Published online Apr 7, 2015. doi: 10.3748/wjg.v21.i13.3921
Peer-review started: June 30, 2014
First decision: July 21, 2014
Revised: September 11, 2014
Accepted: October 20, 2014
Article in press: October 21, 2014
Published online: April 7, 2015
Processing time: 281 Days and 19 Hours
AIM: To study the clinical features and computed tomography (CT) findings of appendiceal diverticulitis vs acute appendicitis.
METHODS: We retrospectively reviewed the records of 451 patients who had undergone appendectomy in our institution from January 2007 to September 2012. Patient demographics, clinical features, pathological findings, and surgical outcomes were analyzed. We also compared preoperative CT images of 25 patients with appendiceal diverticulitis with those of 25 patients with acute appendicitis.
RESULTS: Among 451 patients, 44 (9.7%) were diagnosed to have appendiceal diverticulitis and 398 (86.9%) to have acute appendicitis. Patients with appendiceal diverticulitis were older (59 vs 37 years, P < 0.001) and had a longer duration of the illness (4.0 d vs 1.0 d, P < 0.001). Perforation rates in patients with appendiceal diverticulitis were higher (68% vs 27%, P < 0.001). The appendix could be visualized in only 13 patients (52%) among the appendiceal diverticulitis cases, but in all acute appendicitis cases. CT findings suggestive of appendiceal diverticulitis included the absence of fluid collection in the appendix (84% vs 12%, P < 0.001), absence of appendicolith (92% vs 52%, P = 0.005), and formation of abscess (68% vs 16%, P < 0.001). Appendiceal diverticula were identified in 6 patients (24%).
CONCLUSION: Among patients who had undergone appendectomy, 9.7% had appendiceal diverticulitis. Patients with appendiceal diverticulitis had different clinical features and CT findings from patients with acute appendicitis.
Core tip: To study the clinical features and computed tomography (CT) findings of appendiceal diverticulitis, we retrospectively reviewed 451 patients who had undergone appendectomy in our institution. Among 451 patients, 44 (9.7%) were diagnosed with appendiceal diverticulitis. Patients with appendiceal diverticulitis were older and had a longer duration of illness. Perforation rates in patients with appendiceal diverticulitis were higher. CT findings suggestive of appendiceal diverticulitis included the absence of a fluid collection in the appendix, absence of an appendicolith (92% vs 52%, P = 0.004), and abscess formation. These findings make it possible to clinically differentiate appendiceal diverticulitis from acute appendicitis.
-
Citation: Ito D, Miki K, Seiichiro S, Hata S, Kobayashi K, Teruya M, Kaminishi M. Clinical and computed tomography findings of appendiceal diverticulitis
vs acute appendicitis. World J Gastroenterol 2015; 21(13): 3921-3927 - URL: https://www.wjgnet.com/1007-9327/full/v21/i13/3921.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i13.3921
Diverticula are small, bulging pouches within the bowel wall that typically form within the large intestine, including the appendix. Appendiceal diverticula are relatively rare[1]. Appendiceal diverticulitis is the result of inflammation of the appendiceal diverticulum.
This disease was first described by Kelynack[2] in 1893. The incidence of diverticulitis of the appendix in Europe[3] and the United States[4] is 0.2% and 1.7%, respectively. Appendiceal diverticulitis is considered a relatively rare disease, and has most often been reported in case reports[5].
Acute appendicitis occurs when the appendiceal lumen is obstructed, leading to fluid accumulation, luminal distention, inflammation, and ultimately perforation. Distension of the appendiceal lumen causes dull, periumbilical abdominal pain[6].
Since right lower quadrant pain is the main clinical symptom of both acute appendicitis and appendiceal diverticulitis, appendiceal diverticulitis has been commonly dismissed as a variant of acute appendicitis. Therefore, preoperative diagnosis has been rarely made, and pathologists may fail to differentiate between acute appendicitis and appendiceal diverticulitis.
Several studies have investigated the preoperative diagnosis of appendiceal diverticulitis by identifying inflammation in the appendiceal diverticula using ultrasonography[7] or CT[8]. Recently, two retrospective studies were reported from Japan[9] and Korea[10]. These studies considered appendiceal diverticulitis as a separate clinical entity apart from typical acute appendicitis. We retrospectively reviewed the pathological specimens and clinical charts of patients undergoing appendectomy with a preoperative diagnosis of acute appendicitis. We carefully examined the resected specimens in order to distinguish appendiceal diverticulitis from acute appendicitis.
The aim of this study was to clarify the incidence of appendiceal diverticulitis among patients who underwent appendectomy and to evaluate the clinical features and CT findings of appendiceal diverticulitis.
In this study, we included 451 patients who had undergone appendectomy in our institution from January 2007 to September 2012. We retrospectively reviewed clinical records and re-examined the histopathological specimens to analyze the patients’ pathological findings, clinical characteristics, laboratory findings, operative findings, operative procedures, and postoperative course.
In addition to our review of the pathology reports, the pathologist initially prepared and thoroughly examined the specimens microscopically to detect diverticula. Appendiceal diverticulitis was diagnosed as inflammation of one of the diverticula, with no or slight inflammation of the appendiceal wall[11].
In order to assess the feasibility of making a preoperative CT diagnosis, we compared preoperative CT findings of 25 patients pathologically diagnosed with appendiceal diverticulitis with those of 25 randomly selected patients diagnosed with acute appendicitis. For the retrospective data analysis, patient identification was blocked, and a research identification number was given to each patient.
Statistical analysis was performed for the comparison of cases of appendiceal diverticulitis to acute appendicitis using the Wilcoxon signed-rank test and Fisher’s exact test. All statistical analyses were performed with JMP 5.0.1J, and all P values that were two-sided at a value of < 0.05 were considered statistically significant.
Among 451 patients who underwent appendectomy, 44 (9.7%) were pathologically diagnosed to have appendiceal diverticulitis, while 392 (86.9%), were confirmed to have acute appendicitis. No patients were diagnosed with appendiceal diverticulitis preoperatively. The preoperative clinical characteristics of both appendiceal diverticulitis and acute appendicitis are summarized in Table 1. Operative findings, operative procedures, and postoperative courses of the patients are summarized in Table 2.
| Variable | Appendiceal diverticulitis (n = 44) | Acute appendicitis (n = 398) | |||
| Median | Range | Median | Range | P value | |
| Age (yr) | 59 | 17-89 | 35 | 7-87 | < 0.0012 |
| Duration of symptoms (d) | 4.0 | 10-30 | 1.0 | 0-20 | < 0.0012 |
| Preoperative CRP (mg/dL) | 13.6 | 0.5-29.7 | 6.8 | 0.1-37.2 | < 0.0012 |
| Preoperative WBC (/μL) | 13100 | 3580-20000 | 14000 | 2071-30100 | 0.022 |
| Number | Rate | Number | Rate | ||
| Sex (male/total) | 32 | 72% | 223 | 56% | 0.061 |
| Comorbidity (yes/total) | 26 | 60% | 278 | 70% | 0.201 |
| Variable | Appendiceal diverticulitis (n = 44) | Acute appendicitis (n =398) | |||
| Median | Range | Median | Range | P value | |
| Operating times (min) | 77 | 33-165 | 55 | 15-172 | < 0.0012 |
| Inoperative blood loss (mL) | 60 | 10-970 | 20 | 10-650 | < 0.0012 |
| Postoperative hospital stay (d) | 8 | 4-38 | 5 | 2-48 | < 0.0012 |
| Number | Rate | Number | Rate | ||
| Ileocecal resection (yes/total) | 6 | 13% | 10 | 2% | 0.0081 |
| Skin incision (pararectal incision/total) | 35 | 79% | 143 | 36% | 0.121 |
| Formation of localized abscess (yes/total) | 26 | 60% | 60 | 15% | < 0.0011 |
| Perforation (yes/total) | 32 | 72% | 123 | 31% | < 0.0011 |
| Postoperative wound infection (yes/total) | 7 | 15% | 32 | 8% | 0.121 |
| Postoperative ileus (yes/total) | 3 | 8% | 16 | 4% | 0.301 |
Patients with appendiceal diverticulitis were older than those with acute appendicitis (59 vs 37 years, P < 0.001). Patients with appendiceal diverticulitis had lower white blood cell (WBC) count (13100 vs 14000 WBC/μL, P = 0.02) and higher C-reactive protein (CRP) level than patients with acute appendicitis (13.6 vs 6.8 mg/dL, P < 0.001). The median duration of preoperative symptoms (right lower quadrant abdominal pain and/or abdominal distension) was 4.0 d in the diverticulitis group and 1.0 d in the appendicitis group (P < 0.001). There was no significant difference in the ratio of comorbidities between the two groups.
All patients were treated with open appendectomy. The rate of perforation was significantly higher in the diverticulitis group than in the appendicitis group. Thirty-two patients (72%) in the diverticulitis group and 123 patients (31%) in the appendicitis group had perforated appendices. The number of patients with localized abscess was significantly higher in the diverticulitis group than the appendicitis group (60% vs 15%, P < 0.001). The median operative time was longer in the diverticulitis group (77 min vs 55 min, P < 0.001), and the average amount of operative blood loss was higher in the diverticulitis group than the appendicitis group (60 mL vs 20 mL, P < 0.001).
In the diverticulitis group, pathologic findings showed that all diverticula were of the false type, lacking a proper muscle layer. Multiple diverticula were found in 55% patients.
The differences in clinical characteristics between the patients with perforated appendiceal diverticulitis and perforated acute appendicitis are summarized in Table 3. In patients with perforations, mean blood loss and the ratio of localized abscess were significantly higher in the diverticulitis group than in the appendicitis group. However, the mean duration of postoperative hospital stay, postoperative morbidity rates, and mortality rates were not significantly different between the two groups.
| Variable | Perforated appendiceal diverticulitis (n = 30) | Perforated acute appendicitis (n = 111) | |||
| Median | Range | Median | Range | P value | |
| Operating times (min) | 65 | 45-165 | 67 | 25-172 | 0.982 |
| Inoperative blood loss (mL) | 60 | 10-970 | 40 | 10-650 | 0.052 |
| Postoperative hospital stay (d) | 9 | 5-38 | 9 | 3-48 | 0.772 |
| Number | Rate | Number | Rate | ||
| Ileocecal resection (yes/total) | 4 | 13% | 7 | 6% | 0.201 |
| Skin incision (pararectal incision/total) | 27 | 89% | 82 | 74% | 0.111 |
| Formation of localized abscess (yes/total) | 22 | 72% | 39 | 35% | < 0.0011 |
| Postoperative wound infection (yes/total) | 5 | 17% | 19 | 17% | 0.961 |
| Postoperative ileus (yes/total) | 3 | 11% | 12 | 11% | 0.921 |
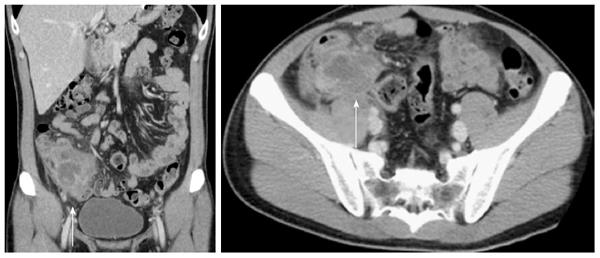
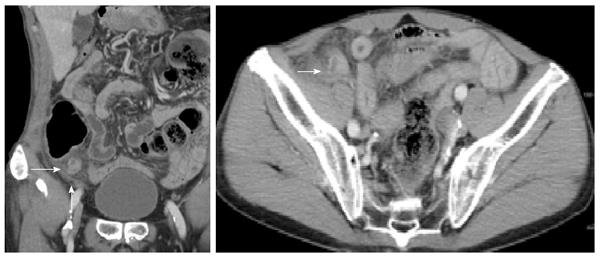
The preoperative CT of patients with acute appendicitis showed several typical findings such as enlarged appendixes, appendiceal wall thickening and enhancement, and periappendiceal fat stranding (Figures 1 and 2). On the other hand, in the appendiceal diverticulitis group, the appendixes could not be clearly visualized on preoperative CT scans. In some cases, it was difficult to identify the appendix, even though a large abscess cavity was visible (Figure 3).
CT findings of appendiceal diverticulitis and acute appendicitis are described in Table 4. The appendix was detected in only 13 of 25 scans (52%) in the appendiceal diverticulitis group but was detected in all scans (100%) in the acute appendicitis group. Only 16% of the scans in the appendiceal diverticulitis group showed fluid in the appendix lumen compared to 88% of the scans in the acute appendicitis group. An appendicolith was visualized in 5 of 25 scans (20%) in the appendiceal diverticulitis group and 13 of 25 scans (52%) in the acute appendicitis group. Localized abscess was visualized in 17 scans (68%) with appendiceal diverticulitis, whereas an abscess was identified in only 4 (16%) scans of patients with acute appendicitis. The number of scans showing appendiceal diameter, appendiceal wall thickening, periappendiceal fat stranding, and appendiceal or abscess wall enhancements were not significantly different between the two groups. Appendiceal diverticula were identified in 6 (24%) of the 25 scans in the appendiceal diverticulitis group.
| Variable | Appendiceal diverticulitis (n = 25) | Acute appendicitis (n = 25) | |||
| Median | Range | Median | Range | P value | |
| Appendiceal diameter (mm) | 13.2 | 4.3-23.4 | 12.4 | 8.1-18.9 | 0.252 |
| Appendiceal wall thickening (mm) | 3.1 | 1.6-5.3 | 3.7 | 2.0-6.2 | 0.772 |
| Number | Rate | Number | Rate | ||
| Visualized appendix (yes/total) | 13 | 52% | 25 | 100% | < 0.0011 |
| Fluid collection in the appendix lumen (yes/total) | 4 | 16% | 22 | 88% | < 0.0011 |
| Formation of localized abscess (yes/total) | 17 | 68% | 4 | 16% | < 0.0011 |
| Periappendiceal fat stranding(yes/total) | 16 | 66% | 11 | 44% | 0.171 |
| Appendiceal or abscess wall enhancement (yes /total) | 10 | 58% | 9 | 41% | 0.271 |
| Apendicolith (yes/total) | 2 | 8% | 12 | 48% | 0.00471 |
| Visualized appendiceal diverticulum (yes /total) | 6 | 24% | 0 | 0% | 0.0251 |
The three major findings of this study are as follows: First, among patients who underwent appendectomy, the incidence of appendiceal diverticulitis was 9.7%, which is much higher than that previously reported. Second, our results revealed several clinical characteristics that may assist in the diagnosis of appendiceal diverticulitis, such as older age, longer duration of symptoms, higher rate of perforation, and higher incidence of localized abscess. These findings are consistent with previous reports. Third, several CT findings suggestive of appendiceal diverticulitis were recognized with a comparison of preoperative CT scans of acute appendicitis with those of appendiceal diverticulitis.
Most appendiceal diverticula were false diverticula, formed by herniation of the mucosa and submucosa through a defect in the muscular layer. This is similar to the anatomical derangement seen in diverticula of the colon. Since the incidence of appendiceal diverticulitis among patients undergoing appendectomy has been reported to vary from 0.004% to 2.1%[1], appendiceal diverticulitis has been considered very rare. However, in our study, appendiceal diverticulitis was found to be a relatively common condition. We believe that the higher incidence in our study is due to the careful resection and pathological processing of the resected appendixes, allowing visualization of the inflamed diverticula. Inflammation of the appendiceal wall is usually very slight in patients with appendiceal diverticulitis in contrast to the intense inflammation observed in patients with acute appendicitis. If only slight inflammation of the appendiceal wall was noted even if the area around the appendix had abscess, we suspected appendiceal diverticulitis and carefully manipulated the specimens, processing multiple thin sections to detect the diverticulum. Usually, appendiceal diverticulitis is diagnosed only when the diverticulum is clearly visualized on a pathologic section. We speculate that appendiceal diverticulitis is overlooked and frequently misdiagnosed as acute appendicitis because the resected tissue is not adequately examined for diverticula. It is very important for both pathologists and surgeons to consider the possibility of appendiceal diverticulitis and to examine the specimen carefully.
Second, several studies have reported that the clinical features of appendiceal diverticulitis are different from those of acute appendicitis[10,11], and that appendiceal diverticulitis should be classified as a separate and unique diagnostic entity. Indeed, when one considers the mechanisms of onset of both diseases, we may gain insight into the differences in clinical characteristics.
Acute appendicitis occurs when the appendix lumen is obstructed[6,12]. Appendiceal obstruction may be caused by fecaliths, calculi, lymphoid hyperplasia, infectious processes, and benign or malignant tumors. The appendix subsequently becomes filled with mucus and swells, increasing pressure within the lumen and causing dull central or periumbilical abdominal pain[13]. Finally, the appendix becomes ischemic and necrotic, resulting in perforation. Well-localized pain occurs later when inflammation spreads to the adjacent parietal peritoneum.
On the other hand, appendiceal diverticulitis usually occurs in acquired diverticula[14], which contain only the mucosal and submucosal layers without a muscular layer. Because of these anatomical characteristics, diverticula can be easily perforated. Since only slight inflammation may be noted initially, symptoms such as dull central or periumbilical abdominal pain may be very slight. The development of localized abscess without well-localized pain occurs after several days, prolonging the duration of preoperative symptoms and increasing the rates of perforation and of intraperitoneal abscess in patients with appendiceal diverticulitis. The WBC level was decreased and the CRP level was increased in patients with appendiceal diverticulitis compared to those with acute appendicitis, suggesting that patients with appendiceal diverticulitis had a longer duration of inflammation at admission. These characteristics have also been reported by Yamana et al[10]. Compared to acute appendicitis, appendiceal diverticula occur mostly in older patients[11]. Appendiceal diverticulitis is often associated with localized abscess formation and perforation, often making surgery more difficult with increased surgical time and intraoperative blood loss compared to appendicitis surgery. The clinical features of appendiceal diverticulitis in our study are quite similar to those in previous reports, providing further evidence that the incidence of appendiceal diverticulitis is higher than previously reported.
Third, Lee et al[15] reported CT findings for 20 patients with appendiceal diverticulitis and commented on the diagnostic potential of CT in differentiating appendiceal diverticulitis from typical acute appendicitis. In 80% of patients with inflamed diverticula, CT revealed a round, cystic pouch with wall enhancement. An appendicolith was rarely present in patients with appendiceal diverticulitis compared to patients with acute appendicitis. Osada et al[16] reviewed the CT images of seven patients with pathologically diagnosed appendiceal diverticulitis. On CT scans, a total of 8 inflamed diverticula were observed as small fluid-filled luminal structures with thick, enhanced walls, or as solid, enhanced masses protruding from the appendix. Previous studies regarding the CT findings of appendiceal diverticulitis focused specifically on visualizing the inflamed diverticula. In this study, we compared the differences in CT findings between patients with acute appendicitis and those with appendiceal diverticulitis. In almost half of the cases with diverticulitis, the appendix was not visualized. We noted inflamed diverticula in only 24% of scans of patients with appendiceal diverticulitis. Fluid collection in the appendix was observed in 88% of patients with acute appendicitis, while seen in only 16% of patients with appendiceal diverticulitis. Therefore, while it is difficult to visualize the inflamed diverticula, CT findings showing an absence of a fluid level, absence of appendicolith, and the presence of localized abscess formation may indicate a possible inflamed appendiceal diverticulum.
Most of the patients who underwent appendectomy were diagnosed as either acute appendicitis or appendiceal diverticulitis. In patients presenting with possible appendicitis, but with atypical clinical features and the above-noted CT findings, a diagnosis of appendiceal diverticulitis should be considered. If CT shows that the appendix is not swollen, even though a localized abscess is noted around the appendix, this should be considered an indirect sign of appendiceal diverticulitis.
This study has several limitations, because it was a retrospective study. there may be a selection bias between the groups who performed CT scans and who did not.
To confirm the exact incidence of appendiceal diverticulitis and differeneces of CT findings between acute appendicitis and appendiceal diverticulitis, a prospective evaluation is necessary.
Despite these limitations, we believe that appendiceal diverticulitis can be diagnosed preoperatively with a combination of clinical features and suggestive findings on CT. If we are able to diagnose appendiceal diverticulitis accurately, we will be able to further investigate whether conservative antibiotic therapy or surgery is desirable for appendiceal diverticultis in the future.
In conclusion, the incidence of appendiceal diverticulitis was 9.7% in patients who underwent appendectomy. The CT findings and clinical features of patients with appendiceal diverticulitis were different from those of patients with acute appendicitis, suggesting it is possible to differentiate appendiceal diverticulitis from acute appendicitis on this basis.
Appendiceal diverticulitis is considered a relatively rare disease, and is usually the subject of case reports. Since right lower quadrant pain is the main clinical symptom of both acute appendicitis and appendiceal diverticulitis, appendiceal diverticulitis has been commonly dismissed as a variant of acute appendicitis. Therefore, a preoperative diagnosis is rarely made, and pathologists may fail to differentiate between acute appendicitis and appendiceal diverticulitis. However, recent studies have considered appendiceal diverticulitis as a separate clinical entity apart from typical acute appendicitis.
With regard to appendiceal diverticulitis, the current research hotspot is how to distinguish appendiceal diverticulitis from acute appendicitis and to accurately determine the incidence of appendiceal diverticulitis.
Appendiceal diverticulitis has been considered very rare. Previous reports have found that the incidence of appendiceal diverticulitis among patients undergoing appendectomy has been from 0.004%-2.1%, However, in this study of 451 patients who underwent appendectomy, 44 (9.7%) were pathologically diagnosed with appendiceal diverticulitis. The authors’ believe that the higher incidence in our study is due to the careful resection and pathological processing of the resected appendixes, allowing visualization of the inflamed diverticula. Moreover, the patients with appendiceal diverticulitis in this study had the same clinical features as in previous studies, even though the incidence of appendiceal diverticulitis was much higher in this study. This similar clinical presentation is further evidence suggesting a higher incidence of appendiceal diverticulitis. Computed tomography findings suggestive of appendiceal diverticulitis included the absence of a fluid collection in the appendix, absence of an appendicolith (92% vs 52%, P = 0.004), and abscess formation.
The study results suggest that it may be possible to clinically differentiate appendiceal diverticulitis from acute appendicitis.
Diverticula are small bulging pouches within the bowel wall that typically form within the large intestine, including the appendix. Appendiceal diverticula are relatively rare. Appendiceal diverticulitis is the result of inflammation of the appendiceal diverticulum.
This interesting study is focused on the clinical, pathological, and radiological features of appendiceal diverticulitis, an uncommon, but more common than previously believed condition commonly confused with acute appendicitis.
P- Reviewer: Contini S, Elpek GO, Goetze TO, Marrelli D S- Editor: Qi Y L- Editor: A E- Editor: Liu XM
| 1. | Trollope ML, Lindenauer SM. Diverticulosis of the appendix: a collective review. Dis Colon Rectum. 1974;17:200-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 35] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Kelynack TN. A contribution to the pathology of the vermiform appendix. London: HK Lewis 1893; 60-61. |
| 3. | Diener HC, Ehninger G, Schmidt H, Stäb U, Majer K, Marquardt B. [Neurologic complications after bone marrow transplantation]. Nervenarzt. 1991;62:221-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Abdullgaffar B. Diverticulosis and diverticulitis of the appendix. Int J Surg Pathol. 2009;17:231-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 73] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Seker D, Seker G, Kahramanca S, Gurler M, Turker A, Kulacoglu H. A rare but distinctive cause of acute abdomen: appendiceal diverticulitis. J Emerg Med. 2013;44:e61-e62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Birnbaum BA, Wilson SR. Appendicitis at the millennium. Radiology. 2000;215:337-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 401] [Cited by in RCA: 343] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 7. | Kubota T, Omori T, Yamamoto J, Nagai M, Tamaki S, Sasaki K. Sonographic findings of acute appendiceal diverticulitis. World J Gastroenterol. 2006;12:4104-4105. [PubMed] |
| 8. | Majeski J. Diverticulum of the vermiform appendix is associated with chronic abdominal pain. Am J Surg. 2003;186:129-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Phillips BJ, Perry CW. Appendiceal diverticulitis. Mayo Clin Proc. 1999;74:890-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Yamana I, Kawamoto S, Inada K, Nagao S, Yoshida T, Yamashita Y. Clinical characteristics of 12 cases of appendiceal diverticulitis: a comparison with 378 cases of acute appendicitis. Surg Today. 2012;42:363-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Sohn TJ, Chang YS, Kang JH, Kim DH, Lee TS, Han JK, Kim SH, Hong YO. Clinical characteristics of acute appendiceal diverticulitis. J Korean Surg Soc. 2013;84:33-37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Burkitt DP. The aetiology of appendicitis. Br J Surg. 1971;58:695-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 105] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Arnbjörnsson E, Bengmark S. Obstruction of the appendix lumen in relation to pathogenesis of acute appendicitis. Acta Chir Scand. 1983;149:789-791. [PubMed] |
| 14. | Collins DC. A study of 50,000 specimens of the human vermiform appendix. Surg Gynecol Obstet. 1955;101:437-445. [PubMed] |
| 15. | Lee KH, Lee HS, Park SH, Bajpai V, Choi YS, Kang SB, Kim KJ, Kim YH. Appendiceal diverticulitis: diagnosis and differentiation from usual acute appendicitis using computed tomography. J Comput Assist Tomogr. 2007;31:763-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Osada H, Ohno H, Saiga K, Watanabe W, Okada T, Honda N. Appendiceal diverticulitis: multidetector CT features. Jpn J Radiol. 2012;30:242-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |