Published online Apr 14, 2015. doi: 10.3748/wjg.v21.i14.4408
Peer-review started: October 27, 2014
First decision: November 26, 2014
Revised: December 10, 2014
Accepted: January 8, 2015
Article in press: January 8, 2015
Published online: April 14, 2015
Processing time: 175 Days and 10.3 Hours
Breast cancer can metastasize to other organs following initial treatment. Bones, liver, and the lung are the most common sites of breast cancer metastases. The digestive tract, on the other hand, is rarely involved. The incidence of mesorectal metastasis (a special category of rectal metastases) from breast cancer has not been described before. The case reported herein concerns a 68-year-old woman who underwent mastectomy. A pelvic mass with no symptoms was subsequently identified by computed tomography in the patient. We ultimately confirmed that this mass was a metastasis from breast cancer located in the mesorectum using surgical exploration and pathology results.
Core tip: Breast cancer is the most frequent tumor in women and can metastasize to other organs following operation. The incidence of mesorectal metastasis, a special category of rectal metastases, from breast cancer has not been described before. In contrast to the rectal metastasis described in previous case reports, the lack of visible clinical symptoms makes mesorectal metastasis more difficult to be discovered and diagnosed. The radiographic and pathologic characteristics of mesorectal metastasis from breast cancer shown in this paper have not been described before.
- Citation: Xue F, Liu ZL, Zhang Q, Kong XN, Liu WZ. Mesorectum localization as a special kind of rectal metastasis from breast cancer. World J Gastroenterol 2015; 21(14): 4408-4412
- URL: https://www.wjgnet.com/1007-9327/full/v21/i14/4408.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i14.4408
Breast cancer is the most frequently occurring tumor in women and can metastasize to other organs following the initial treatment[1]. A study analyzing 11676 pT1-4N0-2M0 breast cancer patients who underwent surgical resection between 1985 and 2009 showed that the total number of distant metastasis cases was 1349 (11.6%)[2]. Lymph node, bone, lung, and liver metastasis are considered to be the most frequent sites for breast cancer metastasis, but more rectal metastasis cases have also been recently reported. Metastatic involvement of the rectum is generally secondary to the lobular histological subtype of breast cancer[3], and usually some symptoms are observed, including obstruction, bleeding, and abdominal pain. Here we present the case of a 68-year-old woman with metastatic ductal breast cancer in the mesorectum with no clinical manifestation 7 years after diagnosis and surgery.
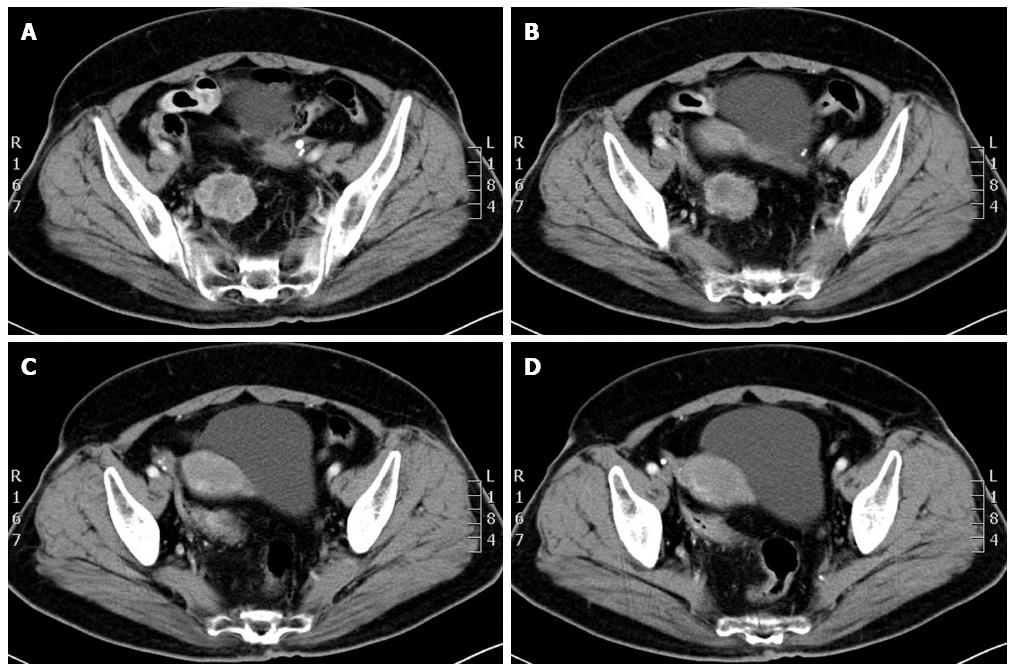
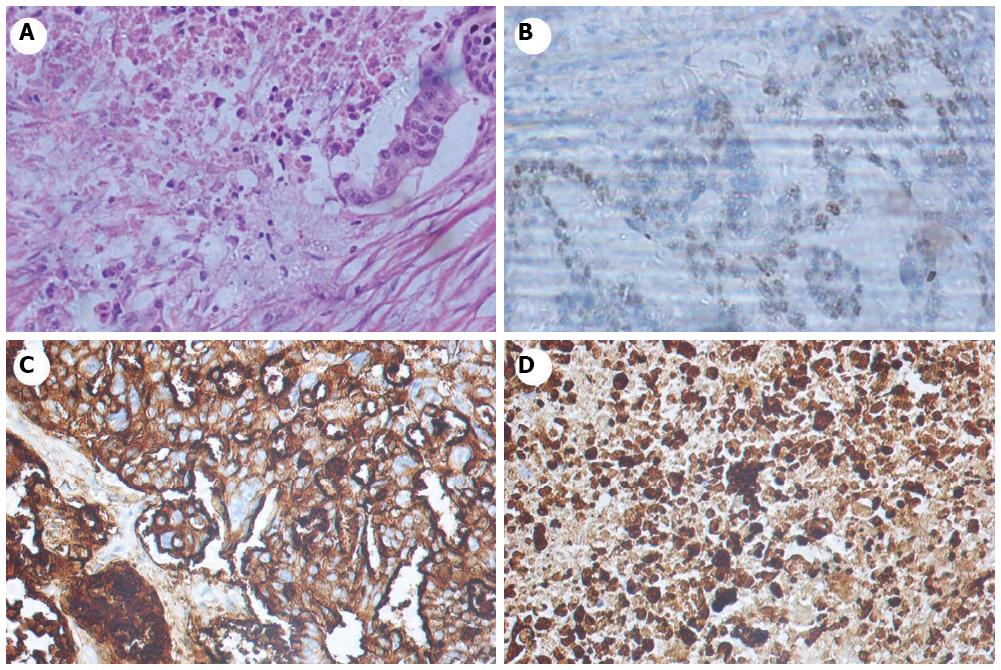
A 68-year-old, post-menopausal woman underwent modified radical mastectomy of the right breast in June 2006 due to breast carcinoma with a 10-year-history of type 2 diabetes. No abnormalities were discovered by chest imaging, liver function tests, and routine blood examination. A post-operative pathologic diagnosis confirmed the presence of invasive ductal carcinoma (pT2, N0/13, and M0), and immunohistochemical stains were positive (++) for the estrogen receptor and negative for the progesterone receptor and HER-2. The patient only received one cycle of chemotherapy, which was implemented as the CMF regimen. There were no abnormalities during follow-up until a 3.2 cm × 4.2 cm malignant lesion was found in the pelvic cavity with heterogeneous density by enhanced CT scan in December 2013 (Figure 1). The patient also had a highly elevated CA-125 level (519.5 U/mL). The patient had no complaints and the colonoscopy result was negative. Therefore, a laparoscopy was performed, and a mass was located in the mesorectum as a result. No other metastasis was identified. We therefore decided to perform a resection of the mass, the diseased mesorectum, and the portion of the rectum to which it belonged. Immunohistochemical analysis revealed metastatic cancer nodules from the breast (ER 30%+, PR-, c-erbB2+, TOPO II 35%+, Ki-67 index 75%, CK7+, CK20-, Villin-, CDX2-, CEA-, GCDFP-15+/-, CA-125+, WT-1+) (Figure 2)
The gastrointestinal (GI) tract is an uncommon metastatic site for breast carcinoma. In a study of 12001 cases of breast carcinoma with metastatic disease, only 73 (approximately 0.6%) had metastasis to the GI tract, while 24 had colorectal metastasis[4]. To our knowledge, there have been at least 15 reports on rectal metastasis of breast carcinoma, but none of these cases mentioned mesorectal metastasis. Therefore, we presume that mesorectal metastasis is a special type of rectal metastasis. The metastatic pathway between these two types may be via the blood, and is presumed to start by the dislodgement and intravasation of tumor cells into the axillary vein (e.g., by surgical manipulation)[5]. It has been suggested that the vertebral plexus of veins, also known as Batson’s plexus, may also serve as a route for metastasis. Batson’s plexus is a venous plexus stretching along the vertebrae from the skull base to the sacrum[6]. These vessels may allow for the transfer of cancer emboli to pelvic organs through the posterior intercostal arteries[7]. The pathological result of primary breast cancer in this case was the infiltration of the ductal BC. Rectal metastases are judged to occur more often in patients with invasive lobular BC[4]. Microscopically, we observed that the tumor consisted of single-file stands of infiltrating tumor cells with the presence of signet-ring cells, the same as has been described for rectal metastasis previously[8]. Moreover, we also found very similar immunohistochemical characteristics to rectal metastasis. Metastatic breast tumor cells in the rectum have been reported to be positive for ER, PR, CK7, and GCDFP-15 and negative for CK20, CEA, and CDX2[9]. In our case, the tumor cell was positive for ER, CK7, GCDFP-15, and CA-125 and negative for CK20, CEA, CDX2, and PR.
CA-125 is commonly known as a tumor marker for ovarian carcinoma, but there has been limited data and less emphasis on metastatic breast carcinoma. Interestingly, the patient in our case had an extremely high CA-125 level. It is now believed that CA-125 can be expressed not only by the mesothelial cells of coelomic-derived tissues, such as the pleura, peritoneum, and pericardium, but also by the breast ducts and bronchiolar epithelium. A retrospective study found that CA-125 had a relatively high rate of detection (65%) in patients with multiple metastases from breast cancer[10]. Furthermore, two analyses based on 26 and 33 patients, respectively, suggested that elevations of CA-125 in metastatic breast cancer implied pleural involvement[11,12]. The data from a retrospective review (51 patients) and a prospective study (40 patients) illustrated that the CA-125 level had parallel responses to the status of post-operative breast cancer[13,14]. Despite these studies, it is unclear whether CA-125 is useful for monitoring the course of disease. Further research and the analysis of larger patient cohorts are needed to determine the utility of CA-125.
Due to the rarity of cases, the management of metastatic breast cancer in GI organs is still controversial. For a patient with serious complications such as obstruction, hematemesis, or perforation, surgery is certainly the first choice, although additional survival data for other treatments are still required. A retrospective review found that systemic chemotherapy or hormonal therapy has a positive effect on survival (P = 0.003)[4]. Moreover, Tang et al[15] reported that two cases with intestinal obstruction attributed to metastatic lobular BC were cured with hormonal therapy (fulvestrant). Additionally, combined treatment of surgery and chemotherapy on a patient with isolated GI involved caused remission[16]. For our patient, with consideration to the immunohistochemical analysis (ER 30%+), we chose a strategy of surgery combined with hormonal therapy.
Mesorectal metastases from breast carcinoma are rare and there have been no prior reports on this disease. Therefore, it has been hard to differentiate between primary GI tumors and pelvic malignancies until the immunohistochemical profile has been determined. Awareness of this special kind of rectal metastasis is helpful for increasing diagnostic accuracy. Additional fundamental and clinical research concerning mesorectal metastases is needed to improve treatment.
A 68-year-old, post-menopausal woman underwent modified radical mastectomy of the right breast in June 2006 due to breast carcinoma with a 10-year-history of type 2 diabetes.
No physical sign was displayed other than that right breast had been excised.
Primary tumors of pelvic organs, uterine, or ovarian metastasis from breast cancer, and other benign or malignant pelvic masses.
CA-125: 519.5 U/mL, with other laboratory values being within normal limits.
A 3.2 cm × 4.2 cm malignant lesion was found in the pelvic cavity with a heterogeneous density by enhanced computed tomography scan.
Immunohistochemical analysis revealed metastatic cancer nodules from breast cancer (ER 30%+, PR-, c-erbB2+, TOPO II 35%+, Ki-67 index 75%, CK7+, CK20-, Villin-, CDX2-, CEA-, GCDFP-15+/-, CA-125+, WT-1+).
The patient received a curative resection combined with hormonal therapy.
The incidence of mesorectal metastasis from breast cancer has not been described before to our knowledge, while 15 reports on rectal breast cancer metastasis could be found in the literature.
CMF regimen is a conventional chemotherapy which is a cyclical application of cyclophosphamide, methotrexate, and fluorouracil. The medication dosages were adjusted based on individual patient characteristics.
We know that mesorectal metastasis is a possibility once a pelvic mass has been found on a patient with a history of breast cancer.
The article highlights the clinical characteristics of mesorectal metastasis from breast cancer and provides insights into the etiology, diagnosis experiences, and therapy through the relevant literature.
P- Reviewer: Gehmert S, Sidiropoulou Z S- Editor: Qi Y L- Editor: Rutherford A E- Editor: Ma S
| 1. | Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61:212-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3032] [Cited by in RCA: 3123] [Article Influence: 223.1] [Reference Citation Analysis (0)] |
| 2. | Makita M, Sakai T, Ogiya A, Kitagawa D, Morizono H, Miyagi Y, Iijima K, Iwase T. Optimal surveillance for postoperative metastasis in breast cancer patients. Breast Cancer. 2014;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Nazareno J, Taves D, Preiksaitis HG. Metastatic breast cancer to the gastrointestinal tract: a case series and review of the literature. World J Gastroenterol. 2006;12:6219-6224. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 68] [Cited by in RCA: 77] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | McLemore EC, Pockaj BA, Reynolds C, Gray RJ, Hernandez JL, Grant CS, Donohue JH. Breast cancer: presentation and intervention in women with gastrointestinal metastasis and carcinomatosis. Ann Surg Oncol. 2005;12:886-894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 192] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 5. | Bockhorn M, Jain RK, Munn LL. Active versus passive mechanisms in metastasis: do cancer cells crawl into vessels, or are they pushed? Lancet Oncol. 2007;8:444-448. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 192] [Cited by in RCA: 176] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 6. | Batson OV. The function of the vertebral veins and their role in the spread of metastases. Ann Surg. 1940;112:138-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1252] [Cited by in RCA: 1149] [Article Influence: 63.8] [Reference Citation Analysis (0)] |
| 7. | Efthimiadis C, Kosmidis C, Fotiadis P, Anthimidis G, Vasiliadou K, Mekras A, Ioannidou G, Basdanis G. Breast cancer metastatic to the rectum: a case report. Tech Coloproctol. 2011;15 Suppl 1:S91-S93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Saranovic D, Kovac JD, Knezevic S, Susnjar S, Stefanovic AD, Saranovic DS, Artiko V, Obradovic V, Masulovic D, Micev M. Invasive lobular breast cancer presenting an unusual metastatic pattern in the form of peritoneal and rectal metastases: a case report. J Breast Cancer. 2011;14:247-250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | López Deogracias M, Flores Jaime L, Arias-Camisón I, Zamacola I, Murillo Guibert J, Suescun García R, Querejeta Usabiaga J, Martínez García F. Rectal metastasis from lobular breast carcinoma 15 years after primary diagnosis. Clin Transl Oncol. 2010;12:150-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Yerushalmi R, Tyldesley S, Kennecke H, Speers C, Woods R, Knight B, Gelmon KA. Tumor markers in metastatic breast cancer subtypes: frequency of elevation and correlation with outcome. Ann Oncol. 2012;23:338-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 11. | Jäger W, Kissing A, Cilaci S, Melsheimer R, Lang N. Is an increase in CA 125 in breast cancer patients an indicator of pleural metastases? Br J Cancer. 1994;70:493-495. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Norum LF, Erikstein B, Nustad K. Elevated CA125 in breast cancer--A sign of advanced disease. Tumour Biol. 2001;22:223-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 45] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Jensen JL, Maclean GD, Suresh MR, Almeida A, Jette D, Lloyd S, Bodnar D, Krantz M, Longenecker BM. Possible utility of serum determinations of CA 125 and CA 27.29 in breast cancer management. Int J Biol Markers. 1991;6:1-6. [PubMed] |
| 14. | Perey L, Hayes DF, Tondini C, van Melle G, Bauer J, Lemarchand T, Reymond M, Mach JP, Leyvraz S. Elevated CA125 levels in patients with metastatic breast carcinoma. Br J Cancer. 1990;62:668-670. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Tang JY, Rampaul RS, Cheung KL. The use of fulvestrant, a parenteral endocrine agent, in intestinal obstruction due to metastatic lobular breast carcinoma. World J Surg Oncol. 2008;6:128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Eljabu W, Finch G, Nottingham J, Vaingankar N. Metastatic deposits of breast lobular carcinoma to small bowel and rectum. Int J Breast Cancer. 2011;2011:413949. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |