Published online Apr 14, 2015. doi: 10.3748/wjg.v21.i14.4413
Peer-review started: November 5, 2014
First decision: December 11, 2014
Revised: December 25, 2014
Accepted: January 21, 2015
Article in press: January 21, 2015
Published online: April 14, 2015
Processing time: 161 Days and 23.2 Hours
Ectopic insulinoma is a very rare and dormant tumor. Here we report the case of a 79-year-old female who presented with repeated episodes of hypoglycemia and was diagnosed with insulinoma based on laboratory and imaging examinations. Computed tomography and positron emission tomography revealed a tumor in the retroperitoneum under and left of the hepatoduodenal ligament, which was resected successfully using a laparoscopic approach. Pathologic results revealed an ectopic insulinoma, which was confirmed immunohistochemically. Ectopic insulinomas are accompanied by hypoglycemia that can be misdiagnosed as drug- or disease-induced. These tumors are difficult to diagnose and locate, particularly in atypical cases or for very small tumors. Synthetic or targeted examinations, including low blood glucose, elevated insulin, proinsulin, and C-peptide levels, 48-h fasting tests, and relevant imaging methods should be considered for suspected cases of insulinoma. Surgery is the treatment of choice for patients with insulinoma, and laparoscopic resection is a feasible and effective method for select ectopic insulinoma cases.
Core tip: Ectopic insulinoma is a very rare and dormant disease that is difficult to diagnose and locate. It should be considered in the differential diagnosis of cases of hypoglycemia thought to be caused by drugs and other diseases. Correlative laboratory and imaging examinations are necessary, and laparoscopic resection is a feasible and effective treatment approach.
- Citation: Liu J, Zhang CW, Hong DF, Wu J, Yang HG, Chen Y, Zhao DJ, Zhang YH. Laparoscope resection of retroperitoneal ectopic insulinoma: A rare case. World J Gastroenterol 2015; 21(14): 4413-4418
- URL: https://www.wjgnet.com/1007-9327/full/v21/i14/4413.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i14.4413
Hypoglycemia is commonly encountered in daily clinical practice and often occurs during the treatment of diabetes mellitus. The condition is most often the result of insulin or other anti-diabetic agents and ethanol[1-3], though a small minority of hypoglycemia cases are spontaneous[4]. Hypoglycemia can also be caused by adrenal or hepatic diseases, gastrointestinal stromal and retroperitoneal tumors, endocrine deficiency, and even breast tumors[5-9], and rarely from hypocortisolism[10] and non-Hodgkin lymphoma[11]. Additionally, some fruits may lead to hypoglycemia[12].
Although rare, hypoglycemia can be caused by an insulinoma, the most common hormone-secreting islet cell tumor. In such instances, the diagnosis is made when hypoglycemia occurs in the presence of symptoms of neuroglycopenia and inappropriately high levels of insulin and C-peptide. Additional imaging is often required to detect the underlying insulinoma. In the present paper, we describe the clinical and pathologic features of a rare case of hypoglycemia involving a functioning retroperitoneal insulinoma, and review the literature related to this topic to provide a comprehensive overview of this very rare and challenging tumor type.
A 79-year-old woman was referred to our hospital because of recurrent vertigo, weakness, and loss of consciousness experienced over a period of 9 mo, which often occurred during fasting, hunger, or exercise. When an episode occurred, serum glucose fluctuated between 2.0 and 2.5 mmol/L (the lowest value was 1.5 mmol/L), and symptoms resolved after ingestion of glucose, dextrose, or dessert. The patient had never taken any sulfonylurea drugs.
Her physical examination was unremarkable; the thyroid was normal and no nodules were palpable. A brain computed tomography (CT) scan ruled out any focal or diffuse encephalic lesion. After admission, her serum glucose level was 2.4 mmol/L (normal value: 3.3-6.2 mmol/L), insulin was 35.4 μU/mL (normal value: 4.0-16.8 μU/mL), and C-peptide was 2.5 ng/mL (normal value: 1.0-4.5 ng/mL). Tumor markers were within normal limits. No symptoms related to upper gastrointestinal occlusion or bleeding were noted. The presence of the Whipple triad and results of the 48-h fasting test suggested a diagnosis of insulinoma.
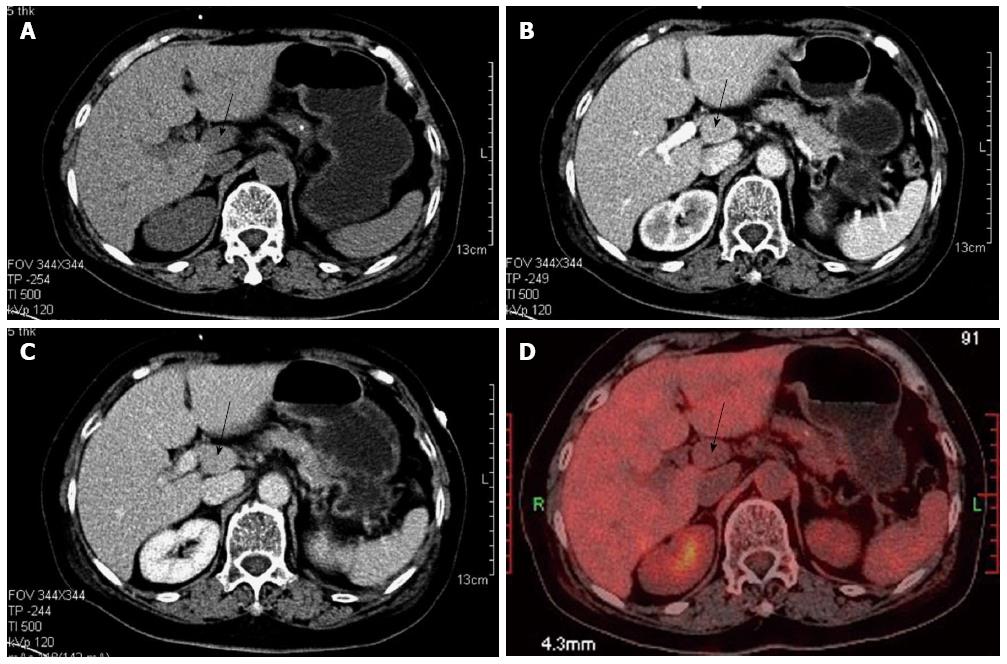
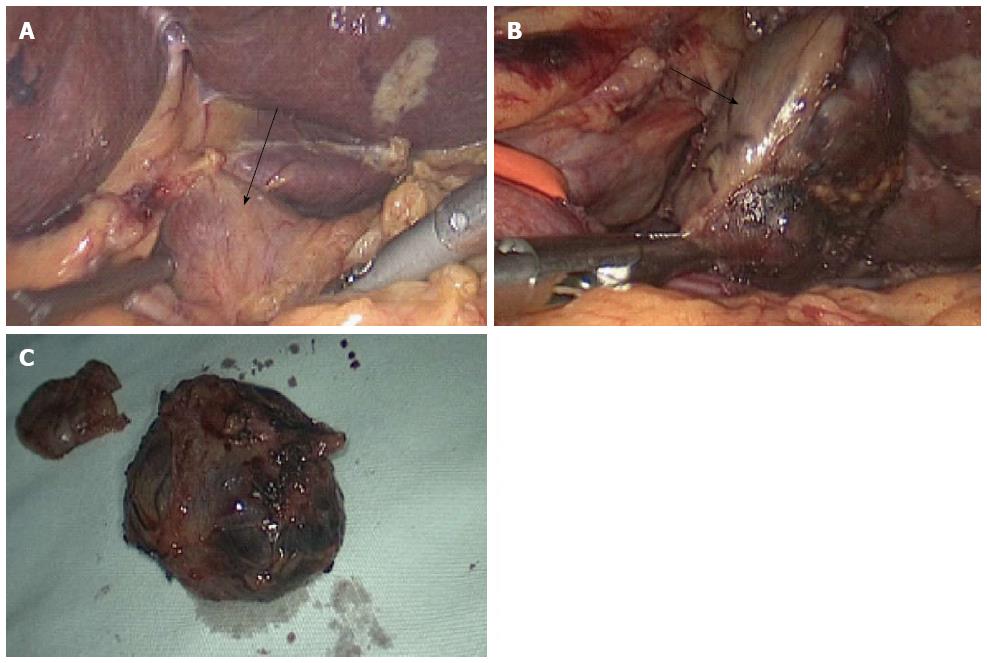
Regular transabdominal ultrasound yielded negative findings in the pancreas. An abdominal CT/positron emission tomography (PET) scan also showed no evidence of a pancreatic tumor, but revealed a 2.5 × 1.0 cm solid polyp in the retroperitoneum under and left of the hepatoduodenal ligament (Figure 1). Thus, the presumptive diagnosis of ectopic insulinoma was made, and a laparoscopic tumor resection was performed. The gastrocolic ligament was detached with a harmonic scalpel to completely expose the neck, body, and tail of the pancreas, and no mass was detected. The lesser omentum was then opened to move the hepatoduodenal ligament to the right in order to expose the tumor. An isolated, pink, and slightly hard tumor (2.5 cm in diameter) was clearly identified in the retroperitoneum under the hepatoduodenal ligament with the assistance of intraoperative laparoscopic endoscopy. A laparoscopic resection of the tumor was successfully performed using a harmonic scalpel (Figure 2).
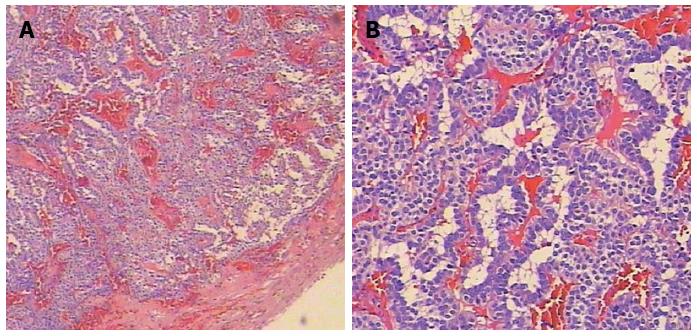
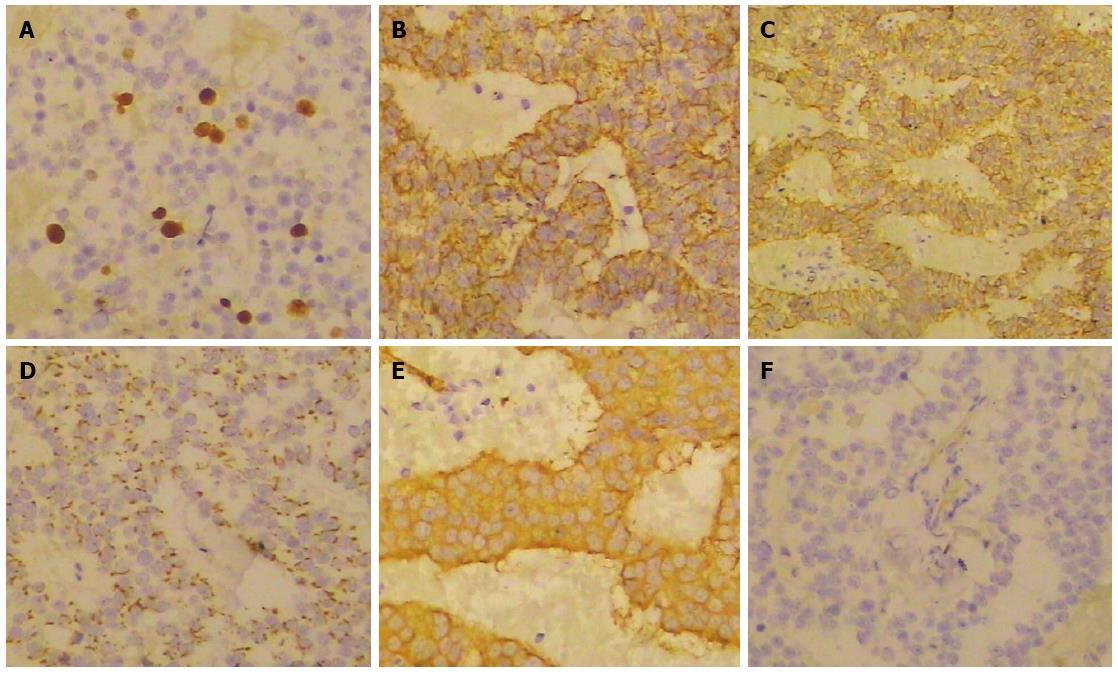
Pathologic evaluation of the resected tissue revealed a well-differentiated tumor with a distinct border surrounding the exocrine pancreatic tissue (Figure 3). Immunohistochemical evaluation showed that the cells were positive for tumor markers and insulin (Figure 4). Taken together, the findings confirmed the diagnosis of ectopic insulinoma, Heinrich’s classification type I.
Glucose blood levels were recorded every 15 min during surgery without dextrose infusion (Table 1). Normoglycemia was achieved promptly after tumor removal. The patient was discharged on postoperative day 7, and a routine follow-up showed no recurrence of hypoglycemic symptoms.
| Time | Glucose blood level (mmol/L) |
| Perioperative | |
| Beginning of procedure | 3.2 |
| Tumor removal | 5.6 |
| 15 min after removal | 5.8 |
| 30 min after removal | 6.6 |
| 45 min after removal | 6.8 |
| End of procedure | 6.9 |
| Postoperative | |
| Day 1 | 5.6 |
| Day 2 | 5.6 |
| Day 3 | 5.8 |
| Day 4 | 6.2 |
| Day 5 | 7.5 |
Insulinoma presents with various clinical manifestations, often with symptoms of hypoglycemia. These tumors are difficult to detect due to their small size. In a study of 114 articles encompassing 6222 cases of insulinoma, the vast majority (84%) were < 20 mm in diameter[13]. Almost all of these tumors were found in the pancreas parenchyma (43.3% head and uncinate, 25.3% body, and 30.9% tail), and < 1% were ectopic (extrapancreatic). Ectopic insulinomas with symptoms of hypoglycemia are extremely rare and can occur in the duodenal wall, ileum, jejunum, gastric wall, hilus of the spleen, gastrosplenic ligament, ligament of Treitz, lung, cervix, and ovary[14,15].
Symptoms of insulinomas include digestive bleeding, jaundice, and abdominal pain[16,17]. The Whipple triad, which includes documented hypoglycemia, neuroglycopenic symptoms, and rapid relief of symptoms with the administration of glucose, is the diagnostic hallmark of an insulinoma. Although the 72-h fasting test has been the standard criterion for diagnosing insulinomas, recent data have verified that the diagnosis can be achieved in about 95.7% of cases undergoing a supervised fasting of 48 h[18].
Although insulinomas are generally observed by abdominal ultrasonography, CT, and magnetic resonance imaging, these methods cannot easily detect ectopic insulinomas, particularly those < 10 mm. Rather, more sensitive methods should be employed for more accurate detection, such as digital subtraction angiography, which uses the characteristic bloodstream distribution. Other methods, including endoscopic ultrasonography, transhepatic portal venous sampling, 18fluorodopa PET/CT scanning, and arterial stimulation/venous sampling, have been widely used to localize insulinoma in clinical practice[19]. Fortunately for the patient in the present case,a combination of ultrasonography and contrast-enhanced CT detected the mass.
The treatment of choice for patients with insulinoma is surgery, including enucleation, segmental pancreatectomy, pancreatoduodenectomy, and distal pancreatectomy preserving the spleen[20]. Laparoscopic resection for insulinoma has now been widely accepted, which can be used for resection of small, benign, solitary, and superficial tumors[21,22], including ectopic insulinomas. This method reduces operation time, blood loss, and morbidity, and involves a shorter hospital stay and faster recovery period for the patient. In our case, ectopic insulinoma was diagnosed based on the typical symptoms and imaging examinations, and was completely removed. However, for patients whose insulinomas have been missed during surgery and for those who refuse or are not candidates for surgery (including malignant insulinoma with metastasis), alternative medical treatment is needed[23].
Ectopic insulinoma is a very rare and dormant disease that is difficult to diagnose and locate, particularly very small tumors or atypical cases. This case report highlights that a diagnosis of ectopic insulinoma for hypoglycemia of unknown cause should be considered, even in cases with negative findings from the pancreas, and specific or targeted examinations for insulinoma need to be followed. In addition, laparoscopic resection is a feasible and effective method for treatment of ectopic insulinomas.
A 79-year-old woman with a 9-mo history of recurrent hypoglycemia that resolved after intake of glucose or dextrose.
Hypoglycemia.
Drug-induced hypoglycemia; hypoglycemia caused by adrenal or hepatic diseases;insulinoma; hypocortisolism.
Serum glucose level: 2.4 mmol/L; insulin: 35.37 μU/mL; C-peptide: 2.54 ng/mL; tumor markers were within normal limits.
Regular transabdominal ultrasonography showed negative findings in the pancreas. An abdominal computed tomography/positron emission tomography scan did not reveal a pancreatic tumor, but showed a 2.5 × 1.0 cm solid polyp localized in the retroperitoneum under and left of the hepatoduodenal ligament with no fluorodeoxyglucose activity.
Immunohistochemical results showed that tumor cells were immunopositive for Ki67, insulin, CD56, chromogranin, and synaptophysin, and negative for serotonin, which supported a diagnosis of insulinoma.
Laparoscopic resection of the tumor was successfully performed by harmonic scalpel.
Very few cases of ectopic insulinoma have been reported in the literature. The clinical characteristics of ectopic insulinomas are sometimes atypical and localization is difficult.
This report showed a very rare and dormant disease that can be confused with non-insulinoma-induced hypoglycemia. Insulinomas are difficult to diagnose and locate, particularly for atypical or very small cases. The diagnosis of ectopic insulinoma for hypoglycemia of unknown cause should be considered even when there are negative findings of the pancreas, and specific or targeted examinations for insulinomas are needed.
The authors have described a case of ectopic insulinoma, which is a very rare, dormant disease that is difficult to diagnose and locate. The article highlights the importance of differential diagnosis with hypoglycemia caused by drugs and other diseases, and the need for correlative laboratory and imaging examinations. The report suggests that laparoscopic resection is a feasible and effective treatment approach.
P- Reviewer: Buanes TA, Gong JP, Pavlidis TE, Scheidbach H S- Editor: Qi Y L- Editor: Cant MR E- Editor: Liu XM
| 1. | Murad MH, Coto-Yglesias F, Wang AT, Sheidaee N, Mullan RJ, Elamin MB, Erwin PJ, Montori VM. Clinical review: Drug-induced hypoglycemia: a systematic review. J Clin Endocrinol Metab. 2009;94:741-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 120] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 2. | Guettier JM, Gorden P. Insulin secretion and insulin-producing tumors. Expert Rev Endocrinol Metab. 2010;5:217-227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Breuer HW, Ptak P. [Hypoglycemia - frequency, causes, induced costs]. Dtsch Med Wochenschr. 2012;137:988-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Martens P, Tits J. Approach to the patient with spontaneous hypoglycemia. Eur J Intern Med. 2014;25:415-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Brown LM, Corrado MM, van der Ende RM, Derks TG, Chen MA, Siegel S, Hoyt K, Correia CE, Lumpkin C, Flanagan TB. Evaluation of glycogen storage disease as a cause of ketotic hypoglycemia in children. J Inherit Metab Dis. 2014;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 53] [Article Influence: 5.3] [Reference Citation Analysis (2)] |
| 6. | Soutelo J, Saban M, Borghi Torzillo F, Lutfi R, Leal Reyna M. [Adrenal carcinoma induced hypoglycemia]. Medicina (B Aires). 2013;73:339-342. [PubMed] |
| 7. | Dutta P, Aggarwal A, Gogate Y, Nahar U, Shah VN, Singla M, Khandelwal N, Bhansali A. Non-islet cell tumor-induced hypoglycemia: a report of five cases and brief review of the literature. Endocrinol Diabetes Metab Case Rep. 2013;2013:130046. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Dean K, Hsieh J, Morosky C, Hoffman J. Gastrointestinal stromal tumor of the pelvic soft tissue presenting with symptomatic hypoglycemia: A case report and brief review of current literature of non-islet cell tumor-induced hypoglycemia. Gynecol Oncol Case Rep. 2012;2:87-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Mir A, Raza S. Congenital ACTH deficiency as a cause of hypoglycemia in a newborn infant. Clin Pediatr (Phila). 2011;50:1150-1152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Savas-Erdeve S, Yılmaz Agladioglu S, Onder A, Peltek Kendirci HN, Bas VN, Sagsak E, Cetinkaya S, Aycan Z. An uncommon cause of hypoglycemia: insulin autoimmune syndrome. Horm Res Paediatr. 2014;82:278-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Elhomsy GC, Eranki V, Albert SG, Fesler MJ, Parker SM, Michael AG, Griffing GT. „Hyper-warburgism,“ a cause of asymptomatic hypoglycemia with lactic acidosis in a patient with non-Hodgkin‘s lymphoma. J Clin Endocrinol Metab. 2012;97:4311-4316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Aktan AH, Ozcelik A, Cure E, Cure MC, Yuce S. Profound hypoglycemia-ınduced by vaccinium corymbosum juice and laurocerasus fruit. Indian J Pharmacol. 2014;46:446-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Mehrabi A, Fischer L, Hafezi M, Dirlewanger A, Grenacher L, Diener MK, Fonouni H, Golriz M, Garoussi C, Fard N. A systematic review of localization, surgical treatment options, and outcome of insulinoma. Pancreas. 2014;43:675-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 183] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 14. | La Rosa S, Pariani D, Calandra C, Marando A, Sessa F, Cortese F, Capella C. Ectopic duodenal insulinoma: a very rare and challenging tumor type. Description of a case and review of the literature. Endocr Pathol. 2013;24:213-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Stanciu IN, Pitale S, Prinz RA, Jakate S, Webb G, Steiner D, Braithwaite S, Gordon D, Emanuele MA. Insulinoma presenting with hyperandrogenism: a case report and a literature review. J Intern Med. 2003;253:484-489. [PubMed] |
| 16. | Watanabe W, Kurumada T, Shirai T, Tsutsumi Y. Aberrant insulinoma of the duodenal bulb. Pathol Int. 1995;45:895-900. [PubMed] |
| 17. | Tolentino LF, Lee H, Maung T, Stabile BE, Li K, French SW. Islet cell tumor arising from a heterotopic pancreas in the duodenal wall with ulceration. Exp Mol Pathol. 2004;76:51-56. [PubMed] |
| 18. | Quinkler M, Strelow F, Pirlich M, Rohde W, Biering H, Lochs H, Gerl H, Strasburger CJ, Ventz M. Assessment of suspected insulinoma by 48-hour fasting test: a retrospective monocentric study of 23 cases. Horm Metab Res. 2007;39:507-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Peranteau WH, Palladino AA, Bhatti TR, Becker SA, States LJ, Stanley CA, Adzick NS. The surgical management of insulinomas in children. J Pediatr Surg. 2013;48:2517-2524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | Guo Q, Wu Y. Surgical treatment of pancreatic islet cell tumor: report of 44 cases. Hepatogastroenterology. 2013;60:2099-2102. [PubMed] |
| 21. | Sciuto A, Abete R, Reggio S, Pirozzi F, Settembre A, Corcione F. Laparoscopic spleen-preserving distal pancreatectomy for insulinoma: experience of a single center. Int J Surg. 2014;12 Suppl 1:S152-S155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Ueda J, Nakamura Y, Aimoto T, Hiroi M, Cho K, Yamahatsu K, Kawamoto M, Uchida E. Laparoscopic distal pancreatectomy preserving spleen and splenic vessels for pancreatic insulinoma. J Nippon Med Sch. 2010;77:175-180. [PubMed] |