Published online Apr 21, 2015. doi: 10.3748/wjg.v21.i15.4440
Peer-review started: December 16, 2014
First decision: January 8, 2015
Revised: January 26, 2015
Accepted: February 11, 2015
Article in press: February 11, 2015
Published online: April 21, 2015
Processing time: 128 Days and 17.1 Hours
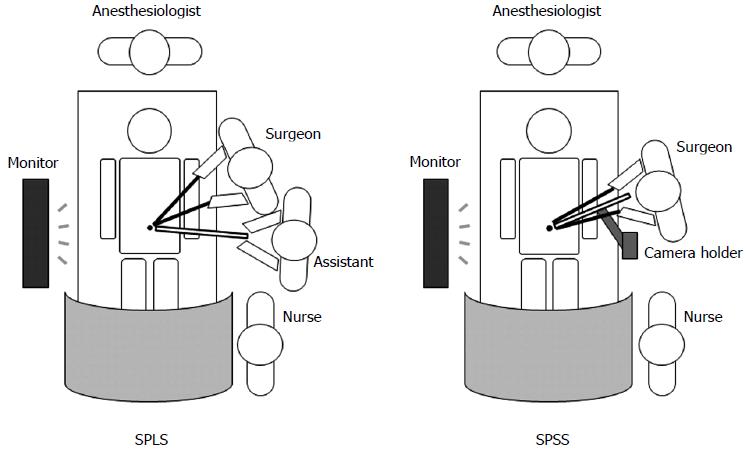
With the aid of advanced surgical techniques and instruments, single-port laparoscopic surgery (SPLS) can be accomplished with just two surgical members: an operator and a camera assistant. Under these circumstances, the reasonable replacement of a human camera assistant by a mechanical camera holder has resulted in a new surgical procedure termed single-port solo surgery (SPSS). In SPSS, the fixation and coordinated movement of a camera held by mechanical devices provides fixed and stable operative images that are under the control of the operator. Therefore, SPSS primarily benefits from the provision of the operator’s eye-to-hand coordination. Because SPSS is an intuitive modification of SPLS, the indications for SPSS are the same as those for SPLS. Though SPSS necessitates more actions than the surgery with a human assistant, these difficulties seem to be easily overcome by the greater provision of static operative images and the need for less lens cleaning and repositioning of the camera. When the operation is expected to be difficult and demanding, the SPSS process could be assisted by the addition of another instrument holder besides the camera holder.
Core tip: Solo surgery occurs when one surgeon operates with only a scrub nurse. The use of a mechanical camera holder makes such surgery possible. Solo surgery is particularly useful when it is applied to single-port laparoscopic surgery (SPLS); it is then termed single-port solo surgery (SPSS). SPSS facilitates a better operative environment than does SPLS by allowing fixed and stable images under the operator’s direct control. SPSS indications include SPLS indications, after the technique has been mastered. Moreover, total skin-to-skin SPSS could be easily realized by the extraperitoneal application of a retractor system that facilitates incision making and peritoneal opening.
- Citation: Kim SJ, Lee SC. Technical and instrumental prerequisites for single-port laparoscopic solo surgery: State of art. World J Gastroenterol 2015; 21(15): 4440-4446
- URL: https://www.wjgnet.com/1007-9327/full/v21/i15/4440.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i15.4440
Surgical techniques have been continually evolving and are currently evolving in the direction of increasing radicality as well as cosmetic effects. Whereas meticulous lymph node dissection for cancer surgery represents the pursuit for radicality, the introduction of laparoscopic surgery represents the pursuit for cosmetic effects. Interestingly, these efforts have resulted, perhaps inevitably, in the reduction of human resources during operations.
The reduction of human resources during operations can be attributed to the advanced surgical techniques and instruments. Laparoscopic surgery usually requires two or three surgical assistants. Recently, the introduction of single-port laparoscopic surgery (SPLS) has further reduced the number of the surgical members; in SPLS, a greater dependence of an operator usually negates the need for a human assistant holding an instrument except for the camera. Therefore, SPLS usually requires just two surgical members, such as an operator and a camera assistant. This environment orchestrated by SPLS opened the possibility of solo surgery.
Solo surgery can be defined as a practice in which a surgeon operates alone, without other surgical members except for a scrub nurse[1]. Several mechanical camera holders have been invented to facilitate solo surgery. The fixation and coordinated movement of a camera held by mechanical devices makes it possible to perform solo surgery. In SPLS, the operating surgeon governs the whole operative process through bimanual manipulation, while an assistant guides the laparoscopic camera. Therefore, the simple replacement of a human assistant by a mechanical camera holder in SPLS makes solo surgery possible. We herein termed the SPLS driven by solo surgery as single-port solo surgery (SPSS); therefore, solo surgery includes SPSS. Currently, SPSS has been rarely reported, and thus, the role of SPSS in surgical operations should be determined.
Initially, SPSS can be applied to operations accomplished within a single abdominal quadrant, because these kinds of operations do not require the camera to be frequently repositioned. Such operations include appendectomies, cholecystectomies, and splenectomies. Moreover, as operators’ experience increases, SPSS indications could be extended to include trans-quadrant operations and even surgeries for malignant diseases. Our institution initiated SPLS in October 2008 and SPSS in September 2012. During that time, we have performed a number of operations using the SPSS technique, including small bowel resection, right hemicolectomy, low anterior resection, total proctocolectomy, combined abdominoperineal resection and cholecystectomy, pancreatectomy and live kidney donor nephrectomy. When a challenging operation was expected, the solo surgery could be assisted by an instrument holder in addition to the camera holder[1]. In our experience, the indications for SPSS are the same as those for SPLS, once the operator has overcome the learning curve for SPSS, because SPSS was not designed to discomfort SPLS, but to comfort SPLS.
Solo surgery is achieved by utilizing a camera holder rather than a human camera assistant. Since the manipulation of the laparoscope is at the operator’s will, solo surgery can overcome the main disadvantage of laparoscopic surgery; namely, the dissociation between the operator’s eye and hand. Laparoscopy has revolutionized surgical operations by providing a novel way to reach target organs. Thereby, it significantly reduces abdominal wall injuries and speeds the patient’s recovery. However, in contrast to open surgery, in laparoscopic surgery, the surgeon cannot control the operative field for himself or herself. This indirect way of observing and manipulating hinders coordinated surgical procedures, especially in challenging and complicated operations. Laparoscopy can sometimes lead to communication problems between the surgeon and the assistant and to unstable camera images when the assistant has to stand fixed for a long time. It has been reported that unsteady camera images directly hinder the performance of goal-directed hand movements[2]. Solo surgery provides fixed and stable images under the direct control of the operator himself or herself. Therefore, solo surgery can be the best way to overcome these shortcomings.
In addition, solo surgery helps economize staff numbers, thus helping to reduce health care costs. In South Korea and certain other countries, a decline in residency applications to surgical departments has produced manpower shortages in a number of hospitals. Under these circumstances, solo surgery paves the way for accommodating larger numbers of operations with limited manpower. Moreover, solo surgery provides sufficient room for an operating surgeon. The shortcomings of SPLS are related not only to the crowding and clashing of instruments but also to the discomfort that arises from being obliged to share a small space with an assistant. In solo surgery, the surgeon can freely use the available space, which not only provides a comfortable environment but also enables the surgeon to perform various procedures freely and conveniently (Figure 1).
There are several considerations in performing solo surgery. The most serious shortcoming of solo surgery is the potential for time lags between an emergency arising and its surgical control, which can be delayed due to later arrival of surgical personnel. To cope with unexpected emergencies, there should be an agreement of temporal (the time interval before the arrival of surgical members) surgical assistance by the personnel in an operating room. Next, the positioning of the fixed camera holder itself occasionally hinders the operative procedure, which can be overcome by repositioning. Finally, solo surgery obligates the solo surgeon to make important surgical decisions alone during surgery by disallowing discussion between surgical members, allows the solo surgeon feel loneliness, and does not provide appropriate residency training.
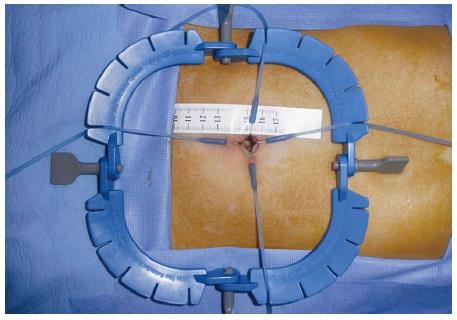
According to the proportion of solo procedures needed for a surgical procedure, solo surgery can be divided into total solo surgery and partial solo surgery. Total solo surgery describes the surgery in which total, skin-to-skin involvement of solo procedure is used, and partial solo surgery describes the surgery in which solo surgery is only a part (i.e., laparoscopic surgery) of the total operation. Therefore, total solo surgery includes solo performance of extraperitoneal procedures, including incision making and peritoneal opening. For this purpose, operators can use the Lone Star Retractor System (Cooper Surgical, Trumbull, CT) with 3-mm sharp disposable hooks (Cooper Surgical) (Figure 2)[3]. The Lone Star Retractor System is a self-retaining retractor that was originally designed for the superior visualization of anal procedures (e.g., anorectal anastomoses), and it can therefore successfully replace human personnel who help visualize optimal skin incision. Just as a camera holder is used for the intraperitoneal procedures, so the Lone Star retractor provides sufficient operative vision for extraperitoneal procedures in total solo surgery.
Camera holders utilized during solo surgery can be divided into passive and active camera holders; the former are manually controlled and the latter are driven by electrical motors[1]. A passive camera holder is composed of several bars connected by a ball-joint system. Its base is anchored to the operating table rail, and its tip usually grasps the camera by a clamp. When using passive camera holders, it is important to determine whether single-handed repositioning is possible, as that increases operative convenience.
Passive camera holders can be subdivided according to whether or not they enable single-handed repositioning (Figure 3). Passive camera holders that enable single-handed repositioning include Unitrac (AESCULAP, Tuttlingen, Germany)[4,5], Endofreeze (AESCULAP)[6], and Laparostat (CIVCO, Carolville, IA)[7]. The ball joints enabling single-handed repositioning are pneumatically blocked, making it possible to reposition them with just one hand. The reposition is usually accomplished by pressing a button or by providing adjustable friction. In addition, passive camera holders that do not allow single-handed repositioning include Martin arm (Gebuder Martin, Tuttlingen, Germany)[4,8,9], Karl Storz Holding systems (Karl Storz, Tullingen, Germany)[10], and Assisto (GEOMED, Tuttlingen, Germany)[11]. After repositioning, they should be manually locked using a knob; one hand releases the brake and the other hand repositions the holder.
Regardless of whether single-handed repositioning is possible, releasing and repositioning the holder can be troublesome during operative procedures. However, there are reports that these activities do not prolong operation times[8,12], which may be attributed to a highly reduced number of camera movements[8,12] and to the provision of a more stable image[9,12]. The operative procedure cannot be advanced during camera repositioning either by a human assistant or by a passive holder. Therefore, surgeons indicate that the time interval consumed for repositioning the camera does not prevent the coordinated process of operation.
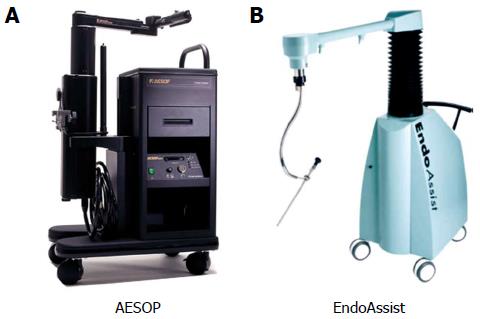
An active camera holder is a motorized camera holder that is typically composed of a machine body and an arm. Various user interfaces determine the way of controlling the electric motor. These holders are not completely autoclavable because of their large capacity and the built-in motor; therefore, during surgery, they are used wrapped with sterile drapes except for the autoclavable portion.
A number of user interfaces have been developed to replace the manual release of the camera holder during repositioning, including head movements, voice control, and finger- and foot activated switches[13-15]. These are convenient ways of controlling the camera; however, they may be less intuitive and slower than passive holders because one controlling activity allows just one degree of freedom.
One of the well-known active camera holders is the AESOP robot (Automated Endoscopic System for Optimal Positioning robot; Computer Motion, Coletta, CA)[8,12,14-20]. It consists of a robotic endoscopic positioning system with an elbow-shaped arm capable of moving the endoscope driven by hand, foot, or voice control[8] (Figure 4A). Another representative active camera holder that incorporates an electromechanical arm is the EndoAssist (Armstrong Healthcare Ltd, High Wycombe, United Kingdom)[8,15,21]. The EndoAssist uses a head-motion navigation system (Figure 4B).
Complicated laparoscopic solo surgery procedures can be assisted by another instrument holder in addition to a camera holder. Because the retracting procedure is static, it seems appropriate to use a passive holder for the retraction. In solo surgery using two passive holders, operators should pay attention to the positioning of these holders because the fixation of the camera holders occasionally hinders the convenience of the operative procedure.
Under general anesthesia, the patient is placed in a supine position. The patient’s one-sided arm is adducted in order to provide sufficient space for the solo surgeon. Only one operative monitor is required for SPSS; the monitor is placed on the opposite site of the operator (Figure 1).
After routine painting and draping of the patient, a vertical 10-mm long transumbilical skin incision is made. Thereafter, a Lone Star retractor (3307G, Cooper Surgical, Trumbull, CT) is applied on the skin (Figure 2). The Lone Star Retractor System consists of self-retaining retractor rings and elastic stays. After putting the Lone Star Retractor centered in the umbilicus, the first stay (3311-8G, 3-mm sharp hook, Cooper Surgical) is placed. The stay is pulled in the desired direction with the desired tension and is then placed in one of the slots of the retractor. Likewise, four stay sutures are placed counter-directionally to maximally expose the fascial layer of the umbilicus. With the fully exposed fascial layer, the fascia is transversely incised and the peritoneum is entered. At this time, two or three transfascial stay sutures are pre-established to facilitate later fascial closure at the end of surgery.
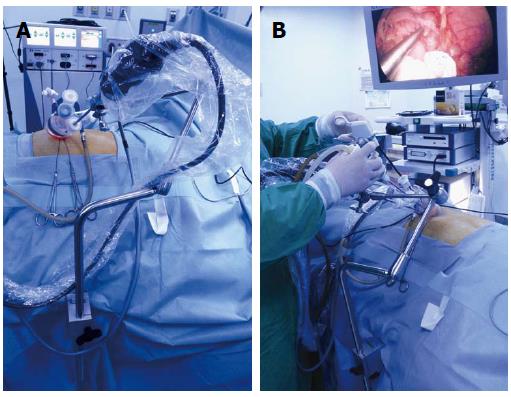
For performing SPSS, one can choose any type of single-port designed for SPLS to one’s taste. We typically used Glove port (431AT-2W; Nelis, Bucheon, South Korea). After the establishment of the single port, the abdomen is insufflated with CO2 to a pressure of 12 mmHg. Then, the solo surgeon installs active or passive camera holder. In our institution, we used a passive camera holder (Karl Storz Holding Systems combining 28172 HR, 28172 HA, and 28172 UL). It has a lockable joint mechanism and five joint functions, which ensure exact positioning of the instrument. The standard laparoscopic 5-mm camera (Full HD Laparoscope 5 mm; AESCULAP) is attached to the camera holder. After attainment of best surgical vision, the laparoscope is fixed using the camera holder (Figure 5A). Thereafter, the solo surgeon can perform the surgical procedure with a bimanual maneuver (Figure 5B). The following surgical procedure does not differ significantly from SPLS. Likewise, throughout the full skin-to-skin procedure, only one surgeon is involved in the procedure.
Passive camera holders were compared with human camera assistants in clinical[9,12] and phantom[8] experiments with no significant differences in the operation time. However, it was reported that the time related to setting up and breaking down was prolonged in the passive holder group.
There have been also several studies comparing laparoscopic surgery assisted by either a human assistant or an active camera holder in clinical[12-14,19,20,22-24] and phantom experiments[8,25]. The operator was more aware of the fact that he or she was focused on the operation using the active camera holder, possibly due to fewer lens cleanings, and the operation time with the active holders was at best equal to those with human assistants. However, set-up and break-down time was prolonged in the active holder group. The use of active holders was also supported by a number of papers in terms of efficiency, safety, and provision of stable operative images[12,16,22]. In a study, two active holders - AESOP and Endosista - were compared, and AESOP was found to be quicker and more accurate in repositioning[15].
Active and passive camera holders and human assistants were also compared. In a study comparing active (AESOP) and passive (PASSIST) camera holders and human assistants, both holders resulted in a similar operative proficiency and operation time[12]. In addition, the use of these camera holders significantly decreased the number of camera repositioning actions compared to human assistance. In a laboratory setting of phantom cholecystectomy, the human assistant groups showed the shortest operation time, and the passive holder group (Tiska and Martin arm) ranked next; the active holder groups (AESOP, Endosista, and FIPS) showed the longest operation time[8]. The authors concluded that the combination of two passive holders, one for the scope and one for the instrument, is the optimal combination for cholecystectomy during solo surgery.
As the SPLS technique has been widely performed, SPSS indications have been extended to include operations covering multiple quadrants and even malignant diseases. Solo surgery using either active or passive holders is intuitive and proficient by allowing eye-and-hand coordination, and provide more static and stable operative images compared to surgery performed with human assistants. Although solo surgery necessitates more actions and longer operative times than surgery with human assistants, these difficulties seemed to be outweighed by the greater provision of stable operative images and a reduced need for lens cleaning and camera repositioning actions. When a challenging operation is encountered, the solo surgery could be assisted by the addition of another instrument holder besides a camera holder.
To date, the use of a passive rather than an active camera holder seems to be the most beneficial, considering the relative advantages in terms of cost, convenient usage, and equivalent surgical outcomes. Regarding passive camera holders, we recommend the use of holders that enable single-handed repositioning because of their convenience. Moreover, total skin-to-skin solo surgery could be easily realized by the extraperitoneal application of the Lone Star Retractor system, which facilitates incision making and peritoneal opening.
P- Reviewer: Iso Y, Karakus OZ, Surlin V S- Editor: Ma YJ L- Editor: A E- Editor: Liu XM
| 1. | Jaspers JE, Breedveld P, Herder JL, Grimbergen CA. Camera and instrument holders and their clinical value in minimally invasive surgery. Surg Laparosc Endosc Percutan Tech. 2004;14:145-152. [PubMed] |
| 2. | Mohrmann-Lendla H, Fleischer AG. The effect of a moving background on aimed hand movements. Ergonomics. 1991;34:353-364. [PubMed] [DOI] [Full Text] |
| 3. | Lone Star Retractor System. 2014, December 11. Available from: http://coopersurgical.com/Our-Brands/Lone-Star-Retractor-System. |
| 4. | Melzer A, Buess G, Cuschieri A. Instrument for endoscopic surgery. In: Cuschieri A, editors. Operative manual of Endoscopic Surgery. 1992;14-36. |
| 5. | Lee YS, Jeon HG, Lee SR, Jeong WJ, Yang SC, Han WK. The feasibility of solo-surgeon living donor nephrectomy: initial experience using video-assisted minilaparotomy surgery. Surg Endosc. 2010;24:2755-2759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Arezzo A, Schurr MO, Braun A, Buess GF. Experimental assessment of a new mechanical endoscopic solosurgery system: Endofreeze. Surg Endosc. 2005;19:581-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Arezzo A; Laparostat. 2014, December 11. Available from: https://www.yumpu.com/no/document/view/20462143/laparostattm-kit-civco-medical-solutions. |
| 8. | Arezzo A, Ulmer F, Weiss O, Schurr MO, Hamad M, Buess GF. Experimental trial on solo surgery for minimally invasive therapy: comparison of different systems in a phantom model. Surg Endosc. 2000;14:955-959. [PubMed] |
| 9. | Laporte E, Arner , AM , Garcia San Pedro A. Usefulness of a arm supporting the camera of video-endoscopy. A comparative study with manual guidance: Proceedings 9th Int Congr EAES 2001; . |
| 10. | KARL Storz Holding systems. 2014, December 11. Available from: https://www.karlstorz.com/cps/rde/xbcr/karlstorz_assets/ASSETS/2193450.pdf. |
| 11. | Robotics in endoscopic surgery: can mechanical manipulators provide a more simple solution for the problem of limited degrees of freedom? Minim Invasive Ther Allied Technol. 2001;10:289-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | den Boer KT, Bruijn M, Jaspers JE, Stassen LP, Erp WF, Jansen A, Go PM, Dankelman J, Gouma DJ. Time-action analysis of instrument positioners in laparoscopic cholecystectomy. Surg Endosc. 2002;16:142-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Gillen S, Pletzer B, Heiligensetzer A, Wolf P, Kleeff J, Feussner H, Fürst A. Solo-surgical laparoscopic cholecystectomy with a joystick-guided camera device: a case-control study. Surg Endosc. 2014;28:164-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 14. | Kalteis M, Pistrich R, Schimetta W, Pölz W. Laparoscopic cholecystectomy as solo surgery with the aid of a robotic camera holder: a case-control study. Surg Laparosc Endosc Percutan Tech. 2007;17:277-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Yavuz Y, Ystgaard B, Skogvoll E, Mårvik R. A comparative experimental study evaluating the performance of surgical robots aesop and endosista. Surg Laparosc Endosc Percutan Tech. 2000;10:163-167. [PubMed] |
| 16. | Merola S, Weber P, Wasielewski A, Ballantyne GH. Comparison of laparoscopic colectomy with and without the aid of a robotic camera holder. Surg Laparosc Endosc Percutan Tech. 2002;12:46-51. [PubMed] |
| 17. | Roe DB, Wang Y. A voice-controlled network for universal control of devices in the OR. Minim Invasive Ther Allied Technol. 2000;9:185-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Sackier JM, Wang Y. Robotically assisted laparoscopic surgery. From concept to development. Surg Endosc. 1994;8:63-66. [PubMed] |
| 19. | Fujii S, Watanabe K, Ota M, Yamagishi S, Kunisaki C, Osada S, Ike H, Ichikawa Y, Endo I, Shimada H. Solo surgery in laparoscopic colectomy: a case-matched study comparing robotic and human scopist. Hepatogastroenterology. 2011;58:406-410. [PubMed] |
| 20. | Proske JM, Dagher I, Franco D. Comparative study of human and robotic camera control in laparoscopic biliary and colon surgery. J Laparoendosc Adv Surg Tech A. 2004;14:345-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Gilbert JM. The EndoAssist robotic camera holder as an aid to the introduction of laparoscopic colorectal surgery. Ann R Coll Surg Engl. 2009;91:389-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Aiono S, Gilbert JM, Soin B, Finlay PA, Gordan A. Controlled trial of the introduction of a robotic camera assistant (EndoAssist) for laparoscopic cholecystectomy. Surg Endosc. 2002;16:1267-1270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 88] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 23. | Kimura T, Umehara Y, Matsumoto S. Laparoscopic cholecystectomy performed by a single surgeon using a visual field tracking camera: early experience. Surg Endosc. 2000;14:825-829. [PubMed] |
| 24. | Niebuhr H, Born O. [Image tracking system. A new technique for safe and cost-saving laparoscopic operation]. Chirurg. 2000;71:580-584. [PubMed] |
| 25. | Buess GF, Arezzo A, Schurr MO, Ulmer F, Fisher H, Gumb L, Testa T, Nobman C. A new remote-controlled endoscope positioning system for endoscopic solo surgery. The FIPS endoarm. Surg Endosc. 2000;14:395-399. [PubMed] |