepatic flexure colon adherent to the gallbladder.
Histopathological examination of the resected specimen showed a gallbladder adenocarcinoma with direct invasion of the colon but no regional lymph node metastases in 10 adjacent lymph nodes.
A right hemicolectomy along with resection of the regional lymph nodes and cholecystectomy performed laparoscopically.
Cholecystocolic fistula secondary to gallbladder carcinoma is extremely rare and has been reported in very few studies.
No uncommon terms present in this case report.
Abdominopelvic CT may be helpful in the preoperative diagnosis of cholecystocolic fistula (CCF). The laparoscopic surgery of CCF secondary to gallbladder carcinoma is considered feasible and effective.
The authors have described a case of cholecystocolic fistula secondary to gallbladder carcinoma, which was managed by laparoscopy. The article highlights the imaging appearance of cholecystocolic fistula secondary to gallbladder carcinoma.
P- Reviewer: Bianchini M, Elalfy H, Solinas A S- Editor: Qi Y L- Editor: A E- Editor: Zhang DN
| 1. | Dwivedi AN, Kumar S, Rana S, Maurya B. Transmural invasion of hepatic flexure of colon causing cholecystocolic fistula by aggressive gallbladder carcinoma. World J Surg Oncol. 2013;11:86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Rastogi R. Cholecystocolic fistula secondary to gallbladder carcinoma: a rare case. Saudi J Gastroenterol. 2008;14:144-146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Angrisani L, Corcione F, Tartaglia A, Tricarico A, Rendano F, Vincenti R, Lorenzo M, Aiello A, Bardi U, Bruni D. Cholecystoenteric fistula (CF) is not a contraindication for laparoscopic surgery. Surg Endosc. 2001;15:1038-1041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 61] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Chowbey PK, Bandyopadhyay SK, Sharma A, Khullar R, Soni V, Baijal M. Laparoscopic management of cholecystoenteric fistulas. J Laparoendosc Adv Surg Tech A. 2006;16:467-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 84] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Glenn F, Reed C, Grafe WR. Biliary enteric fistula. Surg Gynecol Obstet. 1981;153:527-531. [PubMed] |
| 6. | LeBlanc KA, Barr LH, Rush BM. Spontaneous biliary enteric fistulas. South Med J. 1983;76:1249-1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Stagnitti F, Mongardini M, Schillaci F, Dall’Olio D, De Pascalis M, Natalini E. [Spontaneous biliodigestive fistulae. The clinical considerations, surgical treatment and complications]. G Chir. 2000;21:110-117. [PubMed] |
| 8. | Hession PR, Rawlinson J, Hall JR, Keating JP, Guyer PB. The clinical and radiological features of cholecystocolic fistulae. Br J Radiol. 1996;69:804-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Singh AK, Gervais D, Mueller P. Cholecystocolonic fistula: serial CT imaging features. Emerg Radiol. 2004;10:301-302. [PubMed] |
| 10. | Costi R, Randone B, Violi V, Scatton O, Sarli L, Soubrane O, Dousset B, Montariol T. Cholecystocolonic fistula: facts and myths. A review of the 231 published cases. J Hepatobiliary Pancreat Surg. 2009;16:8-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 106] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 11. | Yamashita H, Chijiiwa K, Ogawa Y, Kuroki S, Tanaka M. The internal biliary fistula--reappraisal of incidence, type, diagnosis and management of 33 consecutive cases. HPB Surg. 1997;10:143-147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 62] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Inal M, Oguz M, Aksungur E, Soyupak S, Börüban S, Akgül E. Biliary-enteric fistulas: report of five cases and review of the literature. Eur Radiol. 1999;9:1145-1151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 13. | Fahim RB, Mcdonald JR, Richards JC, Ferris DO. Carcinoma of the gallbladder: a study of its modes of spread. Ann Surg. 1962;156:114-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 196] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 14. | Keill RH, DeWeese MS. Primary carcinoma of the gallbladder. Am J Surg. 1973;125:726-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Godquin B, Favre R, Blanchard J, Boutovitch N. [A cholecysto-colic fistula caused by perforation of a gallbladder cancer. Case report (author’s transl)]. Acta Gastroenterol Belg. 1974;37:236-242. [PubMed] |
| 16. | Morris SJ, Greenwald RA, Barkin JS, Tedesco FJ, Snyder R. Cholecystoduodenocolic fistula secondary to carcinoma of the gallbladder. Am J Dig Dis. 1978;23:849-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Khaira HS, Awad RW, Thompson AK. Squamous cell carcinoma of the gallbladder presenting with a biliary-colic fistula. Eur J Surg Oncol. 1995;21:581-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Ramos-De la Medina A, Medina-Franco H. [Biliary-colonic fistulas. Analysis of 2 cases and literature review]. Rev Gastroenterol Mex. 2002;67:207-209. [PubMed] |
| 19. | Day EA, Marks C. Gallstone ileus. Review of the literature and presentation of thirty-four new cases. Am J Surg. 1975;129:552-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 99] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Gentileschi P, Forlini A, Rossi P, Bacaro D, Zoffoli M, Gentileschi E. Laparoscopic approach to cholecystocolic fistula: report of a case. J Laparoendosc Surg. 1995;5:413-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Fujitani K, Hasuike Y, Tsujinaka T, Mishima H, Takeda Y, Shin E, Sawamura T, Nishisyo I, Kikkawa N. New technique of laparoscopic-assisted excision of a cholecystocolic fistula: report of a case. Surg Today. 2001;31:740-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Jung SY, Lee SJ, Cho JW, Jung JP, Kim JB, Woo JY, Kim BC. Laparoscopic right hemicolectomy and cholecystectomy for a cholecystocolic fistula. J Korean Soc Coloproctol. 2009;25:268-272. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | Hundal R, Shaffer EA. Gallbladder cancer: epidemiology and outcome. Clin Epidemiol. 2014;6:99-109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 152] [Cited by in RCA: 489] [Article Influence: 44.5] [Reference Citation Analysis (0)] |