Published online Apr 21, 2015. doi: 10.3748/wjg.v21.i15.4526
Peer-review started: September 14, 2014
First decision: October 14, 2014
Revised: November 11, 2014
Accepted: January 8, 2015
Article in press: January 8, 2015
Published online: April 21, 2015
Processing time: 222 Days and 6 Hours
AIM: To investigate the effect of alternol on pancreatic cancer cells.
METHODS: Pancreatic cancer cells PANC-1 and BxPC3 were treated with various concentrations of alternol for 24, 48 and 72 h. Cell proliferation was measured by cell counting. Cell cycle distribution and mitochondrial membrane potential were determined by flow cytometry. Apoptosis was determined by a TdT-mediated dUTP nick end labeling assay and Hoechst staining. Expression of caspase 3, Bcl-2, p53 and p21 was measured by western blotting.
RESULTS: Alternol showed dose- and time-dependent inhibition of the proliferation of PANC-1 and BxPC3 cells in vitro. Alternol induced apoptosis and cell cycle arrest at S phase and decreased mitochondrial membrane potential. Alternol activated caspase 3, upregulated p53 and p21 expression, and downregulated Bcl-2 expression in a dose-dependent manner.
CONCLUSION: Our results suggested that alternol is a candidate for treatment of pancreatic cancer.
Core tip: Pancreatic cancer is an aggressive disease with a 5-year survival < 5%. Alternol has shown anti-cancer activity against various types of cancer cells. The aim of this study was to investigate the effect of alternol on pancreatic cancer cells. Alternol inhibited proliferation of PANC-1 and BxPC3 cells. It induced apoptosis and cell cycle arrest and decreased mitochondrial membrane potential. Alternol activated caspase 3, upregulated p53 and p21 expression, and downregulated Bcl-2 expression. In summary, we concluded that alternol may provide an effective regimen for the treatment of pancreatic cancer.
- Citation: Cong PF, Qu YC, Chen JP, Duan LL, Lin CJ, Zhu XL, Li-Ling J, Zhang MX. Growth inhibition and apoptosis induction by alternol in pancreatic carcinoma cells. World J Gastroenterol 2015; 21(15): 4526-4535
- URL: https://www.wjgnet.com/1007-9327/full/v21/i15/4526.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i15.4526
Pancreatic cancer is an aggressive disease with about 44000 new cases and 38000 deaths annually in the United States alone. It represents the fourth-leading cause of cancer mortality worldwide. Despite advances in the understanding of its underlying biology and improvement in imaging modalities, the prognosis for pancreatic cancer remains poor. For all stages combined, its 1-year survival rate is 19% and 5-year survival rate is < 5%. Less than 20% of patients have resectable tumors at the time of initial diagnosis. The fact that the majority of patients are diagnosed at an advanced stage explains the bare improvement in the survival rate over the past 30 years[1-4]. At present, radical surgery offers the only curative treatment for pancreatic cancer. Alternative or combined treatment consists of adjuvant or neoadjuvant chemotherapy with or without radiotherapy[5-7]. Palliative treatment for locally advanced disease may benefit health status and quality of life. Single-agent gemcitabine has been the main stay of treatment for advanced pancreatic cancer. Since 2010, new combination chemotherapy regimens have offered a chance of improved survival compared with gemcitabine alone[8,9]. However, since this disease is notoriously chemo- and radioresistant, more effective therapeutic agents are desirable.
With a molecular weight of 352, alternol is a novel compound isolated from the fermentation product of a novel microorganism mutant strain Alternaria alternata var. monosporus, which was obtained from the bark of yew trees in Kunming, China. Previous studies have shown that alternol can inhibit cell proliferation and induce apoptosis of tumor cells derived from mouse lymphocyte leukemia, melanoma cells, and human gastric carcinoma and prostate cancer[10-14]. It can also inhibit migration and invasion of hepatocellular carcinoma and melanoma cells[15,16]. However, the effect of alternol on pancreatic cancer cells has not yet been explored.
In the present study, we investigated the effect of alternol on the proliferation, cell cycle and apoptosis of pancreatic cancer cells. To explore the underlying molecular mechanisms, we also analyzed the expression of proteins related to apoptosis using western blotting.
Alternol was obtained from Strand Biotechnology Institute of Research, Shantou, China. TdT-mediated dUTP nick end labeling (TUNEL) kit and JC-1 were purchased from Beyotime (Jiangsu, China). Anti Bcl-2, caspase-3, p53, p21, β-actin primary and secondary antibodies (i.e., goat anti-rabbit IgG horseradish peroxidase conjugate), were purchased from Santa Cruz Biotechnology (Santa Cruz, CA, United States). Enhanced chemiluminescence detection reagents were purchased from Amersham Biosciences (Little Chalfont, Bucks, United Kingdom). RPMI 1640 and fetal bovine serum (FBS) were purchased from Gibco Life Technologies (Paisley, United Kingdom). Propidium iodide (PI), Hoechst 33258, dimethyl sulfoxide (DMSO) and other reagents were purchased from Sigma (St Louis, MO, United States).
PANC-1 and BxPC3 pancreatic cancer cells were obtained from Shanghai Institute of Biological Sciences (Chinese Academy of Sciences, China) and maintained in RPMI 1640 supplemented with 10% FBS, 100 U/mL penicillin G and 100 μg/mL streptomycin. Cell cultures were maintained in a 5% CO2 humidified atmosphere at 37 °C.
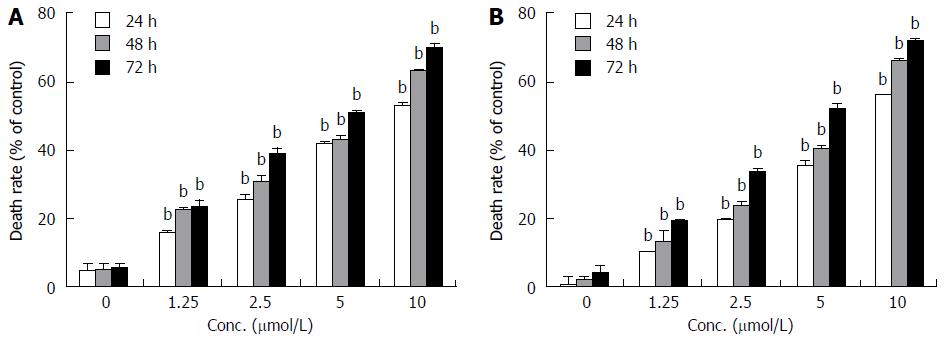
Viability of PANC-1 and BxPC3 cells was evaluated by counting the number of viable cells at 24, 48 and 72 h after addition of alternol. The cells were stained with trypan blue and counted under a hemocytometer. The y axis represents the death rate of viable cells normalized to those of the controls (0.5% DMSO), while the x axis represents the concentration of alternol. The final concentration of 0.5% DMSO showed no inhibition of cell growth. At least three replicate experiments were performed.
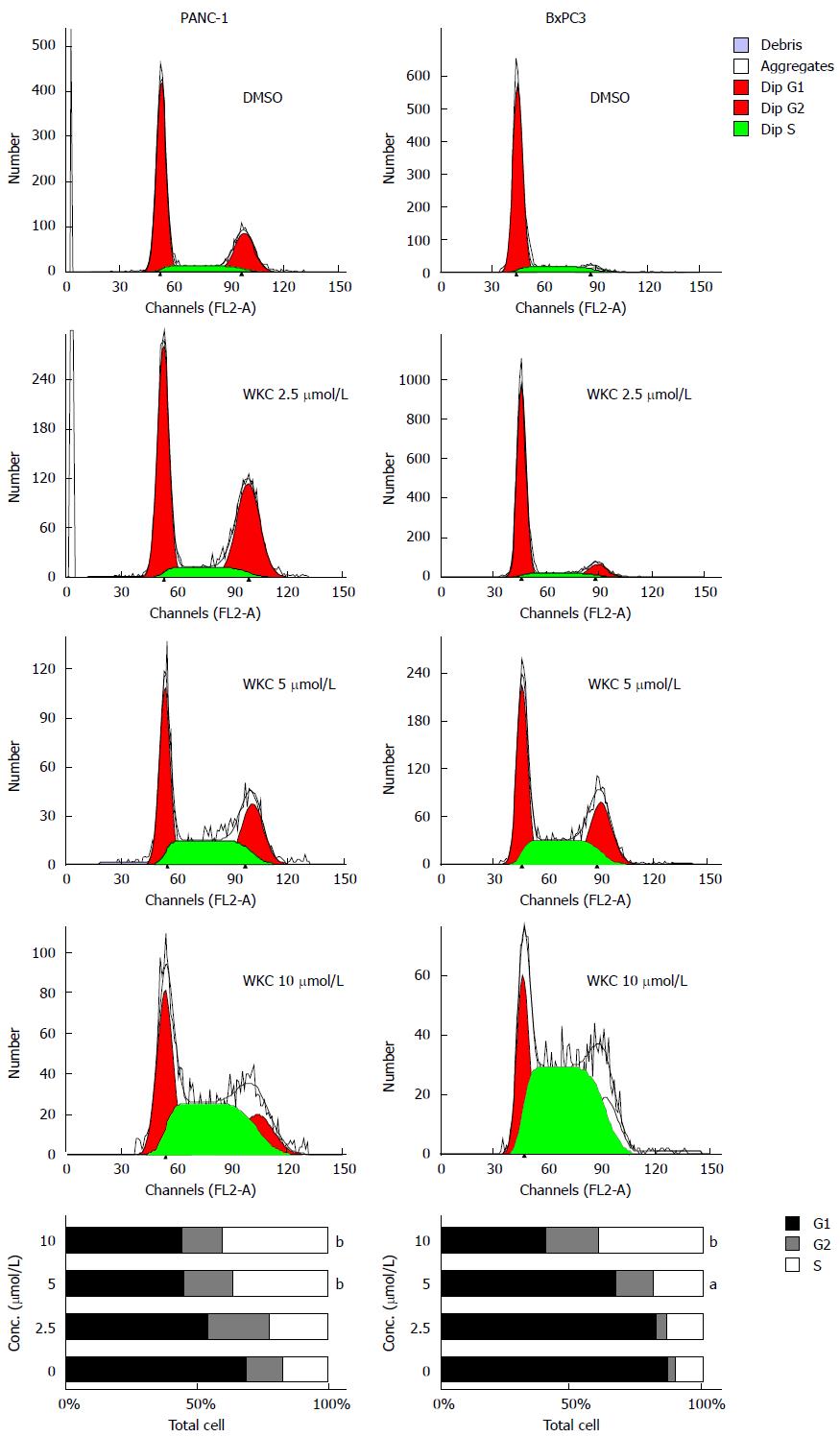
The cell cycle was analyzed with flow cytometry. Cells (7 × 105) were incubated with alternol or vehicle, collected by gentle trypsinization, centrifuged at 1000 rpm for 5 min, and resuspended in phosphate-buffered saline (PBS), fixed by drop-wise addition of ice-cold 70% ethanol, and stored at -20 °C overnight. Prior to use, they were washed with PBS and resuspended in PBS containing 100 μg/mL PI (Sigma), 50 μg/mL ribonuclease A, and 0.1% Triton X-100 in the dark for 30 min. Flow cytometry was carried out on a FACScalibur instrument using a ModFit program (Becton Dickinson, San Jose, CA, United States).
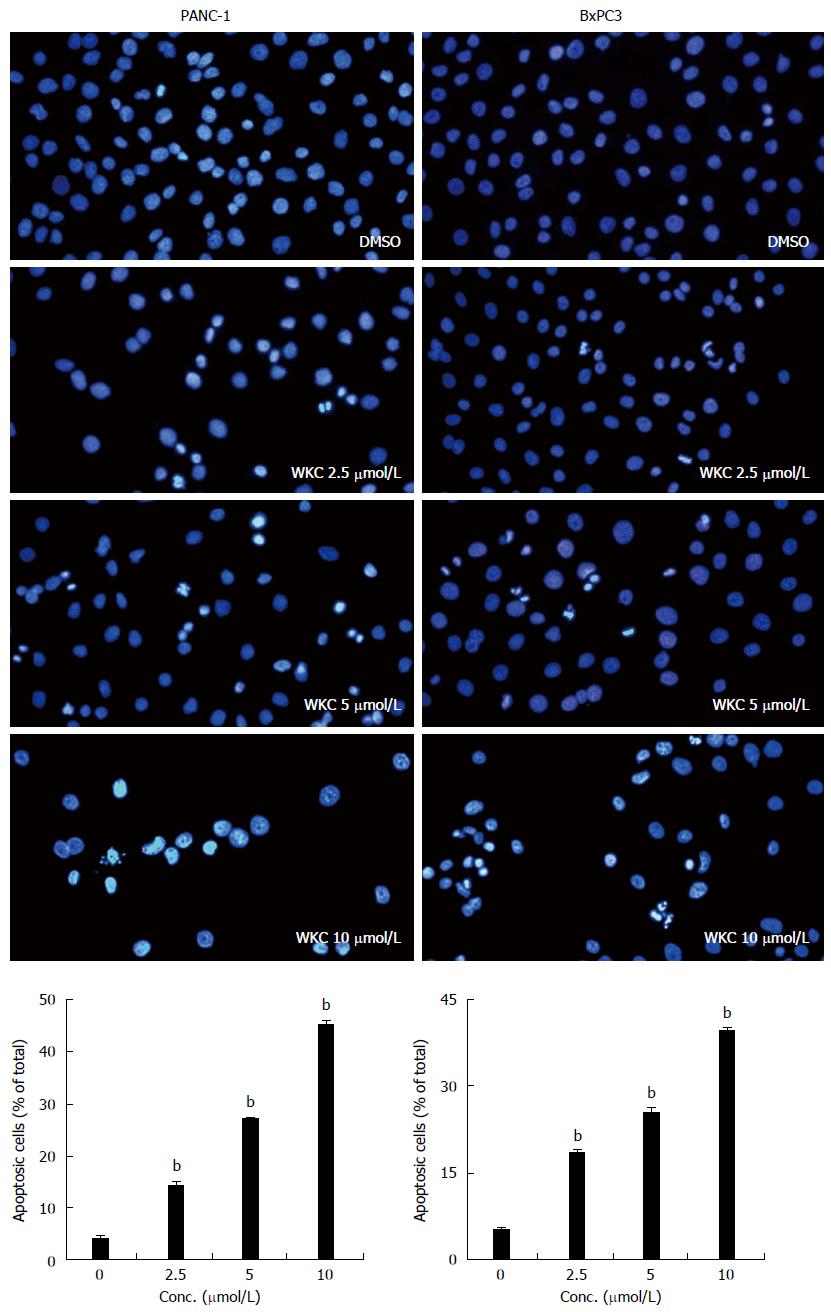
PANC-1 and BxPC3 cells (3.5 × 105) were grown on coverslips placed in six-well plates. After alternol treatment, the cells were fixed with methanol and acetic acid (3/1, v/v) at 4 °C for 15 min, blocked with 5% bovine serum albumin for 30 min, and stained with Hoechst 33258 at 37 °C for 15 min in the dark. After repeated washing in PBS, they were mounted in 50% glycerol in PBS. The processed cells were observed under a fluorescence microscope (Olympus, Tokyo, Japan).
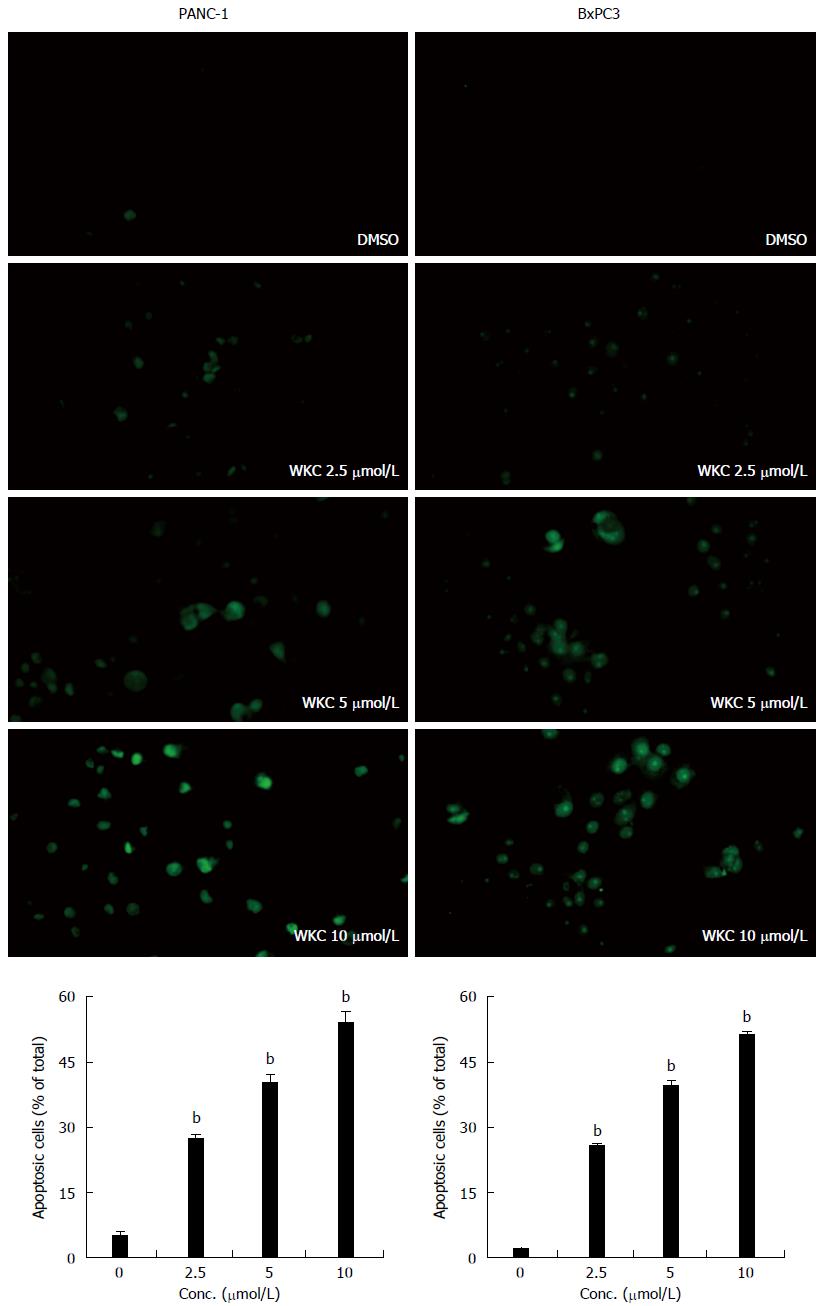
Apoptotic cells was analyzed with a TUNEL assay, which consisted of addition of apoptotically fragmented DNA to the 3’ terminus by terminal deoxynucleotidyl transferase followed by fluorescence labeling. PANC-1 and BxPC3 cells were grown on coverslips at 3.5 × 105/well in six-well plates and exposed to alternol for 24 h. Apoptotic cells were detected using a One Step TUNEL Apoptosis Assay Kit (Beyotime Biotech, Jiangsu, China). The cells were observed under a fluorescence microscope.
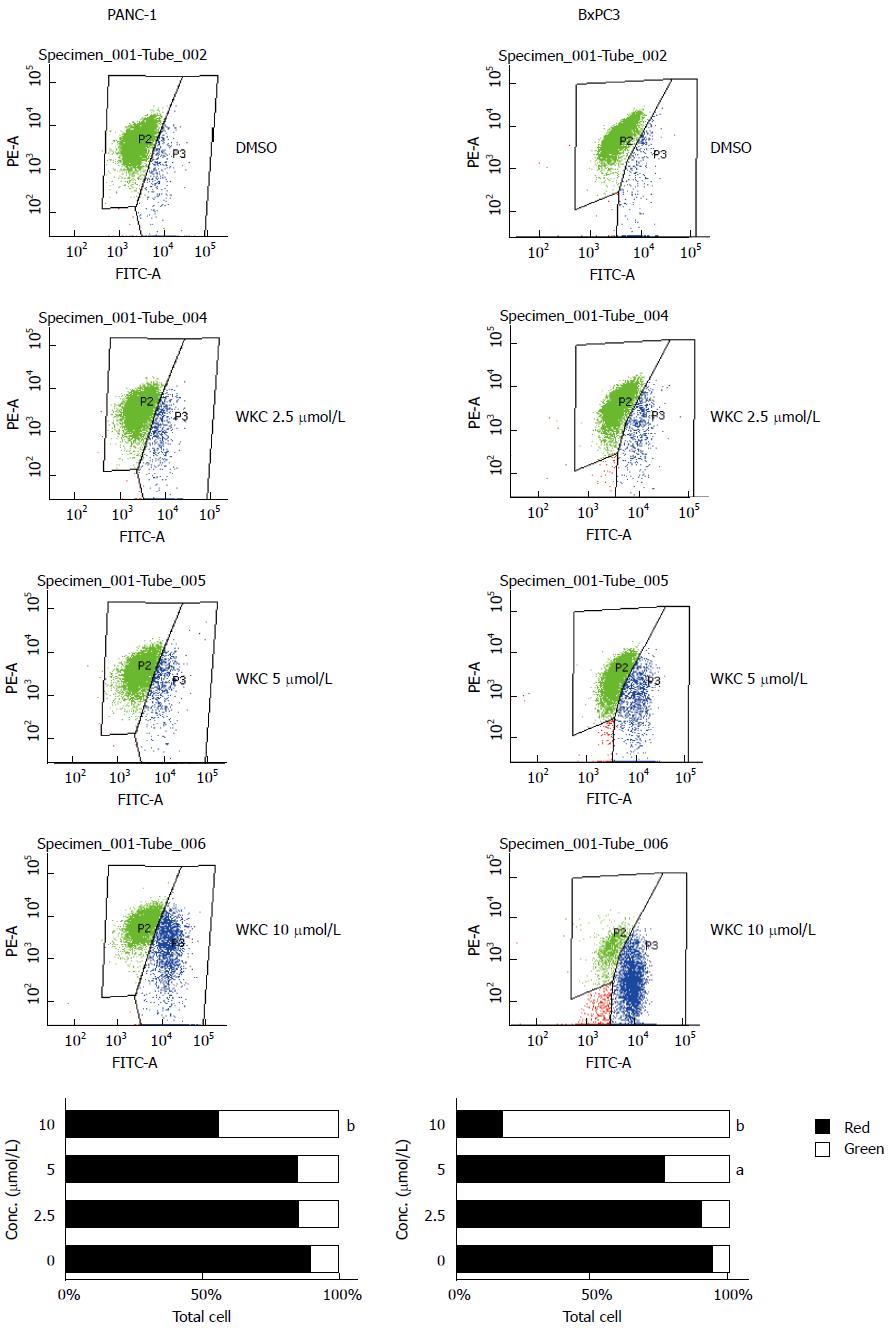
Changes in the mitochondrial membrane potential (MMP) were analyzed by JC-1 staining. JC-1 is a cationic dye that exhibits potential-dependent accumulation in mitochondria, and can be indicated by a fluorescence emission shift from green (525 nm) to red (590 nm). Consequently, mitochondrial depolarization can be indicated by a decrease in the red/green fluorescence intensity ratio. The potential sensitive color shift is due to concentration-dependent formation of red fluorescent J aggregates. All measurements were performed using a FACScalibur flow cytometer. Human PANC-1 and BxPC3 cells (7 × 105) were incubated with alternol for 24 h. The cells were collected and washed with cold PBS. The cells were centrifuged at 1000 rpm for 5 min, resuspended in PBS, incubated with 5 μg/mL JC-1 for 20 min at 37 °C in the dark, and immediately analyzed with a FACScalibur flow cytometer.
Cells (1 × 106/well) seeded in six-well plates were treated with alternol or vehicle control. The medium was aspirated, and the cells were washed with cold PBS. The cells were lysed in lysis buffer supplemented with proteases and phosphotase inhibitors on ice for 20 min and scraped. The lysate was collected by centrifugation at 3000 ×g for 10 min at 4 °C. The supernatant (cell lysate without nucleoli) was stored at -20 °C. For western blotting, 25-50 μg protein was resolved by 12% PAGE and transferred to a polyvinylidene difluoride membrane. The blotting was blocked with buffer (5% nonfat dry milk/0.1% Tween 20 in TBS) for 1 h at room temperature, and incubated with appropriate primary antibodies overnight at 4 °C. It was then incubated with a horseradish-peroxidase-conjugated secondary antibody and detected with enhanced chemiluminescence. β-Actin was detected on the same membrane and used as the loading control.
All values were expressed as mean ± SE. One-way analysis of variance followed by least significant difference t-test was used to compare the differences between the groups. A two-sided P value < 0.05 was considered to be statistically significant.
To determine the effect of alternol on pancreatic cancer cells, PANC-1 and BxPC3 cells were treated with alternol for 24, 48 and 72 h. Cell viability was measured by cell counting. As shown in Figure 1A and B, alternol inhibited the proliferation of PANC-1 and BxPC3 cells in a dose- and time-dependent manner. The IC50 for PANC-1 and BxPC3 cells was 8.09 ± 0.1 and 8.19 ± 0.2 μmol/L at 24 h, 5.91 ± 0.19 and 6.19 ± 0.2 μmol/L at 48 h, and 4.27 ± 0.11 and 4.46 ± 0.19 μmol/L at 72 h, respectively.
For cell cycle analysis, PANC-1 and BxPC3 cells were treated with increased doses of alternol or vehicle for 24 h and analyzed by flow cytometry. Cell DNA was stained with PI, and the proportion of cells in various phases of the cell cycle was determined by flow cytometry. The population of cells in G1 phase decreased and that in S phase increased in a dose-dependent manner (Figure 2). For the PANC-1 cells, the percentage of cells in G1 phase decreased from 69.28% ± 4.16% to 44.29% ± 12.25%, while those in S phase increased from 17.25% ± 2.14% to 40.55% ± 3.65%. For the BxPC3 cells, the percentage of cells in G1 phase decreased from 87.16% ± 1.78% to 29.35% ± 4.67%, while those in S phase increased from 11.67% ± 2.77% to 44.41% ± 9.8%.
To explore whether alternol could induce apoptosis of pancreatic cancer cells, the PANC-1 and BxPC3 cells were exposed to various concentrations of alternol for 24 h, and apoptosis was measured by TUNEL assay. As shown in Figure 3, alternol treatment has induced apoptosis in a dose-dependent manner, with the proportion of apoptotic cells ranging from 5.04% ± 0.86% for the controls to 54.39% ± 2.7% at 10 μmol/L alternol for the PANC-1 cells, and from 1.64% ± 0.25% for the controls to 51.5% ± 0.75% at 10 μmol/L alternol for the BxPC3 cells (P < 0.01).
After treating the cells with alternol for 24 h, marked morphological changes suggestive of apoptosis, including condensation of chromatin, nuclear fragmentations and apoptotic bodies, were clearly seen upon Hoechst 33258 staining. Alternol treatment induced apoptosis in a dose-dependent manner, with the percentage of apoptotic cells ranging from 4.27% ± 0.34% for the control cells to 45.47% ± 0.59% at 10 μmol/L alternol in the PANC-1 cells, and from 5.36% ± 0.12% in the control cells to 39.67% ± 0.4% at 10 μmol/L alternol in the BxPC3 cells (P < 0.01) (Figure 4).
Changes in MMP are critical for progression of intrinsic apoptosis. To determine whether alternol-induced apoptosis was mediated by the mitochondrion-dependent pathway, we used JC-1 as a mitochondrial depolarization indicator to detect changes in the MMP of living cells. As shown in Figure 5, the red/green fluorescence intensity ratio decreased significantly in both types of cells treated with alternol compared with the controls, indicating that alternol decreased MMP (Figure 5).
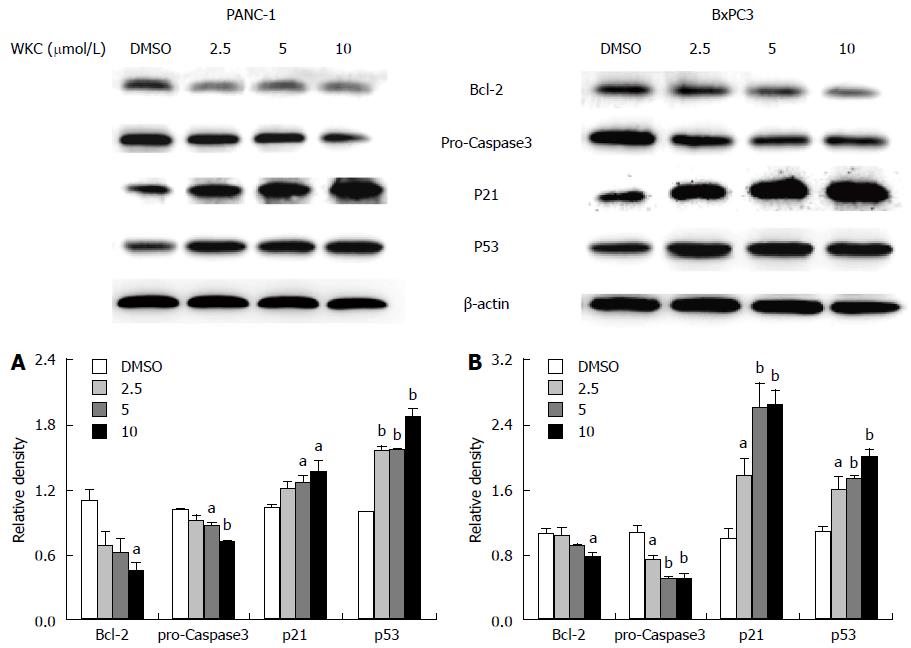
To explore the mechanism of alternol-induced apoptosis, we examined the levels of apoptosis-related proteins in alternol-treated cells. Alternol suppressed expression of Bcl-2 and activated expression of caspase-3 in a dose-dependent manner (Figure 6A and B). For both PANC-1 and BxPC3 cells, treatment with 10 μmol/L alternol for 24 h significantly downregulated expression of Bcl-2 and pro-caspase 3.
Loss of function of p53 has remained a critically important aspect of human cancer development. As a potent inhibitor of cell growth, p53 protein can arrest the progression of cell cycle at several points and induce apoptosis of cells undergoing uncontrolled growth. As shown in Figure 6, alternol treatment upregulated expression of p53 and p21 in a dose-dependent manner (Figure 6A and B).
Alternol is a novel compound isolated from cultured microorganisms from yew bark, and has an inhibitory effect on various cancer cells[11-16]. In the present study, we demonstrated that alternol inhibited the growth of pancreatic cancer cells in vitro in a dose- and time-dependent manner, which suggests a potential role in the treatment of pancreatic cancer.
As shown by flow cytometry, alternol treatment led to accumulation of cells at S phase (Figure 2), and alternol-induced apoptosis increased in a dose-dependent manner (Figure 3). Typical morphological changes of apoptosis were apparent (Figure 4). These suggested that the inhibitory effect of alternol on PANC-1 and BxPC3 cells was probably through induction of cell cycle arrest and apoptosis.
Mitochondria are involved in various cell functions, including differentiation, cell signaling, cell growth, cell death and control of the cell cycle. Mitochondrial disruption may involve changes in MMP and alterations in the oxidation-reduction potential. Changes in MMP are thought to be due to opening of the mitochondrial permeability transition pore, which allows passage of ions and small molecules[17,18]. Therefore, we used JC-1 dye[19] to measure the changes in MMP in alternol-treated cells. We found that red/green fluorescence intensity ratio significantly decreased in PANC-1 and BxPC3 cells treated with alternol compared with control cells (Figure 5). This suggests that alternol-induced apoptosis is caused by mitochondrial depolarization in both cells.
p53 is a tumor suppressor gene that encodes a DNA-binding transcription factor that induces cell growth arrest, senescence and cell death by apoptosis upon cellular stress. p53 can regulate several genes, including p21 that blocks cell cycle progression and Bax that promotes apoptosis[20,21]. Mutations of the p53 gene have been detected in various human tumors, including over half of pancreatic adenocarcinomas. Restoration of p53 function in such tumor cells may induce robust cell death, allowing efficient eradication of the tumor. Targeting of mutant p53 in tumors is a rapidly developing field at the forefront of translational cancer research. Various approaches have led to the identification of small molecules that can rescue mutant p53[22,23]. In the present study, we found that alternol increased the abundance of p53 and p21 proteins in a dose-dependent manner (Figure 6).
The Bcl-2 family of proteins comprises antiapoptotic members such as Bcl-2, Bcl-XL and Mcl-1, and proapoptotic proteins such as Bax, Bak and Bad. Imbalances in the ratio of antiapoptotic vs proapoptotic Bcl-2 family proteins are found in several human cancers including pancreatic carcinoma[18,24,25]. To explore whether alternol can trigger an intrinsic apoptotic cascade in PANC-1 and BxPC3 cells, we examined expression of Bcl-2 protein with western blotting. Expression of Bcl-2 gradually decreased in alternol-treated cells in a dose-dependent manner, suggesting that alternol induces apoptosis through the intrinsic pathway.
Caspases are a family of cysteine proteases that plays a central role in apoptotic signaling. Activation of caspase cascades has been demonstrated in apoptosis. Our study showed that alternol treatment caused a dose-dependent decrease in expression of pro-caspase 3 protein in pancreatic cancer cells (Figure 6).
Our results show that alternol inhibits the growth of pancreatic cancer cells via cell cycle arrest and apoptosis induction. Alternol therefore has the potential to be developed as a therapeutic agent for pancreatic cancer.
At present, radical surgery offers the only curative treatment of pancreatic cancer. Alternative or combined treatment consists of adjuvant or neoadjuvant chemotherapy with or without radiotherapy.
With a molecular weight of 352, alternol is a novel compound isolated from the fermentation products of a novel microorganism mutant strain Alternaria alternata var. monosporus, which is obtained from the bark of yew trees in Kunming, China. It can also inhibit the migration and invasion of hepatocellular carcinoma and melanoma cells. Alternol has shown anti-cancer activity against various types of cancer cells.
The authors investigated the effect of alternol on the proliferation, cell cycle and apoptosis of pancreatic cancer cells. To explore the underlying molecular mechanisms, the authors also analyzed the expression of proteins related to apoptosis using western blotting.
Alternol can inhibit the growth of pancreatic cancer cells via cell cycle arrest and apoptosis induction.
The authors investigated the effect of alternol on pancreatic cancer cells, and they demonstrated that alternol inhibited the growth of pancreatic cancer cells via cell cycle arrest and apoptosis induction. The present data suggest that the agent has the potential to be developed as an anti-tumor agent for the treatment of pancreatic cancers.
P- Reviewer: Koulaouzidis A, Kouraklis G, Iwasaki Y, Shimizu Y, Tian YT S- Editor: Qi Y L- Editor: Kerr C E- Editor: Wang CH
| 1. | Bardou M, Le Ray I. Treatment of pancreatic cancer: A narrative review of cost-effectiveness studies. Best Pract Res Clin Gastroenterol. 2013;27:881-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Gnoni A, Licchetta A, Scarpa A, Azzariti A, Brunetti AE, Simone G, Nardulli P, Santini D, Aieta M, Delcuratolo S. Carcinogenesis of pancreatic adenocarcinoma: precursor lesions. Int J Mol Sci. 2013;14:19731-19762. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 3. | Li D, Sun X, Zhang L, Yan B, Xie S, Liu R, Liu M, Zhou J. Histone deacetylase 6 and cytoplasmic linker protein 170 function together to regulate the motility of pancreatic cancer cells. Protein Cell. 2014;5:214-223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 4. | Antoniou G, Kountourakis P, Papadimitriou K, Vassiliou V, Papamichael D. Adjuvant therapy for resectable pancreatic adenocarcinoma: review of the current treatment approaches and future directions. Cancer Treat Rev. 2014;40:78-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Wolfgang CL, Herman JM, Laheru DA, Klein AP, Erdek MA, Fishman EK, Hruban RH. Recent progress in pancreatic cancer. CA Cancer J Clin. 2013;63:318-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 572] [Cited by in RCA: 680] [Article Influence: 56.7] [Reference Citation Analysis (0)] |
| 6. | Herman JM, Fan KY, Wild AT, Hacker-Prietz A, Wood LD, Blackford AL, Ellsworth S, Zheng L, Le DT, De Jesus-Acosta A. Phase 2 study of erlotinib combined with adjuvant chemoradiation and chemotherapy in patients with resectable pancreatic cancer. Int J Radiat Oncol Biol Phys. 2013;86:678-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Kim EJ, Ben-Josef E, Herman JM, Bekaii-Saab T, Dawson LA, Griffith KA, Francis IR, Greenson JK, Simeone DM, Lawrence TS. A multi-institutional phase 2 study of neoadjuvant gemcitabine and oxaliplatin with radiation therapy in patients with pancreatic cancer. Cancer. 2013;119:2692-2700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 132] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 8. | Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, Seay T, Tjulandin SA, Ma WW, Saleh MN. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369:1691-1703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4035] [Cited by in RCA: 4883] [Article Influence: 406.9] [Reference Citation Analysis (0)] |
| 9. | Ma WW, Hidalgo M. The winning formulation: the development of paclitaxel in pancreatic cancer. Clin Cancer Res. 2013;19:5572-5579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | Yeung ED, Morrison A, Plumeri D, Wang J, Tong C, Yan X, Li J. Alternol exerts prostate-selective antitumor effects through modulations of the AMPK signaling pathway. Prostate. 2012;72:165-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Liu X, Wang J, Sun B, Zhang Y, Zhu J, Li C. Cell growth inhibition, G2M cell cycle arrest, and apoptosis induced by the novel compound Alternol in human gastric carcinoma cell line MGC803. Invest New Drugs. 2007;25:505-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Liu L, Zhang B, Yuan X, Wang P, Sun X, Zheng Q. Alternol induces an S-phase arrest of melanoma B16F0 cells. Cell Biol Int. 2014;38:374-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Liu ZZ, Zhu J, Sun B, Liu S, Geng S, Liu X, Li CL. Alternol inhibits proliferation and induces apoptosis in mouse lymphocyte leukemia (L1210) cells. Mol Cell Biochem. 2007;306:115-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Tang Y, Chen R, Huang Y, Li G, Huang Y, Chen J, Duan L, Zhu BT, Thrasher JB, Zhang X. Natural compound Alternol induces oxidative stress-dependent apoptotic cell death preferentially in prostate cancer cells. Mol Cancer Ther. 2014;13:1526-1536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Zhu XL, Wang YL, Chen JP, Duan LL, Cong PF, Qu YC, Li-Ling J, Zhang MX. Alternol inhibits migration and invasion of human hepatocellular carcinoma cells by targeting epithelial-to-mesenchymal transition. Tumour Biol. 2014;35:1627-1635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Wang Z, Wang D, Liu L, Guo D, Yu B, Zhang B, Han B, Sun X, Zheng Q. Alteronol inhibits the invasion and metastasis of B16F10 and B16F1 melanoma cells in vitro and in vivo. Life Sci. 2014;98:31-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Leu WJ, Chang HS, Chan SH, Hsu JL, Yu CC, Hsu LC, Chen IS, Guh JH. Reevesioside A, a cardenolide glycoside, induces anticancer activity against human hormone-refractory prostate cancers through suppression of c-myc expression and induction of G1 arrest of the cell cycle. PLoS One. 2014;9:e87323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Lindsay J, Esposti MD, Gilmore AP. Bcl-2 proteins and mitochondria--specificity in membrane targeting for death. Biochim Biophys Acta. 2011;1813:532-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 269] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 19. | Lee HS, Cho HJ, Yu R, Lee KW, Chun HS, Park JH. Mechanisms underlying apoptosis-inducing effects of Kaempferol in HT-29 human colon cancer cells. Int J Mol Sci. 2014;15:2722-2737. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 93] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 20. | Liao JM, Cao B, Zhou X, Lu H. New insights into p53 functions through its target microRNAs. J Mol Cell Biol. 2014;6:206-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 21. | Hu W, Zhang C, Wu R, Sun Y, Levine A, Feng Z. Glutaminase 2, a novel p53 target gene regulating energy metabolism and antioxidant function. Proc Natl Acad Sci USA. 2010;107:7455-7460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 561] [Cited by in RCA: 672] [Article Influence: 44.8] [Reference Citation Analysis (0)] |
| 22. | Muller PA, Vousden KH. Mutant p53 in cancer: new functions and therapeutic opportunities. Cancer Cell. 2014;25:304-317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1147] [Cited by in RCA: 1158] [Article Influence: 105.3] [Reference Citation Analysis (0)] |
| 23. | Liu X, Wilcken R, Joerger AC, Chuckowree IS, Amin J, Spencer J, Fersht AR. Small molecule induced reactivation of mutant p53 in cancer cells. Nucleic Acids Res. 2013;41:6034-6044. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 147] [Cited by in RCA: 191] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 24. | Roy MJ, Vom A, Czabotar PE, Lessene G. Cell death and the mitochondria: therapeutic targeting of the BCL-2 family-driven pathway. Br J Pharmacol. 2014;171:1973-1987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 94] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 25. | Fulda S. Targeting apoptosis signaling in pancreatic cancer. Cancers (Basel). 2011;3:241-251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |